Abstract
Neoadjuvant chemotherapy in breast cancer patients aims at preoperative reduction of tumor volume for better resection results and prognosis. As not all patients respond to neoadjuvant therapy, predictive biomarkers are needed for more efficient individual management. In prospectively collected sera of 51 consecutive locally confined breast cancer (LBC) patients receiving preoperative, neoadjuvant chemotherapy, value level kinetics of soluble high mobility group box 1 (HMGB1), soluble receptor for advanced glycation end products (sRAGE) as well as the established breast cancer biomarkers CA 15–3 and carcinoembryonic antigen (CEA) were investigated and correlated with therapy response objectified by pathological staging at surgery. In addition, biomarkers were measured in sera of 30 healthy controls (HC), 13 patients with benign breast diseases, and 28 metastatic breast cancer (MBC) patients. Pretherapeutic levels of soluble HMGB1 were decreased in MBC, while sRAGE was already decreased in LBC. In contrast, CA 15–3 and CEA were strongly elevated in MBC, but not in LBC. Combination of sRAGE and CA 15–3 enabled best discrimination of LBC from HC (AUC 78.2 %; sens 58 % at 95 % spec), while CA15-3 and CEA discriminated best between MBC and all controls (AUC 90.9 %; sens 70 % at 95 % spec). In LBC patients undergoing neoadjuvant chemotherapy, nine patients achieved complete remission (CR), 29 achieved partial remission (PR), while 13 had no change of disease (NC). NC patients tended to have higher HMGB1 and lower sRAGE levels before therapy onset (p = 0.056 and p = 0.054), while CA 15–3 and CEA did not predict therapeutic outcome. Furthermore, kinetics of HMGB1 during therapy correlated with efficacy of the treatment (p = 0.053). Markers of immunogenic cell death are valuable for the diagnosis of MBC and early estimation of response to neoadjuvant therapy in LBC patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
With 226,870 new cases and 39,510 women dying each year from this disease in the US, breast cancer is still the most common cancer among women [1]. Screening programs in many western countries have further improved rates of early stage detection of potentially curative breast cancer [2]. Negative prognostic factors in limited stage breast cancer include lymph node tumor infiltration, aggressive tumor growth pattern (grading), negative hormone receptor status, and Her2/neu and Ki-67 overexpression [3, 4]. Adjuvant systemic chemotherapy following primary surgery has been demonstrated to improve disease-free as well as overall survival (OS) in women with risk factors and is well established in clinical practice [5].
Neoadjuvant treatment concepts (primary systemic chemotherapy, PST) have been demonstrated to be effective in disease downstaging, thereby increasing rates of breast conserving surgery, and to be equally effective in erasing micrometastases [6–8]. PST was first used to treat inflammatory breast cancer and later, also locally advanced breast cancer. Results from the NSABP B-18 trial indicated that PST and adjuvant chemotherapy are equieffective with regard to progression-free survival (PFS) and OS in women with locally advanced breast cancer with an increased rate of breast conservation from 60 % to 68 % [6]. Many neoadjuvant chemotherapy regimens consist of six to eight chemotherapy cycles including docetaxel, adriamycin, and cyclophosphamid (TAC) or epirubicin and cyclophosphamide (EC) followed by docetaxel/paclitaxel with or without trastuzumab depending on Her2neu expression status [7, 8].
In addition, neoadjuvant chemotherapy treatment is considered a functional model of in vivo tumor treatment. While clinical responses were achieved in more than 80 % of patients, complete remission (CR) rates vary from 15 % to 30 % in Her2/neu-negative patients to 50 % in Her2/neu-overexpressing patient subsets [7]. Thus, the response rate (CR rate) correlates well with disease-free survival and OS [4, 5].
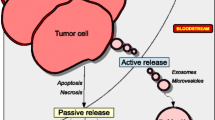
As not all patients benefit from a neoadjuvant therapy regimen, predictive and prognostic clinical and biochemical markers are still needed to pretherapeutically stratify patients for the most effective treatment and to monitor clinical response as early as possible [9]. Among the most promising candidates are breast cancer-related blood biomarkers such as carcinoembryonic antigen (CEA) and CA 15–3 [10], biomarkers of apoptotic and necrotic cell death such as nucleosomes and cytokeratins [11, 12], and markers of immunogenic cell death such as HMGB1 and soluble receptor for advanced glycation end products (sRAGE) that are known to be involved in anticancer stimulation of the immune system [13, 14].
In recent studies on lung cancer patients and patients with other tumors during chemo- and radiotherapy, we demonstrated that the cell death markers nucleosomes and cytokeratin-19 fragments (CYFRA 21–1) have great potential for predicting therapeutic response [12]. Most remarkably, the combination of both biomarkers indicated insufficient treatment efficacy in advanced nonsmall cell lung cancer patients already after 1 cycle of first-line chemotherapy with 29 % sensitivity at 100 % specificity and with 56 % sensitivity at 90 % specificity [15, 16]. Thus, application of these markers could provide an early tool for adjusting therapy in nonresponders.
High mobility group box 1 (HMGB1) protein is a nuclear protein with close association to the chromatin that plays an essential role in the regulation of transcription processes [17, 18]. While early studies reported that HMGB1 is only released during necrotic cell death, recent studies indicate a (potential) release of HMGB1 also during late apoptosis. However, in these cases, HMGB1 is still attached to the chromatin and may be released as HMGB1–nucleosome complexes [19]. In blood circulation, HMGB1 is known to act as a danger-associated molecular pattern (DAMP), a group of proteins binding to specific immune cells, and thus promoting phagocytation and presentation of pathogenic cell death products and, subsequently, stimulation of immune responses [17, 20]. The efficiency of HMGB1 was found to be increased when LPS, DNA, or nucleosomes were bound to HMGB1 [18]. A major mechanism of HMGB1 is the binding to specific receptors on dendritic or antigen-presenting cells such as the receptor for advanced glycation end products (RAGE) or the toll-like receptors 4 (TLR4), especially in association with bacterial lipopolysaccharides, and TLR2 in conjunction with nucleosomes [18, 21].
Phagocytized (tumor-related) particles are subsequently processed intracellularly and cross-presented at the cellular surface leading to promotion of tumor-specific cytotoxic T cell response [13, 22]. Recently, it was found that the release of DAMPs during immunogenic cell death, possibly based on biochemical features of necrosis and apoptosis, is essential for sustained therapy response after chemotherapy [22, 23]. Neutralization or knockdown of HMGB1 or knockout of TLR4 led to reduced anticancer immune response, both in vitro and in vivo with poor therapeutic outcome [22–24]. Nevertheless, whether serum levels of HMGB1 have prognostic or predictive relevance in cancer diseases remains to be seen [25, 26].
However, HMGB1 has dual opposite effects. Apart from triggering the protective T cell response, it also promotes neoangiogenesis [13, 14]. Overexpression of HMGB1 and its further receptor, the multiligand RAGE, is important for invasion and metastasis of tumors. This has been found in gastric cancer and colorectal cancer [27]. As the role of sRAGE is still not clear, this observation is most interesting. While surface RAGE is involved in transmission of DAMP signals, sRAGE can be shed from cells and acts as a decoy receptor inhibiting HMGB1 effects. Alternatively, it may simply correlate with a high expression of cellular sRAGE [28–30]. Here, this new and challenging set of markers involved in cell death, tumor growth, and immunogenicity is investigated in breast cancer patients in order to identify their role in prediction and early estimation of response to neoadjuvant chemotherapy.
Patients and methods
Patients
In the present study, 51 patients suffering from locally advanced breast cancer (stages: T2-4 N0, T2-4 N+, and T1N+) who received preoperative, neoadjuvant chemotherapy between 2007 and 2009 in the Oncological Outpatient Specialty Center Munich, were prospectively and consecutively included (Table 1). Chemotherapy consisted of 4 cycles of epirubicine (90 mg/m2) and cyclophosphamide (600 mg/m2), followed by 4 cycles of docetaxel (75 mg/m2) or paclitaxel (175 mg/m2). Herceptin was added to docetaxel in Her2/neu-overexpressing cases. After completion of chemotherapy, definitive surgery, either breast conserving or not, including axillary lymph node surgery, was carried out.
In all patients, blood was taken before the start of the first and second cycles and at the end of the therapy. As controls, serum samples from 30 healthy individuals, from 13 patients with benign breast diseases and 28 metastatic breast cancer (MBC) patients were used. The study was approved by the local ethics committee and written informed consent was obtained from all patients before the start of the treatment.
Evaluation of response to therapy
Response to neoadjuvant chemotherapy was evaluated by histopathology after surgical tumor resection. Findings were compared with staging investigations before the start of therapy. These were mainly performed by biopsy, sonography, and mammography. The response to therapy was classified according to RECIST criteria for solid tumors defining ‘complete remission’ as complete disappearance of all such manifestations of disease, ‘partial remission’ as reduction of tumor diameter ≥30 %, ‘progression’ as tumor increase ≥20 % or appearance of new tumor manifestations, and ‘stable disease’ as tumor reduction <30 % or increase <20 % in medical imaging [31]. Pathological complete remission (CR) was defined as the complete lack of histologically visible tumor cells in the final preparation.
Methods
Blood samples were centrifuged at 3,000 × g for 15 min within 1 to 2 h after venous puncture. Then, serum samples were aliquoted and stored at −80 °C. HMGB1 concentration was measured using the Sandwich ELISA of Shino-test/IBL (Tokyo, Japan/Hamburg, Germany). The wells of the microtiter strips were coated with purified anti-HMGB1 antibody. HMGB1 in the sample bound specifically to the immobilized antibody during an incubation of 24 h. After a washing step, a second enzyme-marked antibody was added that also recognizes HMGB1. After another washing, a color solution was added for 30 min. Next, the HMGB1 concentration was photometrically determined at 450 nm (reference wavelength at 600–650 nm) with respect to a standard curve as part of the assay kit.
Levels of sRAGE were measured with the Quantikine® Colorimetric Sandwich ELISA of R&D Systems (Abingdon, UK). A monoclonal antibody specific for RAGE (extracellular domain) was precoated onto a microplate. Standards and samples were pipetted into the wells and any RAGE present was bound by the immobilized antibody. After washing off any unbound substances, an enzyme-linked polyclonal antibody specific for RAGE (extracellular domain) was added to the wells. Following a further washing step, a substrate solution was added to the wells. The color development was stopped after 30 min and the intensity of the color was measured photometrically at 450 nm (reference wavelength at 540–570 nm). sRAGE concentrations were calculated according a standard curve as part of the kit.
Prior to this study, HMGB1 and sRAGE assays were tested for their methodical quality including intra- and interassay imprecision and dilution linearity of the assay as well as some influencing factors, such as freeze-thawing, use of different materials (serum/plasma), and storage at different temperatures, and times before and after centrifugation on sRAGE and HMGB1 values. As a result, both assays showed good methodical quality and robustness against preanalytic influences [32, 33]. In all ELISAs, the sample series of single patients were each determined within one run of the assays to minimize methodical variance. Furthermore, serum pools in diverse value ranges were included in all assays to control interassay variability. CEA and CA 15–3 were measured by enzymatic chemiluminescent immunoassay (ECLIA) on the Elecsys 2010 immunoassay analyzer of Roche Diagnostics, Germany.
Statistics
Concentrations of all measured markers before the first and the second cycles and at the end of therapy as well as their percentage changes were considered for statistical evaluation. Concerning their response to therapy, CR and PR were combined into the ‘responder’ group, where they were compared with results from patients who suffered from no change or progressive disease.
Comparison of biomarker concentrations between the diagnostic groups and between groups with different therapy responses was done by the Wilcoxon test. Results are presented in tables as medians, percentiles, and respective p values as well as dot plots. Discriminative power is further demonstrated in receiver operating characteristic (ROC) curves. A p value of <0.05 was considered statistically significant. All calculations were performed with SAS software (version 9.2, SAS Institute Inc., Cary, NC, USA).
Results
Patients with primary LBC had significantly lower pretherapeutic sRAGE concentrations than healthy controls (HC). However, no significant concentration differences were found for HMGB1 or the established markers CA 15–3 and CEA in these two groups. In MBC, HMGB1 levels were significantly lower and CA 15–3 and CEA levels were significantly increased when compared to HC and patients with benign diseases, while for sRAGE, no significant difference was found (Table 2, Fig. 1).
In the pretherapeutic parameters, a general correlation was observed for CEA and CA 15–3 (R = 0.43; p < 0.001), while HMGB1 and CEA correlated inversely (R = −0.32; p = 0.001). In HC, CA 15–3 correlated positively with sRAGE (R = 0.36; p = 0.50); in benign controls, CA 15–3 and HMGB1 (R = 0.71; p = 0.009); in MBC, CEA and CA 15–3 (R = 0.81; p < 0.001), while in LBC, no marker correlation was observed.
In ROC curves, sRAGE showed the best discrimination of LBC from HC (AUC 78.2 %). Although the combination of sRAGE and CA 15–3 yielded a comparable AUC, the sensitivity at 95 % specificity was increased from 34 % to 58 % (Fig. 2a). Concerning the comparison of MBC and all other control groups, CA 15–3 and CEA achieved similar AUCs of 85.4 % and 86.5 %, respectively. Although the combination of both markers increased the AUC slightly to 90.9 %, sensitivity (70 % at 95 %, specificity) was similar to the single markers CEA (70 %) and CA 15–3 (63 %; Fig. 2b).
Of all LBC patients undergoing neoadjuvant chemotherapy, nine achieved complete pathological complete remission (pCR) and 29 partial remission (PR), while in 13 patients, there was no change of disease (NC) status. Pretherapeutic HMGB1 levels tended to be higher in NC patients (median 1.9 ng/mL) when compared with CR or PR patients (1.1 ng/mL; p = 0.056). sRAGE levels were lower in nonresponsive patients (NC 0.48 ng/mL; CR + PR 0.69 ng/mL; p = 0.054), while no differences were found in pretherapeutic values of CA 15–3 and CEA in both response groups (Fig. 3a, b; Table 3). During the course of chemotherapy, there was a drop in HMGB1 values and an increase of sRAGE, CEA, and CA 15–3 values. However, only kinetics of HMGB1 during therapy tended to correlate with efficacy of the treatment (p = 0.053; Table 3). AUCs for the discrimination of response groups (NC vs. CR and PR) revealed best performance for pretherapeutic sRAGE (70.4 %) and HMGB1 (69.3 %; Fig. 3c).
Discussion
For patients with LBC, neoadjuvant chemotherapy is an effective new therapeutic option that reduces tumor size and enables preoperative tumor downstaging, thereby improving surgical treatment results. Long-term outcome in these patients is at least equal to adjuvant chemotherapy after tumor resection [6–8]. As very small nodules are removed immediately by breast-conserving surgery and as patients with lymph node involvement N3 and metastases are not eligible for surgery anymore, neoadjuvant chemotherapy is mainly applied to patients with stage 2 tumor disease [6–8].
Diverse regimens are currently used in the neoadjuvant setting. Most of them contain parallel or serial combinations of substances as used in this study, such as epirubicine, cyclophosphamide, docetaxel, and paclitaxel. These antineoplastic drugs are able to stop or decelerate tumor growth by inhibition of tumor cell division and proliferation or by induction of tumor cell death [7, 8]. The effectivity of these drugs, however, is accompanied by considerable toxicity, such as bone marrow suppression and gastrointestinal and neuronal side effects, especially when the substances accumulate in the body [6–8].
As only some of the patients will benefit from neoadjuvant therapy in terms of significant tumor mass reduction, it is highly desirable to identify patients who are not responsive to the therapy as early as possible in order to adapt the treatment accordingly. This would potentially enable a more efficient therapy and avoid unnecessary toxic side effects for the patient.
Monitoring the individual response to therapy is regularly done by imaging techniques such as computed and magnetic resonance tomography, sonography, and mammography [6, 8]. However, these approaches are costly and show mainly macroscopic changes of tumor volume after several therapy cycles. Changes in tumor biology and direct effects of cytotoxic therapy may be monitored more appropriately with serial measurements of blood biomarkers which are affected by treatment or which mirror biochemical tumor characteristics, such as rates of proliferation and cell death [9, 12].
Cell death biomarkers, such as nucleosomes or cytokeratin fragments, have been found to be highly relevant for prognosis, therapy prediction and monitoring, and early estimation of therapy response in various cancers [12, 34, 35]. In patients with advanced NSCLC, nucleosomes and cytokeratin-19 fragments indicated early–already after one application of chemotherapy–and specifically nonresponse to the treatment [15, 16, 36]. Similar results were obtained in patients with SCLC [37], gastrointestinal cancers [38, 39], and, very recently, in patients with breast cancer undergoing neoadjuvant chemotherapy [40]. In all these settings, high concentrations of nucleosomes before or during therapy were associated with poor therapy response or unfavorable prognosis.
A further biomarker released into circulation during necrotic and apoptotic cell death is the nuclear HMGB1 protein. Especially during apoptosis, HMGB1 is liberated as HMGB1–nucleosome complexes and acts in the blood as a powerful DAMP able to stimulate immune cells efficiently, inter alia by interaction with specific receptors, such as RAGE, TLR4, and TLR2 [17–20]. As the actions of DAMPs during immunogenic cell death are not only known to be crucial for sustained therapy response after chemotherapy, but are also relevant for procarcinogenic processes, such as neoangiogenesis and metastasis, circulating HMGB1 and sRAGE seem to be promising candidates for therapy prediction and prognosis [13, 22–24].
Interestingly, we found decreased levels of sRAGE already in LBC, while HMGB1, CEA, and CA 15–3 remained unchanged. This finding is in line with other studies on sRAGE in pancreatic cancer [41, 42], colorectal cancer [43], lung cancer [44], and breast cancer [45], suggesting that low sRAGE levels contribute to carcinogenesis already in the early stages. In the metastatic stage, HMGB1 was also decreased. This observation was surprising as many studies have found high HMGB1 levels in diverse cancers, especially in advanced stages, such as lung [26, 46], gastric [25], liver [47], and cervical cancers [48]. One explanation may be attributed to the finding that HMGB1 can be masked by serum or plasma proteins such as IgG in certain pathophysiology conditions possibly present especially in systemic tumor disease, with the consequence of false-negative results by conventional ELISA methods [49]. In concordance with clinical experience and many studies, CA 15–3 and CEA were expressed and released in high amounts into blood circulation [50–52]. They correlated well and showed the best performance in ROC curves in advanced disease, while the combination or sRAGE and CA 15–3 had the best profile in local disease.
Concerning prediction of therapy response, high pretherapeutic HMGB1 levels and low sRAGE levels predicted a later therapy response. Interestingly, about one-third of responsive patients could be detected by low HMGB1 values with high specificity as they were lower than those of nonresponsive patients. Furthermore, HMGB1 kinetics during therapy indicated efficacy. The fact that these results were only borderline significant may be attributed to the limited number of patients in the nonresponsive group. Nevertheless, it has to be emphasized that standardized serial blood drawings, controlled preanalytics, and detailed clinical documentation in a prospective single-center study consecutively enrolling a homogenous group of breast cancer patients undergoing defined neoadjuvant therapies was a clinically and (pre-)analytically highly challenging approach which led to the identification of new biomarkers relevant for response prediction and therapy monitoring of these patients. In particular, it has to be mentioned that the established tumor-related biomarkers CA 15–3 and CEA, which were measured in parallel as reference biomarkers, failed to indicate therapy response, neither before nor during therapy.
Conclusion
This is, to our knowledge, the first study showing the relevance of the immunogenic cell death biomarkers HMGB1 and sRAGE for prediction of response to neoadjuvant chemotherapy in LBC patients. These results will have to be validated in larger prospective clinical studies.
References
Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012;62:10–29.
Ozols RF, Herbst RS, Colson YL, et al. American Society of Clinical Oncology. Clinical cancer advances 2006: major research advances in cancer treatment, prevention, and screening—a report from the American Society of Clinical Oncology. J Clin Oncol. 2007;25:146–62.
Bundret NJ. Prognostic and predictive factors in breast cancer. Cancer Trial Rev. 2001;27:137–42.
Von Minckwitz G. Neoadjuvant chemotherapy in breast cancer—insights from the German experience. Breast Cancer 2012; published online.
EBCTCG. Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Early Breast Cancer Trialists Collaborative Group. Lancet. 2005;365:1687–717.
Wolmark N, Wang J, Mamounas E, et al. Preoperative chemotherapy in patients with operable breast cancer: nine-year results from National Surgical Adjuvant Breast and Bowel Project B-18. J Natl Cancer Inst Monogr. 2001;30:96–102.
Buzdar AU, Ibrahim NK, Francis D, et al. Significantly higher pathologic complete remission rate after neoadjuvant therapy with trastuzumab, paclitaxel, and epirubicin chemotherapy: results of a randomized trial in human epidermal growth factor receptor 2-positive operable breast cancer. J Clin Oncol. 2005;23:3676–85.
Kaufmann M, von Minckwitz G, Mamounas EP, Cameron D, Carey LA, Cristofanilli M, Denkert C, Eiermann W, Gnant M, Harris JR, Karn T, Liedtke C, Mauri D, Rouzier R, Ruckhaeberle E, Semiglazov V, Symmans WF, Tutt A, Pusztai L. Recommendations from an international consensus conference on the current status and future of neoadjuvant systemic therapy in primary breast cancer. Ann Surg Oncol. 2012;19:1508–16.
Beachy SH, Repasky EA. Using extracellular biomarkers for monitoring efficacy of therapeutics in cancer patients: an update. Cancer Immunol Immunother. 2008;57:759–75.
Sturgeon CM, Duffy MJ, Stenman UH, et al. National Academy of Clinical Biochemistry laboratory medicine practice guidelines for use of tumor markers in testicular, prostate, colorectal, breast, and ovarian cancers. Clin Chem. 2008;54:e11–79.
Holdenrieder S, Stieber P. Apoptotic markers in cancer. Clin Biochem. 2004;37:605–17.
Holdenrieder S, Stieber P. Clinical use of circulating nucleosomes. Crit Rev Lab Med Sci. 2009;46:1–24.
Sims GP, Rowe DC, Rietdijk ST, Herbst R, Coyle AJ. HMGB1 and RAGE in inflammation and cancer. Annu Rev Immunol. 2010;28:367–88.
Zitvogel L, Apetoh L, Ghiringhelli F, Kroemer G. Immunological aspects of cancer chemotherapy. Nat Rev Immunol. 2008;8:59–73.
Holdenrieder S, Stieber P, von Pawel J, et al. Circulating nucleosomes predict the response to chemotherapy in patients with advanced non small cell lung cancer. Clin Cancer Res. 2004;10:5981–7.
Holdenrieder S, Stieber P, von Pawel J, et al. Early and specific prediction of the therapeutic efficacy in lung cancer by nucleosomal DNA and cytokeratin 19 fragments. Ann N Y Acad Sci. 2006;1075:244–75.
Lotze MT, Tracey KJ. High-mobility group box 1 protein (HMGB1): nuclear weapon in the immune arsenal. Nat Rev Immunol. 2005;5:331–42.
Bianchi ME. HMGB1 loves company. J Leukocyte Biology. 2009;86:573–76.
Urbonaviciute V, Fürnrohr BG, Meister S, Munoz L, Heyder P, De Marchis F, Bianchi ME, Kirschning C, Wagner H, Manfredi AA, Kalden JR, Schett G, Rovere-Querini P, Herrmann M, Voll RE. Induction of inflammatory and immune responses by HMGB1–nucleosome complexes: implications for the pathogenesis of SLE. J Exp Med. 2008;205:3007–18.
Tesniere A, Panaretakis T, Kepp O, Apetoh L, Ghiringhelli F, Zitvogel L, Kroemer G. Molecular characteristics of immunogenic cancer cell death. Cell Death and Differentiation. 2008;15:3–12.
Park JS. G-RF, He Q, Svetkauskaite D, Kim JY, Strassheim D, Sohn JW, Yamada S, Maruyama I, Banerjee A, et al.: High mobility group box 1 protein interacts with multiple toll-like receptors. Am J Physiol Cell Physiol. 2006;290:917–24.
Kepp O, Tesniere A, Schlemmer F, Michaud M, Senovilla L, Zitvogel L, Kroemer G. Immunogenic cell death modalities and their impact on cancer treatment. Apoptosis. 2009;14:364–75.
Apetoh L, Ghiringhelli F, Tesniere A, et al. Toll-like receptor 4-dependent contribution of the immune system to anticancer chemotherapy and radiotherapy. Nat Med. 2007;13:1050–9.
Apetoh L, Tesniere A, Ghiringhelli F, Kroemer G, Zitvogel L. Molecular interactions between dying tumor cells and the innate immune system determine the efficacy of conventional anticancer therapies. Cancer Res. 2008;68:4026–30.
Chung HW, Lee SG, Kim H, Hong DJ, Chung JB, Stroncek D, Lim JB. Serum high mobility group box-1 (HMGB1) is closely associated with the clinical and pathologic features of gastric cancer. J Transl Med. 2009;7:38.
Naumnik W, Nilklińska W, Ossolińska M, Chyczewska E. Serum levels of HMGB1, survivin, and VEGF in patients with advanced non-small cell lung cancer during chemotherapy. Folia Histochem Cytobiol. 2009;47:703–9.
Tang DL, Kang R, Zeh HJ, Lotze MT. High-mobility group box 1 and cancer. Biochimica Et Biophysica Acta-Gene Regulatory Mechanisms. 2010;1799:131–40.
Bierhaus A, Nawroth PP. Multiple levels of regulation determine the role of the receptor for AGE (RAGE) as common soil in inflammation, immune responses and diabetes mellitus and its complications. Diabetologica. 2009;52:2251–63.
Sparvero LJ, Asafu-Adjei D, Kang R, Tang D, Amin N, Im J, Rutledge R, Lin B, Amoscato AA, Zeh HJ, Lotze MT. RAGE (receptor for advanced glycation endproducts), RAGE ligands, and their role in cancer and inflammation. Journal of Translational Medicine. 2010;7:17.
Geroldi D, Falcone C, Emanuele E. Soluble receptor for advanced glycation end products: from disease marker to potential therapeutic target. Curr Med Chem. 2006;13:1971–8.
Therasse P, Arbuck SG, Eisenhauer EA, et al. New guidelines to evaluate the response to treatment in solid tumors. J Natl Cancer Inst. 2000;92:205–16.
Lehner J, Wittwer C, Fersching D, Siegele B, Holdenrieder S, Stoetzer OJ. Methodical and preanalytical evaluation of an HMGB1 immunoassay. Anticancer Res. 2012;32:2059–62.
Wittwer C, Lehner J, Fersching D, Siegele B, Stoetzer OJ, Holdenrieder S. Methodical and preanalytical evaluation of a RAGE immunoassay. Anticancer Res. 2012;32:2075–78.
Holdenrieder S, Nagel D, Stieber P. Estimation of prognosis by circulating biomarkers in patients with non-small cell lung cancer. Cancer Biomarkers. 2010;6:179–90.
Barak V, Holdenrieder S, Nisman B, Stieber P. Relevance of circulating biomarkers for the therapy monitoring and follow-up investigations in patients with non-small cell lung cancer. Cancer Biomarkers. 2010;6:191–6.
Kumar S, Guleria R, Singh V, Bharti AC, Mohan A, Das BC. Plasma nucleosome levels might predict response to therapy in patients with advanced non-small-cell lung cancer. Clin Lung Cancer. 2010;11:36–44.
Holdenrieder S. v Pawel J, Dankelmann E, et al. Nucleosomes, ProGRP, NSE, CYFRA 21–1 and CEA in the therapy monitoring of small-cell lung cancer during first-line chemotherapy. Clin Cancer Res. 2008;14:7813–21.
Kremer A, Wilkowski R, Holdenrieder S, et al. Nucleosomes in pancreatic cancer patients during radiochemotherapy. Tumour Biol. 2005;26:44–9.
Kremer A, Holdenrieder S, Stieber P, et al. Nucleosomes in colorectal cancer patients during radiochemotherapy. Tumour Biol. 2006;27:235–42.
Stötzer OJ, Fersching DIM, Salat C, Siegele B, Nagel D, Holdenrieder S. Prediction of response to neoadjuvant chemotherapy in breast cancer patients by circulating circulating nucleosomes, DNAse activity, M30 and survivin. Cancer Lett, submitted
Jiao L, Weinstein SJ, Albanes D, Taylor PR, Graubard BI, Virtamo J, Stolzenberg-Solomon RZ. Evidence that serum levels of the soluble receptor for advanced glycation end products are inversely associated with pancreatic cancer risk: a prospective study. Cancer Res. 2011;71:3582–9.
Krechler T, Jáchymová M, Mestek O, Zák A, Zima T, Kalousová M. Soluble receptor for advanced glycation end-products (sRAGE) and polymorphisms of RAGE and glyoxalase I genes in patients with pancreas cancer. Clin Biochem. 2010;43:882–6.
Jiao L, Taylor PR, Weinstein SJ, Graubard BI, Virtamo J, Albanes D, Stolzenberg-Solomon RZ. Advanced glycation end products, soluble receptor for advanced glycation end products, and risk of colorectal cancer. Cancer Epidemiol Biomarkers Prev. 2011;20:1430–8.
Jing R, Cui M, Wang J, Wang H. Receptor for advanced glycation end products (RAGE) soluble form (sRAGE): a new biomarker for lung cancer. Neoplasma. 2010;57:55–61.
Tesarová P, Kalousová M, Jáchymová M, Mestek O, Petruzelka L, Zima T. Receptor for advanced glycation end products (RAGE)—soluble form (sRAGE) and gene polymorphisms in patients with breast cancer. Cancer Invest. 2007;25:720–5.
Shang GH, Jia CQ, Tian H, Xiao W, Li Y, Wang AH, Dong L, Lin DJ. Serum high mobility group box protein 1 as a clinical marker for non-small cell lung cancer. Respir Med. 2009;103:1949–53.
Cheng BQ, Jia CQ, Liu CT, Lu XF, Zhong N, Zhang ZL, Fan W, Li YQ. Serum high mobility group box chromosomal protein 1 is associated with clinicopathologic features in patients with hepatocellular carcinoma. Dig Liver Dis. 2008;40:446–52.
Sheng X, Du X, Zhang X, Li D, Lu C, Li Q, Ma Z, Song Q, Wang C. Clinical value of serum HMGB1 levels in early detection of recurrent squamous cell carcinoma of uterine cervix: comparison with serum SCCA, CYFRA21-1, and CEA levels. Croat Med J. 2009;50:455–64.
Urbonaviciute V, Fürnrohr BG, Weber C, Haslbeck M, Wilhelm S, Herrmann M, Voll RE. Factors masking HMGB1 in human serum and plasma. J Leukoc Biol. 2007;81:67–74.
Molina R, Barak V, van Dalen A, Duffy MJ, Einarsson R, Gion M, Goike H, Lamerz R, Nap M, Sölétormos G, Stieber P. Tumor markers in breast cancer—European Group on Tumor Markers recommendations. Tumour Biol. 2005;26:281–93.
Laessig D, Nagel D, Heinemann V, Untch M, Kahlert S, Bauerfeind I, Stieber P. Importance of CEA and CA 15–3 during disease progression in metastatic breast cancer patients. Anticancer Res. 2007;27:1963–8.
Molina R, Gion M, Gressner A, Troalen F, Auge JM, Holdenrieder S, Zancan M, Wycislo M, Stieber P. Alternative antibody for the detection of CA15-3 antigen: a European multicenter study for the evaluation of the analytical and clinical performance of the Access BR Monitor assay on the UniCel Dxl 800 Immunoassay System. Clin Chem Lab Med. 2008;46:612–22.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary materials
Below is the link to the electronic supplementary material.
ESM 1
(PPT 503 kb)
Rights and permissions
About this article
Cite this article
Stoetzer, O.J., Fersching, D.M.I., Salat, C. et al. Circulating immunogenic cell death biomarkers HMGB1 and RAGE in breast cancer patients during neoadjuvant chemotherapy. Tumor Biol. 34, 81–90 (2013). https://doi.org/10.1007/s13277-012-0513-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-012-0513-1