Summary
Background
The purpose of this study was to evaluate the relationships between interleukin 10 (IL10) (rs1800896) and interleukin 1B (IL1B) (rs16944) genetic polymorphisms and the risk for cervical cancer in a cohort of women from Croatia.
Methods
A case–control study of 81 patients with cervical cancer and 80 age-matched healthy controls was performed. We collected peripheral blood samples, extracted deoxiribonucleic acid (DNA), and analyzed two single-nucleotide polymorphisms (SNPs) rs1800896 and rs16944 using TaqMan assays (Fa. Thermo Fisher Scientific, Waltham, MA, USA) and real-time polymerase chain reaction (PCR). We investigated a possible association between two cytokine genetic polymorphisms and the occurrence of cervical cancer.
Results
Our results showed no significant difference in the frequency of IL10 (rs1800896) and IL1B (rs16944) genotypes between the patients and the controls (χ2 test, P < 0.05).
Conclusion
In this study, no association was found between IL10 rs1800896 and IL1B rs16944 polymorphisms and cervical cancer development.
Zusammenfassung
Grundlagen
Das Ziel der vorliegenden Studie war, die Beziehung zwischen den genetischen Polymorphismen IL10 (rs1800896) und IL1B (rs16944) und dem Risiko für Gebärmutterhalskrebs in einer Kohorte von Frauen aus Kroatien zu untersuchen.
Methodik
Es wurde eine Fall-Kontroll-Studie mit 81 Frauen mit invasivem Gebärmutterhalskrebs und 80 altersentsprechenden gesunden Kontrollen durchgeführt. Dazu wurden periphere Blutproben gesammelt, DNA extrahiert und 2 Einzelnukleotidpolymorphismen (SNP; rs1800896 und rs16944) unter Verwendung von TaqMan-Assays (Fa. Thermo Fisher Scientific, Waltham, MA, USA) und der Echtzeit-Polymerasekettenreaktion (PCR) analysiert. Die Autor*innen untersuchten einen möglichen Zusammenhang zwischen dem genetischen Polymorphismus zweier Zytokine und dem Auftreten des Zervixkarzinoms.
Ergebnisse
Dabei zeigte sich kein signifikanter Unterschied in der Häufigkeit der Genotypen IL10 (rs1800896) und IL1B (rs16944) zwischen den Patienten und gesunden Kontrollen (χ2-Test, p < 0,05).
Schlussfolgerung
In dieser Studie wurde kein Zusammenhang zwischen den Polymorphismen IL10 rs1800896 und IL1B rs16944 und der Entwicklung von Gebärmutterhalskrebs festgestellt.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cervical cancer (CC) is considered to be the fourth most common type of cancer in women worldwide. Human papillomavirus (HPV) is central to the development of CC and can be detected in 99.7% of cervical cancers [1]. Most genital HPV infections are transient and the majority of HPV-infected women do not develop CC, because HPV alone is not sufficient to cause invasive disease. The key factor in controlling HPV infection is the immune response [2]. Chronic inflammation and the local immune microenvironment also participate in the neoplastic process [3, 4]. Mechanisms that link virus infection, immune response, chronic inflammation, and cancer development include cytokines produced by activated innate immune cells [3, 5]. The cell-mediated immune response can be reflected as changes in cytokine levels in the cervix [6]. During chronic inflammation, cytokines modulate anti-tumor responses and promote cell transformation [7]. Numerous studies have demonstrated that genetic variants play a critical role in cervical cancer development [8,9,10]. It has been reported that several interleukin genes are associated with development of cervical cancer [11].
Interleukin 10 (IL-10) is the central immune regulator and mediator of the anti-inflammatory response that inhibits production of TNF‑α, IL‑6, and IL-12, which are major proinflammatory cytokines [5, 12]. IL-10 is an important negative regulator of the tumor immune microenvironment [13, 14]. The interaction between HPV and IL-10 can lead to an immunosuppressive environment in the cervix and, consequently, to the persistence of HPV infection, progression of cervical intraepithelial lesions, and finally to cervical cancer development [13,14,15]. Also, accumulating data have shown that during HPV infection, IL-10 levels are enhanced, and that IL-10 stimulates HPV E6 and E7 expression [13]. In the past few decades, the association between IL10 polymorphisms and cervical cancer risk has been the subject of a large number of studies, but with contradictory results [14, 16].
Interleukin 1B (IL-1B) is a proinflammatory cytokine mainly produced during inflammation. Recent studies suggest the important role of chronic inflammation in HPV pathogenesis and promotion of carcinogenesis [17]. Higher levels of proinflammatory cytokines, including IL-1B, were found in women with persistent HPV infection [18]. Several studies have shown an association between IL1B polymorphisms and the risk of gastric and prostate cancers [19,20,21]. Studies regarding CC have revealed that serum IL-1B levels and IL1B polymorphisms may be considered as biomarkers for CC [11, 22].
Considering that many studies have previously shown the association between polymorphisms in cytokine genes and cancer development, we decided to investigate selected single-nucleotide polymorphisms (SNPs) as potential risk factors for cervical cancer development. Our objective was to evaluate the possible correlation of IL10 polymorphism (rs1800896) and IL1B polymorphism (rs16944) with the risk of cervical cancer.
Materials and methods
Among 161 participants, 81 patients with cervical cancer (mean age 53 ± 12 years) were compared with 80 healthy women (mean age 53 ± 11 years). The cervical cancer diagnosis was confirmed by pathohistological examinations of tumor tissues. The control group was represented by age-matched healthy women without a history of malignant disease, chronic systemic inflammatory disorders, conization, or a pathohistologically proven cervical intraepithelial lesion. Only women with three or more consecutive normal Pap smears were included in the control group.
The blood samples were collected at the University Hospital for Tumors, Sestre Milosrdnice University Hospital Center, (Zagreb, Croatia) after obtaining written informed consent from each patient.
According to the manufacturer’s instructions, DNA was extracted from 200 μl of EDTA-anticoagulated peripheral whole blood using spin colons for DNA extraction QIAamp DNA Blood Mini Kit (Qiagen GmBH, Germany) and samples were stored at −20 °C. SNP genotype analysis (rs1800896 and rs16944) was performed using TaqMan-based fluorescent probes (TaqMan SNP Genotyping Assays, Fa. Thermo Fisher Scientific, Waltham, MA, USA) on the ABI PRISM 7500 real-time PCR system (Applied Biosystems, Foster City, CA, USA). The thermocycling procedure consisted of 10-minute holds at 95 °C, 15-second denaturation at 92 °C in 40 cycles, and 60-second primer annealing and extensions at 60 °C. Control samples were run simultaneously within each analyzed real-time PCR plate. The total reaction volume was 25 μL with 5 μL of DNA used as a template.
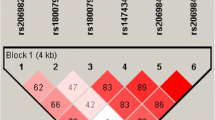
Statistical analyses were performed using the SHEsis software [23]. Analyses of genotypes were conducted using SNPstats software [24]. Pearson chi-square test was used for the analysis of allele frequency differences.
Results
A total of 161 subjects participated in the study, including 81 patients with a diagnosis of cervical cancer and 80 patients in the control group.
There was no statistically significant difference in IL10 gene polymorphism rs1800896 (−1082A > G) and IL1B gene polymorphism rs16944 (−511C/T) between patients with cervical cancer and the control group (Table 1).
The genotype distributions and frequencies of polymorphism rs1800896 (−1082A > G) in the IL10 gene are shown in Table 2, while genotype distributions and frequencies of the IL1B gene polymorphism rs16944 (−511C/T) are presented in Table 3. The data showed no significant difference in distributions and frequencies of the genotypes between the case and the control groups.
Furthermore, the analysis of the three genetic models by SNPStats software showed that the IL10 rs1800896 (−1082A > G) polymorphism and the IL1B rs16944 (−511C/T) polymorphism are not associated with the risk for cervical cancer development (Tables 4 and 5).
Discussion
Chronic inflammation has a significant influence on the pathogenesis of various disorders, especially carcinogenesis [17, 25]. Inflammation-related genetic polymorphism could be associated with the development of cervical cancer.
Several studies have demonstrated a correlation between genetic variants of IL10 and the cervical cancer risk [14, 16, 26]. The IL10 gene is located on chromosome 1 and contains five exons and four introns that encode 178 amino acids [16, 27]. The three most common IL10 SNPs that have been reported to significantly influence cervical cancer risk are −819T > C (rs1800871), −1082A > G (rs1800870), and −592C > A (rs1800872) [14, 16]. In 2018, meta-analyses found a significant association of rs1800870 and rs1800871 polymorphisms with the risk of cervical cancer development, while an association between rs1800872 polymorphism and the risk of cervical cancer was not found [16].
In our study, we decided to investigate a less-commonly researched IL10 single-nucleotide polymorphism, rs1800896, and its association with cervical cancer susceptibility. Kingo et al. found that the rs1800896 polymorphism may have an influence on IL10 mRNA expression and consequently on the production of IL-10 [28]. Recently, an IL10 rs1800896 polymorphism has been reported to increase the risk of acute pancreatitis, liver cirrhosis, esophageal cancer, oral cancer, and colorectal cancer [29,30,31], and to decrease the risk of prostate cancer [30]. Only a few studies have examined the association between the rs1800896 polymorphism and the risk for cervical cancer. Singhal et al. found a fourfold higher risk of cervical cancer associated with the rs1800896 polymorphism (−1082 variant genotype GG) [32]. Other studies did not find an association between the IL10 rs1800896 polymorphism and the cervical cancer risk [33,34,35]. At present, the genetic association between this particular SNP and cervical cancer susceptibility has not been finally determined. Hao et al. concluded in their meta-analysis that the IL10 gene has an ethnicity-specific effect [30] and that studies with more diverse ethnic populations should be performed. Our study failed to find an association between the IL10 gene rs1800896 polymorphism and the risk of cervical cancer in the Croatian population.
Due to the association between increased IL-1B levels and development of cervical cancer [22], several studies attached importance to evaluating whether polymorphisms of the IL1B gene, which is highly polymorphic, have an effect on the development of cervical cancer. The base transition between C and T at position −511 (C–T; dbSNP: rs16944) located in the promoter region has been widely reported. That transition may influence IL-1B protein expression. Previously, the association between the IL1B rs16944 polymorphism and various human cancers, such as gastric, lung, and breast cancer, was investigated, but results are inconsistent and inconclusive [36]. Several studies showed that certain genotypes of the IL1B gene are associated with cervical cancer development [11]. Kang et al. first reported that the IL1B −511 polymorphism is related to cervical cancer risk [37]. Their results confirmed the hypothesis that the −511 T allele causes an increased production of IL-1B and consequently influences cervical carcinogenesis [37]. In their meta-analysis, Xu et al. showed that the IL1B + 3954C/T polymorphism was associated with an overall increased risk for cancer and that the IL1B −511C/T (rs16944) polymorphism was associated with an increased risk of cervical cancer development [36]. Qian et al. found that genotypes IL1B T‑31C TC/CC and C‑511T CT/TT were associated with an increased risk of cervical cancer, especially among patients with higher IL-1B levels, and concluded that the functional IL1B genotypes may modify plasma IL-1B concentrations and consequently contribute to cervical cancer development [38]. Wang et al. also showed that the IL1B rs16944 polymorphism significantly increased cervical cancer risk in the Chinese Uygur female [11]. The IL1B rs16944 polymorphism is also associated with a higher risk of cervical cancer development in the Egyptian population [22]. Our study did not provide evidence for an association between the IL1B rs16944 polymorphism and the risk for cervical cancer in the Croatian population.
To the best of our knowledge, this is the first study that has investigated the association between IL10 rs1800896 and IL1B rs16944 polymorphisms and cervical cancer susceptibility in the Croatian/European population. A major limitation of the present study is the small sample size, which can reduce reliability of the results. Furthermore, additional risk factors for cervical cancer epidemiology, such as smoking, use of oral contraceptives, and sexual behavior, were not included in the analysis. It would therefore be worthwhile to perform further studies on IL10 rs1800896 and IL1B rs16944 polymorphisms in European populations, which would include larger number of patients and take into account additional risk factors for cervical cancer.
Conclusion
In conclusion, within the limitations, our study did not provide evidence of an association between IL10 rs1800896 and IL1B rs16944 polymorphisms and the risk for cervical cancer. These results need to be taken with caution and further studies with a larger sample size are warranted to establish the role of rs1800896 and rs16944 in cervical carcinogenesis in the European population.
References
Walboomers JM, Jacobs MV, Manos MM, et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol. 1999;189:12.
Palefsky J. Human papillomavirus infection in HIV-infected persons. Top HIV Med. 2007;15:130–3.
Osiagwu DD, Azenabor AE, Osijirin AA, et al. Evaluation of interleukin 8 and interleukin 10 cytokines in liquid based cervical cytology samples. Pan Afr Med J. 2019;32:148.
Li B, Zhang L, Zhao J, et al. The value of cytokine levels in triage and risk prediction for women with persistent high-risk human papilloma virus infection of the cervix. Infect Agent Cancer. 2019;14:16.
Kabel AM. Relationship between cancer and cytokines. J Cancer Res Treat. 2014;2:41–3.
Xu Y, Zhu KJ, Zhu N, et al. Expression of Foxp3+CD4+CD25+ regulatory T cells and Th1/Th2, Tc1/Tc2 profiles in the peripheral blood of patients with condyloma acuminatum. Clin Exp Dermatol. 2009;34:229–35.
Su D‑L, Lu Z‑M, Shen M‑N, et al. Roles of pro- and anti-inflammatory cytokines in the pathogenesis of SLE. Biomed Res Int. 2012; https://doi.org/10.1155/2012/347141.
Munoz N, Bosch FX, de Sanjose S, et al. Epidemiologic classification of human papillomavirus types associated with cervical cancer. N Engl J Med. 2003;348:518–27.
Wang SS, Bratti MC, Rodriguez AC, et al. Common variants in immune and DNA repair genes and risk for human papillomavirus persistence and progression to cervical cancer. J Infect Dis. 2009;199:20–30.
Duan HX, Chen YY, Shi JZ, Ren NN, Li XJ. Association of IL‑6 -174G>C (rs1800795) polymorphism with cervical cancer susceptibility. Biosci Rep. 2018;38(5):BSR20181071.
Wang L, Zhao W, Hong J, et al. Association between IL1B gene and cervical cancer susceptibility in Chinese Uygur population: a case-control study. Mol Genet Genomic Med. 2019;7:e779.
Kwaśniak K, Czarnik-Kwaśniak J, Maziarz A, et al. Scientific reports concerning the impact of interleukin 4, interleukin 10 and transforming growth factor β on cancer cells. Cent Eur J Immunol. 2019;44:190–200.
Berti FCB, Pereira APL, Cebinelli GCM, et al. The role of interleukin 10 in human papilloma virus infection and progression to cervical carcinoma. Cytokine Growth Factor Rev. 2017;34:1–13.
Du GH, Wang JK, Richards JR, et al. Genetic polymorphisms in tumor necrosis factor alpha and interleukin-10 are associated with an increased risk of cervical cancer. Int Immunopharmacol. 2019;66:154–61.
Wang B, Wang H, Li P, et al. Relationships of interleukin-10 with the regulatory T cell ratio and prognosis of cervical cancer patients. Clinics (Sao Paulo). 2018;73:e679.
Guo C, Wen L, Song JK, et al. Significant association between interleukin-10 gene polymorphisms and cervical cancer risk: a meta-analysis. Oncotarget. 2018;9:12365–75.
Georgescu SR, Mitran CI, Mitran MI, et al. New insights in the pathogenesis of HPV infection and the associated carcinogenic processes: the role of chronic inflammation and oxidative stress. J Immunol Res. 2018; https://doi.org/10.1155/2018/5315816.
Kemp TJ, Hildesheim A, Garcia-Pineres A, et al. Elevated systemic levels of inflammatory cytokines in older women with persistent cervical human papillomavirus infection. Cancer Epidemiol Biomarkers Prev. 2010;1:1954–9.
Kamangar F, Cheng C, Abnet CC, et al. Interleukin-1B polymorphisms and gastric cancer risk—a meta-analysis. Cancer Epidemiol Biomarkers Prev. 2006;15:1920–8.
El Omar EM, Carrington M, Chow WH, et al. Interleukin‑1 polymorphisms associated with increased risk of gastric cancer. Nature. 2000;404:398–402.
Xu H, Ding Q, Jiang HW. Genetic polymorphism of interleukin-1A (IL-1A), IL-1B, and IL‑1 receptor antagonist (IL-1RN) and prostate cancer risk. Asian Pac J Cancer Prev. 2014;15:8741–7.
Al-tahhan MA, Etewa RL, et al. Association between circulating interleukin‑1 beta (IL-1β) levels and IL-1β C‑511T polymorphism with cervical cancer risk in Egyptian women. Mol Cell Biochem. 2011;353:159–65.
Shi YY, He L. SHEsis, a powerful software platform for analyses of linkage disequilibrium, haplotype construction, and genetic association at polymorphism loci. Cell Res. 2005;15:97–8.
Solé X, Guinó E, Valls J, et al. SNPStats: a web tool for the analysis of association studies. Bioinformatics. 2006;22:1928–9.
Cruz-Gregorio A, Manzo-Merino J, Lizano M. Cellular redox, cancer and human papillomavirus. Virus Res. 2018;246:35–45.
Zoodsma M, Nolte IM, Schipper M, et al. Interleukin-10 and Fas polymorphisms and susceptibility for (pre) neoplastic cervical disease. Int J Gynecol Cancer. 2005;15(3):282–90.
Eskdale J, Kube D, Tesch H, et al. Mapping of the human IL10 gene and further characterization of the 5’ flanking sequence. Immunogenetics. 1997;46:120–8.
Kingo K, Ratsep R, Koks S, et al. Influence of genetic polymorphisms on interleukin-10 mRNA expression and psoriasis susceptibility. J Dermatol Sci. 2005;37:111–3.
Zhou H, Liu A, Zhou B, et al. Interleukin-10 gene rs1800896 polymorphism increases risk of acute pancreatitis. Medicine. 2017;96:e9006.
Chen H, Tang J, Shen N, et al. Interleukin 10 gene rs1800896 polymorphism is associated with the risk of prostate cancer. Oncotarget. 2017;8(39):66204–14.
Cao LN, Cheng SL, Liu W. IL10 rs1800896 polymorphism is associated with liver cirrhosis and chronic hepatitis B. Genet Mol Res. 2016;22:15.
Singhal P, Kumar A, Bharadwaj S, et al. Association of IL-10 GTC haplotype with serum level and HPV infection in the development of cervical carcinoma. Tumour Biol. 2015;36:2287–98.
Bai CY, Shi XY, He J, et al. Association between IL-10 genetic variations and cervical cancer susceptibility in a Chinese population. Genet Mol Res. 2016;5:15.
Torres-Poveda K, Burguete-García AI, Cruz M, et al. The SNP at −592 of human IL-10 gene is associated with serum IL-10 levels and increased risk for human papillomavirus cervical lesion development. Infect Agent Cancer. 2012;7:32.
Zidi S, Gazouani E, Stayoussef M, et al. IL-10 gene promoter and intron polymorphisms as genetic biomarkers of cervical cancer susceptibility among Tunisians. Cytokine. 2015;76:343–7.
Xu J, Yin Z, Cao S, et al. Systematic review and meta-analysis on the association between IL-1B polymorphisms and cancer risk. PLoS One. 2013;8:e63654.
Kang S, Kim JW, Park NH, et al. Interleukin‑1 beta-511 polymorphism and risk of cervical cancer. J Korean Med Sci. 2007;22:110–3.
Qian N, Chen X, Han S, et al. Circulating IL-1beta levels, polymorphisms of IL-1B, and risk of cervical cancer in Chinese women. J Cancer Res Clin Oncol. 2010;136:709–16.
Funding
This work was supported by the Faculty of Medicine in Osijek grant No. 2018-VIF-12 (“IL-1B and IL-10 genetic polymorphism in cervical cancer,” project leader Jasenka Wagner).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
J. Wagner, S. Štibi, N. Selak, I. Alvir, I. Mamić, L. Marcelić, L. Šušnjar, M. Puljiz, M. Heffer, and D. Danolić declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wagner, J., Štibi, S., Selak, N. et al. Interleukin 10 rs1800896 and interleukin 1B rs16944 polymorphisms and the risk of cervical cancer. Wien Med Wochenschr 173, 57–61 (2023). https://doi.org/10.1007/s10354-021-00907-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10354-021-00907-w