Abstract
Prostate cancer (PCa) is the most commonly diagnosed cancer in the developed world, and the incidence of this cancer is rising rapidly in many countries. Several polymorphic genes encoding enzymes involved carcinogenesis have been studied as potential risk factor of prostate cancer. Genetic polymorphisms in glutathione S-transferases M1 (GSTM1), T1 (GSTT1) and P1 (GSTP1) genes have been constantly reported to have a meaningful effect on prostate cancer risk. But other surveys of this relationship have yielded inconsistent results. To assess the possible contribution of the GSTM1, GSTT1, and GSTP1 gene polymorphisms in prostate cancer, we performed a population-based study of 139 prostate cancer patients and 115 healthy controls based on their genotype distributions of the genes. There were no differences in distributions of genotype frequencies of GSTM1 and GSTP1 polymorphisms between prostate cancer patients and controls (OR 1.60, 95 % CI 0.886–2.860 for GSTM1 and OR 1.38, 95 % CI 0.739–2.577 for GSTP1). In contrast, the distribution of GSTT1-null genotype is significantly different between the prostate cancer case and controls (OR 0.26, 95 % CI 0.128–0.518, p < 0.001). Meanwhile, GSTP1 I/V and V/V genotypes were significantly associated with prostate cancer where the PSA level was more than 10.0 (OR 2.73, 95 % CI 1.319–5.639, p = 0.006). Thus, our data imply that the GSTT1-null genotype may not be a risk factor but a protective factor of prostate cancer and GSTP1 Val allele is a risk factor for the prostate cancer where the PSA level was high, although functional studies with larger sample size are necessary to elucidate these findings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Prostate cancer is one of the most commonly diagnosed cancer among men in developed countries, and responsible for 25 % of all new case of cancer (Kim et al. 2007; Kim et al. 2008; Sissung et al. 2014; Mitchell and Neal 2015). In the western industrialized country, the prostate cancer is the second leading cause of cancer mortality (Kim et al. 2008; Safarinejad et al. 2011). It has reported that about 241,740 men in the USA were diagnosed of prostate cancer in 2012. Incidence of prostate cancer in Korea is relatively low when compared to the USA but it has been recently increased that prostate cancer is the fifth leading cancer in Korean men, moreover the mortality of the prostate cancer has also been elevated (Jung et al. 2013; Cho et al. 2015). Multiple variables such as, ethnic origin, environmental, and genetic factor are possibly linked to incidence of prostate cancer (Kim et al. 2008). Especially, the genetic factor may responsible for about 42 % of prostate cancer, according to studies that estimate the difference in the concordant occurrence of prostate cancer between monozygotic and dizygotic twin (Lichtenstein et al. 2000; Mitchell and Neal 2015).
Glutathione S-transferase genes are a multigene family that are classified into at least six classes, including alpha (α), mu (μ), omega (ω), pi (π), theta (θ) and zeta (ζ), that are encoded by the GSTA, GSTM, GSTO, GSTP, GSTT and GSTZ genes, respectively (Townsend and Tew 2003; Karagas et al. 2005; Safarinejad et al. 2011; Bansal et al. 2014). Glutathione S-transferases are members of the phase II enzymes, which are mediating the conjugation of harmful compounds such as chemical carcinogens, pesticides, and antitumor agents, with glutathione, resulting in neutralization (McIlwain et al. 2006; Pan et al. 2014; Zhou et al. 2014). Therefore deficiency in GST enzyme activity may be a risk factor for developing cancer when exposed to certain carcinogens (Zhao et al. 2015). Among glutathione S-transferase genes, GSTM1 (OMIM: 138350), GSTP1 (OMIM: 134660) and GSTT1 (OMIM: 600436) are most widely analyzed for its genetic association with various cancers (Safarinejad et al. 2011; Bansal et al. 2014; Cai et al. 2013; Pan et al. 2014). The homozygous deletion (null genotype) of the GSTM1 and GSTT1 genes result in complete absence of enzyme activities and GSTP1 Ile105Val polymorphism shows decreased enzyme activity (Mao et al. 2004; Safarinejad et al. 2011). GSTM1 and GSTT1 are critical components for the DNA repair pathway, thus absence of these enzymes possibly contribute to the higher risk of prostate cancer (Cai et al. 2013). Meanwhile, the GSTP1 gene inactivation was frequently reported from many prostate tumor cases that the gene was silenced by hypermethylation in the promoter region (Lee et al. 1994; Cai et al. 2013). Despite these genetic associations between GSTM1, GSTP1 and GSTT1, and prostate cancer, other surveys of this relationship have yielded inconsistent results (Kim et al. 2002, 2005; Ntais et al. 2005; Mittal et al. 2009; Mo et al. 2009; Konwar et al. 2010a, b; Wei et al. 2012; Cai et al. 2013; Zhou et al. 2014). Therefore, these discrepancies raised the question of whether or not GSTM1, GSTP1, and GSTT1 polymorphisms are really the genetic risk factors for prostate cancer. The present study investigated an association between the GSTM1-null, GSTT1-null and GSTP1 Ile105Val polymorphisms and the occurrence of prostate cancer by the case–control designed study in 139 prostate cancer case and 115 corresponding controls.
Materials and methods
Subject
The DNA samples included subsets of the samples examined by Kim et al. (2008). We analyzed a total of 139 Korean prostate cancer patients with histologically confirmed prostate adenocarcinoma (PCa), who were recruited for the study from the urology department of the Eulji University School of Medicine in Seoul and Daejeon, Korea. Histological classification of PCa was determined according to the World Health Organization (WHO) recommendations and the Gleason score (Table 1). In addition, a total of 115 Korean men who had been diagnosed as free of prostate cancer by the Eulji University hospital in Seoul and Daejeon, Korea were recruited as normal controls. These subjects were selected at random (and therefore likely to be unrelated) from the same geographical area as the cases. DNAs were prepared from the prostate cancer specimens of patients and whole blood samples of controls according to standard methods (Sambrook et al. 1989). The separate written informed consent was obtained for screening and for enrollment from all participants.
Clinicopathological characteristics
Information on clinical stage, Gleason score and PSA (prostate specific antigen) level were collected from medical records. According to clinicopathological grade, the patients were categorized into two subgroups: the low-grade PCa (Gleason score <7) and the high-grade PCa (Gleason score ≥7) (Safarinejad et al. 2011; Chen et al. 2014). In the Asian population, the detection rate of PCa has been shown to be much lower in the diagnostic gray zone of PSA 4–10 ng/ml (Chen et al. 2014). PSA levels were categorized into two subgroups: the low-grade (PSA ≤10 ng/ml) and the high-grade (PSA >10 ng/ml) (Kesarwani et al. 2009).
Genotyping
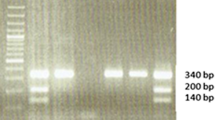
The GSTM1 and GSTT1 genotypes were determined by polymerase chain reaction. The primers used for PCR amplifications were 5′-CTGCCCTACTTGATTGATGG-3′ and 5′-CTGGATTGTAGCAGATCATG-3′ for GSTM1, 5′-TTCCTTACTGGTCCTCACATC-3′ and 5′-TCACCGGATCATGGCCAGCA-3′ for GSTT1. And amplification of the albumin (ALB) gene with primers 5′-GCCCTCTGCTAACAAGTCCT-3′ and 5′-GCCCTAAAAAGAAAATCGCC-3′ was used as an internal control.
Each PCR reaction was performed in a total volume of 20 μl containing 20 ng of genomic DNA, 10 pM each primer, 0.2 mM dNTPs, 2.0 mM MgCl2, 10× PCR buffer and 1.0 U NV DNA polymerase (NAVI BioTech, Korea). The PCR amplification was conducted Bio-rad PCR system under the conditions: 94 °C for 5 min, followed by 35 cycles of 94 °C for 1 min, 58 °C for 1 min and 72 °C for 1 min, then a final extension at 72 °C for 10 min. Each PCR products were analyzed by electrophoresis on 2 % agarose gel. The length of PCR products were 273 bp for individuals with one or more GSTM1 alleles, 480 bp for individuals with one or more GSTT1 alleles and 350 bp for ALB as internal control.
The GSTP1 genotype were determined by PCR–RFLP (restriction fragment length polymorphism) method. GSTP1 was amplified using these primers 5′-ACCCCAGGGCTCTATGGGAA-3′ and 5′-TGAGGGCACAAGAAGCCCCT-3′. Each PCR reaction was performed in a total volume of 20 μl containing 20 ng of genomic DNA, 10 pM each primer, 0.2 mM dNTPs, 2.0 mM MgCl2, 10× PCR buffer and 1.0 U NV DNA polymerase (NAVI BioTech, Korea). The PCR amplification under the conditions: 94 °C for 30 s, followed by 35 cycles of 94 °C for 90 s, 61 °C for 1 min, 72 °C for 30 s, then and a final extension at 72 °C for 10 min. After amplification, the PCR products were restricted by BsmA1. The fragments were separated by electrophoresis on 3 % agarose gel. Ile/Ile had single fragment of 176 bp, and Val/Val had two fragments of 85 and 91 bp, and Ile/Val had three fragment.
Data analyses
To test for association between all the samples for the prostate cases and the control groups, we used a frequencies, Chi squared tests implemented in SPSS 21 Statistics (IBM Korea, Korea). A test of proportion and odds ratio (OR) with 95 % confidence intervals (CI) in a 2 × 2 table were calculated using the statistical analysis on the internet (SISA, http://www.quantitativeskills.com/sisa/). ORs were adjusted for age by using the multivariate logistic regression models. The frequencies of combined genotype were estimated by counting.
A value of p < 0.05 was considered statistically significant. Bonferroni correction was used to adjust the α-level according to the number of independent comparisons.
Results
The mean ages of this study were 70.6 ± 8.3 and 59.4 ± 10.7 for the cases and the controls, respectively (Table 1). The level of PSA and Gleason score also presented Table 1. Eighty-three cases exceeded 10 ng/ml of PSA level and the Gleason score for 47 cases were more than 10.
Genotyping data of GSTM1, GSTP1, and GSTT1 for the 139 prostate cancer cases and 115 controls are summarized in Table 2. The frequencies of GSTM1-null genotype for our study were 56.8 % in the prostate cancer group and 47.8 % in the controls. The adjusted odds ratio was 1.60 (95 % confidence interval 0.886–2.860, p = 0.152) which is not significant. The frequencies of valine related genotypes (I/V + V/V) of GSTP1 were 33.9 % for the controls and 33.1 % for the case samples. The adjusted odds ratio was 1.38 (95 % CI 0.739–2.577, p = 1.000). Again, the value was not significant. However, the genotype distribution GSTT1-null was significantly different between the case group (57.5 %) and controls (79.1 %) (p < 0.001). The adjusted odds ratio and 95 % CI for the GSTT1-null genotype was 0.26 and 0.128–0.518, respectively. The result suggested that the GSTT1-null genotype is a protective factor for prostate cancer in our samples.
The effects from combined genotypes of GSTM1, GSTP1 and GSTT1 were analyzed (Table 3). Significant associations were observed among GSTM1-null + GSTT1-present (p = 0.006), GSTT1-null + GSTP1-I/I (p = 0.006), GSTT1-null + GSTP1-I/V or V/V (p = 0.006), GSTM1-null + GSTT1-present + GSTP1 I/I (p = 0.035) and GSTM1-null + GSTT1-present + GSTP1-I/V or V/V (p = 0.027). However, no values were significant after applying the Bonferroni corrected significant level of 0.0041 and 0.0062 for a combination analysis of two loci and three loci, respectively.
The significant association was observed between GSTP1-I/V + V/V genotype and clinicopathological characteristics of prostate cancer (Table 4). This genotype was more frequently observed in the prostate cancer patients whose PSA level was more than 10 ng/ml (Table 4). The odds ratio was 2.73 (95 % CI 1.319–5.639, p = 0.006).
Discussion
The age was reported to be a major risk factor for prostate cancer (Zhou et al. 2014). Therefore, we adjusted the age for the statistical analyses in this study. There were no differences in the null genotype distribution of GSTM1 and in the genotype distribution of GSTP1 Ile105Val polymorphism between the prostate case samples and controls in this survey (p > 0.05), suggesting that these two polymorphisms do not significantly associated with a higher risk of prostate cancer in Korea. Earlier findings suggest that the GSTM1-null genotype is a risk factor for the occurrence of prostate cancer (Srivastava et al. 2005; Minelli et al. 2011; Haholu et al. 2013; Cai et al. 2013; Zhou et al. 2014). Wei et al. (2012) also supported these reports that the effect of GSTM1-null genotype is a mild risk factor for prostate cancer. Meanwhile, Srivastava et al. (2005) reported that GSTP1-313 A/G polymorphism, that the polymorphism replaces isoleucine at codon 105 with valine, is a strong predisposing risk factor for prostate cancer in North India. In addition, the GSTP1 105Val was found to be a moderately significant risk factor for prostate cancer among men of African descent (Ntais et al. 2005; Lavender et al. 2009; Safarinejad et al. 2011).
However, others reported the lack of association between the GSTM1 and GSTP1 polymorphisms and prostate cancer (Ntais et al. 2005; Så et al. 2014). Ntais et al. (2005) reported from their meta-analysis that GSTM1-null and GSTP1 105Val genotypes were not a risk for prostate cancer. Så et al. (2014) also could not find any association between the GSTP1 105Val polymorphism and increased risk of prostate cancer in a Brazilian population cohort. These findings are consistent with the present results (Table 2).
In contrast, we found a significant association between GSTT1-null genotype and prostate cancer that the null genotype was deficit among prostate cases (OR 0.26, 95 % CI 0.128–0.518, p < 0.001). It has reported that the GSTT1-null genotype is a strong risk factor of prostate cancer (Ntais et al. 2005; Srivastava et al. 2005; Safarinejad et al. 2011). However, the GSTT1-null genotype was not a risk factor for prostate cancer in our study. The frequencies of GSTT1-null genotypes are 57.5 % for prostate cancer cases and 79.1 % for controls (Table 2). This result means that the effect of GSTT1-null genotypes in Korean population is indeed protective. A similar association in Korean population was reported that the GSTT1-null genotype is a protective factor of bladder cancer (Kim et al. 2002). The author also suggested that GSTT1-present genotype is rather risk factor for bladder cancer in Koreans (Kim et al. 2005). Bansal et al. (2014) also reported that the GSTT1-null genotype was detected in 51.04 % for controls in comparison to 20.2 % of breast cancer patient, hence protective. Therefore, comprehensive analyses with larger sample sets are required to clarify the effect of GSTT1-null genotype in the prostate cancer.
Nominal associations between genotypes and cancer risk were observed in the combined analyses of these three markers (Table 3). The combined genotype of GSTM1-null/GSTT1-present showed that the risk increased ~fourfolds (p = 0.006). This result may support the previous result that the GSTM1-null and GSTT1-present genotypes are risk factors for bladder cancer in Korean population (Kim et al. 2005). The combined genotype of GSTM1-null, GSTT1-present and GSTP1 I/V or V/V genotype increased the risk almost ninefolds (p = 0.027). In the previous report, GSTP1 I/V or V/V genotype is a possible risk factor for prostate cancer (Safarinejad et al. 2011). Therefore, GSTM1-null, GSTT1-present and GSTP1 I/V or V/V combined genotype can be a strong candidate risk factor for prostate cancer in Korea. However, none of them are survived after Bonferroni correction (p = 0.0041 for a combination of two loci and p = 0.0062 for a combination of three loci).
The genotype distributions of GSTM1, GSTP1, and GSTT1 were compared to clinicopathological characteristics (Table 4). There is a significant surplus of GSTP1 I/V + V/V genotypes in the prostate patients, whose PSA levels are exceeded 10 ng/ml (Table 4). Measuring PSA concentration in blood is a powerful tools to predict lifelong risk of prostate cancer in men (Vickers et al. 2013; Attard et al. 2015). But other studies reported lack of association between GST gene polymorphisms and prostate cancer status based on PSA level (Ashtiani et al. 2010; Qadri et al. 2011). Thus, additional survey of samples with various ethnicities and data of precisely estimate PSA level for each samples are the subjects for further analyses.
The present study has an inherent deficiency that the number of studied samples was relatively small. The sample numbers of this study were 139 prostate cancer cases and 115 controls. Despite the methodological limitation, this study has an advantage that both the prostate case group and controls in this study underwent strict clinical evaluation by urologists, therefore the purity of our samples is relatively high. Besides, this study conducted with 254 subjects and the calculated analysis power of our study was over 95 %. However, genetic association studies should be carefully interpreted, because the possibility of common errors contributed to statistical fluctuation, for example, GWAS approaches have a high rate of false negative because of the burden of multiple testing. Inversely, the candidate approaches that conducted in this study, typically showed a high rate of false positive and overestimation in genetic effects (Sissung et al. 2014). Therefore, further analyses with larger sample sizes and various genetic markers are required to exclude possible errors.
In conclusion, the statistically significant association was observed between GSTT1-null genotype and prostate cancer. Our results imply that the GSTT1-null genotype may be protective in Korean samples. In addition, we find a significant association between GSTP1 I/V + V/V genotype and PSA level in patients.
References
Ashtiani ZO, Hasheminasab SM, Ayati M, Goulian BS, Modarressi MH (2010) Are GSTM1, GSTT1 and CAG repeat length of androgen receptor gene polymorphisms associated with risk of prostate cancer in Iranian patients? Pathol Oncol Res 17:269–275
Attard G, Parker C, Eeles RA, Schröder F, Tomlins SA, Tannock I, Drake CG, de Bono JS (2015) Prostate cancer. Lancet. doi:10.1016/S0140-6736(14)61947-4 (in press)
Bansal VK, Rajan K, Sharma A, Paliwal P, Chaubal G, Jindal V, Misra M.C, Kucheria K (2014) Prospective case–control study to evaluate the role of glutathione s transferases (GSTT1 and GSTM1) gene deletion in breast carcinoma and its prognostic significance. Indian J Surg 1–6
Cai Q, Wang Z, Zhang W, Guo X, Shang Z, Jiang N, Tian J, Niu Y (2013) Association between glutathione S-transferases M1 and T1 gene polymorphisms and prostate cancer risk: a systematic review and meta-analysis. Tumour Biol 35:247–256
Chen R, Ren S, Chinese Prostate Cancer Consortium, Yiu MK, Fai NC, Cheng WS, LH Ian, Naito S, Matsuda T, Kehinde E et al (2014) Prostate cancer in Asia: a collaborative report. Asian J Urol 1:15–29
Cho IC, Kim JE, Kim SH, Joung JY, Seo HK, Chung JS, Park WS, Lee KH (2015) Oncologic aspects of long-term followed incidental prostate cancer detected by cystoprostatectomy in Korean patients. Prostate Int 3:56–61
Haholu A, Berber U, KaragözB Tuncel T, Bilgi O, Demirel D (2013) Is there any association of glutathione S-transferase T1 (GSTT1) and glutathione S-transferase M1 (GSTM1) gene polymorphism with gastric cancers? Pol J Pathol 64:247–252
Jung KW, Won YJ, Kong HJ, Oh CM, Seo HG, Lee JS (2013) Cancer statistics in Korea: incidence, mortality, survival and prevalence in 2010. Cancer Res Treat 45:1–14
Karagas MR, Park S, Warren A, Hamilton J, Nelson HH, Mott LA, Kelsey KT (2005) Gender, smoking, glutathione-S-transferase variants and bladder cancer incidence: a population-based study. Cancer Lett 219:63–69
Kesarwani P, Singh R, Mittal RD (2009) Association of GSTM3 intron 6 variant with cigarette smoking, tobacco chewing and alcohol as modifier factors for prostate cancer risk. Arch Toxicol 83:351–356
Kim HJ, Liu X, Wang H, Kohyama T, Kobayashi T, Wen FQ, Romberger DJ, Abe S, MacNee W, Rahman I et al (2002) Glutathione prevents inhibition of fibroblast-mediated collagen gel contraction by cigarette smoke. Am J Physiol Lung Cell Mol Physiol 283:L409–L417
Kim EJ, Jeong P, Quan C, Kim J, Bae SC, Yoon SJ, Kang JW, Lee SC, Jun Wee J, Kim WJ (2005) Genotypes of TNF-alpha, VEGF, hOGG1, GSTM1, and GSTT1: useful determinants for clinical outcome of bladder cancer. Urology 65:70–75
Kim W, Yoo TK, Kim SJ, Shin DJ, Tyler-Smith C, Jin HJ, Kwak KD, Kim ET, Bae YS (2007) Lack of association between Y-chromosomal haplogroups and prostate cancer in the Korean population. PLoS ONE 2:e172
Kim W, Yoo TK, Shin DJ, Rho HW, Jin HJ, Kim ET, Bae YS (2008) Mitochondrial DNA haplogroup analysis reveals no association between the common genetic lineages and prostate cancer in the Korean population. PLoS ONE 3:e2211
Konwar R, Manchanda PK, Chaudhary P, Nayak VL, Singh V, Bid HK (2010a) Glutathione S-transferase gene variants and risk of benign prostate hyperplasia in a North Indian population. Asian Pac J Cancer Prev 11:365–370
Konwar R, Manchanda PK, Chaudhary P, Nayak VL, Singh V, Bid HK (2010b) Glutathione S-transferase (GST) gene variants and risk of benign prostatic hyperplasia: a report in a North Indian population. Asian Pac J Cancer Prev 11:1067–1072
Lavender NA, Benford ML, VanCleave TT, Brock GN, Kittles RA, Moore JH, Hein DW, Kidd LC (2009) Examination of polymorphic glutathione S-transferase (GST) genes, tobacco smoking and prostate cancer risk among men of African descent: a case-control study. BMC Cancer 16:397
Lee WH, Morton RA, Epstein JI, Brooks JD, Campbell PA, Bova GS, Hsieh WS, Isaacs WB, Nelson WG (1994) Cytidine methylation of regulatory sequences near the pi-class glutathione S-transferase gene accompanies human prostatic carcinogenesis. Proc Natl Acad Sci USA 91:11733–11737
Lichtenstein P, Holm NV, Verkasalo PK, Iliadou A, Kaprio J, Koskenvuo M, Pukkala E, Skytthe A, Hemminki K (2000) Environmental and heritable factors in the causation of cancer-analyses of cohorts of twins from Sweden, Denmark, and Finland. N Engl J Med 343:78–85
Mao GE, Morris G, Lu QY, Cao W, Reuter VE, Cordon-Cardo C, Dalbagni G, Scher HI, deKernion JB, Zhang ZF (2004) Glutathione S-transferase P1 Ile105Val polymorphism, cigarette smoking and prostate cancer. Cancer Detect Prev 28:368–374
McIlwain CC, Townsend DM, Tew KD (2006) Glutathione S-transferase polymorphisms: cancer incidence and therapy. Oncogene 25:1639–1648
Minelli C, Wei I, Sagoo G, Jarvis D, Shaheen S, Burney P (2011) Interactive effects of antioxidant genes and air pollution on respiratory function and airway disease: a HuGE review. Am J Epidemiol 173:603–620
Mitchell T, Neal DE (2015) The genomic evolution of human prostate cancer. Br J Cancer 113:193–198
Mittal RD, Kesarwani P, Singh R, Ahirwar D, Mandhani A (2009) GSTM1, GSTM3 and GSTT1 gene variants and risk of benign prostate hyperplasia in North India. Dis Mark 26:85–91
Mo Z, Gao Y, Cao Y, Gao F, Jian L (2009) An updating meta-analysis of the GSTM1, GSTT1, and GSTP1 polymorphisms and prostate cancer: a HuGE review. Prostate 69:662–688
Ntais C, Polycarpou A, Ioannidis JP (2005) Association of GSTM1, GSTT1, and GSTP1 gene polymorphisms with the risk of prostate cancer: a meta-analysis. Cancer Epidemiol Biomark Prev 14:176–181
Pan C, Zhu G, Yan Z, Zhou Y, Liu Z (2014) Glutathione S-transferase T1 and M1 polymorphisms are associated with lung cancer risk in a gender-specific manner. Oncol Res Treat 37:164–169
Qadri Q, Sameer AS, Shah ZA, Hamid A, Alam S, Manzoor S, Siddiqi MA (2011) Genetic polymorphism of the glutathione-S-transferase P1 gene (GSTP1) and susceptibility to prostate cancer in the Kashmiri population. Genet Mol Res 10:3038–3045
Så RA, Moreira Ados S, Cabello PH, Ornellas AA, Costa EB, Matos Cda S, Alves G, Hatagima A (2014) Human glutathione S-transferase polymorphisms associated with prostate cancer in the Brazilian population. Int Braz J Urol 40:463–473
Safarinejad MR, Shafiei N, Safarinejad SH (2011) Glutathione S-transferase gene polymorphisms (GSTM1, GSTT1, GSTP1) and prostate cancer: a case-control study in Tehran. Iran. Prostate Cancer Prostatic Dis 14:105–113
Sambrook J, Fritsch EF, Maniatis T (1989) Molecular cloning: a laboratory manual, 2nd edn. Cold Spring Harbor Laboratory Press, New York
Sissung TM, Price DK, Del Re M, Ley AM, Giovannetti E, Figg WD, Danesi R (2014) Genetic variation: effect on prostate cancer. Biochim Biophys Acta 1846:446–456
Srivastava DS, Mandhani A, Mittal B, Mittal RD (2005) Genetic polymorphism of glutathione S-transferase genes (GSTM1, GSTT1 and GSTP1) and susceptibility to prostate cancer in Northern India. BJU Int 95:170–173
Townsend D, Tew K (2003) Cancer drugs, genetic variation and the glutathione-S-transferase gene family. Am J Pharmacogn 3:157–172
Vickers AJ, Sjoberg DD, Ankerst DP, Tangen CM, Goodman PJ, Thompson IM Jr (2013) The prostate cancer prevention trial risk calculator and the relationship between prostate-specific antigen and biopsy outcome. Cancer 119:3007–3011
Wei B, Xu Z, Zhou Y, Ruan J, Cheng H, Xi B, Zhu M, Jin K, Zhou D, Hu Q et al (2012) Association of GSTM1 null allele with prostate cancer risk: evidence from 36 case-control studies. PLoS ONE 7:e46982
Zhao Y, Wang B, Hu K, Wang J, Lu SU, Zhang Y, Lu W, Zhao E, Yuan L (2015) Glutathione S-transferase θ1 polymorphism contributes to lung cancer susceptibility: a meta-analysis of 26 case-control studies. Oncol Lett 9:1947–1953
Zhou TB, Drummen GP, Jiang ZP, Qin YH (2014) GSTT1 polymorphism and the risk of developing prostate cancer. Am J Epidemiol 180:1–10
Acknowledgments
The present research was conducted by the research fund of Dankook University in 2013.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Bioethical statements
This study was approved by the Ethics Committee and institutional review boards of Eulji Medical Center of the Eulji University School of Medicine in Seoul, Korea.
Conflict of interest
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Shin, YE., Hwang, IW. & Jin, HJ. Association between glutathione S-transferases M1, T1 and P1 gene polymorphisms and prostate cancer in Koreans. Genes Genom 38, 235–241 (2016). https://doi.org/10.1007/s13258-015-0382-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13258-015-0382-2