Abstract
The continuous and noninvasive blood pressure (BP) measurement based on pulse transit time (PTT) doesn’t need cuff and could monitor BP in real time for a long period. However, PTT is just a time index derived from electrocardiogram (ECG) and photoplethysmogram (PPG), while BP-related information within the PPG waveform has seldom been taken into consideration. We hypothesized that PPG waveform feature might be useful for BP estimation. Nine healthy subjects took part in an exercise stress test, including baseline resting, exercise on bicycle ergometry and recovering resting. ECG of lead V5 and PPG from left finger were collected simultaneously, and systolic blood pressure (SBP) and diastolic blood pressure (DBP) were recorded from a cuff sphygmometer on the right wrist. The correlation coefficients were obtained between BP (SBP, DBP and pulse pressure (PP)) and PPG morphological indices (total 15 indices in terms of waveform amplitude, time span and area ratio). Five PPG indices were correlated with both SBP and PP (absolute value of correlation coefficient |r| > 0.6) and were further tested for the capability to BP estimation, which were: (1) PTTA, time delay between the R peak of ECG and the foot point of PPG; (2) RSD, time ratio of systole to diastole; (3) RtArea, area ratio of systole to diastole; (4) TmBB, time span of PPG cycle; (5) TmCA, diastolic duration. Comparisons were made between the measured BP and the estimated BP by regression lines and quadratic curve fitting, respectively. As a result, the mean errors of SBP liner fitting with RSD, RtArea, TmBB and TmCA respectively were 5.5, 5.4, 5.2, 5.1 mmHg, which were smaller than that with PTTA of 5.8 mmHg. And the mean errors of SBP quadratic curve fitting with RSD, RtArea, TmBB and TmCA were all 5.1 mmHg, which were smaller than that with PTTA of 5.7 mmHg. The mean errors of multiple regression for SBP, PP and DBP was 4.7, 4.7, 3.5 mmHg respectively, which were more accurate than the regression with single PTTA of 5.8, 5.3, 5.2 mmHg respectively. However, PPG-based SBP and DBP could under estimate cuff pressure by 8 mmHg and over estimate by 10 mmHg respectively, which is a clinically significant error. In conclusion, the combination of time span (PTT, time ratio of systole to diastole, time span of PPG cycle and diastolic duration) and waveform morphology (area ratio of systole to diastole) could improve the performance of PPG-based BP estimation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Blood Pressure (BP) including systolic blood pressure (SBP) and diastolic blood pressure (DBP) is an important and vital sign of health care. SBP is the peak pressure in the arteries when the blood flows from the ventricles to the arteries during ventricular systole, and DBP is the minimum pressure in the arteries during ventricular diastole when the ventricles are full of blood. The metrical unit of blood pressure is called millimeters of mercury (mmHg). BP can be measured both invasively and non-invasively, using or not using cuff, non-continuously and continuously. Instantaneous BP cannot show real-time physiological status momently, while the continuous BP can provide superior data for predicting risk of serious cardiovascular events and making antihypertensive therapy decisions [1]. Most invasive researches on cardiovascular circulation system have been involved with clinical patients or animals [2]. And the continuous, cuffless and non-invasive blood pressure estimation based on the pulse transit time (PTT) has gained increasing attention in recent years [3]. PTT is usually measured based on the continual and simultaneous monitoring of electrocardiogram (ECG) and photoplethysmogram (PPG) [3], which is a function of pulse wave velocity (PWV) and therefore a function of blood pressure [4]. Because of that, PTT is the one of the most popular parameter nowadays that is utilized for noninvasive, long-term, continuous and cuffless BP monitoring [5]. Newlin [6] reported that PTT was moderately correlated (0.5 < |r| < 0.6) with SBP elicited by the heterogeneity regression in pooling data from all subjects [6], whereas Lane et al. [7] found that the correlation increased (|r| > 0.7) if it was considered individually [7]. PTT-based least-squares regression was used by Wong et al. [8] to estimate BP in the first test and a repeatability test carried out half year later on 14 subjects, and the standard deviation (SD) of estimation differences increased from 5.3 to 10.2 mmHg for SBP, and from 2.9 to 7.3 mmHg for DBP when the regression coefficients in the first test were used for prediction. Therefore, the regression coefficients for PTT-based BP estimations need calibration for long term using. Foo et al. [9] had made series and systematic studies about the function of PTT, and proved its potentials to monitor timing changes in peripheral pulse in cardiovascular and respiratory studies. PTT is significantly related to peripheries’ path length, heart rate (HR), SBP (P < 0.05) in children, except for DBP and mean arterial pressure (MAP) [9].
However, PTT reveals only a facet of the complex cardiovascular changes that induced by BP fluctuation [10], which is influenced by many physiologic variables like HR, BP, arterial compliance and breathing efforts. Most cardiovascular parameters (e.g., HR, BP, artery resistance) are linked with one to another, and may be correlated with the feature in PPG, which reveals the changes of blood volume during a cardiac cycle [11]. PPG has been used for heart rate calculation, blood pressure evaluation, arterial compliance monitoring and oxygen saturation determination [11]. Besides PTT, more BP-related information may be contained within the PPG waveform, which has seldom been investigated intensively. The waveform of PPG is similar in appearance to that of arterial blood pressure [4], while the former is noninvasive whereas the latter usually requires invasive measurement.
This paper focused on finding out some BP-related PPG waveform indices except for PTT, which might be appropriate for robust BP estimation. Compared with the predominance of parasympathetic tone during relaxation period, sympathetic tone predominated during exercise period and usually increased SBP. During the recovery period after exercise, vagal reactivation resulted in the decline of SBP. SBP might increase gradually during stable exercise, and decline gradually during recovery rest. In this paper, a schedule involved baseline rest, exercise stress and recovery rest was used to make the BP changing in a wide range and thus make the BP estimation available in a broad value range.
Methods
Data recording
Nine healthy subjects (all male, age 28.36 ± 5.21 years, body mass index 20.49 ± 4.09 kg/m2, with accumulated exercise time for at least one hour per week) participated in the investigations, and no subject participated in any form of drastic activity before the experiment. All subjects gave their consent to the experiment. An exercise test with three sections of baseline resting, exercise on bicycle ergometry and recovering resting was consisted as follows: (1) baseline period: relaxation for 5 min before exercise; (2) workload period: exercise on bicycle ergometry for 20 min; (3) recovery period: relaxation for 5 min immediately after exercise. During workload period, workload of 100 W was imposed on each subject by the bicycle ergometry with speed maintaining at 20 km/hr.
According to the manual of a cuff-wrist sphygmometer HEM-6000 (OMRON, Japan), the cuff can be applied to either left or right wrist, and it should be aligned with the same level of heart during BP measurement. SBP and DBP were recorded from HEM-6000 on the right wrist during the whole experiment. And BP measurement was carried out every minute by manually reading a watch. The wait time allows the arteries to return to the condition prior to taking the blood pressure measurement. One channel ECG and One channel PPG was continuously recorded by the noninvasive cardiac function monitor (NCFM) all through the experiment for each subject. NCFM was made by Zhejiang University of China, with 12 bits A/D converter at the sampling frequency of 250 points per second for both PPG and ECG. The channel of ECG was placed near the V5 precordial position with Ag/AgCl electrodes in order to yield large and clear R wave for heartbeat segmentation. The PPG was measured at the middle finger tip in left hand by 940 nm wavelength, surface mounted type infrared LED and photo-diode. The left hand should keep still during PPG monitoring in order to suppress interference, because PPG signal is very sensitive to artifacts, while motion artifact is a common occurrence that contaminates PPG [12].
Data preprocessing
A low-pass filter with a corner frequency of 50 Hz was used to remove high-frequency interference for both ECG and PPG. Then baseline wandering from ECG was removed by barycenter of QRS triangle combined with wavelet transform [13], which got better results in baseline wandering correction than filtering and function fitting methods. The DC component of PPG was removed and then the baseline of PPG was put to zeros level by subtracting quadratic polynomial that based on the points at PPG start points in each heartbeat cycle. After that, R wave peak in ECG and peak points in PPG were automatically detected by the heartbeat segmentation with the combination of ECG and PPG [14].
Characters extraction
Correlation between BP and 15 parameters of ECG and PPG were analyzed in this paper, including one ECG cycle, ten PPG measurements (five amplitude indices, four time span indices and one wave area ratio), and four PTT parameters based on the combination of ECG and PPG, as shown in Table 1 and Fig. 1.
Figure 1 illustrates the definitions of time span and amplitude indices. Letters ‘A’, ‘B’, and ‘C’ in Table 1 and Fig. 1 represent the foot, the peak and the dicrotic notch in PPG, respectively. Point P in PPG corresponds to the point whose amplitude relative to peak A is about 25 % of the amplitude between A peak and B peak, while point Q is the maximal slope point during the systolic rise phase. PTTA and PTTB are the time intervals measured from the R-wave peak of ECG to the foot and the peak of PPG respectively [5], while PTTP and PTTQ are determined by calculating the time difference between the R wave peak in ECG and the characteristic point P and point Q respectively in PPG [15]. In addition, the area ratio RtArea is shown in Fig. 2.
Waveform amplitude was achieved by calculating the difference of the amplitude between two points, e.g., amplitude AmAB between A peak and B peak in PPG is obtained by formula (1), i.e., AmAB represents the distance between apex A and apex B in vertical coordinate.
where Ay and By are the y-coordinates of point ‘A’ and point ‘B’ respectively, whose unit is millivolt. As a result, unit of AmAB is also millivolt.
Waveform time span was obtained by calculating the difference of the time between two points, e.g., time span TmAC between A peak and C peak in PPG is obtained by formula (2), i.e., TmAC represents the horizontal distance between apex A and apex C.
where Ax and Cx are the x-coordinates of point ‘A’ and point ‘C’ respectively, whose unit is sampling points; Fs is the PPG sampling frequency whose unit is sampling points per second. As a result, unit of TmAC is second.
Amplitude ratio RtAC_AB and RtAC_BC are derived by formula (3) and (4) respectively, and the time ratio of systole to diastole (RSD) is obtained by formula (5). Area ratio of diastole segment (Algebraic sum of segment CA as ‘Area 2’ in Fig. 2) to systole segment (‘Area 1’ in Fig. 2) is determined by formula (6).
where ‘ppg’ stands for PPG, Ak and Ck belong to the current heartbeat, and Ak+1 locates at the next heartbeat.
As the BP measurement was done every minute, the means of each index in Table 1 were calculated every minute. As a result, 30 values were obtained for all BP and PPG indices during the whole test including baseline rest, exercise stress and recovery rest. Then correlation coefficients [16] during the whole test between BP and the indices from Table 1 respectively were determined by formula (7) when X represent one character series in Table 1 and Y another one from SBP, DBP and pulse pressure (PP). PP is the difference between SBP and DBP, as shown by formula (8).
where ‘C’ is covariance, and ‘D’ denotes variance.
One variable linear regression model takes the form as formula (9) according to the least-squares procedure, while multiple variables linear regression model has an expression as formula (10). Variable x or vector {x i } represent the indices from Table 1, while variable y represents SBP or PP. Then estimated SBP and PP were obtained by formula (9) or (10), and DBP was calculated by formula (11) that derived from formula (8).
where ‘a’ is the slope coefficient and ‘b’ is the intercept value of the regression line derived from the independent variable x and the dependent variable y.
where vector {a i } are the regress coefficients and ‘b’ is the intercept value of the regression line derived from the independent vector {x i } and the dependent variable y.
Results
Correlation coefficients between BP and PPG characters
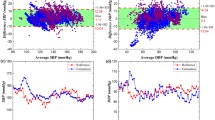
The mean value and SD of correlation coefficients between BP and each index from Table 1 for all 9 subjects was obtained and shown in Table 2. And the correlation coefficients between PPG amplitude indices and blood pressure for each subject are shown in Table 3. No index was related with DBP when selecting a |r| > 0.6 means that correlated relationship do exist, as shown in Table 2. Five indices of PTTA, RSD, RtArea, TmBB (almost the same as TmRR) and TmCA, having correlation |r| > 0.6 with both SBP and PP, were further tested for their capability to BP estimation. Fluctuation of BP and five PPG indices of one subject are shown as Fig. 3, in which the data of the first 5 min was gotten during the baseline rest period, the middle 20 min data was obtained during exercise period and the final 5 min data was acquired during the recovery rest period. Compared with rest state, RSD increased while not only PTT but also diastolic duration TmCA and heartbeat cycle TmBB decreased during exercise.
One variable linear regression for BP estimation
Table 4 shows the means of the difference between the measured BP and the predicted BP from the regression lines and quadratic curve fitting in individuals. The means of SBP estimation error by linear regression were bigger than that of PP estimation error, whereas estimated DBP had the smallest error. Quadratic curve fitting performed better than the linear fitting for individual subject, as shown in Table 4, which suggested that the non-linear relationship was stronger than a global linear correlation. The results implicated that RSD, RtArea, TmBB and TmCA were potential parameters for BP estimation.
ErSBP, ErPP and ErDBP are the algebraic deviation between the measured BP and the predicted BP, respectively. Correlation coefficient between ErSBP and ErPP in Table 5 is higher than that between ErSBP and ErDBP, or that between ErPP and ErDBP. As shown in Fig. 4 of one subject, the algebraic deviation of ErSBP and ErDBP has very similar trend, which contributes to the smaller ErDBP with formula (11) by correlation cancelling effect. Therefore, the means of the estimation error of DBP in Table 4 is smaller than that of SBP and PP (5.11 vs. 5.41 and 5.27 mmHg) by individual linear fitting and quadratic curve fitting (3.92 vs. 5.22 and 4.15 mmHg).
Figure 5 shows the scatter plots from 3 subjects of SBP and PP against PTTA, RSD, RtArea, TmBB and TmCA respectively. In Fig. 5, SBP is inversely correlated with PTTA, RtArea, TmBB and TmCA respectively, but positive correlated with RSD, which is consistent with Table 2. However, the orientations of regression lines were different from one subject to another. Therefore, without calibration process for individual subject, PPG-based BP estimation may not be accurate enough.
The slope coefficient ‘a’ and the intercept value ‘b’ in formula (9) derived from all data is shown in Table 6. The negative linear trend is found both in SBP and PP against PTTA, RtArea, TmBB and TmCA respectively, which reveals that both SBP and PP are negatively correlated with PTTA, RtArea, TmBB and TmCA. As shown in Table 6, when the linear regression is derived by all data, the error between the measured BP and the estimated SBP, PP and DBP are about 14 mmHg, 8 mmHg and 10 mmHg respectively, which is not acceptable in clinical diagnosis.
Multiple variables linear regression for BP estimation
Multiple variables linear regression was tested individually and collectively with (1) single index PTTA; (2) combination of PTTA and RSD; (3) combination of PTTA, RSD and RtArea; (4) combination of PTTA, RSD, RtArea and TmBB; (5) combination of PTTA, RSD, RtArea, TmBB and TmCA, respectively. Results in Table 7 indicated that individually multiple variables regression performed much better than collectively multiple variables regression. Smaller estimation error will be for SBP, PP and DBP when more parameters are involved in the multiple variables regression.
Comparison between upper arm and wrist sphygmomanometers
The cuff BP instruments contain wrist and upper arm sphygmomanometers. A comparison between the upper arm sphygmomanometer (HEM-907, OMRON) and the wrist sphygmomanometer (HEM-6000, OMRON) was made, and both sphygmomanometers record SBP, DBP and HR. All subjects were in a relaxed, seated position to rest for 5 min before taking the BP measurement. And then BP was recorded with HEM-907 on the left upper arm and simultaneously with HEM-6000 on the right wrist every minute by manually reading a watch. Subjects should remain still and do not talk during the BP measurements. Totally four groups of BP values were recorded for every subject.
The comparison results are shown in Table 8, and the difference between the two sphygmomanometers for SBP, DBP and HR is defined as △SBP, △DBP and △HR, respectively. There was high consistent between the wrist sphygmomanometer HEM-6000 and the upper arm sphygmomanometer HEM-907, and the mean difference between them was less than 3 mmHg for both SBP (−2.7 mmHg) and DBP (2.7 mmHg). The difference (analysis of covariance, P < 0.001 as △SBP and △DBP compared with zeros vector respectively) could be considered as system error between HEM-907 and HEM-6000.
Discussion
Blood pressure is a vital parameter to examine physical stress and to indicate cardiovascular diseases, and its measuring approaches can be classified into invasive and non-invasive methods [17]. The invasive measurement is a gold standard which reveals accurate beat-to-beat blood pressure. However, it might cause severe pain, bleeding even infection, which needs close supervision and is very difficult to operate. The non-invasive method is more desirable to develop, including non-continuous and continuous BP measurement. The non-continuous ways contain auscultatory and oscillometric methods, and nowadays they are the reliable BP measurements in hospitals. However, they are both cuff-based methods that placed a cuff around the arm or wrist to stop the blood flow in the artery and thus are occlusive, which could only provide intermittent BP readings.
Noninvasive and cuffless measurement of arterial blood pressure could get continuous or beat-by-beat BP readings. These methods are arterial tonometry, volume clamp method, and PTT-based method. However, both arterial tonometer and volume clamp methods suffer from high cost and poor accuracy caused by wrist movement. And both of them partly occlude blood flow. The PTT-based method has several advantages over arterial tonometry and volume clamp methods. It requires only the ECG and the PPG and there is no danger of cessation of blood perfusion, and can be used for a long time of BP monitoring. In recent years, PTT-based method is the most popular method for the continuous and cuffless measurement of blood pressure. PTT is usually determined by calculating the time span between R peak in ECG and a feature point in PPG (the peak point, the foot point, or the maximal slope point during the systolic rise phase). PTT is usually strongly correlated with the psychological and physical stress. PTT and systolic arterial pressure are inversely related [18], and there is no significant difference for the continuously BP measurements between volume clamp method and PTT-based method [19]. Increased BP leads to an increase in stiffness of arterial wall [15], which makes the pulse wave propagate faster and thereby leads to shorter PTT duration [15]. Conversely when BP falls, there is a lesser stiffness in the arterial walls, which causes the pulse wave to propagate slower and hence in turn lengthening PTT [15].
It was noticed that the mean error in Table 6 was much bigger than that in Table 4, supporting the concept that cardiovascular-related factors (such as blood viscosity, reflection coefficient, arterial radius, stiffness and etc.) are different from subject to subject, because weight, length of arm, height, circumference of arm, body mass index, body fat, age, and gender are all associated with BP [20]. Therefore, the correlations between BP and PTT should be analyzed individually but not collectively [5]. Wong et al. [5] showed that the mean of individual correlation of SBP ~ PTTB was −0.77, SBP ~ PTTA as −0.92, and the difference between the measured SBP and the predicted SBP from regression lines of SBP ~ PTTB and SBP ~ PTTA were 6.6 and 4.3 mmHg respectively on 12 healthy subjects, which indicated that PTTA was more proper than PTTB for SBP estimation. Furthermore, we found that PTTA was more proper than PTTB, PTTP and PTTQ for both SBP and PP estimation, and the error of PTTA-based SBP estimation was about 5.8 mmHg on 9 healthy subjects, as shown in Table 4. Moreover, PTTA has more clearly conception, as R peak in ECG is the moment about the beginning of ventricular mechanical contraction at heart, while the A peak in PPG is the moment that the pulse wave transmits to artery. As a result, PTTA is the time delay between the contraction phase beginning at heart and that at artery.
In this paper, the BP regression lines were estimated by all the data including baseline rest, exercise stress and recovery rest, but not by the data during different periods. The whole process of rest, exercise and recovery made the BP changing in a wide range, which led to the regression lines for blood pressure estimation adapting to a wide BP range. Compared with the predominance of parasympathetic tone during relaxation period, sympathetic tone predominated during exercise period, which increased the cardiovascular workload and resulted in declined PPG time span indices and elevated blood pressure. During the recovery period after exercise, vagal reactivation resulted in increased parasympathetic tone and declined in both heart rate and blood pressure, which induced most PPG time span indices increased when comparing with exercise period. The mechanism above might form the foundation of PPG-based BP estimation, and the stress-correlated characters may have similar fluctuating trend during the exercise test, as shown in Fig. 3.
This paper focused on finding out some BP-related PPG waveform indices except for PTT, and it revealed that time ratio of systole to diastole, time span of PPG cycle, diastolic time duration and area ratio of systole to diastole are at least as better as PTT for BP estimation, and the combination of time span and PPG waveform morphology could improve the performance of PPG-based BP estimation. PPG is useful for noninvasively detecting cardiovascular system stress to exercise, because not only PPG rhythm but also PPG waveform parameters had the discrimination ability to distinguish exercise state from relaxation state [21]. The dicrotic notch in PPG downward segment during resting period is very pronounced and identifiable, while it is less obvious or even disappears during exercise [10] and therefore might contribute to the smaller RtArea during exercise than that during resting period. Moreover, BP restored their baseline values at the end of recovery period in Fig. 3. As a result, elevated SBP and PP usually come along with increased RSD and decreased PTT, RtArea, TmCA and TmBB.
Increased sympathetic tone usually increases in arterial blood pressure but is unsure with PPG amplitude, as the relationship between arterial blood pressure and PPG amplitude is so complicated that large PPG amplitude may go with high or low arterial blood pressure [4]. In this paper, PPG amplitude of most subjects was not correlated with SBP or PP, as shown in Table 3, which supported the conception that there is not linear correlation relationship between PPG amplitude and SBP (or PP). Correlation coefficients between SBP (or PP) and PPG amplitude parameters varied a lot from subject to subject. For subject No. 3, strong correlation was observed between SBP (or PP) and AmAB (or AmBC), as the absolute values of correlation coefficients exceeded 0.7. Subject No. 1 had absolute values of correlation coefficients up to about 0.9 between SBP (or PP) and RtAC_AB (or RtAC_BC). However, only poor correlation was observed between SBP (or PP) and PPG amplitude parameters in most subjects. Furthermore, the PPG amplitude strongly depends on the force and orientation that the sensor attaching on finger, which might made the PTT more appropriate than PPG amplitude for BP estimation.
One limitation was that only 9 subjects have been studied in this paper. More subjects, including both men and women of different races and of a wider age range will be more appropriate to prove the conclusion of this paper. Another limitation was that BP-related indices from PPG were selected by linear correlation coefficients between BP and PPG feature. However, it was more possible that the correlation between BP and PPG feature might be non-linear, and non-linear ways of feature selection might get different feature indices for BP estimation. In addition, the PPG waveform acquired from different positions of the body are quite different in appearance. It is possible that the BP-sensitive indices of PPG on the ear might not entirely be the same as that of PPG on the finger tip. All these limitations above need more investigations and further studies.
According to Table 8, wrist sphygmomanometer (HEM-6000, OMRON) might under read SBP by 3 mmHg and over read DBP by 3 mmHg. Moreover, the accuracy of HEM-6000 is ±3 mmHg. Therefore SBP might be under read by 0 to 6 mmHg and DBP might be over read by 0 to 6 mmHg with wrist sphygmomanometer from upper arm cuff BP. Furthermore, our PPG-based methods at best will add another error of 5 mmHg. Therefore, SBP could have a range of 2 mmHg over reading and 8 mmHg under reading from Cuff BP, and DBP could have a range of 10 mmHg over reading and 11 mmHg under reading from Cuff BP. The 8 and 11 mmHg errors are clinically significant, and the accuracy of our methods is not enough for clinical application.
In this paper, indices of RSD, RtArea, TmBB and TmCA were better than PTTA for SBP, DBP and PP estimation respectively by both linear fitting and quadratic curve fitting for individual subject, as shown in Table 4. Moreover, BP estimation based on the multiple regression from PTTA, RSD, RtArea, TmBB and TmCA was more accurate than the linear estimation with single PTTA, with mean error of SBP, PP and DBP less than 5, 5 and 4 mmHg respectively, as shown in Table 7. Consequently, the morphology of PPG waveform may give comprehensive information about the cardiovascular system.
In conclusion, not only time span indices of PTT, time ratio of systole to diastole, time span of PPG cycle and diastolic time duration, but also PPG waveform area ratio of systole to diastole have the potential to estimate blood pressure, and the combination of time span and PPG waveform morphology could improve the performance of PPG-based BP estimation.
References
Peloff D, Sokolow M, Cowa R (1983) The prognostic value of ambulatory blood pressure. J Am Med Assoc 249(20):2792–2798
Ding H, Chen Z, Shen L et al (2009) Heart pump system in “heart—mural coronary artery—myocardial bridge” simulative device. Australas Phys Eng Sci Med 32(2):105–111
Yang X, Hu W, Yan H et al (2011) Research progress of noninvasive continuous blood pressure measurements based on pulse wave velocity. Space Med Med Eng 24(6):467–472
Reisne A, Shaltis PA, Combie DM et al (2008) Utility of the photoplethysmogram in circulatory monitoring. Anesthesiology 108(5):950–958
Wong MYM, Zhang YT (2006) The Relationship between Pulse Transit Time and Systolic Blood Pressure on Individual Subjects after Exercises. In: Proceedings of the 1st Distributed Diagnosis and Home Healthcare Conference Arlington, Virginia: 37–38
Newlin DB (1981) Relationships of pulse transmission times to pre-ejection period and blood pressure. Phychophysiology 18:316–321
Lane JD, Greenstadt L, Shapiro D (1983) Pulse transit time and blood pressure: an intensive analysis. Phychophysiology 20:45–49
Wong MY, Poon CC, Zhang YT (2009) An evaluation of the cuffless blood pressure estimation based on pulse transit time technique: a half year study on normotensive subjects. Cardiovasc Eng 9(1):32–38
Foo JYA, Wilson SJ, Williams G et al (2004) Pulse transit time to monitor changes in peripheral pulse timing characteristics of children. Australas Phys Eng Sci Med 27(4):338–339
Barreto A, Li C, Zhai J (2004) Computer evaluation of exercise based on blood volume pulse (BVP) waveform changes. WSEAS Trans Biol Biomed 1(1):120–125
Shelley KH (2007) Photoplethysmography: beyond the calculation of arterial oxygen saturation and heart rate. Anesth Analg 105(6):S31–S36
Foo JYA, Wilson SJ, Williams GR et al (2004) Motion artefact reduction of the photoplethysmographic signal in pulse transit time measurement. Australas Phys Eng Sci Med 27(4):165–173
Song JZ, Yan H, Li YJ et al (2010) Research on electrocardiogram baseline wandering correction based on wavelet transform, QRS barycenter fitting, and regional method. Australas Phys Eng Sci Med 33:279–283
Yu CG, Liu ZQ, Mckenna T et al (2006) A method for automatic identification of reliable heart rates calculated from ECG and PPG waveforms. J Am Med Inform Assoc 13(3):309–320
Foo JYA (2007) Pulse transit time in paediatric respiratory sleep studies. Med Eng Phys 29:17–25
Song JZ, Yan H, Xu Z et al (2011) Myocardial ischemia analysis based on electrocardiogram QRS complex. Australas Phys Eng Sci Med 34(4):515–521
Nitzan M (2011) Automatic noninvasive measurement of arterial blood pressure. IEEE Instrum Meas Mag 14(1):32–37
Porta A, Gasperi C, Nollo G et al (2005) SEQUENCE analysis of pulse transit time and systolic blood pressure during dynamic exercise. Comput Cardiol 32:849–852
Teng XF, Zhang YT (2006) An Evaluation of a PTT-Based Method for Noninvasive and Cuffless Estimation of Arterial Blood Pressure. In: Proceedings of the 28th IEEE EMBS Annual International Conference New York City:6049–6052
Langenberg C, Hardy R (2003) Influence of height, leg and truck length on pulse pressure, systolic and diastolic blood pressure. J Hypertens 21(3):537–543
Li Y, Yan H, Xu Z et al (2013) Analysis of the changes in Photoplethysmogram induced by exercise stress. J Med Imaging and Health Inf 3(3):347–355
Acknowledgments
This work was supported by Advanced Space Medico-Engineering Research Project of China(SJ201006),and supported by State Key Laboratory of Space Medicine Fundamentals and Application, China Astronaut Research and Training Center (SMFA12B09, SMFA13B03).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Li, Y., Wang, Z., Zhang, L. et al. Characters available in photoplethysmogram for blood pressure estimation: beyond the pulse transit time. Australas Phys Eng Sci Med 37, 367–376 (2014). https://doi.org/10.1007/s13246-014-0269-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13246-014-0269-6