Abstract
The aim of this paper is to study the outcome of single-layer end to side dunking pancreatojejunostomy technique in 32 patients of malignant pancreatic disease undergoing Whipple’s surgery in a tertiary care oncology centre in India. From January 2013 to January 2016, 32 consecutive patients who underwent pancreatoduodenectomy for malignant diseases were analysed retrospectively. All the patients underwent standard Whipple’s operation. Pancreatojejunostomy was established in a single-layer end to side dunking manner with PDS 4-0. Various patient data, i.e. preoperative symptoms and demography, intra-operative time, blood loss and need of blood transfusion, postoperative hospital stay and complications, were noted. Mean operative time was 3.5 h approximately. Mean blood loss was 328 ml approx (range 150–600 ml). Postoperative delayed gastric emptying was observed in 8 (25%) patients. Three (9.4%) patients developed superficial surgical site infection. Mean hospital stay was 16.5 days (range 13–20 days). There were no pancreatic leak or fistula and no perioperative mortality. It is a feasible technique. It achieved zero leak rates, zero mortality and minimal morbidity without compromising any oncologic principles.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pancreatic adenocarcinoma is the ninth most common cancer diagnosed worldwide. However, pancreatic cancer death ranks fourth in cancer deaths each year. Despite all possible treatments, the 5-year survival remains dismal and less than 5% of patients survive [1]. The first successful pancreatoduodenectomy was performed by Kausch in 1912. Whipple et al. described pancreatoduodenectomy for ampullary cancers in 1935 [2, 3]. Since then, pancreatoduodenectomy is commonly performed for various benign and malignant diseases of the pancreas and ampullary region. Despite all surgical and technical advances, pancreatoduodenectomy surgery still has high morbidity and mortality [4, 5]. Once resection of the specimen is done, three anastomoses are established: pancreato-enteric, biliary-enteric and gastro-enteric anastomoses. Among the three anastomoses, the pancreato-enteric anastomosis is the most crucial one and its complications are responsible for most of the morbidities and mortalities of pancreatoduodenectomy surgery.
Dehiscence of pancreato-enteric anastomosis leads to a life-threatening complication in the form of a pancreatic fistula. A pancreatic fistula leading to an intra-abdominal sepsis is the leading cause of mortality in pancreatoduodenectomy surgery [6]. Other causes of mortality are haemorrhage, cardiac event and pulmonary embolism [7]. Several large studies worldwide showed the pancreatic fistula rate to be 11–15% [8, 9]. According to International Study Group of Pancreatic Fistula (ISGPF), pancreatic fistula is defined as any measurable amount of persistent intra-abdominal drain output on or after the third postoperative day which has amylase content greater than three times the upper limits of a normal serum level [10].
There are several anastomotic techniques used to restore the pancreto-enteric continuity, i.e. pancreatojejunostomy (duct to mucosa), pancreatogastrostomy in single or double layers and pancreatojejunostomy by dunking method. Dunking can be done in an ‘end to end’ or ‘end to side’ fashion. Regardless of the choice of technique, the complication rate ranges from 30 to 50% and the overall mortality rate between 1.4 and 10% [11, 12]. But there is paucity of data from Indian studies. Herewith, we report our own experience with a single-layer end to side dunking pancreatojejunostomy technique in a retrospective study and evaluate postoperative complications in a tertiary care oncology centre in central India.
Method
From January 2013 to January 2016, 32 consecutive patients who underwent pancreatoduodenectomy for malignant pancreatic disease were analysed retrospectively. All procedures performed in the study were in accordance with the ethical standards of the institution. Twenty-one patients were diagnosed to have carcinoma in the head of the pancreas and 11 patients had periampullary carcinoma. All the patients underwent standard Whipple’s operation.
All routine biochemical blood tests were carried out. Chronic anaemia and malnutrition were corrected. Haemoglobin level was maintained above 10 g/dl, and TPN was given to patients who had chronic malnutrition. Abdominal ultrasound and triple-phased contrast-enhanced CT were ordered preoperatively for all the patients to stage the disease and to rule out inoperability. Preoperative ERCP and biliary drainage in the form of biliary stenting were used for the 12 patients who had bilirubin level above 20 mg/dl or complaints of severe pruritus.
Various patient data, i.e. preoperative symptoms and demography, intra-operative time, blood loss and need of blood transfusion, postoperative hospital stay and complications, were noted. Patients were followed up for a maximum period 1 year for any adverse effect and survival.
Surgical Technique
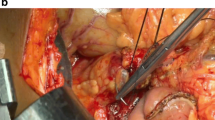
All the patients were operated under general anaesthesia. The abdomen was opened through bilateral subcoastal incision. Standard Whipple’s operation was performed in all patients with peripancreatic and hepatoduodenal lymph node dissection en bloc (Fig. 1). After resection of the specimen, pancreatojejunal anastomosis was established in an end to side dunking fashion.
Pancreatic remnant was mobilised ventrally for at least 2-cm dividing superior and inferior attachments. The pancreatic duct was cannulised with a feeding tube to prevent it from any injury during anastomosis. The end of the jejunum was closed with a linear stapler, and approximately 2 cm distal to the staple line pancreatojejunal, anastomosis was established in an end to side manner. The jejunum was cut open longitudinally at the anti-mesenteric border with an electrocautery. The opening was around the same size as the diameter of the pancreatic remnant. Posterior layer of the pancreatic capsule and parenchyma were sutured with the full thickness of the inner layer of the jejunal opening with interrupted PDS 4-0. Care was taken to prevent any injury to the pancreatic duct during this step. A single suture was passed through the pancreatic duct and mucosa of the jejunum to hold the stent in place while suturing the posterior layer. Similarly, the anterior layer of the pancreatic capsule and parenchyma were sutured with the anterior layer of the jejunal opening in a full thickness manner. Thus, a single-layer end to side dunking anastomosis between the jejunum and the pancreas was accomplished (Figs. 2 and 3). Feeding jejunostomy was done in every patient to start enteric feeding as early as possible.
Postoperatively, nasogastric tube and intra-abdominal drainage tubes were kept. Drain output was monitored regularly. All patients received postoperative antibiotics and proton pump inhibitors. Somatostatin analogue (Octreotide) was used routinely. Feeding jejunostomy was created in every patient.
Results
Thirty-two consecutive patients (21 patients of ampullary carcinoma and 11 patients of carcinoma in the head of the pancreas) were operated from January 2013 to January 2016. Nineteen patients were males, and 13, were females. Mean age of the patients was 53.9 years (range 19–70 years). Jaundice and weight loss were the most common symptoms in these patients (Table 1).
Mean operative time was 3.5 h approximately and mean blood loss was 328 ml (range 150–600 ml) approximately. Three patients required intra-operative blood transfusion. None of the patients showed postoperative anastomotic leakage or pancreatic fistula. Drain fluid amylase was measured on the third, seventh and tenth postoperative days to confirm the absence of pancreatic fistula. In our study, the drain was kept for 10 days to look for any late leak from pancreatojejunostomy under close monitoring. Postoperative delayed gastric emptying was observed in 8 (25%) patients and required prolonged nasogastric tube intubation. Three (9.4%) patients developed superficial surgical site infection. All the patients were started on feeding through feeding jejunostomy on the next day, and trial of oral liquid on the fifth postoperative day. Mean hospital stay was 16.5 days (range 13–20 days). There was no perioperative and in hospital mortality. All the patients were followed up for 1 year. There was no 90-day mortality in our study. Three patients developed liver metastasis and died of liver failure. The 12-month survival was 90.6%.
Discussion
Pancreatojejunal anastomosis is the most important anastomosis in respect to the risk of leakage, and if leakage occurs, it is the leading cause of morbidity and mortality. There are many risk factors for leakage of pancreatojejunal anastomosis like main pancreatic duct diameter, blood supply of the cut end of the jejunum, pancreatic texture, preoperative nutritional status of the patient and finally the anastomotic technique [13, 14]. Anastomotic technique remains the most important factor to reduce the risk of pancreatic leak; hence, many surgeons keep on improvising upon the surgical technique. Despite many techniques, none of the techniques yet have been proven to be superior to the others conclusively [15].
Some authors reported better results with duct to mucosa technique whereas a prospective randomised study conducted by Bass et al. proved that end to side dunking technique is better [16,17,18]. Giacomo et al. showed that patients with major breakdown of pancreatojejunal anastomosis which required reoperation belonged to the duct to mucosa anastomotic group when compared to the end to side dunking group in his study (25 vs 11%) [19].
It is proven that soft pancreas and small pancreatic diameter have high risk of leakage. Hence, a surgical technique which incurs minimal damage to the duct and pancreatic parenchyma tends to have the highest rate of success. In the current study, surgeons performed single-layer end to side dunking pancreatojejunal anastomosis which appears to have many fold advantages compared to other techniques which translated into a zero leak rate in our setup. End to side pancreatojejunal anastomosis is more anatomical for both pancreatic remnant and jejunum. Single-layer anastomosis reduces the injury to already soft-textured pancreas and risk of damage. The end to side dunking technique is superior to end to end dunking because in the end to end dunking, the mesenteric end of the jejunum is prone to hematoma formation if mesenteric vessels are accidently taken into sutures and thus leads to leakage. There can be a luminal disparity between jejunal end and pancreatic remnant diameter while performing end to end dunking which can be avoided in end to side dunking.
In the present study, all the cases were of malignant pancreatic disease and majority had soft and friable pancreas. In soft and friable pancreas, dunking technique appears to be better as compared to duct to mucosa technique which is better for fibrotic pancreas and dilated main pancreatic duct [15, 20, 21].
In our study, the most common complication is delayed gastric emptying (25%) followed by superficial surgical site infection (9.37%) which is as per the literature available [22, 23]. Preoperative nutritional status is an important factor for favourable outcome. In our study, all the patients had preoperative haemoglobin level of above 10 g/dl and chronic malnutrition was treated by TPN.
Although the number of patients in the current study was limited, the single-layer end to side dunking anastomosis has been proven to be safe and feasible. Larger randomised trials are required to come to any conclusion regarding which technique is better. In our series of Indian patients, this surgical technique helped to achieve a zero leak rate, zero mortality and minimal morbidity without compromising any oncologic principles. Amidst all the results, good training in hepatobiliary surgery and good surgical technique is of utmost importance regardless of the technique used. This study gives us the opportunity to explore the feasibility and safety of this technique in a larger prospective randomised controlled study in Indian patients.
References
Yachida S, Jones S, Bozic I, Antal T, Leary R, Fu B et al (2010) Distant metastasis occurs late during the genetic evolution of pancreatic cancer. Nature 467:1114–1117
Kausch W (1912) Das carcinoma der papilla duodeni und seine radikale entfernung. Beitrage zur Klinischen Chirurgie 78:439–486
Whipple AO, Parsons WB, Mullins CR (1935) Treatment of carcinoma of the ampula of vater. Ann Surg 102:763–779
Buchler MW, Friess H, Wagner M, Kulli C, Wagener V, Z'graggen K (2000) Pancreatic fistula after pancreatic head resection. Brit J Surg 87:883–889
Choi SH, Moon HJ, Heo JS, Joh JW, Kim Y (2004) Delayed hemorrhage after pancreaticoduodenectomy. J Gastro Surg 9:1293–1299
Yeo CJ, Cameron JL, Sohn TA, Lillemoe KD, Pitt HA, Talamini MA et al (1997) Six hundred fifty consecutive pancreaticoduodenectomies in the 1990: pathology, complications and outcomes. Ann Surg 226(3):248–257
Bassi C, Butturini G, Molinari E, Mascetta G, Salvia R, Falconi M (2004) Pancreatic fistula rate after pancreatic resection. The importance of definitions. Dig Surg 21(1):54–59
Shrikhande S, Kleeff J, Büchler M et al (2007) Pancreatic anastomosis after pancreaticoduo denectomy: how we do it. Indian J Surg 69:224–229
Caronna R, Peparini N, Russillo GC et al (2012) Pancreaticojejuno anastomosis after pancreaticoduodenectomy: brief pathophysiological considerations for a rational surgical choice. Int J Sur Oncol 2012:1–4
Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki Z et al (2005) Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery 138(1):8–13
Kostov DV, Kobakov GL, Yankov DV et al (2014) A simple and dependable technique for pancreatic-enteric anastomosis with a soft pancreas and nondilated duct. Surg Sci 5:444–453
Poon RT, Lo SH, Fong D, Fan ST, Wong J (2002) Prevention of pancreatic anastomosis leakage after pancreaticoduodenectomy. Am J Surg 183:42–52
van Berge Henegouwen MI, De Wit LT, Van Gulik TM, Obertop H, Gouma DJ (1997) Incidence, risk factors and treatment of pancreatic leakage after pancreaticoduodenectomy: drainage versus resection of the pancreatic remnant. J Am C Surg 18:18–24
Yeo CJ, Cameron JL, Lillemoe KD, Sauter PK, Coleman J, Sohn TA et al (2000) Does prophylactic octreotide decrease the rates of pancreatic fistula and other complications after pancreatico-duodenectomy? Results of a prospective randomized placebo-controlled trial. Ann Surg 232:419–429
Sikora SS, Posner M (1995) Management of the pancreatic stump following pancreatoduodenectomy. Br J Surg 82:1590–1597
Howard JM (1997) Pancreatojejunostomy: leakage is a preventable complication of Whipple resection. J Am Coll Surg 184:454–457
Matsumoto Y, Fuji H, Miura K, Inoue S, Sekikawa T, Aoyama H et al (1992) Successful pancreatojejunal anastomosis for pancreatoduodenectomy. Surg Gynecol Obstet 175:555–562
Bassi C, Falconi M, Molinari E, Mantovani W, Butturini G, Gumbs AA et al (2003) Duct to mucosa versus end to side pancreaticojejunostomy reconstruction after pancreaticoduodenectomy results of a prospective randomized trial. Surgery 134:766–771
Batignani G, Fratini G, Zuckermann M, Bianchini E, Tonelli F (2005) Comparison of Wirsung-jejunal duct to mucosa and dunking technique for pancreatojejunostomy after pancreatoduodenectomy. Hepatobiliary Pancreat Dis Int 4(3):450–455
Marcus SG, Cohen H, Ranson JH (1995) Optimal management of the pancreatic remnant after pancreaticoduodenectomy. Ann Surg 221:635–648
Kawai M, Kondo S, Yamaue H, Wada K, Sano K, Motoi F et al (2011) Predictive risk factors for clinically relevant pancreatic fistula analysed in 1239 patients with pancreaticoduodenectomy: multicentre data collection as a project study of pancreatic surgery by the Japanese Society of Hepato-Biliary-Pancreatic Surgery. J Hepato-Biliary-Pancreatic Sciences 18:601–608
Wiroon B, Thawatchai A, Darin L (2005) Whipple’s operation without an operative mortality in 37 consecutive patients: Thai surgeon’s experiences. J Med Assoc Thail 88(4):467–472
Gupta BB, Bellurkar AN, Changole SS et al (2016) Whipple’s procedure: yesterday and today. Int J Hepatobiliary Pancreat Dis 3:1–5
Acknowledgements
The authors would like to thank the Regional Cancer Centre, Pt. Jawahar Lal Nehru Memorial Medical College, Raipur, India.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gupta, A., Nandi, S., Tiwari, S. et al. 32 Consecutive Cases of Whipple’s Operation with Single-Layer End to Side Dunking Pancreatojejunostomy Without Any Pancreatic Fistula: Our Institutional Experience. Indian J Surg Oncol 9, 162–165 (2018). https://doi.org/10.1007/s13193-017-0707-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13193-017-0707-5