Abstract
Background/purpose
It is important to predict the development of clinically relevant pancreatic fistula (grade B/C) in the early period after pancreaticoduodenectomy (PD). This study has been carried out as a project study of the Japanese Society of Hepato-Biliary-Pancreatic Surgery (JSHPBS) to evaluate the predictive factors associated with clinically relevant pancreatic fistula (grade B/C).
Method
The data of 1,239 patients from 11 medical institutions who had undergone PD between July 2005 and June 2009 were retrospectively analyzed to review patient characteristics and perioperative and postoperative parameters.
Results
A drain amylase level >4,000 IU/L on postoperative day (POD) 1 was proposed as the cut-off level to predict clinical relevant pancreatic fistula by the receiver operating characteristic (ROC) curve. The sensitivity, specificity, and accuracy of this cut-off level were 62.2, 89.0, and 84.8%, respectively. A multivariate logistic regression analysis revealed that male [odds ratio (OR) 1.7, P = 0.039], intraoperative bleeding >1,000 ml (OR 2.5, P = 0.001), soft pancreas (OR 2.7, P = 0.001), and drain amylase level on POD 1 >4,000 IU/L (OR 8.6, P < 0.001) were the significant predictive factors for clinical pancreatic fistula.
Conclusion
The four predictive risk factors identified here can provide useful information useful for tailoring postoperative management of clinically relevant pancreatic fistula (grade B/C).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In most patient series, the incidence of pancreatic fistula has been reported to vary between 5 and 20% after pancreaticoduodenectomy (PD) and to be associated with a high mortality rate [1–7]. In 2005, the International Study Group of Pancreatic Fistula (ISGPF) proposed a consensus definition and clinical grading of postoperative pancreatic fistula [8]. The most important issue currently being debated regarding pancreatic fistulas is whether it is possible to predict the development of clinically relevant pancreatic fistula (grade B/C) according to the ISGPF proposal in the early period after PD. The risk factors for developing a pancreatic fistula in previously reported studies may have been able to predict all grades of pancreatic fistulas but, unfortunately, could not predict the extent of severe clinically relevant pancreatic fistula (grade B/C) [9–13].
Molinari et al. [14] proposed that a drain amylase value on postoperative day (POD) 1 of >5,000 U/L was a significant predictive factor for the incidence of all grades of pancreatic fistula after PD. However, this amylase value could not distinguish clinically relevant pancreatic fistulas (grade B/C) from insignificant disease during the early postoperative period. Kawai et al. proposed that a combination of two predictive postoperative factors on POD 4, namely, serum albumin level ≤3.0 g/dL and leukocyte counts >9,800/mm3, can predict the development of clinically relevant pancreatic fistula [15]. However, these two factors may also reflect serious systemic inflammation, such as that due to other intra-abdominal or respiratory complications. It therefore remains unclear which predictive risk factor(s) can be used to precisely distinguish the risk of clinically relevant pancreatic fistula (grade B/C) in the early postoperative period. In an attempt to clarify this situation, the Japanese Society of Hepato-Biliary-Pancreatic Surgery (JSHPBS) decided to perform a survey of high-volume PD centers in Japan to evaluate the predictive factors for the development of clinically relevant pancreatic fistula (grade B/C) in the early period after PD.
Methods
Patients
Data were collected by a questionnaire survey on all patients who underwent PD between July 2005 and June 2009 at one of 11 high-volume centers participating in the project study of the JSHPBS. The following patient characteristics and perioperative and postoperative parameters were reviewed: age, gender, body mass index (BMI), American Society of Anesthesiologists (ASA) class, preoperative laboratory data, such as hemoglobin, creatinine, HbA1c (glycated hemoglobin), albumin, total bilirubin, and amylase, preoperative biliary drainage, length of the surgery, intraoperative bleeding, blood transfusion, pancreatic texture (soft or hard), presence or absence of dilatation of the main pancreatic duct, histologic diagnosis (malignant or benign), and the serum C-reactive protein (CPR) and drain amylase levels on POD 1, 3, and 4. In total, data on 1,331 patients were collected from the 11 institutions. Of these 1,331 patients, 1,239 (749 men, 490 women; median age 67 years, age range 35–91 years) were enrolled in the study, and their data used for the analysis of the occurrence of pancreatic fistula using the ISGPF criteria.
Postoperative complications
The diagnosis of pancreatic fistula was made based on the ISGPF guidelines [8], namely, an amylase level in the drainage fluid on POD 3 of more than threefold the serum amylase level. Pancreatic fistulas were classified into three categories according to the ISGPF guidelines:
-
Grade A: Transient fistula. There is no clinical impact. The patient is fed orally and remains clinically well.
-
Grade B: Patients are usually supported with partial, total parenteral, or enteral nutrition. Antibiotics are usually used for signs of infections and a somatostatin analogue may also be required. Percutaneous drainage or persistent drainage for more than 3 weeks is usually required.
-
Grade C: A major change in clinical management or deviation from the normal clinical pathway. Total parenteral, enteral nutrition, antibiotics, or somatostatin analogue is often instituted in an intensive care unit (ICU) setting. Radiologic intervention or reoperation is required. The patients typically require an extended hospital stay with a major delay in hospital discharge and have life-threatening complications, such as intra-abdominal bleeding or sepsis. There is a real possibility of postoperative mortality[8].
Grades B + C were defined as “clinically relevant pancreatic fistula”. Delayed gastric emptying (DGE) was defined according to a consensus definition and the clinical grading of postoperative DGE according to the proposals of the International Study Group of Pancreatic Surgery (ISGPS) [16], using the web-based calculator (http://pancreasclub.com/calculator/) to improve the homogeneity of the definition [17]. DGE was then classified into three categories (grade A, B, or C) by the ISGPS clinical criteria based on the clinical course and postoperative management, such as reinsertion of a nasogastric tube, the period of inability to tolerate a solid diet, presence or absence of vomiting, and the use of prokinetics. Other postoperative complications were graded according to the Clavien classification [18], where grade I is any deviation from the normal postoperative course but without any need for pharmacologic treatment or surgical, endoscopic, or radiologic intervention; grade II is indicated by complications requiring pharmacologic treatment; grade III, by complications requiring surgical, endoscopic, or radiologic intervention; grade IV, life-threatening complications requiring intermediate or ICU management; grade V, death. Complications in this study were defined as a condition that was more than grade II according to the Clavien classification.
Statistical analysis
Continuous variables were expressed as the mean ± standard deviation (SD). Patient characteristics and perioperative and postoperative factors between the groups were compared using chi-square statistics, the Fisher exact test, and the Mann–Whitney U test. Variables with P < 0.05 were entered into a logistic regression model to determine independent risk factors of postoperative complications. The independent risk factors of the variables were expressed as odds ratios (OR) with their 95% confidence intervals (CI). The measurement of drain amylase levels on POD 1 has a major benefit by enabling the development of clinically relevant pancreatic fistula (grade B/C) to be predicted in the early period after PD. In fact, amylase values in drains on POD 1 of >5,000 U/L have been reported to be a significant predictive factor for the incidence of all grades of pancreatic fistula after PD [14]. Therefore, the optimal cut-off levels of the drain amylase level on POD 1 for differentiation between the no pancreatic fistula/grade A group and the grade B/C group were sought by constructing receiver operating characteristic (ROC) curves, which were generated by calculating the sensitivities and specificities of the drain amylase level on POD 1 at several predetermined cut-off points. Line graphs were used for graphical visualization (SPSS, Chicago, IL). Statistical significance was defined as P < 0.05.
Results
The indications for PD in the 1,239 patients were 573 pancreatic adenocarcinoma, 237 bile duct carcinoma, 124 ampullary adenocarcinoma, 127 intraductal papillary neoplasms, 38 duodenal adenocarcinoma, 37 pancreatic endocrine neoplasms, 46 tumor-forming pancreatitis, and 57 “other” diseases.
Postoperative complications
Table 1 shows the postoperative complications among the patient cohort after PD. The overall morbidity was 44.2% (548/1,239 patients). The overall rate of pancreatic fistula was 30.2% (374 patients). When the pancreatic fistula was classified into the three categories according to the ISGPF criteria, 15.8% (196/1,239) of the patients had grade A fistula; 11.8% (146 patients) had grade B; 2.6% (32 patients) had grade C. In total 139 (11.2%) patients had intra-abdominal abscess, and 58 patients (4.7%) required percutaneous drainage for the development of intra-abdominal abscess related to pancreatic fistula after PD. The reoperation rate due to pancreatic fistula was 0.72% (9/1,239 patients), and the overall incidence of DGE was 16.9% (211/1,239 patients). The DGE was categorized according to the ISGPS guidelines into grade A (107 patients, 9.6%), grade B (51 patients, 4.1%), and grade C (53 patients, 4.3%). The overall mortality rate was 0.97% (12/1,239 patients).
Comparison of patient characteristics, intraoperative status, and postoperative outcome among types of pancreatic fistula
Table 2 shows the general characteristics, intraoperative status, and postoperative outcome of the 1,239 patients classified by ISGPF. Based on the ISGPF criteria, 865 of the 1,239 patients (69.8%) did not develop a pancreatic fistula, and 196 patients (15.8%) developed only transient pancreatic fistula (grade A), while a clinically relevant pancreatic fistula (grade B/C) developed in 178 patients (14.4%). The ratio of male to female patients was significantly higher in those patients with a grade B/C fistula than in those with no pancreatic fistula or a grade A fistula. In those patients with a grade B/C fistula, the length of the surgery was significantly longer, and the intraoperative bleeding or the need for blood transfusion was significantly higher, compared to subjects with no pancreatic fistula or a grade A fistula. Patients with soft pancreatic parenchyma or a pancreatic duct <3 mm had a significantly higher incidence of pancreatic fistula (grade A and grade B/C) than those with no pancreatic fistula (P < 0.01). There were no significant differences between patients with grade A and grade B/C pancreatic fistual in term of the presence of soft pancreatic parenchyma or pancreatic duct <3 mm.
With regard to the postoperative outcome, the drain amylase level on POD 1 in the grade B/C group (18,846 ± 37,287 IU/L) was significantly higher than that in the grade A group (7,951 ± 15,322 IU/L) (P = 0.002), whereas there was no significant difference between the grade A group and grade B/C group in terms of drain amylase level on POD 3 and 4.
Predictive factors for the development of a clinically relevant pancreatic fistula (grade B/C)
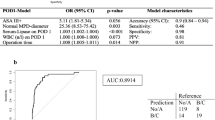
With regard to the sensitivity and specificity of the drain amylase level on POD 1, an area under the ROC curve of 0.840 was obtained (P < 0.001; 95% confidence interval: 0.807–0.874) (Fig. 1). Drain amylase level >4,000 IU/l on POD 1 was suggested to be the best cut-off for prediction of the clinically relevant pancreatic fistula. The sensitivity, specificity, accuracy, positive predictive value and negative predictive value of drain amylase level on POD1 >4,000 IU/l were 62.2, 89.0, 84.8, 51.1 and 92.7%, respectively.
Receiver operating characteristic (ROC) curves fore drain amylase level on postoperative day (POD 1) to predict clinically relevant pancreatic fistula (grade B/C). An area under the ROC curve of 0.841 was obtained taking the sensitivity and specificity of the drain amylase level on POD 1 into consideration [P < 0.001, 95% confidence interval (CI) 0.806–0.876]. A drain amylase level >4,000 IU/l on POD 1 was therefore suggested to be the best cut-off for predicting the clinical occurrence pancreatic fistula
Univariate and multivariate analysis were used to reveal those factors predicting grade B/C pancreatic fistula. Table 3 presents the results of the univariate analysis of 18 parameters as potential risk factors in the 178 patients with clinically relevant pancreatic fistula (grade B/C) versus 1,061 patients with no pancreatic fistula or with transient pancreatic fistula (grade A). Nine factors were extracted and identified as being useful for discriminating between those who would develop grade B/C fistula and those who would not develop a fistula or would develop only grade A fistula: (1) preoperative factors, namely, male gender (P < 0.001), BMI >25 kg/m2 (P = 0.005), HbA1c >7.0% (P = 0.001), and creatinine >1.5 mg/dL (P = 0.039); (2) intraoperative factors, namely, operative time >480 min (P = 0.012), intraoperative bleeding >1,000 mL (P = 0.001), soft pancreatic parenchyma (P < 0.001), and main pancreatic duct <3 mm (P < 0.001); (3) one postoperative factor, namely, drain amylase level on POD 1 >4,000 IU/L (P < 0.001). A multivariate logistic regression analysis revealed that male gender (OR 1.7, 95% CI 1.0–3.0, P = 0.039), intraoperative bleeding >1,000 mL (OR 2.5, 95% CI 1.4–4.6, P = 0.001), soft pancreatic parenchyma (OR 2.7, 95% CI 1.5–4.8, P = 0.001), and drain amylase level on POD 1 >4,000 IU/L (OR 8.6, 95% CI 5.2–14.2, P < 0.001) were the significant predictive factors for developing clinically relevant pancreatic fistula of grade B/C (Table 4).
Discussion
The development of pancreatic fistula has been reported to be a potentially life-threatening complication after PD [19–21]. Although lower grade fistula can still complicate patient recovery, it is very important to be able to predict whether a patient will develop clinically relevant pancreatic fistula (grade B/C) in the early period after PD, since these fistulas require changes in patient management and are associated with a higher mortality rate. This study was conducted as a project study of the JSHPBS and was designed to evaluate the predictive factors associated with the development of a clinically relevant pancreatic fistula (grade B/C) after PD. We found that male gender, intraoperative bleeding >1,000 mL, soft pancreatic parenchyma, and drain amylase level on POD 1 of >4,000 IU/L were the most significant predictive factors of the development of clinically relevant pancreatic fistula (grade B/C). In particular, a drain amylase value >4,000 U/L on POD 1 correlated with 8.6-fold increased risk of developing clinically relevant pancreatic fistula.
Some authors have proposed that drain-related data, including the drain amylase level, are useful for defining the risk of developing a pancreatic fistula after PD [14, 22, 23], including Molinari et al. [14], who suggested that a drain amylase value on POD 1 >5,000 U/L was a significant predictive factor for the incidence of pancreatic fistula. However, the latter study was limited due to the small sample size (n = 137). Moreover, of the 137 patients enrolled in the study, 36 patients underwent distal pancreatectomy, and 12 (44%) of the 27 patients with pancreatic fistula reported in their results underwent distal pancreatectomy, not PD [14]. In these three studies [14, 22, 23], clinically relevant pancreatic fistula (grade B/C) could not be distinguished from transient (grade A) fistula in the early postoperative period solely based on the drain amylase value. In three other studies [15, 24, 25], the authors were unable to determine whether the drain amylase value was reflective of clinically relevant pancreatic fistula, although they did propose the evaluation of predictive risk factors, such as the presence of soft pancreas, intra-abdominal bleeding, and the postoperative albumin level, as indicators for the development of clinically relevant pancreatic fistula. To the best of our knowledge, our study is the first published report demonstrating that the drain amylase value on POD 1 can predict the development of clinically relevant pancreatic fistula (grade B/C). Therefore, based on the results of this study, early removal of drains can be done when the drain amylase value is <4,000 U/L on POD 1 because these patients are unlikely to develop clinically relevant fistula. Moreover, early drain removal has previously been demonstrated to play a critical role in reducing the incidence of pancreatic fistula or intra-abdominal abscess [26, 27].
In contrast, the authors of a number of other studies have found that the amylase level in drainage fluid after PD has no clinical significance [28, 29]. The ISGPF has proposed that the ability to detect pancreatic fistula is imperfect when only drain data are used [28]. Two factors may underlie this low predictive ability: first, there have been patients who ultimately demonstrated no clinically relevant symptoms of pancreatic fistula despite having amylase-rich fluid on POD 1; second, there was the pattern of pancreatic fistula defined by Pratt et al. [30] as latent pancreatic fistula. Latent fistulas have been defined as initially lacking amylase-rich fluid but ultimately becoming clinically relevant pancreatic fistula (grade B/C). Pratt et al. [30] proposed that advanced age and small pancreatic duct size were significantly associated with latent fistulas.
There are several limitations to our study because of the multicenter and retrospective nature of the data collection. First, the surgical procedures, such as pancreaticoenterostomy (pancreaticogastrostomy or pancreaticojejunostomy) or use of pancreatic duct stent (internal, external, or no stent), were not standardized across institutions. Second, drain management, such as the number of drains, location of placed drains, or drain type, varied widely according to institutional experience. There were cases which ultimately demonstrated no clinically relevant symptoms of pancreatic fistula despite having amylase-rich fluid on POD 1. In fact, 48.9% of patients with a drain amylase value >4,000 U/L on POD 1 did not develop a clinically relevant pancreatic fistula. Therefore, further studies are necessary to prospectively validate these predictive risk factors to confirm the possible relationship between these factors and the development of clinically relevant pancreatic fistula (grade B/C).
In conclusion, the results of this study, which was an initiative of the JSHPBS, indicated that male gender, soft pancreas, intraoperative bleeding >1,000 ml, and amylase value >4,000 U/L in drains on POD 1 were significant predictive risk factors for developing clinically relevant pancreatic fistula (grade B/C). Management of pancreatic fistula in the early period after PD is not sufficiently standardized. Therefore, the identification of these predictive risk factors can provide useful information to tailor the postoperative management for patients who are at an increased risk of developing pancreatic fistula, including drain management, and the administration of antibiotics, a protease inhibitor, octreotide, or enteral nutrition.
References
McPhee JT, Hill JS, Whalen GF, Zayaruzny M, Litwin DE, Sullivan ME, et al. Perioperative mortality for pancreatectomy. A national perspective. Ann Surg. 2007;246:246–53.
Bűchler MW, Wagner M, Schmied BM, Uhl W, Friess H, Z’graggen K. Changes in morbidity after pancreatic resection. Toward the end of completion pancreatectomy. Arch Surg. 2003;138:1310–4.
Tani M, Terasawa H, Kawai M, Ina S, Hirono S, Uchiyama K, et al. Improvement of delayed gastric emptying in pylorus-preserving pancreaticoduodenectomy: results of a prospective, randomized, controlled trial. Ann Surg. 2006;243:316–20.
Balcom JH, Rattner DW, Warshaw AL, Chang Y, Castillo CF. Ten-year experience with 733 pancreatic resections. Changing indications, older patients, and decreasing length of hospitalization. Arch Surg. 2001;136:391–8.
Kazanjian KK, Hines OJ, Eibl G, Reber HA. Management of pancreatic fistulas after pancreaticoduodenectomy: results in 437 consecutive patients. Arch Surg. 2005;140:849–54.
DeOliveira ML, Winter JM, Schafer M, Cunningham SC, Cameron JL, Yeo CJ, et al. Assessment of complications after pancreatic surgery: a novel grading system applied to 633 patients undergoing pancreaticoduodenectomy. Ann Surg. 2006;244:931–7.
Tani M, Kawai M, Hirono S, Ina S, Miyazawa M, Shimizu A, et al. A prospective randomized controlled trial of internal versus external drainage with pancreaticojejunostomy for pancreaticoduodenectomy. Am J Surg. 2010;199:759–64.
Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, et al. International Study Group on Pancreatic Fistula Definition. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 2005;138:8–13.
Wada K, Traverso LW. Pancreatic anastomotic leak after the Whipple procedure is reduced using the surgical microscope. Surgery. 2006;139:735–42.
Poon RT, Fan ST, Lo CM, Ng KK, Yuen WK, Yeung C, Wong J. External drainage of pancreatic duct with a stent to reduce leakage rate of pancreaticojejunostomy after pancreaticoduodenectomy: a prospective randomized trial. Ann Surg. 2007;246:425–33.
Adam U, Makowiec F, Riediger H, Schareck WD, Benz S, Hopt UT. Risk factors for complications after pancreatic head resection. Am J Surg. 2004;187:201–8.
Sato N, Yamaguchi K, Chijiiwa K, Tanaka M. Risk analysis of pancreatic fistula after pancreatic head resection. Arch Surg. 1998;133:1094–8.
Bottger TC, Junginger T. Factors influencing morbidity and mortality after pancreaticoduodenectomy: critical analysis of 221 resections. World J Surg. 1999;23:164–71. discussion 171-2.
Molinari E, Bassi C, Salvia R, Butturini G, Crippa S, Talamini G, et al. Amylase value in drains after pancreatic resection as predictive factor of postoperative pancreatic fistula: results of a prospective study in 137 patients. Ann Surg. 2007;246:281–7.
Kawai M, Tani M, Hirono S, Ina S, Miyazawa M, Yamaue H. How do we predict the clinically relevant pancreatic fistula after pancreaticoduodenectomy? An analysis in 244 consecutive patients. World J Surg. 2009;33:2670–8.
Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, et al. Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery. 2007;142:761–8.
Hashimoto Y, Traverso LW. Incidence of pancreatic anastomotic failure and delayed gastric emptying after pancreatoduodenectomy in 507 consecutive patients: use of a web-based calculator to improve homogeneity of definition. Surgery. 2010;147:503–15.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Akamatsu N, Sugawara Y, Komagome M, Shin N, Cho N, Ishida T, et al. Risk factors for postoperative pancreatic fistula after pancreaticoduodenectomy: the significance of the ratio of the main pancreatic duct to the pancreas body as a predictor of leakage. J Hepatobiliary Pancreat Sci. 2010;17:322–8.
Parr ZE, Sutherland FR, Bathe OF, Dixon E. Pancreatic fistulae: are we making progress? J Hepatobiliary Pancreat Surg. 2008;15:563–9.
Okabayashi T, Kobayashi M, Nishimori I, Sugimoto T, Onishi S, Hanazaki K. Risk factors, predictors and prevention of pancreatic fistula formation after pancreatoduodenectomy. J Hepatobiliary Pancreat Surg. 2007;14:557–63.
Shinchi H, Wada K, Traverso LW. The usefulness of drain data to identify a clinically relevant pancreatic anastomotic leak after pancreaticoduodenectomy? J Gastrointest Surg. 2006;10:490–8.
Yamaguchi M, Nakano H, Midorikawa T, Yoshizawa Y, Sanada Y, Kumada K. Prediction of pancreatic fistula by amylase levels of drainage fluid on the first day after pancreatectomy. Hepatogastroenterology. 2003;50:1155–8.
Pratt WB, Callery MP, Vollmer CM Jr. Risk prediction for development of pancreatic fistula using the ISGPF classification scheme. World J Surg. 2008;32:419–28.
Fuks D, Piessen G, Huet E, Tavernier M, Zerbib P, Michot F, et al. Life-threatening postoperative pancreatic fistula (grade C) after pancreaticoduodenectomy: incidence, prognosis, and risk factors. Am J Surg. 2009;197:702–9.
Kawai M, Tani M, Terasawa H, Ina S, Hirono S, Nishioka R. Early removal of prophylactic drains reduces the risk of intra-abdominal infections in patients with pancreatic head resection: prospective study for consecutive 104 patients. Ann Surg. 2006;244:1–7.
Bassi C, Molinari E, Malleo G, Crippa S, Butturini G, Salvia R. Early versus late drain removal after standard pancreatic resections: results of a prospective randomized trial. Ann Surg. 2010;252:207–14.
Reid-Lombardo KM, Farnell MB, Crippa S, Barnett M, Maupin G, Bassi C, et al. Pancreatic anastomotic leakage after pancreaticoduodenectomy in 1,507 patients: a report from the Pancreatic Anastomotic Leak Study Group. J Gastrointest Surg. 2007;11:1451–8. discussion 1459.
Shyr YM, Su CH, Wu CW, Lui WY. Does drainage fluid amylase reflect pancreatic leakage after pancreaticoduodenectomy? World J Surg. 2003;27:606–10.
Pratt WB, Callery MP, Vollmer CM Jr. The latent presentation of pancreatic fistulas. Br J Surg. 2009;96:641–9.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Kawai, M., Kondo, S., Yamaue, H. et al. Predictive risk factors for clinically relevant pancreatic fistula analyzed in 1,239 patients with pancreaticoduodenectomy: multicenter data collection as a project study of pancreatic surgery by the Japanese Society of Hepato-Biliary-Pancreatic Surgery. J Hepatobiliary Pancreat Sci 18, 601–608 (2011). https://doi.org/10.1007/s00534-011-0373-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00534-011-0373-x