Abstract
Breast cancer (BC) has become the most common cancer in urban women. Unfortunately, most women are not aware of BC symptoms/signs, prevention, and management. In resource-limited countries like India where we do not have structured screening/awareness programs, a majority of women present with locally advanced BC. The aim of our study is to identify the present status of awareness about BC prevention, early detection, symptoms, and management in urban and rural Indian women (medical, paramedical, and nonmedical) and to assess whether education and socioeconomic strata have any role in better awareness about BC or not. We did a prospective cross-sectional observation study among the medical, paramedical, and nonmedical women in the northern part of India. We designed a questionnaire keeping in mind the three domains about BC—knowledge (questions 1–25 include risk factors, genetics, lifestyle changes, hormones, associated cancers, and modes of presentation like lump, nipple/skin changes), breast self-examination (questions 25–37), and attitude to prevention and early detection (questions 38–44). We also asked how many do breast self-examination (BSE) and what they think are the three main factors responsible for late presentation and the three main ways to increase BC awareness. The Likert scale was used for objective assessment. We analyzed the whole data using SPSS software version 15. A total of 220 women out of 270 completed the questionnaire. Out of 220 women, 26.4% were medical, 20.9% paramedical, and 52.7% nonmedical. Most women were educated (82.7%) and married (65%). 59.5% women resided in urban areas and the rest (40.5%) were from rural areas. We found that there was relatively more knowledge in the medical group; however, the skills of BSE and attitude to prevention and early detection in all the three subgroups and among rural and urban women were suboptimal and not different significantly. The three main factors responsible for delayed presentation were shyness and not knowing BSE, ignorance about BC symptoms, and social stigma of cancer along with financial constraints. The three main ways to improve BC awareness suggested were to have more advertisements on television and social media, roadside campaigns and in colleges along with group discussions and debates, and at grassroots level to involve Anganwadi workers and nurses to create more awareness in villages. There was less breast cancer knowledge and awareness among the nonmedical women compared to those among the medical and paramedical, the skills of BSE and attitude to prevention and early detection were suboptimal in all the three groups. Rural or urban dwellings did not make much difference in BC knowledge, skills of BSE, and attitude to prevention. More awareness regarding breast cancer symptoms with early detection and BSE need to be addressed with more information dissemination via social media, campaigns, and involvement of paramedics and social workers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
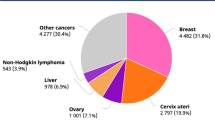
Breast cancer (BC) has surpassed cervical cancer and has become the most common cancer among Indian women residing in urban areas [1]. BC in India is seen most commonly in the fourth decade; however, incidence in the third decade is also rising [2]. BC in younger women behaves more aggressively and is more of a triple-negative hormonal status as compared to BC in older postmenopausal women. Most Indian women present with a locally advanced stage of BC which further reduces the survival rates. Patients presenting with early stage BCs have a better survival rate and good prognosis [3].
Lack of awareness is one of the biggest barriers to BC screening and early detection [4]. This sounds alarming and we need to create more awareness about early detection, knowledge of BC symptoms and signs, and breast self-examination. All screening programs recommend mammography after 40 years of age. In younger women, due to dense breasts, mammography is also not sensitive to detect small lesions. Hence, we need Indian solutions for our Indian problems and not extrapolate Western data on our patients.
Hence, we planned to do this study with its aim to identify the present status of awareness about BC prevention, early detection, symptoms, and management in urban and rural Indian women (medical, paramedical, and nonmedical) and to assess whether education and socioeconomic strata have any role in better awareness about BC or not.
Material and Methods
We did a prospective cross-sectional observation study among the medical, paramedical, and nonmedical women in the northern part of India. We designed a questionnaire keeping in mind the three domains about BC—knowledge (questions 1–25 include risk factors, genetics, lifestyle changes, hormones, associated cancers, and modes of presentation like lump, nipple/skin changes), skills of breast self-examination (questions 25–37), and attitude to prevention and early detection (questions 38–44).
We had three groups, medical, nonmedical, and paramedical women, for this study. Medical women included doctors working in King Georges’ Medical University, Lucknow where the study was performed, and these women doctors were not working in endocrine surgery/surgical oncology departments and were not dealing with breast cancer patients directly. The paramedical staff working in King Georges’ Medical University (KGMU) constituted the paramedical group. The nonmedical group included women working in Amity University, Noida who were mostly engineers, nonmedical women who worked in KGMU as technical staff, and some women who were working as household maids, and some who were known to them residing in nearby rural areas. We included all adult women 18 years of age and above. All these women who filled the questionnaire were normal healthy individuals and did not suffer from breast cancer at any stage of their lives.
We had given the questionnaire to 270 women, out of which 220 completed and returned the questionnaire. Fifty women who did not answer the questionnaire were not interested in our survey and did not return to us the filled questionnaire. This speaks of apathy in some women who think if they are not affected by disease/cancer then why bother about having knowledge/awareness about it. Most breast cancer survivors are the best people who value awareness, write books, and talk in public to create awareness and desire to see change in our society.
We also asked how many do breast self-examination (BSE) and what they think are the three main factors responsible for late presentation of patients to a doctor and the three main ways to increase BC awareness. The duration of getting the questionnaire circulated and filled was 3 months (June–August, 2016). The Likert scale was used for objective assessment. We analyzed the whole data using SPSS software version 15.
Results
Out of 220 women, 26.4% (n = 58) were medical, 20.9% (n = 46) paramedical, and 52.7% (n = 116) nonmedical. Most women were educated (82.7%) (n = 182) and married (65%) (n = 143). 59.5% (n = 131) women resided in urban areas and the rest (40.5% (n = 89)) were from rural areas. The mean age was 29 years (range 18 to 74 years).
We found many common myths among all the women which need to be cleared from their minds by conducting awareness programs. These myths included the following: 92 women thought BC happens only in women and does not affect men, 90 thought FNAC/core biopsy spreads cancer cells and 70 thought certain types of undergarments and deodorants/body perfumes cause BC. Seventy-five women did not know about the treatment parts of BC. One hundred and twenty-eight women thought BC treatment must be very costly and were not aware about the government’s health care scheme under which whole treatment is free for those of lower socioeconomic strata.
Figure 1 shows the comparison of knowledge, skills of BSE, and attitude to prevention and early detection in all the three subgroups (medical, paramedical, and nonmedical). We found that there was more knowledge component in medical women (58%, n = 34) compared to that in paramedics (50%, n = 28) and nonmedical women (41%, n = 48). We found that only 42% of the medicos knew about BSE compared to 36% of the paramedics and 28% of the nonmedical group. However, attitude to prevention and early detection was not very high or different in medicos (47%, n = 27), paramedics (44%, n = 20), and nonmedical women (34%, n = 39). This shows that we need to make all women irrespective of their socioeconomic status/education levels more aware about health-seeking behavior and its benefits.
Figure 2 shows the comparison of all the three components among women residing in rural and urban areas. The three domains were not different significantly. The knowledge component was poor in both the urban-residing women (38%, n = 132) and rural women (31%, n = 88). Less than one third did BSE in both the groups; also, the attitude to prevention and early detection was also less than 30% in both the subgroups.
Table 1 shows the details about BSE methodology questions and the comparison in all the three subgroups. A total of 146 women felt the need to learn BSE techniques and also desired to learn about the signs and symptoms of BC presentation. This shows that we need to have more awareness programs with more emphasis on BSE and signs and symptoms of BC with emphasis on the benefits of early presentation to a doctor. There was relatively more practice of BSE in the medical group; however, only 36% did BSE, so the overall practice of BSE was low. Only a third of women felt confident in doing BSE and did it regularly every month and a majority (67% of nonmedical women) felt the need for help from a clinician. The medical (48%) and paramedical (41%) groups recommended BSE to their friends and family members as compared to the nonmedical (10%) group. Only 19% of the medical, 4% of the paramedical, and 2% of the nonmedical group had a screening mammogram for themselves.
We found 60 women who had relatives/friends suffering from BC and had undergone treatment. We compared them to the other 160 women whose friends/relatives did not have BC. On this subgroup analysis, knowledge component was better (45%) in those whose relatives/friends were affected by BC as compared to those (30%) whose relatives/friends were never affected by BC. Even BSE practice was better in the former group (48%) as compared to that in the latter (31%). This shows that women do get concerned and have more knowledge and seek to consult doctors for their breast examination and themselves do BSE whenever they hear/see someone close to them getting BC.
The three main factors responsible for delayed presentation were shyness and not doing regular BSE, ignorance about breast cancer signs and symptoms, and social stigma of cancer along with financial constraints. Most women were not aware about BSE and many did in the wrong manner so did not know the correct technique.
The three main ways to improve breast cancer awareness suggested were to have more advertisements on television and social media, to do a lot of roadside campaigns and in colleges along with group discussions and debates to motivate the younger generation, and at grassroots level to involve Anganwadi workers and nurses to create more awareness in villages.
Discussion
Breast cancer incidence is growing in both developed and less developed countries; however, there are more deaths due to BC in less developed countries [5]. There are many factors responsible for increased mortality due to BC in resource-limited countries like younger age of presentation, more locally advanced BC stage, more triple-negative BC, more aggressive histology and higher grades of the tumor, patients defaulting and not completing whole treatment or total number of chemotherapies due to poverty/toxicities, money problems, and going for alternative methods of medicine like homeopathy [6].
There are no well-organized BC screening programs in India [7]. Mammographic screening has been debatable but most agree that BC awareness and BSE teaching programs are more useful for the society. Most studies show that BC awareness is much lower in less developed countries as compared to developed and that may be the reason for late stage of presentation and poor survival rates of BC in less developed countries [8]. Cochrane meta-analysis and many other studies show that BC awareness programs and interventions help educate women and improve BC care and health [9]. Hence, it is high time that we give equal importance to these educational programs and community activities as we devote our time on BC patients’ treatment.
A study by Gadgil A. et al. found 83% women knew that BC is curable if detected in the early stage and were willing to have more information about BC [10]. They found positive association of high income with better awareness. In our study, we found 72% of women knew about these facts and were willing to receive more information. Hence, we need to create more awareness about BC so that patients come in the earlier stage and have better survival rates. We also need to find out the barriers preventing patients from coming early and not completing the whole treatment so that we can work on those barriers and break them to improve our health care and health-seeking system.
A study done in South Africa showed that in patriarchal societies, women’s health is often ignored and women need permission and financial and moral support from their family members to pursue their treatment [11]. This also applies in our Indian scenario and we need to address this issue also in our awareness programs. We found many myths among women with regard to BC like FNAC causing spread of cancer cells, cost issues, and deviating to alternative medicines, and these need to be clarified and we need to impart correct knowledge to them.
In India, BC incidence is rising more in urban women compared to rural women. A study done on women residing in urban areas in Mumbai, India reported that the waist to hip ratio and late age of first child delivery in urban women compared to rural women were key factors responsible for BC to occur more in urban women [12]. Gupta A. et al. showed in their study that there is very poor awareness among Indian women irrespective of their socioeconomic status with regard to BC symptoms and early detection [13]. Abbas Balouchi et al. did a study in rural areas in Iran and found the reasons for poor scores in those women with regard to knowledge about BC were due to low literacy rates, lack of BSE technique trainings, and lack of medical facilities [14]. In our study, there were no statistically significant differences among urban and rural women; and hence, both sections need awareness programs.
The diagnostic power of BSE as reported in the literature is between 80 and 90% and helps in reduction of mortality rates [14]. In Malaysia, as a step to improve their BC care, the Ministry of Health has incorporated BSE education to all women above 20 years of age in their screening guidelines [15]. Another study done in Malaysia showed that scores of knowledge about BC and BSE practices and benefits improved in the intervention group who was educated and reassessed at 6-month and 1-year intervals as compared to the group who did not receive education modules [15]. A study done in the UK on elderly women also showed that intervention in the form of knowledge about BC symptoms helped in detecting BC in the early stage as compared to women who did not receive any information [16]. In our study, only a third of the total number of women did BSE and most were not confident in doing it correctly. Hence, we need to emphasize BSE techniques with correct methods in BC awareness programs. A study done on Thai women has used a self-validated BC awareness questionnaire and showed its effectiveness [17].
A study done in Delhi showed that financial constraints were the main barrier which prevented women of lower socioeconomic strata to seek BC treatment [18]. In our BC awareness programs, we need to highlight the government’s health care schemes under which the whole treatment is free for poor patients. Hence, financial constraints should no more be the limiting factor for patients to not come to doctors in the early stage of the disease.
The main limitations of our study were as follows: it was not a population-based study with a higher number of data, and there was no randomization and no intervention. Hence, we plan to conduct this survey among a larger population and we will have randomization in two groups, those who got education and those who did not, and will follow them for 2 years. This will give us a more meaningful outcome.
Conclusion
Breast cancer knowledge and awareness was less among the nonmedical women compared to that among the medical and paramedical groups. However, the skills of BSE and attitude to prevention and early detection were suboptimal in all the three groups. Rural or urban dwellings did not make much difference in BC knowledge, skills of BSE, and attitude to prevention. More structured awareness modules regarding breast cancer symptoms with early detection and BSE need to be addressed with more information dissemination via social media, campaigns, and involvement of paramedics and social workers.
References
Gupta S (2016) Breast cancer: Indian experience, data and evidence. South Asian J Cancer 5:85–86
Rangarajan B, Shet T, Wadasadawala T, Nair NS, Sairam RM, Hingmire SS, Bajpai J (2016) Breast cancer: an overview of published Indian data. South Asian J Cancer 5:86–92
Lannin DR, Wang S (2017) Are small breast cancers good because they are small or small because they are good? N Engl J Med 376:2286–2291
Schilling MP, Silva IF, Opitz SP, Borges MF, Koifman S, Rosalina Jorge K (2017) Breast cancer awareness among women in western Amazon: a population based cross-sectional study. Asian Pac J Cancer Prev 18:847–856
Nageeti TH, Abdelhameed AAN, Jastania RA, Felemban RM (2017) Perspective of Saudi women in the Makkah region on breast cancer awareness. J Fam Community Med 24:97–101
Akhtar M, Dasgupta S, Rangwala M (2015) Triple negative breast cancer: an Indian perspective. Breast Cancer (Dove Med Press) 7:239–243
Agarwal G, Ramakant P, Forgach ER, Rendón JC, Chaparro JM, Basurto CS, Margaritoni M (2009) Breast cancer care in developing countries. World J Surg 33:2069–2076
Kwok C, Fethney J, White K (2012) Breast cancer screening practices among Chinese-Australian women. Eur J Oncol Nurs 16:247–252
O'Mahony M, Comber H, Fitzgerald T, Corrigan MA, Fitzgerald E, Grunfeld EA, Flynn MG, Hegarty J (2017) Interventions for raising breast cancer awareness in women. Cochrane Database Syst Rev 2:CD011396
Gadgil A, Sauvaget C, Roy N, Grosse Frie K, Chakraborty A, Lucas E, Bantwal K, Haldar I, Sankaranarayanan R (2015) Breast cancer awareness among middle class urban women—a community-based study from Mumbai, India. Asian Pac J Cancer Prev 16:6249–6254
Maree JE, Wright SC (2010) How would early detection be possible? An enquiry into cancer related knowledge, understanding and health seeking behaviour of urban Black women in Tshwane, South Africa. Eur J Oncol Nurs 14:190–196
Nagrani R, Mhatre S, Boffetta P, Rajaraman P, Badwe R, Gupta S, Romieu I, Parmar V, Dikshit R (2016) Understanding rural-urban differences in risk factors for breast cancer in an Indian population. Cancer Causes Control 27:199–208
Gupta A, Shridhar K, Dhillon PK (2015) A review of breast cancer awareness among women in India: cancer literate or awareness deficit? Eur J Cancer 51:2058–2066
Balouchi A, Shahdadi H, AlKhasawneh E, Abdollahimohammad A, Firouzkouhi M, Sarani H, Gorgij A (2016) Rural women’s awareness about breast cancer in southeastern Iran: a cross-sectional study. Asian Pac J Cancer Prev 17:1875–1879
Akhtari-Zavare M, Juni MH, Said SM, Ismail IZ, Latiff LA, Ataollahi Eshkoor S (2016) Result of randomized control trial to increase breast health awareness among young females in Malaysia. BMC Public Health 16:738
Dodd RH, Forster AS, Sellars S, Patnick J, Ramirez AJ, Forbes LJL (2017) Promoting early presentation of breast cancer in older women: sustained effect of an intervention to promote breast cancer awareness in routine clinical practice. BMC Health Serv Res 17:386
Rakkapao N, Promthet S, Moore MA, Solikhah S, Hurst C (2017) Assessing breast cancer awareness in Thai women: validation of the breast cancer awareness scale (B-CAS). Asian Pac J Cancer Prev 18:995–1005
Dey S, Sharma S, Mishra A, Krishnan S, Govil J, Dhillon PK (2016) Breast cancer awareness and prevention behavior among women of Delhi, India: identifying barriers to early detection. Breast Cancer (Auckl) 10:147–156
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ramakant, P., Singh, K.R., Jaiswal, S. et al. A Survey on Breast Cancer Awareness Among Medical, Paramedical, and General Population in North India Using Self-Designed Questionnaire: a Prospective Study. Indian J Surg Oncol 9, 323–327 (2018). https://doi.org/10.1007/s13193-017-0703-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13193-017-0703-9