Abstract
Imaging plays a vital role in the evaluation of peritoneal malignancies. The presence of peritoneal metastases (PM) alters tumor staging, with direct implications in treatment choice and prognosis. Cytoreductive surgery (CRS) and Hyperthermic intraperitoneal chemotherapy (HIPEC) as a combined modality treatment have led to prolonged survival and even cure in selected patients with PM. Better outcomes are seen in patients with limited disease spread. Therefore, early diagnosis of peritoneal tumor seeding is essential. Despite significant advancement of technology, assessment of the origin of PM is often difficult, due partly to the complex peritoneal anatomy and partly due to the complex overlap of imaging features. Multidetector CT (MDCT) is the main stay due to its wide availbility, rapid evaluation, robust technique and good resolution. Imaging plays a vital role in selecting patients for the combined modality treatment. MRI is not as popular as CT due to limited availability, time required for the study and lack of experience with interpreting the results. PET-CT is useful in ruling out extra peritoneal disease and it is the CT component that is more reliable for predicting the disease extent. This article reviews the current use of various imaging modalities in various stages of treatment of patients with PM especially those undergoing CRS and HIPEC.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Peritoneal metastases (PM), defined as seeding and implantation of neoplastic cells in the peritoneum can result from tumors within or outside the peritoneal cavity or rarely in cases of primary tumors of the peritoneum. Over the last couple of decades, there is increased interest in PM due to the prolonged survival achieved with the combined modality treatment of CRS and HIPEC in these patients. Imaging plays a vital role in the diagnosis and treatment of PM. This article reviews the normal peritoneal anatomy, function, modes of disease spread, common imaging features and common sites of disease spread as well its role in selecting patients for CRS and HIPEC.
Anatomy of Peritoneum and Flow of Peritoneal Fluid
Normal Anatomy
The parietal peritoneum lines the anterior abdominal wall, retroperitoneum, pelvis, sub diaphragmatic space. The visceral peritoneum partly or completely encases the abdominal organs. The potential space between the two layers of peritoneum is termed the peritoneal cavity. The peritoneal ligaments (coronary, gastrohepatic, hepatoduodenal, falciform, gastrocolic, duodenocolic, gastrosplenic, gastrosplenic, splenorenal, and phrenicocolic) and mesenteries (transverse mesocolon, small bowel mesentery, and sigmoid mesentery) are double folds of peritoneum. These suspend and support the intraperitoneal organs and subdivide the peritoneal cavity into interconnected compartments that dictate the flow of fluid and location of disease (Fig. 1) [1].
Pathways of ascitic fluid and sites of pooling and seeding. The force of gravity operates to pool peritoneal fluid in pelvic recesses while negative sub diaphragmatic pressure directs fluid upward along paracolic gutters. From the right infracolic space fluid pools at the ileo-cecal junction while from the left infracolic space it pools at the sigmoid mesocolon and then overflows into the pelvis. From the pelvis, fluid ascends the right paracolic gutter to the right subhepatic and subphrenic spaces. The falciform ligament prevents diffusion to the left subphrenic space. Passage along the shallower left paracolic gutter is slow and weak and limited cephalad by the phrenicocolic ligament.(Adapted from Abreu e Silva,M. J. Magalhães,H. Duarte,C. Fernandes,S.Ramos Alves,A. Guimarães dos Santos,M. V. P. G. Almeida,Porto/PT, CT and PET-CT findings of peritoneal carcinomatosis,Educational Exhibit,ECR 2013)
The peritoneal cavity normally contains a very small volume of sterile fluid, which is similar to plasma. This fluid allows frictionless movement of visceral organs within the abdominal cavity which accumulates by gravity in the dependent portions and circulates in a cephalad direction by negative pressure produced in the upper abdomen by respiration [2].
In males, the peritoneum forms a closed sac resulting in a continuous peritoneal cavity. In females, the peritoneum is perforated by the lateral end of the fallopian tubes allowing communication with the extra-peritoneal compartment of the pelvis. [3].
Flow of Fluid in the Peritoneal Cavity
Meyers [3, 4] has shown that the transverse mesocolon, small bowel mesentery, sigmoid mesocolon, and peritoneal attachments of the ascending and descending colon serve as watersheds that direct the flow of intraperitoneal fluid.
Initially, peritoneal fluid preferentially seeks gravity-dependent spaces, such as the Pouch of Douglas in women and the retro vesical space in men, the lateral paravesical spaces, and then ascends cephalad in the paracolic gutters to reach the sub diaphragmatic spaces.
Most of the fluid ascends along the right paracolic gutter into the right sub diaphragmatic space, because the left paracolic gutter is shallow and discontinuous with the left sub diaphragmatic space at phrenicocolic ligament. Because direct passage from the right to left sub diaphragmatic space is prevented by the falciform ligament [2, 4, 5], fluid may be redirected caudally into the pelvis through the inframesocolic compartment, thus completing the circulatory pathway.
In disease state, fluid collects in well-defined areas of stasis, in the deep peritoneal recesses of the pelvis, the right lower quadrant (near the termination of the small bowel mesentery at the ileocecal junction), the superior aspect of the sigmoid mesocolon, and the right paracolic gutter [6].
Peritoneal Folds and Spaces
A ligament is defined as two folds of peritoneum that supports a structure within the abdominal cavity. The omentum is a specialised ligament that connects the stomach to an additional structure. The mesentery consists of two peritoneal folds that connect a portion of a bowel to the posterior abdominal wall. [7] The small and large bowel are thus suspended by peritoneal folds known as the small bowel mesentery and mesocolon or large bowel mesentery respectively. The infolding of the visceral peritoneum supports the abdominal viscera. The stomach, liver and spleen are suspended by the mesogastrium [8].This is a single complex mesenteric fold and is subdivided into lesser omentum (gastrohepatic and hepatoduodenal ligaments),greater omentum coronary ligaments, falciform ligament, gastrosplenic and splenorenal ligaments.
The peritoneal cavity (potential space in non-pathological states) consists of several communicating spaces. It is divided by the mesentery of the transverse mesocolon into supra and infra mesocolic spaces. The supramesocolic space is divided into left and right by the falciform ligament.
The right supramesocolic space can be subdivided into 3 spaces, which communicate freely with the right paracolic space [9]
-
(a).
Right subphrenic space - between the diaphragm and the right lobe of the liver
-
(b).
Subhepatic space - inferior to the right lobe of the liver, segment VI. The anterior compartment is bound inferiorly by the transverse colon and its mesentery. The posterior component (also referred to as the Morrison pouch) extends anterior to the right Gerota’s fascia.
-
(c).
Lesser sac: this is situated behind the stomach and to the left of the midline. It communicates with the peritoneal cavity through a narrow opening, the epiploic foramen (or Foramen of Winslow)
The left supramesocolic space is divided into:
(a) Perihepatic space: this space is further subdivided into anterior and posterior compartments. The posterior component (gastrohepatic recess) extends between the stomach, anterior to the gastrohepatic ligament (lesser omentum) and posterior to the left lobe of liver.
(b) Subphrenic space: also divided into anterior and posterior components. The anterior space freely communicates with the posterior subphrenic (perisplenic) space, which almost completely covers the splenic surface. [10].Inferior to the spleen, the phrenicocolic ligament (which attaches the left transverse mesocolon to the diaphragm) forms an important barrier separating the left paracolic gutter from the supramesocolic compartments. [11].
The subphrenic submesothelial lymphatics communicate with subpleural lymphatics and provide the majority of the lymphatic clearance from the peritoneal cavity. Consequently, the subphrenic peritoneal surfaces and the visceral peritoneal surface of the liver and spleen become major sites of dissemination of primary and secondary peritoneal malignancies. [12].
Inframesocolic Space
The inframesolic compartment is divided into two by the oblique orientation of the small bowel mesentery, where it attaches from the left upper quadrant at the ligament of Trietz to the right iliac fossa at the ileocaecal junction. [9] The larger left inframesocolic space freely communicates with the pelvis, except at the sigmoid mesocolon. The right infracolic space is bound inferiorly by the caecum. [9] Paracolic gutters represent peritoneal recesses lateral to the ascending and descending colon. Although both paracolic spaces freely communicate with the pelvis, it is only the larger right paracolic space that communicates with the right supramesocolic space. [9].
Overview of Various Imaging Modalities for Peritoneal Metastases
Radiography
Radiography has a limited role. It is useful in the initial evaluation of patients presenting with abdominal distention or pain abdomen, to exclude bowel perforation, bowel obstruction. It is also useful in the follow up of patients in the post-operative period.
Ultrasound
Ultrasound plays a limited role in the assessment of these pathologies but allows for the identification of ascites with or without peritoneal nodules. It may be used in the initial evaluation of a patient with abdominal pain or a pelvic mass. Sonography is very sensitive for the detection of ascitic fluid, pelvic lesions and are seen as hypoechoic or mixed echogenic lesions in the cul-de-sac or along the peritoneal surfaces of the uterus.
Ultrasound also plays a useful role in the assessment of abdominal collections, post-operative complications and intervention.
Computed Tomography (CT Scan)
It is the primary imaging modality of choice due to wide availability, robust techniques and protocols, good resolution and rapid acquisition times. CT scan is generally performed with both oral and intravenous contrast. Rectal contrast is used as required. The use of a negative contrast medium or a water density contrast is recommended for optimal visualisation of the bowel wall, serosa and peritoneum. The use of a positive oral contrast limits visualisation of surface deposits and limits identification of calcified serosal or peritoneal deposits. CT has a sensitivity of 25–100 % and a specificity of 78–100 % for detection of PM. [13–16] Tumor deposits of less than 5 mm, those at the root of mesentery, lesser omentum, left hemidiaphragm and serosal surface of bowel have a low sensitivity for detection by CT scan.(11–48 %). [13, 16–18] Some of the common CT findings in PM are
-
Thickening and enhancement of peritoneal reflections (especially if nodular)
-
Peritoneal nodules, plaques/sheets of soft-tissue that form small or large masses
-
Thickening, stranding and distortion of the mesentery
-
Stranding and thickening of the omentum (omental cake)
-
Thickening and nodularity of bowel wall
-
Various amounts of ascites and lymphadenopathy.
-
‘Scalloping’ of the liver surface due to surface/subcapsular deposits.
-
Calcification (if found prior to initiation of treatment is indicative of a mucin producing tumor. [19]
Specific characteristics of PM arising from different primary tumors are:
-
(a).
Mucinous Tumors( of ovarian or colonic origin) deposits show fluid densities
-
(b).
Carcinoid Tumours – show calcifications
-
(c).
Neuroendocrine Tumors – show hyper vascular deposits
-
(d).
Stellate pattern – seen in pancreatic, colonic, breast and ovarian tumors
-
(e).
Confluent adenopathy
CT has a low sensitivity for detection of metastases <1 cm in size and for bowel surface deposits.
Magnetic Resonance Imaging (MRI)
MRI inherently has excellent soft tissue contrast. More discrete changes can be determined by multiphasic image acquisition. MRI is comparable to CT in several aspects, in detecting deposits of more than 1 cm [18]. The use of fat suppression, delayed post contrast enhancement and water soluble enteric contrast have allowed detection sensitivities to surpass CT [20] Peritoneal enhancement more than liver enhancement is abnormal and is visualised due to the superior contrast resolution-a sign that may not be readily appreciated on MDCT. [18] MRI is more sensitive that CT for subcentimetric sized deposits and also in anatomically difficult sites (e.g. subphrenic, mesenteric and serosa of bowel) [21].These are seen best on fat suppressed T2 weighted and fat suppressed T1 weighted post contrast studies. [22].
However, with all the inherent advantages and superior contrast resolution, MRI is still less utilised as the primary modality. Long scanning times, various contraindications, susceptibility to motion artefacts, high cost, non-availability and well as dependence on interpreter evaluation have led to MRI being utilized less for evaluation of PM. Priest et al. demonstrated the use of Dynamic Contrast MRI ( DCE-MRI) in the detection of peritoneal metastases in advanced ovarian cancer, using 3 T-MRI [23].
Differentiation between scar tissue due to previous surgery and the identification of micro nodular peritoneal malignancies without tumor masses is challenging for imaging techniques mainly relying on morphology. A diffusion weighted MRI may be more useful in such cases.
Diffusion Weighted MRI (DWI)
When combined with conventional MRI, DWI has been shown to increase the sensitivity(90 %) and specificity( 95.5 %) [24] Site specific disease, particularly small deposits in mesentery, serosa of bowel, peri-hepatic and peri-pancreatic areas are better evaluated by DWI MRI [25] (Fig. 2).
Magnetic Resonance Spectroscopy (MRS)
MRS has been used by McLean et al. in the in-vivo evaluation of primary and metastatic ovarian cancer. [26] This modality uses the principle of evaluating choline metabolites. Further advances in MRI technology may help in evaluating the technique further.
Positron Emission Tomography (PET) Scan and PET-CT
PET-CT is used extensively in oncological imaging in staging and evaluation of primary malignancies and metastatic disease. 18(F) FDG - 18 F-2-deoxy-2-fluro-D-glucose, is the most commonly used radiotracer. PET-CT combines anatomical imaging (CT) with functional imaging (PET). This allows accurate localisation of disease processes thereby differentiating between physiological uptake from pathology. Features include well circumscribed nodules to diffuse uptake over peritoneal, serosal surfaces. False-negative results are seen in small tumour deposits, mucinous tumours of colon or ovary, signet-ring gastric cancers. False positive results are seen in inflammatory, infective and non- malignant conditions. Several studies combining PET alone, PET with unenhanced CT, PET with contrast-enhanced CT, have shown various sensitivities and specificities from 58 % to 100 % [27] . For ovarian cancer, both sensitivity and specificity in detecting PM is in the range of 78 %–97 %. [28–33] A recent meta-analysis of imaging modalities for recurrent ovarian cancer showed that PET-CT had the highest pooled sensitivity of 92 %,compared with PET,CT or MRI alone [34].
Classification of Tumors Involving the Peritoneum
Primary Peritoneal Tumors
Tumors arising from the peritoneum itself.
Primary peritoneal tumors can be classified according to their origin as:
-
a.
Mesothelial origin - Mesotheliomas
-
b.
Epithelial origin – Primary peritoneal carcinoma.
-
c.
Smooth muscle origin -Leiomyomatosis peritonealis disseminata
-
d.
Uncertain origin – Desmoplastic small cell tumours. [35]
Secondary tumors (Peritoneal Metastases) are tumors that spread to the peritoneum producing PM. Peritoneal metastases can virtually arise from any primary tumor, the commonest being colorectal, ovarian, pancreatic carcinomas and extra abdominal malignancies like breast and lung cancer.
Imaging features are varied and non-specific to a large extent. Considerable overlap exists with primary tumors, PM and other rare tumors like lymphomas and pseudomyxoma peritonei. Features include nodules either discrete or confluent masses, omental, mesenteric thickening, nodularity, enhancement, ascites and serosal deposits along the bowel wall. Lymph node involvement is also common. Mucinous deposits from colon or ovary may give the appearance of fluid densities. Calcified deposits can be seen in certain cancers. [36–39].
A spectrum of imaging appearances of peritoneal tumours exist, which depend, in part, on the histology, anatomical site and period at which the malignancy is imaged in its life cycle, influence of chemotherapy with certain tumors showing necrosis, cystic change or calcifications [27, 40]. A stellate pattern of tumour deposit has been described with secondaries from pancreatic, colonic, breast and ovarian cancers [41].
Primary Peritoneal Malignancies
These are generally rare compared to secondary tumors.
Peritoneal Mesothelioma (MPM)
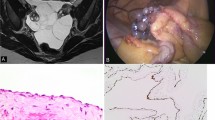
These are rare tumors that are similar to the pleural mesotheliomas and almost exclusively in males. There is a strong link to prior exposure to asbestos or abdominal radiotherapy. Imaging shows peritoneal nodules, masses, sheet-like infiltration, bowel wall thickening, mesenteric and omental thickening (omental cake) Associated asbestos-related changes with calcification or thickening of pleura or pleural masses are common. [42] There are 3 histopathologic subtypes of malignant mesothelioma, the commonest is the epithelioid variety found in 75–92 % of the cases, the others being the biphasic and sarcomatoid varieties seen in 8–22 % of the cases. The epithelioid variety has a much better prognosis as compared to the other varieties and is treated aggressively. The cytological and histologic features of MPM have been described in recent articles [43, 44]. The tumor arises from mesothelial cells lining the peritoneal cavity. Three broad subtypes of MPM have been described: epithelioid, mixed/biphasic, and sarcomatoid. Epithelioid MPM is by far the most commonly found subtype, diagnosed in approximately 75–92 % of cases; while mixed/biphasic comprises 8–22 % [44–46]. Sarcomatoid MPM is very rare. This distinction is important because biphasic and sarcomatoid MPM are extremely resistant to treatment and are associated with a poor prognosis. Benign Cystic mesothelioma (BCM) is a rare, low grade tumor that occurs in young and middle aged women with a predilection for peritoneal surfaces of the pelvis, around the urinary bladder, rectum and pouch of Douglas. It has as a favourable prognosis with tumor recurrence of 25 %–50 % after resection [47]. Imaging shows a multilocular, thin walled cystic lesion in the pelvis. These can be intra peritoneal or retroperitoneal. The cyst walls may enhance on CT and MRI.MRI confirms the cystic nature of the contents with low signal on T1 and high signal on T2 weighted images[47].
Primary Peritoneal Carcinoma (PPC)
PPC is a serous papillary tumour seen almost exclusively in women. These tumors present in post-menopausal women with multiple peritoneal masses and ascites. They share similar embryologic origin with ovarian serous tumours and are indistinguishable on imaging and histology with serous papillary tumours of the ovary [48] The abdominal peritoneum is preferentially involved. Peritoneal masses, nodules, omental thickening, ascites are seen. Calcification of the peritoneal nodules is seen in about 30 % of cases.
Criteria for diagnosis of PPC are:
-
Normal ovaries
-
Preferential involvement of extra-ovarian sites
-
Involvement of ovary that is limited to surface epithelium without stromal invasion, or with stromal invasion with tumour size of less than 5 mm [48, 49] (Fig. 3).
Desmoplastic Small Round Cell Tumors (DSRCT)
These are highly aggressive tumours, often seen in children and young adults. Lesions involve the peritoneum with metastasises to liver, lung, adrenals and lymph nodes. Imaging shows extensive peritoneal nodules or masses with no clear organ of origin. The masses may be calcified and show necrosis. [50].
Lymphomas
Secondary involvement of the peritoneum is far more common than primary peritoneal involvement and is associated with high grade non-Hodgkin’s lymphoma. Primary peritoneal lymphoma is also known as body cavity lymphoma or primary effusion lymphoma (PEL) is rare and seen in immuno-compromised individuals, commonly in patients with HIV. Imaging shows diffuse peritoneal masses, nodules, ascites and lymph node involvement [51] (Fig. 4).
MDCT transverse sections shows extensive peritoneal, omental lesions, and ascites.Large confluent adenopathy is seen in the retro peritoneum encasing the aorta, celiac axis ,superior mesenteric artery and their branches.CT sections of the Chest showed bilateral pleural collections. Patient was subsequently diagnosed to have high grade Non-Hodgkin’s Lymphoma on lymph node biopsy
Miscellaneous Tumours
Different types of Sarcoma, lymphomas, leiomyomatosis and gastrointestinal stromal tumours (GIST) can arise primarily from the peritoneum.
Secondary Peritoneal Malignancies (Peritoneal Metastases)
Ovarian and Gastrointestinal tract carcinomas account for the majority of peritoneal metastases [52].
71 % of ovarian, 17 % of gastric and 10 % of colonic tumours have peritoneal metastases at the time of presentation. [14] Tumors of breast, pancreas, biliary tract, lung, liver, appendix also may have peritoneal spread. The commonest extra-abdominal primary tumor producing PM is breast cancer.
Routes of Peritoneal Cancer Spread
There are four main pathways of peritoneal cancer spread.
1. Direct invasion,
2. Lymphatic metastases,
3. Intraperitoneal seeding,
4. Hematogenous spread.
Although tumours may have a preferential pathway for spread, many show spread through one or more routes. [53]
-
1.
Direct spread occurs with contiguous spread of tumor from one organ to another can occur directly via the serosa. Tumors of the stomach, colon and pancreas spread in that manner to contiguous and non-contiguous organs. [54]
-
2.
Along the flow of ascitic fluid (Redistribution phenomenon) This is characteristic of pseudomyxoma peritonei and ovarian cancer. [55, 56] The tumor cells follow the movement of intraperitoneal fluid. Gravity causes the fluid to collect in the pelvis. The negative pressure created by respiratory movement causes an upward movement of the fluid along the paracolic gutter to the subdiaphragmatic area from where it is redistributed via the falciform ligament to the lesser and greater omenta and over the bowel surfaces. The commonest sites of PM are the pelvis, the lower end of the small bowel mesentery, the right paracolic gutter, the undersurface of the diaphragm and the greater and lesser omenta. Besides, PM tend to involve the visceral peritoneum in greater volumes at 3 definite sites, where the bowel is anchored to the retroperitoneum. These are the recto sigmoid colon where it emerges from the pelvis (this site is also dependent and tends to be more often heavily involved), the region of the ileocecal valve and the region of the pylorus. Small bowel sparing is characteristic and is due to the constant peristaltic activity
-
3.
Lymphatic spread: Tumor can also spread directly from one noncontiguous organ to another through the sub peritoneal lymphatics along the ligaments, mesenteries and omenta. This pattern of spread accounts for a small percentage of PM and is seen is lymphomas especially non-Hodgkin’s lymphomas. [57]
-
4.
Hematogenous route: This route of spread is seen in both intra and extra- abdominal tumors and PM arising from breast cancer, lung cancer and melanoma spread by this route. [58]
Imaging Features and Patterns of Involvement of Peritoneal Surfaces
Perihepatic Spaces
The tumour deposits on the surface of the liver as well as along all its ligaments (ligamentum teres, ligamentum venosum, and falicform ligament), fissures and fossae (umbilical fissue and gall bladder fossa) and the spaces around the liver. Tumor from the right paracolic gutter spreads to the right subphrenic space and from the gall bladder fossa to the Morrison’s pouch. Some studies say that this region is better evaluated on MRI [18] Tumor deposits on the liver surface/capsule produce scalloping of the liver and/or direct parenchymal infiltration. [59].
Para Colic Gutters
The right paracolic gutter is prone to tumour deposits than the left. Tumor extends onto the serosa of the adjacent colon and can also infiltrate the bowel wall. This space promotes free movement of fluid from the pelvis to the supramesocolic space. [59].
Small Bowel Mesentery
The attachment of the mesentery directs the flow of ascitic fluid towards the terminal ileum and hence this region is more commonly involved compared to other regions of the bowel. Small bowel and its mesentery are involved early on in the high grade malignancies like colon, gastric and pancreatobiliary. Early changes appear just as a haziness of the mesentery whereas extensive involvement may produce masses. Carcinoid tumors are known to produce a desmoplastic reaction.
Mesocolon
The transverse and sigmoid mesocolon are common sites of involvement. The transverse colon is contiguous with the duodenocolic ligament on the right, with the phrenicocololic ligament on the left and with the small bowel mesentery centrally. The sigmoid mesocolon is a dependent site and accumulates tumour deposits.
Serosal deposits
These are probably the most difficult to detect on imaging and require adequate bowel distension with the use of negative or water-density oral contrast. The imaging findings range from focal nodules to confluent masses with or without bowel obstruction.
The lesser and greater omenta
These are common sites of involvement in both high grade and low grade malignancies. Again, the disease extent dictates the imaging findings ranging from subtle haziness to nodularity, confluent masses and omental cake formation. These lesions can be demonstrated by both CT and DWI MRI. [25]
Pelvis
The uterus, bladder and rectum are partially covered by the peritoneum. The recto vesical space in males and the rectovaginal space in females form the most dependent portions of the pelvic cavity and therefore are frequent sites of metastatic disease. The involvement is seen in both high grade and low grade malignancies. Contiguous involvement may occur in primary pelvic malignancies. These sites are well evaluated on a CT scan and a contrast enhanced MRI (Figs. 5 and 6).
Pseudomyxoma Peritonei (PMP)
This is a clinical entity which deserves a special mention due to its characteristic radiological appearances. PMP is mucinous ascites produced by an underlying mucinous tumor, arising from the appendix is majority of the cases. [60] It is characterized by recurrent, recalcitrant, voluminous mucinous ascites. Associated thickened and enhancing cake-like mesentery is noted. Lesions can sometimes show calcifications. Broadly, PMP is divided into high grade PMP and low grade PMP pathologically. [61–63] Low grade PMP does not invade the stroma and appears to spread along the peritoneal surfaces, characteristics that make it amenable to surgical debulking. It tends to have a relatively indolent or protracted clinical course, especially if debulking is successful. The second category is peritoneal mucinous carcinomatosis, which is characterized by invasive, high grade, moderately or poorly differentiated mucinous carcinoma with large extracellular pools of mucin. Imaging shows well circumscribed to ill-defined lesions along the surface of liver and spleen forming bi-convex deposits. Scalloping of the visceral surfaces of the intraperitoneal organs is an important diagnostic finding that helps differentiate pseudomyxoma from simple ascites [6].
Differentiating the true PMP from mucinous carcinomatosis at CT alone is difficult because their CT findings overlap despite their different pathologic features and clinical course. [6] Mucinous carcinomatosis tends to involve the chest more frequently with effusions or pleural masses and may also be accompanied by mesenteric or retroperitoneal lymphadenopathy, omental caking, and invasion into parenchymal organs [39].
PMP typically does not invade visceral organs or spread by lymphatic or haematogenous routes. Pleural extension of pseudomyxoma peritonei is rare and may be the consequence of cytoreductive surgery and subphrenic peritonectomy or congenital pleuroperitoneal communication [64] (Fig. 7).
Distinguishing Tuberculous Peritonitis from Peritoneal Metastases
Though tuberculosis is relatively less common in the developed world, it still is very common in India and abdominal tuberculosis is quite rampant. [65] There are three forms of tuberculous peritonitis: the “wet” (with ascites), the “dry” (peritoneal involvement without ascites) and the “fibroid” type (with profound omental thickening and extensive adhesion formation). [66, 67] TB peritonitis can have similar findings as ovarian cancer and is even more difficult to distinguish from it in immunocompromised patients. Analysis of ascitic fluid analysis is can be nonspecific. Ascitic fluid culture for tuberculosis is the confirmatory test for peritoneal tuberculosis.
The ADA in ascitic fluid shows good sensitivity and specificity whereas CA 125 lacks specificity. [68] Imaging/CT in TB shows smooth thickening and enhancing dirty omentum and dense ascites, necrotic lymphadenopathy, bowel lesions whereas imaging in carcinomatosis may show nodular peritoneal thickening and nodular omentum. [69] Based on clinical, laboratory findings it still may be inconclusive and a diagnostic laparoscopy or exploratory laparotomy may be required.
CT versus MRI for Determining the Extent of PM
A contrast enhanced CT scan of the thorax, abdomen and pelvis is the most common investigation for patients with PM. The limitations being inability to detect small deposits <1 cm in size and bowel surface deposits. [70, 71] Some studies have shown that MRI may be better in this regard. However it is subject to interpreter’s evaluation, requires a prolonged duration of study time and is not widely available as a CT scan. [72, 73] Both techniques provide morphological information enabling detection of peritoneal masses, nodules, ascites. For all imaging techniques, exact information regarding the extent and localization of the extent and localization of PC is mandatory [74]. Differentiation between scar tissue due to previous surgery and the identification of micro nodular pc without tumor masses is challenging for imaging techniques mainly relying on morphology. [75].
MRI versus PET-CT for Detecting the Extent of PM
MRI and PET-CT can both accurately predict the extent of PC [76] MRI provides excellent soft tissue contrast, more discrete changes of tissue involvement, multiphasic image acquisition. Dynamic contrast shows tissue vascularization information. MRI is robust regarding image quality. MRI is less robust regarding breathing or body motion artefacts resulting in reduced image quality with restricted diagnostic accuracy. MRI enables equal diagnostic yield in the case of good or excellent image quality compared with PET/CT, especially regarding small bowel involvement, but suffers from restricted image quality in patients with low compliance.
18f-fdg PET/CT provides metabolic information enabling the identification of malignant lesions. There is better diagnostic accuracy and inter-observer agreement as well as better correlation with surgical findings for PET/CT in comparison to MRI. Another asset of PET/CT is the coverage of the whole body providing information about the presence of distant metastases. In a comparative study, the positive predictive value for PM was 97/98 %,(MRI vs PET-CT), negative predictive value 73/84 %, sensitivity 87/93 %, specificity 92/96 %, and diagnostic accuracy 88/94 %.With high diagnostic accuracy for PC of both, MRI and PET/CT, PET/CT provides better diagnostic accuracy and especially better NPV. [76].
In spite of good results for MRI and PET/CT, the detection of diffuse micro nodular spread and small bowel involvement is challenging and to some extent still unsatisfactory. Macro nodular manifestations and involvement of parietal peritoneum can be identified with ease by both methods.
Multiphasic contrast enhanced MRI could be regarded as alternative in the case of contraindications for PET/CT or lack of availability of PET/CT.
Peritoneal Carcinomatosis Index (PCI)
Surgical PCI is based on complete exploration of the peritoneal cavity with histopathological sampling. According to the PCI, there are 13 peritoneal segments of which four are intestinal segments including upper and lower-jejunum as well as upper and lower-ileum. Each segment could be assigned 0–3(zero-three) points (with 0 - no lesion identified, 1- lesion up to 0.5 cm in maximum diameter, 2 - lesion exceeding 0.5 cm but not 5 cm in maximum diameter and 3 - lesion or confluent lesions exceeding 5 cm in maximum diameter). The resulting PCI score ranges between zero and 39. [77].
PCI is usually calculated during surgery.The PCI is determined during the complete abdominal and pelvic exploration that is conducted before the cytoreductive surgery. Lesion size/score is determined after complete lysis of all adhesions and complete inspection of all parietal and visceral peritoneal surfaces. The greatest diameter of tumour implants distributed on the peritoneal surfaces. Primary tumours or localized recurrences at the primary site that can be definitively removed are excluded from the lesion size assessment.
Accurate prediction of the extent of disease can be useful in selecting patients for CRS. [78] In patients with PM of colonic origin, those with a PCI ≤ 20 qualify for CRS and HIPEC. The PCI in patients with gastric cancer should be <10 or ≤15, in patients with pseudomyxoma peritonei arising from mucinous neoplasms and peritoneal mesothelioma there is no PCI cut off for selecting patients for surgery. [79–81].
However, preoperative CT-PCI does not correlate with the intra operative PCI. [82] In 52 patients with peritoneal carcinomatosis of colonic origin from 19 international centres the mean CT-PCI was 8.6 vs. 13.2.
ON pre-op CT, the location and quantity of mucinous adenocarcinoma within the peritoneal cavity can be determined. If the small bowel and its mesentery are involved with tumour, the chance of achieving complete cytoreduction is small.
For appendiceal mucinous neoplasms, Jacquet and co-workers reported two radiologic findings that predict incomplete cytoreduction (a) segmental obstruction of the small bowel and (b) tumour mass > 5 cm in diameter associated with the small bowel and its mesentery (exclusive of the distal ileum) - With these findings, patients had an 88 % probability of incomplete resection. Without such findings, the probability of complete resection was 92 %. [83].
Some other imaging findings that preclude a complete cytoreduction and are contra-indications for the procedure are
-
Extensive bowel resection that is likely to compromise the future quality of life e.g. 2 or more sites of segmental small bowel obstruction, patients requiring a total gastrectomy with a total colectomy
-
Involvement of pancreas head, bladder trigone, porta hepatis.
-
Massive or diffuse involvement of pleural space. [84]
In peritoneal mesothelioma, there are 2 crucial sites of disease involvement which preclude a complete CRS. Large tumours in the epigastric region may preclude a lesser omentectomy because of involvement of the right or left gastric vascular arcade. Removal of this site of disease often necessitates a total gastrectomy - a substantial undertaking, which, if not performed, will result in suboptimal cytoreduction. The second region is the small bowel, and extensive tumor in this area leads to suboptimal CRS which leads to morbidity and no benefit in survival. [85].
Conclusion
Imaging in patients of peritoneal malignancy (primary or secondary) is important in the detection, staging, management and follow-up. The presence of peritoneal carcinomatosis alters tumor staging, with implications in treatment choice and prognosis. Therefore, early diagnosis of peritoneal tumor seeding is fundamental.
MDCT remains the most robust imaging technique for assessment. MRI and PET/CT provide reliable detection of Peritoneal Carcinomatosis. Multiphasic contrast enhanced MRI could be regarded as alternative in the case of contraindications for PET/CT or lack of availability of PET/CT.
References
Meyers MA, Oliphant M, Berne AS, Feldberg MA (1987) The peritoneal ligaments and mesenteries: pathways of intraabdominal spread of disease. Radiology 163:593–604
Meyers MA (1973) Distribution of intra-abdominal malignant seeding: dependency on dynamics of flow of ascitic fluid. Am J Roentgenol Radium Therapy, Nucl Med 119:198206
Standring S. (2004) Peritoneum and peritoneal cavity. Grays anatomy: the anatomical basis of clinical. practice. 39th ed. Churchill Livingstone
Meyers MA (1973) Peritoneography: normal and pathologic anatomy. Am J Roentgenol Radium Therapy, Nucl Med 117:353–365
Meyers MA (2000) Dynamic radiology of the abdomen: normal and pathologic anatomy. Springer, New York, NY
Levy AD, Shaw JC, Sobin LH (2009) Secondary tumors and tumor like lesions of the peritoneal cavity: imaging features with pathologic correlation. Radio Graphics 29:347–373
DeMeo JH, Fulcher AS, Austin RF Jr (1995) Anatomic CT demonstration of the peritoneal spaces, ligaments, and mesenteries: normal and pathologic processes. Radiographics 15:75570
Coakley FV, Hricak H (1999) Imaging of peritoneal and mesenteric disease: key concepts for the clinical radiologist. Clin Radiol 54:56374
Rubenstein WA, Auh YH, Whalen JP, Kazam E (1983) The perihepatic spaces: computed tomographic and ultrasound imaging. Radiology 149:2319
Kneeland JB, Auh YH, Rubenstein WA, et al. (1987) Perirenal spaces: CT evidence for communication across the midline. Radiology 164:65764
Meyers MA (1970) Roentgen significance of the phrenicocolic ligament. Radiology 95:53945
Feldman GB, Knapp RC (1974) Lymphatic drainage of the peritoneal cavity and its significance in ovarian cancer. Am J Obstet Gynecol 119:991–994
Pannu HK, Horton KM, Fishman EK (2003) Thin section dual-phase multidetector-row computed tomography detection of peritoneal metastases in gynaecologic cancers. J Comput Assist Tomogr 27:33340
Coakley FV, Choi PH, Gougoutas CA, et al. (2002) Peritoneal metastases: detection with spiral CT in patients with ovarian cancer. Radiology 223:495–499
Franiel T, Diederichs G, Engelken F, Elgeti T, Rost J, Rogalla P (2009) Multi-detector CT in peritoneal carcinomatosis: diagnostic role of thin slices and multiplanar reconstructions. Abdom Imaging 34:4954
Marin D, Catalano C, Baski M, et al. (2010) 64-section multi-detector row CT in the preoperative diagnosis of peritoneal carcinomatosis: correlation with histopathological findings. Abdom Imaging 35:69470
deBree BE, Koops W, Kroger R, vanRuth S, Witkamp AJ, Zoetmulder FA (2004) Peritoneal carcinomatosis from colorectal or appendiceal origin: correlation of preoperative CT with intraoperative findings and evaluation of interobserver agreement. J Surg Oncol 86:6473
Low RN (2007) MR imaging of the peritoneal spread of malignancy. Abdom Imaging 32:26783
e Silva J. Abre, Magalhães M. J., Duarte H., Fernandes C., Ramos Alves S., Guimarães dos Santos A. (2013) M. V. P. G. Almeida;Porto/PT CT and PET-CT findings of peritoneal carcinomatosis ,ECR Educational Exhibit
Low RN, Barone RM, Lacey C, Sigeti JS, Alzate GD, Sebrechts CP (1997) Peritoneal tumor: MR imaging with dilute oral barium and intravenous gadolinium-containing contrast agents compared with unenhanced MR imaging and CT. Radiology 204:51320
Low RN (2009) Diffusion-weighted MR imaging for whole body metastatic disease and lymphadenopathy. Magn Reson Imaging Clin N Am 17:24561
Low RN, Sigeti JS (1994) MR imaging of peritoneal disease: comparison of contrast-enhanced fast multiplanar spoiled gradient-recalled and spin-echo imaging. AJR Am J Roentgenol 163:113140
Priest AN, Gill AB, Kataoka M, et al. (2010) Dynamic contrast-enhanced MRI in ovarian cancer: initial experience at 3 tesla in primary and metastatic disease. Magn Reson Med 63:10449
Fuji S, Matsusue E, Kanasaki Y, et al. (2008) Detection of peritoneal dissemination in gynecological malignancy: evaluation by diffusion-weighted MR imaging. Eur Radiol 18:1823
Low RN, Sebrechts CP, Barone RM, Muller W (2009) Diffusion weighted MRI of peritoneal tumours: comparison with conventional MRI and surgical and histopathologic findings: a feasibility study. AJR Am J Roentgenol 193:46170
McLean MA, Priest AN, Joubert I, et al. (2009) Metabolic characterization of primary and metastatic ovarian cancer by 1H-MRS in vivo at 3 T. Magn Reson Med 62:85561
Patel Chirag M., Sahdev Anju, and Reznek Rodney H. (2011) CT, MRI and PET imaging in peritoneal malignancy, Cancer Imaging 11, 123139
Turlakow A, Yeung HW, Salmon AS, Macapinlac HA, Larson SM. (2003) Peritoneal carcinomatosis: role of (18) F-FDG PET.J Nucl Med 44: 140712
Yoshida Y, Kurokawa T, Kawahara K, et al. (2004) Incremental benefits of FDG positron emission tomography over CT alone for the preoperative staging of ovarian cancer. AJR Am J Roentgenol 182:22733
Kitajima K, Murakami K, Yamasaki E, et al. (2008) Diagnostic accuracy of integrated FDG PET/contrast-enhanced CT in staging ovarian cancer: comparison with enhanced CT. Eur J Nucl Med Mol Imaging 35:191220
Kitajima K, Murakami K, Yamasaki E, et al. (2008) Performance of integrated FDG-PET/contrast-enhanced CT in the diagnosis of recurrent ovarian cancer: comparison with integrated FDG-PET/non-contrast-enhanced CT and enhanced CT. Eur J Nucl Med Mol Imaging 35:143948
Dirisamer A, Schima W, Heinisch M, et al. (2009) Detection of histologically proven peritoneal carcinomatosis with fused 18F-FDGPET/MDCT. Eur J Radiol 69:53641
Pannu HK, Cohade C, Bristow RE, Fishman EK, Wahl RL (2004) PETCT detection of abdominal recurrence of ovarian cancer: radiologic-surgical correlation. Abdom Imaging 29:398403
Gu P, Pan LL, Wu SQ, Sun L, Huang G. (2009) CA 125, PET alone,PET-CT, CT and MRI in diagnosing recurrent ovarian carcinoma: a systematic review and meta-analysis Eur J Radiol 71:16474.
Levy AD, Arnáiz J, Shaw JC, Sobin LH (2008) From the archives of the AFIP: primary peritoneal tumours: imaging features with pathologic correlation. Radiographics 28(2):583–607
Woodward PJ, Hosseinzadeh K, Saenger JS (2004) From the archives of the AFIP: radiologic staging of ovarian carcinoma with p pathologic correlation. Radiographics 24:22546
Matsuoka Y, Itai Y, Ohtomo K, Nishikawa J, Sasaki Y (1991) Calcification of peritoneal carcinomatosis from gastric carcinoma: a CT demonstration. Eur J Radiol 13:2078
Matsuoka Y, Ohtomo K, Itai Y, Nishikawa J, Yoshikawa K, Sasaki Y (1992) Pseudomyxoma peritonei with progressive calcifications: CT findings. Gastrointest Radiol 17:1618
.Mitchell DG, Hill MC, Hill S, Zaloudek C. (1986) Serous carcinoma of the ovary: CT identification of metastatic calcified implants. Radiology 158: 64952.
Amin Z, Reznek RH. (2009) Peritoneal metastases. In: Husband JE, Reznek RH, editors. Imaging in oncology. 3rd ed. InformaHealthcare p. 1094114
Kawamoto S, Urban BA, Fishman EK (1999) CT of epithelial ovarian tumors. Radiographics 19:S85102
Patel N, Taylor C, Levine E, Trupiano J, Geisinger K (2007) Cytomorphologic features of primary peritoneal mesothelioma in effusion, washing, and fine-needle aspiration biopsy specimens: examination of 49 cases at one institution, including post-intraperitoneal hyperthermic chemotherapy findings. Am J Clin Pathol 128:414–422
Husain AN, Colby TV, Ordóñez NG, Krausz T, Borczuk A, Cagle PT, Chirieac LR, Churg A, Galateau-Salle F, Gibbs AR, Gown AM, Hammar SP, Litzky LA, Roggli VL, Travis WD (2009) Wick Blackham and Levine E guidelines for pathologic diagnosis of malignant mesothelioma: a consensus statement from the international mesothelioma interest group. Arch Pathol Lab Med. 133:1317–1331.
Kannerstein M, Churg J (1977) Peritoneal mesothelioma. Hum Pathol 8:83–94
Cerruto D, Brun E, Chang D, Sugarbaker P (2006) Prognostic significance of histomorphologic parameters in diffuse malignant peritoneal mesothelioma. Arch Pathol Lab Med 130:1654–1661
Smith TR (1994) Malignant peritoneal mesothelioma: marked variability of CT findings. Abdom Imaging 19:279
van Ruth S, Bronkhorst MW, vanCoevorden F (2002) Zoetmulder FAPeritoneal benign cystic mesothelioma: a case report and review of the literature Eur J Surg Oncol 28:1925
Mok SC, Schorge JO, Welch WR, Hendricksen MR, Kempson RL (2003) Peritoneal tumours. In: Tavassoli FA, Devilee P (eds) Pathology and genetics of tumours of the breast and female genital organs. IARC, Lyon, pp. 197–202
Chiou SY, Sheu MH, Wang JH, Chang CY (2003) Peritoneal serous papillary carcinoma: a reappraisal of CT imaging features and literature review. Abdom Imaging 28:81519
Hayes-Jordan A, Anderson PM (2011) The diagnosis and management of desmoplastic small round cell tumor: a review. Curr Opin Oncol 23(4):385–389
Jain S, Palekar A, Monaco SE, Craig FE, Bejjani G, Pantanowitz L (2015) Human immunodeficiency virus-associated primary effusion lymphoma: an exceedingly rare entity in cerebrospinal fluid. Cyto Journal 12:22. doi:10.4103/1742-6413.168059
Walkey MM, Friedman AC, Sohotra P, Radecki PD (1988) CT manifestations of peritoneal carcinomatosis. AJR Am J Roentgenology 150:103541
Sheth S, Horton KM, Garland MR, Fishman EK (2003) Mesenteric neoplasms: CT appearances of primary and secondary tumors and differential diagnosis. Radiographics 23:457–473 . doi:10.1148/rg.232025081quiz 535-536
Oliphant M, Berne AS (1982) Computed tomography of the sub peritoneal space: demonstration of direct spread of intraabdominal disease. J Comput Assist Tomogr 6:1127–1137. doi:10.1097/00004728-198212000-00014
Sugarbaker PH (1994) Pseudomyxoma peritonei. A cancer whose biology is characterized by a redistribution phenomenon. Annals of Surgery 219(2):109–111
Lengyel E (2010) Ovarian cancer development and metastasis. The American Journal of Pathology 177(3):1053–1064. doi:10.2353/ajpath.2010.100105
Karaosmanoglu D, Karcaaltincaba M, Oguz B, Akata D, Ozmen M, Akhan O (2009) CT findings of lymphoma with peritoneal, omental and mesenteric involvement: peritoneal lymphomatosis. Eur J Radiol 71:313–317. doi:10.1016/j.ejrad.2008.04.012
Le O (2013) Patterns of peritoneal spread of tumor in the abdomen and pelvis. World Journal of Radiology 5(3):106–112. doi:10.4329/wjr.v5.i3.106
Patel CM, Sahdev A, Reznek RH (2011) CT, MRI and PET imaging in peritoneal malignancy. Cancer Imaging 11(1):123–139. doi:10.1102/1470-7330.2011.0016
Pai RK, Longacre TA (2007) Pseudomyxoma peritonei syndrome: classification of appendiceal mucinous tumours. In: Ceelen WP (ed) Peritoneal carcinomatosis:a multidisciplinary approach. Springer, New York, NY, pp. 71–107
Bradley RF, Stewart JH, Russell GB, Levine EA, Geisinger KR (2006) Pseudomyxoma peritonei of appendiceal origin: a clinicopathologic analysis of 101patients uniformly treated at a single institution, with literature review. Am J Surg Pathol 30:551–559
Carr NJ, Arends MJ, Deans GT, Sobin LH (2000) Adenocarcinoma of the appendix. In: Aaltonen LA, Hamilton SR (eds) World Health Organization classificationof tumours: pathology and genetics of tumours of the digestive system. IARC, Lyon, France, pp. 95–102
Ronnett BM, Zahn CM, Karman RJ, Kiss ME, Sugarbaker PH, Shmookler BM (1995) Disseminated peritoneal adenomucinosis and peritoneal mucinous carcinomatosis: a clinicopathologic analysis of 109 cases with emphasis on distinguishing pathologic features, site of origin, prognosis, and relationship to“pseudomyxoma peritonei. Am J Surg Pathol 19:1390–1408
Pestieau SR, Esquivel J, Sugarbaker PH (2000) Pleural extension of mucinous tumor in patients with pseudomyxoma peritonei syndrome. Ann Surg Oncol 7:199–203
Vagenas K, Stratis C, Spyropoulos C, Spiliotis J, Petrochilos J, Kourea H, Karavias D (2005) Peritoneal carcinomatosis versus peritoneal tuberculosis: a rare diagnostic dilemma in ovarian masses. Cancer Therapy Vol 3:489–494
Groutz A, Carmon E, Gat A (1998) Peritoneal tuberculosis versus advanced ovarian cancer: a diagnostic dilemma. Obstet Gynecol 91(5 Pt 2):868
Bilgin T, Karabay A, Dolar E, Develioglu OH (2001) Peritoneal tuberculosis with pelvic abdominal mass, ascites and elevated CA 125 mimicking advanced ovarian carcinoma: a series of 10 cases. Int J Gynecol Cancer 11:290–294
Gosein MA, Narinesingh D, Narayansingh GV, Bhim NA, Sylvester PA (2013) Peritoneal tuberculosis mimicking advanced ovarian carcinoma: an important differential diagnosis to consider. BMC Research Notes 6:88. doi:10.1186/1756-0500-6-88
Da Rocha EL, Pedrassa BC, Bormann RL, Kierszenbaum ML, Torres LR, D’Ippolito G (2015) Abdominal tuberculosis: a radiological review with emphasis on computed tomography and magnetic resonance imaging findings. Radiologia Brasileira 48(3):181–191. doi:10.1590/0100-3984.2013.1801
Verwaal VJ, Kusamura S, Baratti D, et al. (2008) The eligibility for local-regional treatment of peritoneal surface malignancy. J Surg Oncol 98:220–223
Yan TD, Morris DL, Kusamura S, et al. (2008) Preoperative investigations in the management of peritoneal surface malignancy with cytoreductive surgery and perioperative intraperitoneal chemotherapy. J Surg Oncol 98:224–227
Low RN (2016) Preoperative and surveillance MR imaging of patients undergoing cytoreductive surgery and heated intraperitoneal chemotherapy. J Gastrointes Oncol 2. doi:10.3978/j.issn.2078-6891.2015.11
Torkzad MR, Casta N, Bergman A, Ahlström H, Påhlman L, Mahteme H. (2015) Comparison between MRI and CT in prediction of peritoneal carcinomatosis index (PCI) in patients undergoing cytoreductive surgery in relation to the experience of the radiologist. J Surg Oncol 111(6):746–51. doi: 10.1002/jso.23878.
Dromain C, Leboulleux S, Auperin A, et al. (2008) Staging of peritoneal carcinomatosis: enhanced CT vs. PET/CT. Abdom Imaging 33:87–93
Iafrate F, Ciolina M, Sammartino P, et al. (2011) Peritoneal carcinomatosis:imaging with 64-MDCT and 3 T MRI with diffusion weighted imaging. Abdom Imaging
Bernhard Daniel Klumpp, Schwenzer Nina, Aschoff Philip, Miller Stephan, Kramer Ulrich, Claussen ClausD., Bruecher Bjoern, Koenigsrainer Alfred, fannenberg Christina P (2012) Preoperative assessment of peritoneal carcinomatosis: intraindividual comparison of 18F-FDG PET/CT and MRI,Abdom Imaging doi: 10.1007/s00261-012-9881-7
Jacquet P, Sugarbaker PH (1996) Clinical research methodologies in diagnosis and staging of patients with peritoneal carcinomatosis. Cancer Treat Res 82:359–374
Jacquet P, Jelinek JS, Steves MA, Sugarbaker PH (1993) Evaluation of computed tomography in patients with peritoneal carcinomatosis.Cancer 72:1631–1636
Goéré D, Souadka A, Faron M, Cloutier AS, Viana B, Honoré C, Dumont F, Elias D (2015) Extent of colorectal peritoneal carcinomatosis: attempt to define a threshold above which HIPEC does not offer survival benefit: a comparative study. Ann Surg Oncol 22(9):2958–2964
Coccolini F, Catena F, Glehen O, Yonemura Y, Sugarbaker PH, Piso P, Montori G, Ansaloni L (2015) Complete versus incomplete cytoreduction in peritoneal carcinosis from gastric cancer, with consideration to PCI cut-off. Systematic review and meta-analysis. Eur J Surg Oncol 41(7):911–919
Chua TC, Moran BJ, Sugarbaker PH, Levine EA, Glehen O, Gilly FN, Baratti D, Deraco M, Elias D, Sardi A, Liauw W, Yan TD, Barrios P, Gómez Portilla A, de Hingh IH, Ceelen WP, Pelz JO, Piso P, González-Moreno S, Van Der Speeten K, Morris DL (2012) Early- and long-term outcome data of patients with pseudomyxoma peritonei from appendiceal origin treated by a strategy of cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. J Clin Oncol 30(20):2449–2456
Esquivel J, Elias D, Baratti D, Kusamura S, Deraco M (2008) Consensus statement on the loco regional treatment of colorectal cancer with peritoneal dissemination. J Surg Oncol 98:263
Jacquet P, Jelinek JS, Chang D et al. (1995) Abdominal computed tomographic scan in the selection of patients with mucinous peritoneal carcinomatosis for cytoreductive surgery Journal of the American College of Surgeons 181: 530–538.
Cotte E, Passot G, Gilly F-N, Glehen O (2010) Selection of patients and staging of peritoneal surface malignancies. World Journal of Gastrointestinal Oncology 2(1):31–35. doi:10.4251/wjgo.v2.i1.31
Yan TD, Haveric N, Carmignani P, Chang D, Sugarbaker PH (2005) Abdominal computed tomography scans in the selection of patients with malignant peritoneal mesothelioma for comprehensive treatment with cytoreductive surgery and perioperative intraperitoneal chemotherapy. Cancer 15:839–849. doi:10.1002/cncr.20836
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Krishnamurthy, S., Balasubramaniam, R. Role of Imaging in Peritoneal Surface Malignancies. Indian J Surg Oncol 7, 441–452 (2016). https://doi.org/10.1007/s13193-016-0539-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13193-016-0539-8