Abstract
Background
In order to investigate whether 1-mm thin slices and multiplanar reconstructions (MPRs) of multi-detector computed tomography (CT) datasets interpreted in addition to isotropic 5-mm thick slices in one session improve the detection of peritoneal carcinomatosis.
Methods
The abdominal CT datasets of 44 patients with histologically proven tumors of the abdomen or pelvis were retrospectively evaluated for peritoneal carcinomatosis by four radiologists with variable experience (radiologist 1: ≥10 years, radiologists 2 and 3: 1.5 years, radiologist 4: 0.5 years). In three successive steps, the radiologists evaluated first the axial 5-mm slices, second the 1-mm slices, and third the MPRs and rated their diagnostic confidence.
Results
Specificity was nearly unchanged for all the four radiologists. Sensitivity improved for the most experienced and the least experienced radiologists and was unchanged for the two readers with intermediate skills. Except for the third step of radiologist 4, no statistically significant differences in diagnostic performance were detected. The diagnostic confidence of all the four readers benefited to variable degrees from interpretation of the 1-mm slices and MPRs.
Conclusions
While 5-mm slices are sufficient for the detection of peritoneal carcinomatosis, 1-mm slices and MPRs can improve sensitivity and diagnostic confidence.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
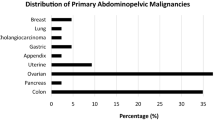
Peritoneal carcinomatosis occurs in a wide range of malignant tumors such as ovarian, gastrointestinal, endometrial, urothelial, and breast cancer as well as malignant melanoma [1–4]. Seeding of the peritoneal cavity occurs as a result of circulation of peritoneal fluid after the metastatic spread of a primary tumor [5–7]. Peritoneal carcinomatosis can manifest as nodular or plaque-like lesions, ascites, or the tumorous infiltration of mesenteric fatty tissue [8]. Patients with peritoneal implants have an unfavorable prognosis. In a review of studies including patients with different primary tumors, mean survival was 1–8 months in patients with malignant ascites [9] and 5–32 months in patients with peritoneal metastases from colorectal cancer [10]. Therefore, reliable confirmation or the exclusion of peritoneal carcinomatosis is important for the individual patient’s prognosis and therapeutic management.
Computed tomography (CT) is the most widely used imaging modality for diagnosing peritoneal carcinomatosis. Studies including patients with different primary tumors reported sensitivities ranging from 41% to 79% and a specificity of up to 100% [3, 11–13]. For detection of peritoneal carcinomatosis in patients with ovarian cancer, sensitivity was found to be as high as 85% to 93% [14, 15]. These results were obtained with single-row CT scanners. Multidetector-row CT (MDCT) technology shortens the examination time and allows the generation of thin slices with subsequent multiplanar reconstruction (MPR). This new CT technique has been shown to improve the evaluation of local tumor extent and metastatic spread in patients with various malignancies [16–19]. MPRs of axial thin slices can be used to evaluate the abdominal and pelvic organs and compartments in several planes and may therefore improve the detection of peritoneal implants [20]. Only little data are available on the use of MDCT in diagnosing peritoneal carcinomatosis. Therefore, we conducted a study to investigate whether the additional interpretation of thin slices (1 mm) and MPRs improves the detection of peritoneal carcinomatosis and radiologists’ diagnostic confidence compared to the interpretation of isotropic 5-mm thick slices alone.
Patients and methods
Patients
The study was approved by the local ethics committee. A total of 44 patients with abdominal or pelvic cancer were retrospectively included in the study.
Twenty-two patients (15 women, 7 men) had peritoneal carcinomatosis. There were seven patients with ovarian cancer, five with colon cancer, five with gastric cancer, three with pancreatic cancer, and two with rectal cancer. The patients had a median age of 64 years (range 32–84 years) at the time of the CT examination. The median interval between CT and histologic confirmation of peritoneal carcinomatosis was 6 days (range 1–30 days). The tissue for histology was obtained by surgery in 16 cases: ascites puncture in 4, and biopsy in 2 instances.
The 22 patients in the control group (6 women, 16 men) had colon cancer in 15 cases, rectal cancer in 4, gastric cancer in 2, and pancreatic cancer in 1 case. Median age at the time of CT was 66 years (range 41–86 years). The median interval between CT and tissue acquisition for histology was 6 days (range 1–30 days). The absence of peritoneal carcinomatosis was confirmed by surgery and histologic workup in all cases.
CT protocol
All patients underwent CT scanning after the injection of 120 mL Ultravist 370 (Bayer Schering Pharma, Berlin, Germany) at a flow rate of 2.5 mL/s into an antecutibal vein followed by 30 mL saline. Twelve patients of the peritoneal carcinomatosis group and four patients of the control group additionally received an oral contrast agent. The CT scan extending from above the diaphragm to below the pubic bone was started with a delay of 60 s.
All axial source images were obtained on 16-detector row scanners (17 patients with peritoneal carcinomatosis and 21 patients of the control group) or 4-detector row scanners (4 patients with peritoneal carcinomatosis and 1 control patient) (Aquilion 16/Aquilion 4, Toshiba, Otawara, Japan). Collimation was 1 mm on both scanners with a pitch of 0.938 for 16-detector row CT and 1.375 for 4-detector row CT. All CT examinations were performed at 120 kV without gantry tilting and a maximum tube current of 200 mA to achieve a predetermined signal-to-noise ratio. The source datasets served to generate axial thick slices with a thickness of 5.0 mm and 20% overlapping reconstruction. In addition, axial thin slices with a thickness of 1.0 mm and 20% overlap were generated as well as coronal and sagittal MPRs with a slice thickness of 5.0 mm without overlap. The data were electronically transferred to the archive and stored (SIENET MagicStore VE42A, Siemens, Erlangen, Germany).
Radiological analysis
The axial slices and coronal and sagittal MPRs were evaluated by a radiologist with over 10 years of experience in interpreting abdominal CT (radiologist 1), two radiologists with 1.5 years of experience in interpreting abdominal CT (radiologists 2 and 3), and one radiologist with 0.5 years of experience in this area (radiologist 4). The CT data of all patients including axial 5-mm thick slices, axial 1-mm thin slices, and MPRs were evaluated for signs of peritoneal carcinomatosis in a single session starting with the axial 5-mm slices. Each radiologist made a diagnosis regarding the presence/absence of peritoneal carcinomatosis and rated his diagnostic confidence on a 10-point scale (1 = very unsure to 10 = definitely sure). The second step, the evaluation of the axial 1-mm slices using the same procedure, followed immediately after the analysis of the 5-mm slices. In the third step, the radiologists interpreted the coronal and sagittal MPRs. Once a step was completed, the images were no longer available in any of the subsequent readings. The correct diagnoses were disclosed to the readers after completing the evaluation of the CT data of all patients.
The readers knew that all patients had an abdominal or pelvic tumor that might potentially cause peritoneal carcinomatosis but had no information regarding the kind of tumor and its localization before interpreting the CT images.
All radiologists interpreted the images on identical consoles using the ViewForum R4.2 V1L2 software (Philips Medical Systems Nederlands B.V., DA Best, Netherlands).
Statistical analysis
Statistical analysis was done using SPSS for Windows, version 13.0. Sensitivity, negative predictive value (NPV), specificity, and positive predictive value (PPV) were determined for each radiologist and each of the three reading steps. The Wilcoxon test for paired samples was used to compare the diagnoses made on the basis of the 5-mm axial thick slices, 1-mm axial thin slices, and coronal/sagittal reconstructions and the diagnostic confidence ratings. P-values ≤ 0.05 were considered to indicate statistical significance.
Interobserver agreement was calculated using the kappa test with the following degrees of agreement: <0.2 poor, 0.21–0.40 adequate, 0.41–0.60 moderate, 0.61–0.80 good, and 0.81–1.00 excellent [21].
Medians, 25% and 75% quantiles, minimum and maximum values were calculated for the diagnostic confidence scores for each radiologist and diagnostic step.
Results
Radiologist 1 improved sensitivity and NPV for the detection of peritoneal carcinomatosis to 96% by interpretation of the axial 1-mm thin slices (second step) and to 100% by interpretation of the MPRs (third step) (Table 1). Specificity and PPV were fairly constant ranging from 95% to 96% in all the three readings. The differences in diagnostic performance between the three steps were statistically not significant (P = 0.157, P = 0.317).
Radiologists 2 and 3 with the same level of experience did not achieve improvement in sensitivity, specificity, PPV, or NPV in the second or third step (Table 1). These parameters were nearly constant in all the three readings except for a decrease in sensitivity from 91% to 86% and NPV from 91% to 88% in the MPR reading for radiologist 2. The differences in diagnostic performance between the second and third steps were not significant (P = 0.317).
Radiologist 4 increased sensitivity and NPV from 64% to 82% and 71% to 83%, respectively, in the MPR reading (Table 1), while specificity decreased from 91% to 86% and PPV from 88% to 86%. The difference in diagnostic performance between interpretation of the MPRs and 1-mm thin slices was statistically significant (P = 0.025).
Interobserver agreement between radiologists 1 and 2/3 was good with κ values ranging between 0.63 and 0.78 for the three steps (Table 2), while agreement between radiologists 1 and 4 was moderate for the 5-mm slices (κ = 0.53) and 1-mm slices (κ = 0.55) and good only for the MPRs (κ = 0.64). Interobserver agreement between radiologists 2 and 3 with the same level of experience was excellent (κ-values of 0.86 to 0.91). Interobserver agreement between radiologists 2 and 4 and radiologists 3 and 4 was moderate with κ-values ranging between 0.62 and 0.68.
For radiologist 1, diagnostic confidence increased significantly between the first and second steps (P = 0.005) and reached a maximum score of 10 but did not change significantly between the second and third steps (P = 0.20) (Table 3 and Fig. 1). Diagnostic confidence for radiologist 2 increased significantly between the first and second steps and between the second and third steps (P = 0.017, P ≤ 0.001), while there were no statistically significant changes for radiologist 3 (P = 0.102, P = 0.680). Radiologist 4 had no statistically significant change in diagnostic confidence between the first and second steps (P = 0.770) but a statistically significant increase between the second and third steps (P = 0.043).
Discussion
Published sensitivities for the detection of peritoneal carcinomatosis by CT range from 41% to 93% and the specificities from 78% to 96% [3, 13–15]. The highest sensitivities of 85% to 93% were achieved in patients with ovarian cancer [14, 15] compared to sensitivities of 41% to 79% in patients with colorectal or appendix cancer [3, 13]. All studies just quoted used spiral or conventional CT with an axial slice thickness of 5–10 mm. In our study, sensitivity for the interpretation of the 5-mm axial sections ranged from 82% to 91% for radiologists 1 to 3. This is intermediate between the reported sensitivities for ovarian cancer and the colorectal/appendix cancer and reflects the fact that our patient population included patients with different primary abdominal and pelvic tumors. The most experienced radiologist (radiologist 1) had a sensitivity of 96% when looking at the 1-mm thin slices and 100% when looking at the reconstructions. Therefore, MDCT with the option of generating 1-mm thin slices with isotropic voxels and MPRs appears to be superior in detecting peritoneal carcinomatosis when the images are interpreted by a highly experienced radiologist compared with the performance reported for spiral and conventional CT with a slice thickness of 5–10 mm. Radiologists 2 and 3 with identical levels of training showed no or only slightly improved sensitivity, and the benefit of 1-mm thin slices and MPRs is thus not immediately apparent for this group of less experienced readers. However, at least one of the two readers (radiologist 2) definitely benefited by a statistically significant gain in diagnostic confidence when interpreting the 1-mm slices and MPRs. The least experienced reader (radiologist 4) mainly benefited from the interpretation of the MPRs, which resulted in an increase in sensitivity from 64% to 82% and a statistically significant increase in diagnostic confidence. Thus, the generation of 1-mm slices and above all MPRs appears to be beneficial for this group of radiologists as well.
A study investigating diagnostic accuracy in relation to the size of peritoneal implants showed that sensitivity dropped as low as 25% to 50% for implants smaller than 1 cm [14]. Since pathology reports do not provide detailed information on each individual implant, we could not perform a comprehensive analysis of cases with implants <1 cm. Therefore, studies including larger numbers of cases with proven implants <1 cm are needed for a final appraisal of both techniques regarding the detection of small peritoneal implants.
In agreement with other studies, we found a high specificity and PPV suggesting that the features of peritoneal carcinomatosis are highly specific. Nevertheless, there are some conditions that can mimic peritoneal carcinomatosis. These are tuberculosis, mesenteritis, disseminated peritoneal leiomyomatosis, and extramedullary hematopoiesis [22–26].
We think that there are several reasons why the only statistically significant improvement of diagnostic performance was seen for the least experienced radiologist and only after the interpretation of the MPRs. The first reason is that there are always several peritoneal implants and typically several different signs of peritoneal carcinomatosis and that therefore the correct diagnosis could be made even when the radiologist overlooked one implant or one sign (Fig. 2A, B). The second reason is that 5-mm slices through the abdomen and pelvis are detailed enough for an adequate diagnosis of peritoneal carcinomatosis in most cases. A possible third reason is the relatively small number of cases investigated. The most experienced reader (radiologist 1) who had three false-negative diagnoses made correct diagnoses when looking at the 1-mm thin slices and MPRs in all three instances, thereby increasing sensitivity and NPV to 100%. Nevertheless, the improvement in diagnostic performance was not statistically significant.
In our study, we included patients with peritoneal carcinomatosis regardless of its extent. Our study population thus represents a good cross-section of patients with peritoneal carcinomatosis. This also means that there were many clear-cut cases and the radiologists already assigned the highest ratings to their diagnostic confidence when looking at the 5-mm slices. Thus, radiologists 1 to 3 often did not need the extra spatial information provided by the MPRs. Only the least experienced radiologist (radiologist 4) benefited from the MPRs by markedly improving his sensitivity while specificity remained nearly constant.
A limitation of our study is the lack of correlation of the peritoneal implants identified by the radiologists with the histopathologic gold standard. This is due to the retrospective design of our study but also the fact that it would be very time-consuming to establish the histologic gold standard with exact localization of all peritoneal implants.
In summary, our results show that 5-mm thin slices acquired with multi-detector CT are sufficient for diagnosis of peritoneal carcinomatosis when the images are interpreted by radiologists with at least 1.5 years of experience in abdominal CT. Additional 1-mm thin slices and MPRs further improve sensitivity and diagnostic confidence when a highly experienced radiologist interprets the data. A radiologist with little experience benefits from extra looking at MPRs, which results in similar sensitivities and NPVs as for radiologists with 1.5 years of experience.
References
Coakley FV, Hricak H (1999) Imaging of peritoneal and mesenteric disease: key concepts for the clinical radiologist. Clin Radiol 54:563–574
Dähnert W (2003) Gastrointestinal tract. In: Dähnert W (ed) Radiology review manual. Philadelphia: Lippincott Williams & Wilkins, p 852
de Bree E, Koops W, Kroger R, van Ruth S, Witkamp AJ, Zoetmulder FA. (2004) Peritoneal carcinomatosis from colorectal or appendiceal origin: correlation of preoperative CT with intraoperative findings and evaluation of interobserver agreement. J Surg Oncol;86:64–73
Scaglione M, Pinto A, Romano S et al (2005) Using multidetector row computed tomography to diagnose and stage pancreatic carcinoma: the problems and the possibilities. JOP 6:1–5
Meyers MA (1973) Distribution of intra-abdominal malignant seeding: dependency on dynamics of flow of ascitic fluid. Am J Roentgenol Radium Ther Nucl Med 119:198–206
Meyers MA (1981) Intraperitoneal spread of malignancies and its effect on the bowel. Clin Radiol 32:129–146
Meyers MA (1994) Intraperitoneal spread of malignancies. In: Meyers MA (ed) Dynamic radiology of the abdomen. New York Berlin Heidelberg London Paris Tokyo: Springer Verlag, pp 115–218
Raptopoulos V, Gourtsoyiannis N (2001) Peritoneal carcinomatosis. Eur Radiol 11:2195–2206
Baker AWJ (1993) Treatment of malignant ascites. In: De Vita VT Jr, Hellmann S, Rosenberg SA (eds) Cancer: principles and practice of oncology. Philadelphia: Lippincott, pp 2255–2261
Koppe MJ, Boerman OC, Oyen WJ, Bleichrodt RP (2006) Peritoneal carcinomatosis of colorectal origin: incidence and current treatment strategies. Ann Surg 243:212–222
Buy JN, Moss AA, Ghossain MA et al (1988) Peritoneal implants from ovarian tumors: CT findings. Radiology 169:691–694
Halvorsen RA Jr, Panushka C, Oakley GJ, Letourneau JG, Adcock LL (1991) Intraperitoneal contrast material improves the CT detection of peritoneal metastases. AJR 157:37–40
Jacquet P, Jelinek JS, Steves MA, Sugarbaker PH (1993) Evaluation of computed tomography in patients with peritoneal carcinomatosis. Cancer 72:1631–1636
Coakley FV, Choi PH, Gougoutas CA et al (2002) Peritoneal metastases: detection with spiral CT in patients with ovarian cancer. Radiology 223:495–499
Fultz PJ, Jacobs CV, Hall WJ et al (1999) Ovarian cancer: comparison of observer performance for four methods of interpreting CT scans. Radiology 212:401–410
Kulinna C, Eibel R, Matzek W et al (2004) Staging of rectal cancer: diagnostic potential of multiplanar reconstructions with MDCT. AJR 183:421–427
Smith SL, Rajan PS (2004) Imaging of pancreatic adenocarcinoma with emphasis on multidetector CT. Clin Radiol 59:26–38
Schreyer AG, Scheibl K, Zorger N et al (2005) Detection rate and efficiency of lymph node assessment with axial and coronal image reading based on 16 row multislice CT of the neck. Rofo 177:1430–1435
Shimizu K, Ito K, Matsunaga N, Shimizu A, Kawakami Y (2005) Diagnosis of gastric cancer with MDCT using the water-filling method and multiplanar reconstruction: CT-histologic correlation. AJR Am J Roentgenol 185:1152–1158
Pannu HK, Bristow RE, Montz FJ, Fishman EK (2003) Multidetector CT of peritoneal carcinomatosis from ovarian cancer. Radiographics 23:687–701
Landis JR, Koch GG (1977) An application of hierarchical kappa-type statistics in the assessment of majority agreement among multiple observers. Biometrics 33:363–374
Ha HK, Jung JI, Lee MS et al (1996) CT differentiation of tuberculous peritonitis and peritoneal carcinomatosis. AJR 167:743–748
Rodriguez E, Pombo F (1996) Peritoneal tuberculosis versus peritoneal carcinomatosis: distinction based on CT findings. J Comput Assist Tomogr 20:269–272
Fujiyoshi F, Ichinari N, Kajiya Y et al (1997) Retractile mesenteritis: small-bowel radiography, CT, and MR imaging. AJR 169:791–793
Papadatos D, Taourel P, Bret PM (1996) CT of leiomyomatosis peritonealis disseminata mimicking peritoneal carcinomatosis. AJR 167:475–476
Scott WW Jr, Fishman EK (1990) Extramedullary hematopoiesis mimicking the appearance of carcinomatosis or peritoneal mesothelioma: computed tomography demonstration. Gastrointest Radiol 15:82–83
Acknowledgment
The authors thank Bettina Herwig for translating the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Franiel, T., Diederichs, G., Engelken, F. et al. Multi-detector CT in peritoneal carcinomatosis: diagnostic role of thin slices and multiplanar reconstructions. Abdom Imaging 34, 49–54 (2009). https://doi.org/10.1007/s00261-008-9372-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-008-9372-z