Abstract
Objective
Adult granulosa cell tumors (AGCTs) account for less than 5 % of all ovarian malignancies, whereas the majority (95 %) occurs after the age of 30 (adult-type) and present at an early stage. Aim of this study is to identify clinical and pathological risk factors for recurrence in early stage AGCTs.
Methods
Retrospective review of patients with AGCT of the ovary, treated surgically at our institution from 1996 to 2011. Clinical, pathological and follow-up data were collected. Systematic analysis was performed to determine variables for predicting recurrence.
Results
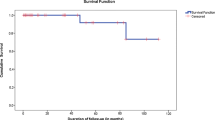
In total, 43 patients were identified. The mean age at diagnosis was 54.3 years and 65.1 % of them were postmenopausal. All patients underwent surgical staging and intraoperative rupture of the tumor occurred in four of them (9.3 %). The majority of the cases were staged as IA (72.1 %) while 10 (23.3 %) were staged as IC and only two patients as IIB. Mitotic index was 4 or more in 34.9 % of the patients and nuclear atypia was moderate to high in 60.5 %. During follow-up period (mean 9.2 years), recurrence occurred in three patients (7 %) with no deaths recorded so far. The cumulative recurrence free rate for the first 2 years was 97.6 % (SE = 2.4 %), for 5 years 94.9 % (SE = 3.5 %) and for 10 years 91.0 % (SE = 5.1 %).Tumor size, stage and mitotic index proved to be independent predictors for recurrence at the multivariate analysis.
Conclusions
Recurrence in early stage AGCT seems to be associated with stage, tumor size and mitotic index. All the above should be taken into consideration when tailored postoperative management is planned.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adult granulosa cell tumors (AGCT) form a part of sex cord–stromal ovarian malignancies. AGCT account for approximately less than 5 % of all ovarian tumors and can be classified into adult (95 %), and juvenile (5 %) types depending on histological findings [1]. AGCTs are usually diagnosed in menopausal or postmenopausal women (average age 50–54) and are thought to be tumors of low malignant potential, following a benign course, with only a small percentage showing aggressive behavior [1].
Although there is no consensus on the pathogenesis of these tumors, most investigators believe they originate from early ovarian mesenchyma as they are composed of granulosa cells, theca cells and fibroblasts in varying degrees [2, 8]. The reported incidence rate in the Unites States is 0.99 person per 100,000 and in Europe ranges from 0.4 to 1.7 person per 100,000. Since AGCT is so rare, limited data is available regarding predisposing risk or prognostic factors [3, 4, 8].
Surgery is the mainstay of treatment for patients with AGCT both in the primary and the recurrent setting. Adjuvant chemotherapy and/or radiotherapy are reserved for patients diagnosed with advanced disease after surgical staging, and for patients with unresectable recurrent tumor. Recurrences develop in 15–25 % of patients in early stage and in 50–70 % in advanced stages, often after a long disease free interval [23]. Advanced stage seems to be an important prognostic factor, while other variables, such as age, tumor size and histological characteristics might also play a significant prognostic role [6].
In this study, we aimed to identify prognostic factors related to recurrence and overall survival in early stage adult granulosa cell tumors of the ovary, by analyzing clinical data, treatment method and pathological features of patients with AGCT treated in our hospital. We decided to exclude the advanced stages as these were not as common, and for that reason would not provide us with any important clinical findings.
Materials and methods
This is a retrospective single center cohort study of all patients with early stage (I and II) AGCT diagnosed and treated at the 1st Department of Obstetrics and Gynecology, University of Athens, Alexandra Hospital, Greece, from January 1996 to December 2011. A review of their medical records was performed and clinico-pathological parameters, such as age, menopausal status, presenting symptoms, examination findings, radiologic and laboratory workup, operative findings, procedures performed, cytoreduction rate, postoperative treatment and follow-up were collected. The patients were staged according to FIGO 2009 [10] and the histopathological classification was according to WHO [11]. The study was registered within the audit department of our institution.
Quantitative variables were expressed as mean values (SD: standard deviation) or as median values (IQR: interquartile range). Qualitative variables are expressed as absolute and relative frequencies. The prognostic value of age, menopause, U/S finding, CA-125, tumor size, intraoperative rupture of tumor, stage, pelvic lymphadenectomy, surgical staging, nuclear atypia, mitotic index and endometrial histology for recurrence was first assessed by univariate Cox regression analysis [1]. Multiple Cox proportional-hazards analysis in a stepwise method (p for removal was set at 0.1 and p for entry was set at 0.5) was used to find independent predictors associated with recurrence. Hazard ratios with 95 % confidence intervals are presented from the results of Cox regression analysis. The assumption of proportional hazards was evaluated by testing for interaction with a continuous time variable. Kaplan–Meier survival estimates for recurrence were graphed over the follow-up period. Life table analyses were used to calculate cumulative recurrence free rates (standard errors) for specific time intervals. Using receiver operating characteristic (ROC) curve, we determined the optimal cutoff of tumor size for the prediction of recurrence. Sensitivity and specificity were calculated for the optimal cutoff as well. All reported p values are two-tailed. Statistical significance was set at p < 0.05 and analyses were conducted using SPSS statistical software (ver 19.0).
Results
A total of 43 women with a mean age of 54.3 years (SD = 17.4 years) were included in the study. Sample demographics and clinical characteristics are presented in Table 1. Among the patients, 64.6 % were postmenopausal. In all cases, a computed tomography was performed preoperatively and showed a mainly cystic ovarian tumor in 45.8 % of cases, while the ovarian mass was hugely solid in 22.9 % of cases. The mean diameter of the ovarian mass was 10.3 cm (SD = 6.5).
Serum tumor marker CA-125 was studied in all patients and was measured preoperatively. It was found to be within normal levels and the average was 14.7 IU/ml (range 11.0–38.0 IU/ml).
The primary treatment was surgery in all cases. In postmenopausal women or women who had completed their childbearing, surgery included at least total abdominal hysterectomy and bilateral salpingo-oophorectomy. If further pregnancy was desirable, conservative surgical approach including only unilateral oophorectomy was performed in selected cases and after informed consent was obtained. Bilateral pelvic lymphadenectomy was not standard and was again performed in selected cases depending on tumor rupture presence of macroscopic pelvic metastasis, surgeon’s preference and performance status of the patient (18.8 % had pelvic lymphadenectomy). Among all patients, 28 (58.3 %) underwent primary staging surgery including total abdominal hysterectomy, bilateral salpingo-oophorectomy, while the rest of the patients had unilateral salpingo-oophorectomy. Both groups of patients also underwent infracolic omentectomy and pelvic or no pelvic lymphadenectomy. According to FIGO surgical staging, two of the cases (4.7 %) were staged as IIB, while the majority was IA and IC. Intraoperative rupture of tumor occurred in four patients 9.3 %. No adjuvant treatment was given to any of the patients included in this study.
Mitotic index was 4 or more in 34.9 % of the patients and nuclear atypia was moderate to high in 60.5 % of the cases. The mean follow-up period was 9.2 years (SD = 4.6) with median equal to 9.1 years (interquartile range from 5.1 to 13.3 years). During the follow-up period recurrence occurred in three patients (7 %) and none of them died. The cumulative recurrence free rate for the first two years was 97.6 % (SE = 2.4 %), for 5 years 94.9 % (SE = 3.5 %) and for 10 years 91.0 % (SE = 5.1 %). None of the patients with stage 1A AGCT recurred. The recurrences occurred in both the patients with stage 2 disease and one patient with stage 1C disease due to intraoperative rupture of the tumor.
Univariate Cox regression analysis showed (Table 2) a significant association of tumor size, stage and mitotic index with the risk for recurrence. All other factors, including age, intraoperative rupture of tumor and nuclear atypia were not significantly associated with recurrence free survival. Multiple Cox proportional hazard analysis (Table 3) indicated that the tumor size, stage and mitotic index were independent predictors of recurrence free survival. Specifically, increased tumor size by one cm was associated with 12 % greater hazard. Also, patients with mitotic index 4 or more had 4.9 times greater hazard for recurrence compared to those with mitotic index less than four. Additionally, patients with stage II had 7.71 greater hazard for recurrence compared to those with stage IA to IC. ROC curve analysis (Fig. 1) showed that the optimal cutoff of tumor size for the prediction of recurrence was 12 cm with sensitivity equal to 100 % and specificity equal to 80 %. The AUC was equal to 0.93 (95 % CI 0.82–1.00, p = 0.015).
In addition, histologic examination revealed that 25 patients (58.1 %) had endometrial abnormalities in the hysterectomy specimens (Table 1). This is mainly caused by resumption of endometrial proliferation due to estrogen production by the AGCT tumor. Various degrees of hyperplasia were diagnosed in 23 patients, while endometrial cancer was detected in two cases. The histological subtype was endometrioid adenocarcinoma with moderate differentiation, no adjuvant therapy was given, and as mentioned before, this finding was not an independent factor for recurrence.
Discussion
Although early stage ovarian AGCT are considered low grade malignancies with a favorable prognosis, patients diagnosed with AGCT still suffer from recurrent disease despite surgical treatment. Therefore, an effort for determination of prognostic factors in these relatively rare tumors should be attempted.
According to published data, stage, age and presence or absence of residual disease after initial surgery were shown to be important prognostic factors in AGCTs. [5–7] However, all studies have important limitations mainly because they have included only a small number of patients and also due to heterogeneity in the population included. Our study as well has important limitations as the number of patients included is small and the number of incidences (recurrences) is small as well. For that reason the confidence intervals presented are quite wide and results should be interpreted with caution. In addition, being a retrospective study carries a significant amount of selection bias and missed data that might influence the results. Nevertheless, our study has the advantage to focus and analyze only early stage disease minimizing the influence and biases of other confounding factors like adjuvant chemotherapy in studies including also advanced AGCT’s.
Analysis of clinical data from our patients with AGCT shows that general features such as age distribution were coherent with findings studied in relevant reports. Since AGCTs are usually functional, due to estrogen secretion, the most common symptom is abnormal uterine bleeding. As a result, endometrial hyperplasia and/or endometrial adenocarcinoma can be a concomitant finding in women with AGCT (5–10 %). Sekkate et al. [16] showed that 56 % of patients with AGCT had bleeding disorders (postmenopausal or intermenstrual bleeding), while Chua et al. [21] reported that 40 % of them were also refined with endometrial hyperplasia. In our study, we found 25 cases (58 %) associated with endometrial pathology in the hysterectomy specimens, whereas in two of them endometrioid adenocarcinoma was revealed.
Palpable mass and acute abdominal pain may also be presented as common symptoms in AGCTs, related to big size of the tumor in 85–97 % [5, 7, 8]. The majority of other reports conclude that an increase of tumor size can be associated with a poor prognosis, especially tumors measuring more than 10–15 cm [22, 23]. Our analyses also confirmed that increased tumor size by one cm was associated with 13 % greater risk for recurrence (cutoff 10.3 cm).
Despite some debates in the detection of more precise prognostic factors for recurrence, it seems that our study is in accordance with others as far as stage is concerned, which is considered to be the most important factor. Our study validates that even in between early stage tumors more advanced stage (II) was one of the main reasons for recurrence. In addition, we found that the number of mitoses seems to be inversely proportional to the recurrences. All our patients even the ones with stage 2 disease were completely debulked at initial surgery. The role of adjuvant chemotherapy in this setting is hugely debatable and for that reason none of our patients received chemotherapy. In light of our results one could argue that chemotherapy might have a role in stage 2 disease even in complete cytoreduction, however, this cannot be supported or recommended by this small retrospective study.
Although surgery is the mainstay of treatment for CGT, the extent of the surgical approach necessary remains controversial, and especially in regards to the role of lymphadenectomy. A resent systematic review on lymph node metastasis in stage I and II sex cord stromal and malignant germ cell tumors of the ovary reports that surgical approach varied widely in different studies and complete staging procedure, as advised by FIGO (hysterectomy with bilateral salpingo-oophorectomy and infracolic omentectomy, biopsy of the diaphragmatic peritoneum, para-aortic gutters, pelvic and para-aortic lymphadenectomy) was performed in a small number of patients. [24, 25, 28] Multiple reasons can account for the different surgical management of patients with AGCT by different Gynecological Oncologists. First, there is an extremely low incidence of lymphovascular invasion in patients with AGCT (0–8.8 %) [19, 26]. Therefore, most of the published reports are not supportive of routine lymphadenectomy during surgical staging, as in studies where this was performed, the incidence of lymph node involvement was almost zero [25, 26]. In addition, in most cases, histopathological diagnosis is made after initial surgery and a relaparotomy to complete staging with lymphadenectomy is not considered necessary. In our series, even though lymphadenectomy was performed in a considerable amount of patients no positive lymph node was identified.
Moreover, when managing AGCTs, it seems to be appropriate and oncologically safe to preserve a normal-appearing uterus and contralateral ovary in a reproductive-aged woman with apparent early stage disease. According to a recent retrospective multicenter study, no significant difference in overall survival was found between patients with AGCTs managed conservatively (unilateral salpingo-oophorectomy) in a more comprehensive staging strategy, including retroperitoneal lymphadenectomy, compared to those treated with only unilateral salpingo-oophorectomy, without comprehensive staging. As it was shown, the survival rates at 5 years were 92 and 97 %, respectively [29]. For that reason, in 15 patients (41.7 %) of our series a completion staging operation with hysterectomy, contra lateral oophorectomy and retroperitoneal lymphadenectomy was not considered necessary. None of these patients with this more conservative approach suffered a recurrence.
Median follow-up in our study was 9.1 years, which is significantly longer compared to other similar studies and may account for the higher recurrence rate observed in our series [2–9, 12–18]. Recurrent disease 37 and 25 years after initial diagnosis has been observed and is characteristic of AGCT’s [20, 27]. For that reason, long-term follow-up is essential for the best management of the patients and to receive reliable information about the clinical course of this disease.
In conclusion, and in accordance with our logistic regression analysis, tumor stage, size and number of mitosis remain significant as clinical prognostic parameters, since they are not only factors of proliferation rate but also signs of invasive and metastatic potential. Currently, they seem to be the only factors on which clinical treatment decisions can be based. Given the rarity of AGCTs of the ovary, prospective multicenter studies based on international registry are needed to clarify further possible prognostic factors as well as best management of these patients.
References
Young RH, Scuuly RE (1994) Sex cord-stromal, steroid cell and other ovarian tumors with endocrine, paraendocrine, and paraneoplastic manifestations. In: Kurman RJ (ed) Blaustein’s pathology of the female genital tract, 4th edn. Springer-Verlag, New York, pp 738–797
Fox H, Agrawal K, Langley FA (1975) A clinicopathologic study of 92 cases of granulosa cell tumor of the ovary with special reference to the factors influencing prognosis. Cancer 35:231–241
Malmstrom H, Hogberg T, Risberg B et al (1994) Granulosa cell tumor of the ovary: prognostic factors and outcome. Gynecol Oncol 52:50–55
Ohel H, Kaneti HAND, Schenker JG (1983) Granulosa cell tumors in Israel: a study of 172 cases. Gynecol Oncol 15:278–286
Fujimoto T, Sakuragi N, Okuyama F et al (2001) Histopathological prognostic factors of adult granulosa cell tumors of the ovary. Acta Obstet Gynecol Scand 80:1069–1074
Scwartz PE, Smith JP (1976) Treatment of ovarian stromal tumors. Am J Obstet Gynecol 125:402–411
Ayhan A, Salman MC, Velipasaoglu M et al (2009) Prognostic factors in adult granulosa cell tumors of the ovary: a retrospective analysis of 80 cases. J Gynecol Oncol 20:158–163
Sang Hoon Kwon (2010) A clinicopathologic study of ovarian granulosa cell tumor. J of Women’s Med 3:12–17
Miller BE, Barron BA, Wan JY et al (1997) Prognostic factors in adult granulosa cell tumor of the ovary. Am Cancer Soc 79:1951–1955
FIGO Committee on Gynecologic (2009) Oncology: current FIGO staging for cancer of the vagina, fallopian tube, ovary, and gestational trophoblastic neoplasia. Int J Gynaecol Obstet 105(1):3–4
International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10) Version for 2010; chapter XIV: diseases of the genitourinary system (N00-N99)
Ud Din N, Kayani N (2014) Recurrence of adult granulosa cell tumor of the ovary: experience at a tertiary care center. Ann Diagn Pathol 18(3):125–128
Ertas IE, Gungorduk K, Taskin S et al (2013) Prognostic predictors and spread patterns in adult ovarian granulosa cell tumors: a multicenter long-term follow-up study of 108 patients. Int J Clin Oncol. doi:10.1007/s10147-013-0630-x
Huang Ben-Shian, Sun Hsu-Dong, Hsu Yen-Mei et al (2014) Clinical presentation and outcome of adult-type granulosa cell tumors: a retrospective study of 30 patients in a single institute. J Chin Med Assoc 77(1):21–25. doi:10.1016/j.jcma.2013.09.007
Lee IH, Choi CH, Hong DG et al (2011) Clinicopathologic characteristics of granulosa cell tumors of the ovary: a multicenter retrospective study. J Gynecol Oncol 22(3):188–195
Sekkate S, Kairouani M, Serji B et al (2013) Ovarian granulosa cell tumors: a retrospective study of 27 cases and a review of the literature. World J Surg Oncol 11:142
Khosla D, Dimri K, Pandey AK et al (2014) Ovarian granulosa cell tumor: clinical features, treatment, outcomes, and prognostic factors. N Am J Med Sci 6(3):133–138
Sehouli J, Drescher FS, Mustea A et al (2004) Granulosa cell tumor of the ovary: 10 years follow-up data of 65 patients. Anticancer Res 24(2C):1223–1229
Fotopoulou C, Savvatis K, Braicu EI et al (2010) Adult granulosa cell tumors of the ovary: tumor dissemination pattern at primary and recurrent situation, surgical outcome. Gynecol Oncol 119(2):285–290
Hines JF, Khalifa MA, Moore JL et al (1995) Recurrent granulosa cell tumor of the ovary 37 years after initial diagnosis: a case report and review of the literature. Gynecol Oncol 60:484–488
Chua IS, Tan KT, Lim-Tan SK et al (2001) A clinical review of granulosa cell tumors of the ovary cases in KKH. Singap Med J 42:203–207
Bompas E et al (2000) Granulosa cell tumor: review of the literature. Bull Cancer 87:709–714
Schumer ST, Cannistra SA (2003) Granulosa cell tumor of the ovary. J Clin Oncol 21(6):1180–1189
Lee YK, Park NH, Kim JW et al (2008) Characteristics of recurrence in adult-type granulosa cell tumor. Int J Gynecol Cancer 18:642–647
Park JY, Jin KL, Kim DY et al (2012) Surgical staging and adjuvant chemotherapy in the management of patients with adult granulosa cell tumors of the ovary. Gynecol Oncol 125:80–86
Abu-Rustum NR, Restivo A, Ivy J et al (2006) Retroperitoneal nodal metastasis in primary and recurrent granulosa cell tumors of the ovary. Gynecol Oncol 103:31–34
Hasiakos D, Papakonstantinou K, Karvouni E et al (2008) Recurrence of granulosa cell tumor 25 years after initial diagnosis. Report of a case and review of the literature. Eur J Gynaecol Oncol 29(1):86–88
Kleppe M, Amkreutz LCM, Van Gorp T et al (2014) Lymph-node metastasis in stage I and II sex cord stromal and malignant germ cell tumors of the ovary: a systematic review. Gynecol Oncol 133:124–127
Liu Q, Ding X, Yang J et al (2013) The significance of comprehensive staging surgery in malignant ovarian germ cell tumors. Gynecol Oncol 131:551–554
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
For this type of study formal consent is not required.
Rights and permissions
About this article
Cite this article
Thomakos, N., Biliatis, I., Koutroumpa, I. et al. Prognostic factors for recurrence in early stage adult granulosa cell tumor of the ovary. Arch Gynecol Obstet 294, 1031–1036 (2016). https://doi.org/10.1007/s00404-016-4135-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-016-4135-5