Abstract
The periodontal health of abutment teeth and the durability of fixed partial denture depends on the marginal adaptation of the prosthesis. Any discrepancy in the marginal area leads to dissolution of luting agent and plaque accumulation. This study was done with the aim of evaluating the accuracy of marginal fit of four unit crown and bridge made up of Ni–Cr and Cr–Co alloys under induction and centrifugal casting. They were compared to cast fixed partial denture (FPD) and soldered FPD. For the purpose of this study a metal model was fabricated. A total of 40 samples (4-unit crown and bridge) were prepared in which 20 Cr–Co samples and 20 Ni–Cr samples were fabricated. Within these 20 samples of each group 10 samples were prepared by induction casting technique and other 10 samples with centrifugal casting technique. The cast FPD samples obtained were seated on the model and the samples were then measured with travelling microscope having precision of 0.001 cm. Sectioning of samples was done between the two pontics and measurements were made, then the soldering was made with torch soldering unit. The marginal discrepancy of soldered samples was measured and all findings were statistically analysed. The results revealed minimal marginal discrepancy with Cr–Co samples when compared to Ni–Cr samples done under induction casting technique. When compared to cast FPD samples, the soldered group showed reduced marginal discrepancy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The accuracy of well adapted margins of cast fixed partial dental restorations is considered a primary factor in determining the long-term success of any prostheses [1]. The precise fit of the restorative margin is necessary for preventing gingival inflammation and failure of the restoration. It will also enhance the retention and reduce the amount of failure of the restoration. In addition, marginal accuracy is considered a primary factor in the prevention of secondary caries.
The solidification shrinkage of alloys and sagging can lead to inaccurate marginal fit of fixed partial denture (FPD). To improve the accuracy of marginal fit of long span FPD in posterior edentulous area, soldered connectors have been advocated. Soldering may improve dimensional accuracy or reduce the distortion of multiunit fixed prostheses [2].Soldering technique has been generally used for joining retainers and pontics in FPD [3]. Tylman, Ryge & Skinner recommended a gap of 0.1–0.25 mm to be provided between the units to be soldered to prevent the warpage produced by the metal expansion which is greater than the expansion of soldering investment [4–6].The cast FPDs were made by induction casting and centrifugal casting techniques but the clinically acceptable complete castings can be obtained with the induction casting technique if optimum heating conditions are selected. Hence the study was conducted to evaluate the accuracy of marginal fit of 4-unit FPD made up of centrifugal and induction casting techniques and also compared the marginal fit of cast FPD and soldered FPD made of nickel–chromium (Ni–Cr) and chromium–cobalt (Cr–Co) alloys [7–9].
Materials and Methods
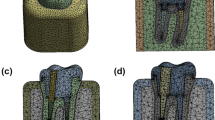
To evaluate the marginal fit of cast and soldered FPD, a typodont was used to represent the clinical situation of 4-unit crown and bridge. The left maxillary canine and first molar were used as abutments, to which the full veneer preparation was made with shoulder finish line with rounded axio gingival line angle. An impression of prepared segment was made with addition silicone impression material. To standardize the study a metal model (Fig. 1) was made with copper based alloy (copper 75 %, zinc 15 %, and tin) (Fig. 3). To standardize the location of measurement reference lines were marked on the mid mesial and mid distal surfaces of anterior and posterior abutment of the model. The wax patterns (Fig. 2) were made over the model (Fig. 3) which were invested with phosphate bonded investment material (Ivoclar, liechtenstein).To standardize the technique all 40 samples were fabricated using lost wax technique (the fabrication of wax pattern, spruing, investing, casting, sandblasting and measurements were carried out by the same operator). Burn out was carried out at 800 °C/1,470 °F. Altogether 40, 4-unit crown and bridge samples were made, which were grouped as.
Group-A: 20 samples were made with Cr–Co alloy (Ivoclar vivadent, liechtenstein), which was further sub divided into (Fig. 3)
-
Subgroup a: 10 samples were made using induction casting machine
-
Subgroup b: 10 samples were made using centrifugal casting machine
Group-B: 20 samples were made with Ni–Cr alloy (Ivoclar vivadent, liechtenstein), which was further sub divided into (Fig. 4)
-
Subgroup c: 10 samples were made using induction casting machine
-
Subgroup d: 10 samples were made using centrifugal casting machine
For Ni–Cr alloy the casting temperature was 1,405 °C/2,560 °F and for Cr–Co alloy casting temperature was 1,240 °C/2,265 °F. After cooling, the castings were retrieved from investment and sandblasted using medium grit (50 μm) aluminum oxide.
To evaluate the marginal accuracy, the 4-unit crown and bridges were seated on the model (Fig. 5) and subjected to constant load of 500 g for 5 min. The restorations were not cemented onto the tooth specimen to simulate the clinical situation. If the specimens were cemented onto the tooth, it would be difficult to visualize the reference points if the margins were covered with luting material. The marginal discrepancy was measured using a travelling microscope having precision of 0.001 cm. The measurements of 4-unit cast samples were made between the cervical margin of the casting and the finish line of the abutments in the region of reference line. Then the samples were vertically sectioned between two pontics using 0.4 mm thickness carborundum disc. Sectioned samples were placed on the model and the gap was maintained by temporarily joining with sticky wax and stabilized using wooden stick and then invested with soldering investment (Whip Mix, Louisville). To standardize the study, Dental universal solder (Produits dentaires SA, Switzerland) which was a silver based prefluxed solder (Ag 59 %, Cu 16 % and Zn 25 %) with ISO 9333:2005 ideal for Ni–Cr and Cr–Co alloys was used. Soldering was done with the help of torch soldering unit (Bego, Germany). The marginal accuracy of soldered samples was also measured in the same reference points. The measurements were tabulated and statistically analyzed.
Results
The values were subjected to statistical analysis using one way ANOVA test for group comparison (induction ¢rifugal casting) and Tukey’s post hoc test for comparison within the group for Ni–Cr and Cr–Co was done. The results of the analysis are given in tables.
Table 1 show the value of the descriptive statistics of the sample size, mean, standard deviation and standard error of cast, sectioned and soldered samples. The table also illustrates the F value (the ratio of the variances) 0.687 cm and the P value 0.514 cm which show the probability from the distribution. Since the P value is greater than 0.05, there is no significant difference in the mean scores of the mean discrepancy.
Table 2 describe the marginal discrepancy of cast samples which was significant (0.285 cm) when compared to sectioned and soldered samples.
In Table 3 the comparative mean values of (Cr–Co) soldered samples showed minimal marginal discrepancy with induction casting technique which was shown in Graph 1, Whereas the marginal discrepancy was minimal with centrifugal casting technique for (Ni–Cr) soldered samples it was mentioned in Graph 2.
In Table 4 the Cr–Co samples made with induction casting technique (Bar dig: 1) showed minimal marginal discrepancy when compared to Ni–Cr samples which was shown in Graph 3.
Discussion
The marginal adaptation of FPD is necessary for longevity and periodontal health, as marginal discrepancies contribute to cement dissolution and plaque accumulation resulting in recurrent decay and periodontal disease. Definitions to describe the marginal adaptation can vary greatly and make comparisons of studies difficult. Holmes et al. [10] defined an external marginal gap and an internal marginal gap that was also influenced by the horizontal over extension and under extension of the restoration margin. There are also variations in the methods used to measure the marginal adaptation of crowns due to complex gap morphology and also the number of sites measured. Factors that may affect marginal adaptation include tooth preparation, margin design, alloy types, casting procedures, porcelain firing cycles, and cementation techniques. Shoulder and shoulder-bevel designs were found to have less marginal distortion than chamfer designs. So in this study shoulder finish line was used to prepare the abutments. Marginal adaptation assessments can be completed by direct visualization of the crown on the die, clinical evaluation of the tooth/restoration interface, the impression replica technique and use of a cross-sectional view or by using travelling microscope [11]. Thus in this study travelling microscope was used to measure the marginal accuracy of all the samples.
Recently, the use of Ni–Cr base metal alloys in fixed prosthesis tends to increase because of the continued inflation of gold price. Base metal alloys have various advantages such as higher yield and tensile strength and better resistance to creep compared with noble alloys. However, base metal alloys also have several crucial disadvantages to be used. One of the critical disadvantages is the technique sensitivity in laboratory procedures, especially during casting and soldering [12]. The Co–Cr alloys are used in this study because of its high strength, hardness, strong, non-tarnishing qualities due to chromium oxide forms an adherent and resistant surface layer and lighter in weight. So the Cr–Co samples showed minimal marginal discrepancy when compared to Ni–Cr samples. But the disadvantages of using Cr–Co alloys are difficulty in cutting, grinding, finishing and the casting shrinkage is greater than gold alloys due to high fusion temperature [13]. The casting accuracy of Ni–Cr and Cr–Co alloy for crown and bridge prostheses were difficult to obtain with an acceptable retention and minimal marginal discrepancies [14].
The objective of the casting process is to provide a metallic duplication of missing tooth structure with as much accuracy as possible. In centrifugal casting technique alloy is melted by a torch flame in a glazed ceramic crucible, attached to the broken arm of the casting machine. Once the metal fills the mold there is a hydrostatic pressure gradient developed along the length of the casting [15, 16]. But in induction casting technique, alloy is melted by induction field then cast into the mold centrifugally by motor or spring action by air pressure, or by vacuum [17–19]. So in this study both the casting techniques were used to prepare the samples.
Soldering is a traditional method for joining components of fixed partial dentures using an intermediate metal. The longevity of a soldered prosthesis depends on the mechanical properties of its solder joints [20, 21]. Previous studies described an improvement in the accuracy of the marginal fit of both retainers on respective abutments by using soldered connectors [22]. The soldering process involves the substrate metals to be joined, a filler metal (solder), a flux and a heat source. The composition of the substrate metal determines the oxide that forms on the surface during heating, and if used, a flux must be able to reduce this oxide. The solder chosen must wet the metal at as low contact angle as possible to ensure wetting of the joint area. To prevent flow onto adjacent areas, an antiflux such as rouge mixed with chloroform can be painted on the areas before heating the assembly [23, 24]. Another study described that the improvement in marginal fit was achieved by sectioning and soldering when compared to conventional FPD [25]. Thus in the present study soldering technique was used to join sectioned samples, and it was used to compare with cast samples.
Mean and standard deviation values of marginal discrepancy of cervical margins of cast samples were 0.02400 and 0.0161 cm and for soldered samples were 0.1525 and 0.00665 cm. Higher marginal gap was recorded in cast FPD samples when compared to soldered samples. The mean and standard deviation values of induction casting samples were 0.0102 and 0.0070 cm and for centrifugal casting were 0.0298 and 0.0162 cm, so the marginal discrepancy was higher for centrifugal casting when compared to induction casting. The mean and standard deviation values of Cr–Co samples were 0.0102 and 0.0070 cm and for Ni–Cr samples were 0.0216 and 0.0116 cm thus the marginal gap in higher for Ni–Cr samples when compared to Cr–Co samples.
The limitations of this study are:
-
The effect of investment towards marginal discrepancy was not evaluated
-
Only torch soldering unit was used for joining the sectioned samples whereas other methods like welding, oven and infra red soldering can also influence the final results of study
-
Ni–Cr and Cr–Co base metal alloys were used in this study, if some other base metal alloys were used it may influence the final result
-
If any other solders were used, other than dental universal solder it may influence the result
Clinical Implications
The clinical significance implicate, in the posterior region with long span edentulous area, soldering of long span FPDs will enhance the marginal fit when compared to cast FPD. Crown and bridges made of Cr–Co alloys showed minimal marginal discrepancy when compared to Ni–Cr alloys. FPDs made of Induction casting technique showed improved marginal fit when compared to centrifugal casting technique.
Conclusion
Within the limitations of this study the following conclusions were made.
-
1.
The FPDs made of Cr–Co alloys showed minimal marginal discrepancy when compared to Ni–Cr alloys
-
2.
The FPDs made of induction casting technique showed improved marginal fit when compared to centrifugal casting technique
-
3.
The soldered samples showed improved marginal fit when compared to cast FPD samples
References
Rosenstiel SF, Land MF (2006) Contemporary fixed prosthodontics, 4th edn. Mosby-year Book, St Louis
Byrne G (2011) Soldering in prosthodontics—an overview. J Prosthodont 20:233–243
Ziebert GJ et al (1980) Accuracy of one piece castings, preceramic and postceramic soldering. J Prosthet Dent 43:272
Malone WFP, Koth DL (1989) Tylman‘s theory and practice of fixed prosthodontics, 8th edn. Ishiyaku EuroAmerica, Tokyo
Willis LM (1980) Distortion in dental soldering as affected by gap distance. J Prosthet Dent 43:272–278
Huling JS (1977) Compratative distortion in three unit fixed prostheses joined by laser welding, conventional soldering or casting in one-piece. J Dent Res 56:128–134
Sass F, Eames W (1980) Fit of unit-cast fixed partial dentures related to casting ring size and shape. J Prosthet Dent 43:163–164
Hansson O (1985) Casting accuracy of a nickel and beryllium-free cobalt–chromium alloy for crown and bridge prostheses and resin-bonded bridges. Swed Dent J 9:105–115
Hinman R et al (1985) Improving the casting accuracy of fixed partial dentures. J Prosthet Dent 53:466
Holmes JR, Bayne SC (1982) Considerations in measurement of marginal fit. J Prosthet Dent 62:405–408
Cogolludo PG, Suarez MJ, Peláez J, Lozano JF (2010) Influence of melting and casting methods and finish line design on the marginal discrepancy of nickel-chromium-titanium alloy crowns. Int J Prosthodont 23(5):443–445
Kasloff Z (1961) Casting techniques and some variables. J Prosthet Dent 11:533–536
Anusavice KJ (2003) Phillips science of dental materials, 11th edn. Saunders, Philadelphia, pp 295–345
Wu JC, Lai LC, Sheets CG, Earthman J, Newcomb R (2011) A comparison of the marginal adaptation of cathode-arc vapor-deposited titanium and cast base metal copings. J Prosthet Dent 105(6):403–409
Gegauff AG (1989) The seating of one-piece and soldered fixed partial dentures. J Prosthet Dent 62:292–297
Calesini G (2000) One-piece castings in fixed prosthodontics; a study of marginal adaptation using computerized SEM images. Int J Prosthodont 13:275–281
Milan FM, Consani S, Correr Sobrinho L, Sinhoreti MA, Sousa-Neto MD, Knowles JC (2004) Influence of casting methods on marginal and internal discrepancies of complete cast crowns. Braz Dent J 15:127–132
Bruce R (1967) Clinical applications of multiple unit castings for fixed prostheses. J Prosthet Dent 18:359–364
Bauer JR (2006) Microhardness of Ni–Cr alloys under different casting conditions. Braz Oral Res 20:40–46
Konstantoulakis E (1998) Marginal fit and surface roughness of crowns made with an accelerated casting technique. J Prosthet Dent 80:337–345
Schilling ER (1999) Marginal gap of crowns made with a phosphate-bonded investment and accelerated casting method. J Prosthet Dent 18:129–134
Madan N (1999) An investigation into the accuracy of fit of a cast fixed partial denture compared to a soldered fixed partial denture—an in vitro study. J Indian Prosthodont Soc 10:25–28
Fusayama T et al (1964) Accuracy of F.P.Ds made by various soldering techniques and one piece casting. J Prosthet Dent 14:334
Stackhouse JA (1967) Assembly of dental units by soldering. J Prosthet Dent 18:131–139
Lee SY, Lee JH (2010) Effect of soldering techniques and gap distance on tensile strength of soldered Ni–Cr alloy joint. J Adv Prosthodont 2(4):117–121
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jei, J.B., Mohan, J. Comparative Evaluation of Marginal Accuracy of a Cast Fixed Partial Denture Compared to Soldered Fixed Partial Denture Made of Two Different Base Metal Alloys and Casting Techniques: An In vitro Study. J Indian Prosthodont Soc 14, 104–109 (2014). https://doi.org/10.1007/s13191-013-0286-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13191-013-0286-2