Abstract
Objectives
This study aimed to evaluate a digital multi-piece zirconia post-crown to restore a mandibular second molar with extensive coronal loss and limited restoration space, and to compare the stress distribution between endocrowns made of zirconia or alloy and CAD/CAM multi-piece zirconia post-crowns.
Material and methods
Four three-dimensional finite element analysis models of a mandibular second molar with extensive coronal loss and limited restoration space were created as follows: (A) intact molar; (B) zirconia endocrown restored molar; (C) multi-piece post-crown restored-molar with tapered nail; (D) multi-piece post-crown restored molar with T-shaped nail. Models C and D were divided into two subgroups according to the material type: C1/D1, zirconia; C2/D2, NiCr alloy. The maximum modified von Mises failure criterion (mvM) stresses were calculated, and the stress distribution was recorded to analyze the effects of the restoration and material types on the biomechanical properties of dentin and prosthesis.
Results
The maximum mvM stress of dentin in model B (33.80 MPa) was lower compared with models C (C1, 37.81 MPa; C2, 36.36 MPa) and D (D1, 36.34 MPa; D2, 34.97 MPa) under vertical load, but the opposite was observed under oblique load. The highest mvM stress was concentrated in the nail region located in the root canal, and the T-shaped nail values were greater than the tapered nail, whereas model D with T-shaped nail showed a lower mvM stress level in dentin compared with Model C with tapered nail.
Conclusions
The digital multi-piece zirconia post-crown is a potential approach to restore mandibular second molars with extensive coronal loss and limited restoration space.
Clinical relevance
The digital multi-piece zirconia post-crown has potential to restore mandibular second molars with extensive coronal loss and limited restoration space using an innovative approach.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The molars of Asians and Europeans are relatively smaller than that of Oceanians and Africans [1, 2], resulting in shorter occluso-cervical dimension, which can lead to an insufficient retention of potential restorations. The antagonist teeth are prone to elongate when a mandibular second molar with excessive loss of coronal tissue is not restored immediately, which can normally lead to limited restoration space. Moreover, the crowding, higher angle of inclination, or insufficient distance between the mandibular first molar and mandibular ramus characterize the mandibular second molar impaction [3].
An occluso-cervical dimension of 3 mm is generally accepted as the minimum threshold for full-crown retention [4]. Full crowns are commonly used to restore mandibular second molars with normal occluso-cervical dimension. Mandibular second molars that present with insufficient occluso-cervical dimension should be modified with auxiliary features, such as grooves/boxes. However, mandibular second molars with excessive loss of coronal tissue that cannot benefit from auxiliary features should be restored with a post-and-core crown, which is needed to increase the retention through extending sufficient length of the post in the root canal [5]. Unfortunately, post-and-core crowns fail to restore mandibular second molars with excessive loss of coronal dental tissue and limited restoration space given the 3-mm minimum threshold of occluso-cervical dimension [6]. Rehabilitation of these mandibular second molar with extensive coronal loss and limited restoration space remains a major challenge. Therefore, direct filling, orthodontic treatment, and crown lengthening surgery are available alternative methods in these cases. However, direct filling is inferior to achieve functional and esthetic effects compared with indirect restorations [7, 8]; orthodontic treatment is time-consuming and costly, bringing great pain to patients [9]; and crown lengthening surgery is traumatic and time-consuming as well as shortening the actual length of the root in the alveolar bone which leads to long-term instability [10]. Endocrown has been recently developed to restore molars with excessive loss of dental tissue and insufficient restoration space, especially in cases of molars with narrow and frequently curved canals [5, 8, 11,12,13]. Tooth reduction is decreased with endocrowns compared with post-and-core crown, and no interference between the root canals occur [14]. Through three-dimensional finite element analysis (FEA), studies have shown that leucite-reinforced ceramic endocrowns had lower modified von Mises failure criterion (mvM) stress level in dentin compared with conventional leucite-reinforced ceramic crowns supported by fiber-reinforced composite post-and-core [15]. Moreover, the endocrowns in molars are less susceptible to damage compared with the post-core crown [15]. However, not all studies have shown positive results. Previous reports have shown that root fractures, debonding, excessive preparation of the pulp chamber, and inconformity to the concept of “minimally invasive” was accompanied with endocrown restoration. The endocrown cannot connect with the root, and thus was easily fractured when the residual tooth tissue was weak, and the force was uneven [16].
A multi-piece metal post-crown restoration design has been proposed to obtain enough retention in the root canal and to avoid interference between the root canals [17]. However, this restoration has shown disadvantages, including limited precision, corrosion, high technical sensitivity in the wax casting process, and shortcomings of metal in esthetics [18,19,20,21,22], and its original intention was not for restoring mandibular second molar with extensive coronal loss and limited restoration space. However, a multi-piece metal post-crown design can be improved to potentially restore mandibular second molar with extensive coronal loss and limited restoration space.
The aim of the present study was to introduce a CAD/CAM zirconia post-crown with a special nail structure that can potentially be used as an alternative for restoring mandibular second molar with extensive coronal loss and limited restoration space. FEA was applied to evaluate the effectiveness of the structure introduced post-crown in comparison with the endocrown and metal post-crown. Advantages of this design include smaller trauma, lower technical sensitivity, and applicability for digital design and processing. The null hypothesis tested was that no differences would be found in the mvM stress and stress distribution between zirconia/alloy endocrown and CAD/CAM multi-piece zirconia post-crown.
Materials and methods
Generation of FEA models
Our study was approved by the Ethical Committee Department, Affiliated Hospital of Stomatology, Nanjing Medical University (Protocol no. PJ2019-091–001).
The maxillary and mandibular arches of a patient with normal occlusion were digitized by a CBCT (NewTom, Italy) scan with a voxel dimension of 100 µm (approved by Ethical Committee Department, Affiliated Hospital of Stomatology, Nanjing Medical University, number: PJ2019-091–001). The obtained scans of the lower left second molar were processed with MIMICS software (MIMICS 19.0, Materialise, Belgium). Scan datasets were introduced into the FEA ANSYS software (ANSY Workbench 18.0, PA, USA), and four FEA models were fabricated through precise calculations using the software program. The periodontal ligament and the trabecular were simulated around the models. The periodontal ligament thickness was 0.2 mm, and the cortical bone thickness was 2 mm [15].
The X-axis and Z-axis in all models showed the molar lingual surface and mesial surface, respectively, and the Y-axis was directed upward. Four FE models are described in detail as follows.
Model A: intact molar
The occluso-cervical dimension of the crown was 3 mm to simulate a molar with a low occluso-cervical dimension. The bucco-lingual diameter was 10.5 mm, and the distal root length and mesial root length were 10.2 and 9.8 mm, respectively (Fig. 1).
Model B: zirconia endocrown restored molar
The tooth model was sectioned perpendicular along the long axis from the cusps, at a distance of 2 mm. Within the pulp chamber, a cube with a dimension of 6.3 × 5.2 × 5.7 mm3 was created and joined with the divided portion of the crown [15]. The thickness of the cement layer between the prepared tooth and the crown was set as 0.1 mm (Fig. 1) [12].
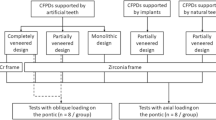
Model C: multi-piece post-crown restored molar with tapered nail
A zirconia full crown supported by posts was divided vertically into sections along the tooth’s long axis at 2 mm from the cusp tips [23]. Then two simulated posts were introduced into the mesial and distal canals of the second lower molar model at a depth of 5.8 mm and 6.2 mm, respectively, and their diameters were 1/3 of the root diameter. Subsequently, the post in the distal canal was then joined to the cube at the same dimension as in model B, while the post in the mesial canal was separated from the cube and penetrated through its interior to the occlusal surface of the post-crown, which was defined as nail (Fig. 1). The cement layer thickness was set at 0.1 mm, as well as between the nail and the post-crown.
Model D: multi-piece post-crown restored molar with T-shaped nail
Model D is an innovation based on model C, wherein the nail was designed as T-shaped. Detailed clinical design and manufacturing of the digital multi-piece zirconia post-crown with T-shaped nail are included in “Supplementary Materials.” The T-shaped nail creation process was as follows: (1) the diameter of the nail located above the root canal orifice was approximately 1 mm wider than the part below the root canal orifice, and (2) a 120° slope was formed at the joint of the two parts (Figs. 1 and 2). Schematic representations of digital multi-piece zirconia post-crowns with one or two T-shaped nails are shown in Fig. 2.
Model C and model D were divided into two subgroups according to material types as follows: model C1/D1—zirconia; model C2/D2—NiCr alloy.
Mesh generation
For calculation purposes, the tooth models were meshed and redefined by 8-node parametric elements that contained 3 degrees of freedom per node. Information on the nodes and elements is shown in Table 1.
Boundary condition and load application
The materials used were homogenous, isotropic, linearly elastic, and flawless. FEA models were securely fixed within the alveolar bone, and no movement was allowed in any direction.
The vertical (axial) load was exerted directly toward the models’ occlusal surfaces to simulate the normal occlusal load using five diverse contact points, including three points on the outer aspects of buccal cusps and two points on the inner aspects of lingual cusps. A load of 600 N was vertically applied to the restoration to simulate the maximum bite force; meanwhile, loads of 225 N were applied from three different directions (vertically, at a 45° angle, and horizontally) to simulate masticatory force [24].
Material properties
The endocrown and zirconia multi-piece post-crown were made of e.max ZirCAD (Ivoclar, Vivadent AG, Schaan, Lichtenstein) and were luted to the tooth using a Variolink II composite cement (Ivoclar, Vivadent, Schaan, Lichtenstein). NiCr multi-piece post-crown (KENNAMETAL, PA, USA) was luted to tooth structures with glass ionomer cement (Ketac Cem Easymix, 3M ESPE St. Paul, MN, USA). The values for elasticity modulus and Poisson’s ratio of the dentin [15, 25], periodontal ligament [23, 26], cortical bone [27], trabecular bone [27], zirconia [28], NiCr alloy [23], composite luting cement [23], and glass ionomer cement were entered [29]. The data are detailed in Table 2. The materials used in our study model differed in tensile and compressive strength, but they were isotropic, homogenous, and linearly elastic [23].
Analysis mode
The maximum mvM stress for models with restorations was calculated and stress distribution was recorded to analyze the effects of the restoration type and material type on the biomechanical properties of dentin and prosthesis.
Results
The stress distributions are shown in Figs. 3, 4 and 5, and the maximum mvM stresses in models with restoration under vertical and oblique loads (MPa) are shown in Figs. 6 and 7, respectively.
Distribution of the mvM stresses in model B with zirconia endocrowns under vertical load and oblique load. Distribution of the mvM stresses in zirconia endocrowns under vertical load (A) and oblique load (B). (a, b) The mvM stresses in zirconia endocrowns; (c) the mvM stresses in composite resin luting cement; (d) the mvM stresses in dentin
Distribution of the mvM stresses in model C with multi-piece zirconia post-crown under vertical load and oblique load. Distribution of the mvM stresses in multi-piece zirconia post-crown under vertical load (A) and oblique load (B). Distribution of the mvM stresses in model C with multi-piece NiCr post-crown under vertical load (C) and oblique load (D). (a, b) The mvM stresses in multi-piece post-crown; (c) the mvM stresses in nail; (d) the mvM stresses in dentin
Distribution of the mvM stresses in model D using a multi-piece zirconia post-crown under vertical load and oblique load. Distribution of the mvM stresses in a multi-piece zirconia post-crown under vertical load (A) and oblique load (B). Distribution of the mvM stresses in model D using a multi-piece NiCr post-crown under vertical load (C) and oblique load (D). (a, b) The mvM stresses in multi-piece post-crowns; (c) the mvM stresses in a nail; (d) the mvM stresses in dentin
Maximum mvM stresses in finite element models of mandibular molars with various restorations under vertical load. Model B: zirconia endocrown restored molar; model C1: zirconia multi-piece post-crown restored-molar with tapered nail; model C2: NiCr alloy multi-piece post-crown restored-molar with tapered nail; model D1: Zirconia multi-piece post-crown restored molar with T-shaped nail; model D2: NiCr alloy multi-piece post-crown restored molar with T-shaped nail
Maximum mvM stresses in finite element models of mandibular molars with various restorations under oblique load. Model B: Zirconia endocrown restored molar; model C1: zirconia multi-piece post-crown restored-molar with tapered nail; model C2: NiCr alloy multi-piece post-crown restored-molar with tapered nail; model D1: zirconia multi-piece post-crown restored molar with T-shaped nail; model D2: NiCr alloy multi-piece post-crown restored molar with T-shaped nail
Effects of restoration type on mvM stress
The maximum mvM stress of dentin in model B with endocrown (33.80 MPa) was lower compared with model C (C1: 37.81 MPa; C2: 36.36 MPa) and model D (D1: 36.34 MPa; D2: 34.97 MPa) with post-crown under vertical load, but the opposite was found under oblique load (model B: 15.66 MPa; model C1: 9.00 MPa; C2: 8.65 MPa; model D1: 8.45 MPa; D2: 8.19 MPa). The maximum mvM stress of dentin in model D was lower than that in model C, whereas the stress values in the T-shaped nail were greater compared with the tapered nail, and zirconia nail in model D1 obtained the highest mvM stress compared with nails in other tooth models.
Effects of material type on mvM stress
Regardless of restoration type, at the restoration, dentin, and post, the maximum mvM stress values of models C1/D1 (restored tooth with zirconia) were higher compared with those of model C2/D2 (restored tooth with NiCr alloy).
Effects of restoration type and material type on stress distribution
The stress distribution was significantly affected by the restoration type, whereas in the same model groups, the stress distribution of subgroups with different materials was similar.
In model B, the highest mvM stress of the restoration was concentrated on the functional cusp of the zirconia endocrown. In the cement, the maximum mvM stress was recorded around the zirconia crown shoulder.
In model C and model D, the mvM stress in the posts significantly was higher compared with the pulp chamber under vertical load, and the highest mvM stress of the nails was situated on the region of the nails that were located in the root canal. According to the stress distribution on dentin, the stress of the root canal orifice where the tapered nail was located was greater than the root canal orifice where the post connected to the post-crown was located (model C), whereas this result was not found in model D with T-shaped nail.
Discussion
According to FEA results, the highest mvM stress value of dentin in the models of various restorations was 38.81 MPa, which is far lower than the fracture strength of healthy dentin (232–305 MPa) [24], suggesting that both the zirconia endocrown and the newly digital metal/zirconia multi-piece post-crowns were safe.
The fracturing of restorations is an important factor that contributes to the failure of mandibular second molar with extensive coronal loss and limited restoration space [30]. Fatigue failures of restorative materials in mandibular second molar with extensive coronal loss and limited restoration space might result from normal or increased functional stresses [3]. Crown fractures are caused by insufficient thickness of restorations and/or interocclusal space [31]. Because of the lower coefficient of friction in zirconia material than in enamel, when excessive occlusal pressure was applied, the occlusal crown was thinned, and the enamel of the antagonist tooth caused a hole in the zirconia crown [32]. Fortunately, the new digital zirconia multi-piece post-crown ensured enough thickness in the occlusal surface because of the adequate space from the pulp chamber.
Tooth fracture is another main concern for mandibular second molars with extensive coronal loss and limited restoration space. A 1.5–2-mm ferrule has shown a positive effect on the fracture resistance of mandibular second molars with extensive coronal loss and limited restoration space [33]. The residual height of the walls is low (less than 2 mm), thus not allowing for the ferrule effect during the preparation of a crown [30], which could increase the risk of tooth fracture [34].
In the present study, the maximum mvM stress of dentin in model B with an endocrown was lower compared with models of post-crown under vertical loads, including the designed multi-piece zirconia post-crown. However, under oblique load, the results were reversed because the maximum mvM stress of dentin in model B with an endocrown was higher compared with that in models of post-crowns, suggesting an increased risk in tooth fracture. A previous report has shown that the root fractures for endocrowns is 6%, and that most failures (71%) are due to loosening [5]. For restoration using endocrowns, the intracoronal depths of molars decreased the fracture resistance of endodontically treated teeth [35], which was more significant when the depth of intracoronal extension of endocrowns was lower (such as 1 mm). The lower the extension of the endocrowns, the greater tendency of rotating and falling off with the stressed side as the fulcrum occurs. Meanwhile, a greater depth of the pulp chamber is achieved through preparing dentin more deeply. However, this technique cannot be considered minimally invasive or a conservative alternative approach [35]. The maximum difference between the mvM stresses in finite element models of mandibular molars with various restorations was 14.7 MPa, and the minimum was approximately 1 MPa. Although the maximum mvM stresses among the groups were similar, the retention effect was significantly different. The endocrown depended on box form retention, and the multi-piece post-crown relied on box form retention and radicular retention of root post, and the latter was obviously stronger because of the additional retention [8, 15].
Materials with a higher elastic modulus concentrate more stresses, thus, may transmit undamped stresses at the tooth-and-material bonded interface [5]. The multi-piece post-crowns made from two materials in the present study showed that the highest mvM stress values of dentin in models restored with multi-piece zirconia post-crown were slightly higher compared with those in corresponding models repaired with multi-piece NiCr post-crown, which might be attributed to the extremely high elastic modulus of zirconia [36, 37]. Fortunately, the stress value was far less than the flexural strength of dentin. Nevertheless, it should be noted that the stress is transferred from the post with high elastic modulus to the dentin with low elastic modulus during the process of mastication, forming concentration in the root, which increases the risk of root fracture. Thus, optimization of the structure or shape of zirconia nails is required to avoid stress concentration in zirconia materials or tooth tissue.
The shape of the previous nails in the cast multi-piece post-crown was tapered [38, 39], whereas little attention has been shown to problems with the shapes of metal nails because of the adequate bending strength provided by metal and alloy. However, zirconia is ceramic and tends to fracture due to brittleness [40, 41]. According to the stress distribution of the nails in model C and model D, the stresses of the nails were concentrated at the region located in the root canals, which was consistent with a previous study [42], wherein the stress was accumulated within the cast post core and apical 1⁄3 region of the tooth in a post core cast system; the stress was distributed to the cervical 1⁄3 region of the tooth and to the supporting bone structure in a fiber composite laminate post core system. In addition, the maximum mvM stress of zirconia nail was higher than that of NiCr nail within the same model, indicating that healthy dentin should be retained as much as possible to reduce the risk of root fracture when manufacturing a multi-piece post-crown with zirconia materials. However, the highest stress values were lower than the flexural strength of the zirconia material (900–1200 MPa) [43, 44]. Simultaneously, attention should be paid to the appropriate diameter of the zirconia post itself to avoid fracture. Regardless of the materials, the highest mvM stress of the dentin post-crown using T-shaped nails was lower compared with that of the post-crown using tapered nails, suggesting that the nail designed and manufactured by digital technology with a certain diameter difference and angle was more conducive to the stress dispersion of dentin. Therefore, the null hypothesis that no differences would be found in the mvM stress and stress distribution between zirconia/alloy endocrown and CAD/CAM multi-piece zirconia post-crown was rejected.
Clinicians should consider parafunctional occlusal load when planning treatment. Parafunctional loading has been shown to increase stress in the cortical bone tissue [45]; thus, the maximum mvM stress of restorations should increase. Moreover, Mendonça et al. reported that single posterior crowns may be more susceptible to micromovement above the physiological limit under masticatory function [46].
Noticeably, it was not possible to include all factors present in the oral cavity with computer simulations. The durability of restorations was determined not only by the stiffness and strength of the materials from which they are made, but also by their resistance to cyclic loading, process of aging, hardness, abrasion, wear, etc. The present results should be confirmed by clinical studies to recommend the proposed restoration design, including parafunctions, which should improve safety and treatment planning.
Conclusions
Within the limitations of the present study, the following conclusions can be drawn:
-
1.
The digital multi-piece zirconia post-crown is a potential alternative approach for restoring mandibular second molars with extensive coronal loss and limited restoration space.
-
2.
The maximum mvM stress of dentin in the digital multi-piece zirconia post-crown was higher compared with the zirconia endocrown under a vertical load. Under an oblique load, the maximum mvM stress of dentin in the digital multi-piece zirconia post-crown was lower than that in the zirconia endocrown.
-
3.
In the digital multi-piece zirconia post-crown, a T-shaped nail design was recommended because it presented a lower mvM stress level in dentin compared with the tapered nail design.
References
Hanihara T, Ishida H (2005) Metric dental variation of major human populations. Am J Phys Anthropol 128:287–298. https://doi.org/10.1002/ajpa.20080
Pilloud MA, Hefner JT, Hanihara T, Hayashi A (2014) The use of tooth crown measurements in the assessment of ancestry. J Forensic Sci 59:1493–1501. https://doi.org/10.1111/1556-4029.12540
Cassetta M, Altieri F, Di Mambro A, Galluccio G, Barbato E (2013) Impaction of permanent mandibular second molar: a retrospective study. Med Oral Patol Oral Cir Bucal 18:e564–e568. https://doi.org/10.4317/medoral.18869
Goodacre CJ, Campagni WV, Aquilino SA (2001) Tooth preparations for complete crowns: an art form based on scientific principles. J Prosthet Dent 85:14. https://doi.org/10.1067/mpr.2001.114685
Govare N, Contrepois M (2020) Endocrowns: a systematic review. J Prosthet Dent 123(3):411-418.e9. https://doi.org/10.1016/j.prosdent.2019.04.009
Huang YC, Lin CL, Ko EW (2015) Effects of proximal grooves and abutment height on the resistance of resin-cemented crowns in teeth with inadequate resistance: an in vitro study. Biomed J 38:336–341. https://doi.org/10.4103/2319-4170.148905
Fei X, Wang Z, Zhong W, Li Y, Miao Y, Zhang L, Jiang Y (2018) Fracture resistance and stress distribution of repairing endodontically treated maxillary first premolars with severe non-carious cervical lesions. Dent Mater J 37:789–797. https://doi.org/10.4012/dmj.2017-203
Sedrez-Porto JA, de O da Rosa WL, da Silva AF, Münchow EA, Pereira-Cenci T (2016) Endocrown restorations: a systematic review and meta-analysis. J Dent 52:8–14. https://doi.org/10.1016/j.jdent.2016.07.005
Alcañiz M, Grau V, Monserrat C, Juan C, Albalat S (1999) A system for the simulation and planning of orthodontic treatment using a low cost 3D laser scanner for dental anatomy capturing. Stud Health Technol Inform 62:8–14
Parashis A, Tripodakis A (1994) Crown lengthening and restorative treatment in mutilated molars. Quintessence Int 25:167–172
Zou Y, Bai J, Xiang J (2018) Clinical performance of CAD/CAM-fabricated monolithic zirconia endocrowns on molars with extensive coronal loss of substance. Int J Comput Dent 21:225–232
Biacchi GR, Mello B, Basting RT (2013) The endocrown: an alternative approach for restoring extensively damaged molars. J Esthet Restor Dent 25:383–390. https://doi.org/10.1111/jerd.12065
Dartora G, Rocha Pereira GK, Varella de Carvalho R, Zucuni CP, Valandro LF, Cesar PF, Caldas RA, Bacchi A (2019) Comparison of endocrowns made of lithium disilicate glass-ceramic or polymer-infiltrated ceramic networks and direct composite resin restorations: fatigue performance and stress distribution. J Mech Behav Biomed Mater 100:103401. https://doi.org/10.1016/j.jmbbm.2019.103401
Zarow M, Devoto W, Saracinelli M (2009) Reconstruction of endodontically treated posterior teeth–with or without post? Guidelines for the dental practitioner. Eur J Esthet Dent 4:312–327
Helal MA, Wang Z (2019) Biomechanical assessment of restored mandibular molar by endocrown in comparison to a glass fiber post-retained conventional crown: 3D finite element analysis. J Prosthodont 28:988–996. https://doi.org/10.1111/jopr.12690
Forberger N, Göhring TN (2008) Influence of the type of post and core on in vitro marginal continuity, fracture resistance, and fracture mode of lithia disilicate-based all-ceramic crowns. J Prosthet Dent 100:264–273. https://doi.org/10.1016/S0022-3913(08)60205-X
Lü LW, Meng GW, Liu ZH (2013) Finite element analysis of multi-piece post-crown restoration using different types of adhesives. Int J Oral Sci 5:162–166. https://doi.org/10.1038/ijos.2013.50
Glantz PO (2000) Nilner K (1994) The devitalized tooth as an abutment in dentitions with a reduced but healthy periodontium. Periodontol 4:52–57. https://doi.org/10.1111/j.1600-0757.1994.tb00005.x
Glazer B (2000) Restoration of endodontically treated teeth with carbon fibre posts–a prospective study. J Can Dent Assoc 66:613–618
Luu KQ, Walker RT (1992) Corrosion of a nonprecious metal post: a case report. Quintessence Int 23:389–392
Meyenberg KH, Lüthy H, Schärer P (1995) Zirconia posts: a new all-ceramic concept for nonvital abutment teeth. J Esthet Dent 7:73–80. https://doi.org/10.1111/j.1708-8240.1995.tb00565.x
Habibzadeh S, Rajati HR, Hajmiragha H, Esmailzadeh S, Kharazifard M (2017) Fracture resistances of zirconia, cast Ni-Cr, and fiber-glass composite posts under all-ceramic crowns in endodontically treated premolars. J Adv Prosthodont 9:170–175. https://doi.org/10.4047/jap.2017.9.3.170
Dejak B, Młotkowski A (2013) 3D-Finite element analysis of molars restored with endocrowns and posts during masticatory simulation. Dent Mater 29:e309-317. https://doi.org/10.1016/j.dental.2013.09.014
Nakamura T, Imanishi A, Kashima H, Ohyama T, Ishigaki S (2001) Stress analysis of metal-free polymer crowns using the three-dimensional finite element method. Int J Prosthodont 14:401–405
Giannini M, Soares CJ, de Carvalho RM (2004) Ultimate tensile strength of tooth structures. Dent Mater 20:322–329. https://doi.org/10.1016/S0109-5641(03)00110-6
Ruse ND (2008) Propagation of erroneous data for the modulus of elasticity of periodontal ligament and gutta percha in FEM/FEA papers: a story of broken links. Dent Mater 24:1717–1719. https://doi.org/10.1016/j.dental.2008.04.006
Lin CL, Chang YH, Pai CA (2011) Evaluation of failure risks in ceramic restorations for endodontically treated premolar with MOD preparation. Dent Mater 27:431–438. https://doi.org/10.1016/j.dental.2010.10.026
Belli R, Wendler M, de Ligny D, Cicconi MR, Petschelt A, Peterlik H, Lohbauer U (2017) Chairside CAD/CAM materials. Part 1: measurement of elastic constants and microstructural characterization. Dent Mater 33:84–98. https://doi.org/10.1016/j.dental.2016.10.009
McComb D, Sirisko R, Brown J (1984) Comparison of physical properties of commercial glass ionomer luting cements. J Can Dent Assoc 50:699–701
Miura S, Yamauchi S, Kasahara S, Katsuda Y, Fujisawa M, Egusa H (2021) Clinical evaluation of monolithic zirconia crowns: a failure analysis of clinically obtained cases from a 3.5-year study. J Prosthodont Res 65:148–154. https://doi.org/10.2186/jpr.JPOR_2019_643
Tang W, Wu Y, Smales RJ (2010) Identifying and reducing risks for potential fractures in endodontically treated teeth. J Endod 36:609–617. https://doi.org/10.1016/j.joen.2009.12.002
Zurek AD, Alfaro MF, Wee AG, Yuan JC-C, Barao VA, Mathew MT, Sukotjo C (2019) Wear characteristics and volume loss of CAD/CAM ceramic materials. J Prosthodont 28:e510–e518. https://doi.org/10.1111/jopr.12782
Juloski J, Radovic I, Goracci C, Vulicevic ZR, Ferrari M (2012) Ferrule effect: a literature review. J Endod 38:11–19. https://doi.org/10.1016/j.joen.2011.09.024
Otto T, Mörmann WH (2015) Clinical performance of chairside CAD/CAM feldspathic ceramic posterior shoulder crowns and endocrowns up to 12 years. Int J Comput Dent 18:147–161
Dartora NR, de Conto Ferreira MB, Moris ICM, Brazão EH, Spazin AO, Sousa-Neto MD, Silva-Sousa YT, Gomes EA (2018) Effect of Intracoronal depth of teeth restored with endocrowns on fracture resistance: in vitro and 3-dimensional finite element analysis. J Endod 44:1179–1185. https://doi.org/10.1016/j.joen.2018.04.008
Guazzato M, Albakry M, Ringer SP, Swain MV (2004) Strength, fracture toughness and microstructure of a selection of all-ceramic materials. Part II Zirconia-based dental ceramics. Dent Mater 20:449–456. https://doi.org/10.1016/j.dental.2003.05.002
Eraslan O, Aykent F, Yücel MT, Akman S (2009) The finite element analysis of the effect of ferrule height on stress distribution at post-and-core-restored all-ceramic anterior crowns. Clin Oral Investig 13:223–227. https://doi.org/10.1007/s00784-008-0217-5
Owen TA, Barber M (2018) Direct or indirect post crowns to restore compromised teeth: a review of the literature. Br Dent J 224:413–418. https://doi.org/10.1038/sj.bdj.2018.218
Sahafi A, Peutzfeldt A, Asmussen E, Gotfredsen K (2004) Retention and failure morphology of prefabricated posts. Int J Prosthodont 17:307–312
Pontius O, Nathanson D, Giordano R, Schilder H, Hutter JW (2002) Survival rate and fracture strength of incisors restored with different post and core systems and endodontically treated incisors without coronoradicular reinforcement. J Endod 28:710–715. https://doi.org/10.1097/00004770-200210000-00008
Heydecke G, Butz F, Strub JR (2001) Fracture strength and survival rate of endodontically treated maxillary incisors with approximal cavities after restoration with different post and core systems: an in-vitro study. J Dent 29:427–433. https://doi.org/10.1016/s0300-5712(01)00038-0
Eskitaşcioğlu G, Belli S, Kalkan M (2002) Evaluation of two post core systems using two different methods (fracture strength test and a finite elemental stress analysis). J Endod 28:629–633. https://doi.org/10.1097/00004770-200209000-00001
Piconi C, Maccauro G (1999) Zirconia as a ceramic biomaterial. Biomaterials 20:1–25. https://doi.org/10.1016/s0142-9612(98)00010-6
Ozkurt Z, Işeri U, Kazazoğlu E (2010) Zirconia ceramic post systems: a literature review and a case report. Dent Mater J 29:233–245
Silva LS, Verri FR, Lemos CAA, Martins CM, Pellizzer EP, de Souza Batista VE (2021) Biomechanical effect of an occlusal device for patients with an implant-supported fixed dental prosthesis under parafunctional loading: A 3D finite element analysis. J Prosthet Dent 126:223.e1-e8. https://doi.org/10.1016/j.prosdent.2021.04.024
Mendonça JA, Francischone CE, Senna PM, Matos de Oliveira AE, Sotto-Maior BS (2014) A retrospective evaluation of the survival rates of splinted and non-splinted short dental implants in posterior partially edentulous jaws. J Periodontol 85:787–794. https://doi.org/10.1902/jop.2013.130193
Funding
This study was funded by the National Natural Science Foundation of China (grant number 81970927); the Medical Research Projects of the Health Department of Jiangsu Province (grant number M2020066); the Priority Academic Program Development of Jiangsu Higher Education Institutions (grant number 2018–87).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in the studies involving human participants were in accordance with the ethical standards of the institution and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the present study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Jiaxue Yang and Fei Han contributed equally to this work.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file2 (MP4 571 KB)
Rights and permissions
About this article
Cite this article
Yang, J., Han, F., Chen, C. et al. Comparison of stress distribution between zirconia/alloy endocrown and CAD/CAM multi-piece zirconia post-crown: three-dimensional finite element analysis. Clin Oral Invest 26, 5007–5017 (2022). https://doi.org/10.1007/s00784-022-04470-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-022-04470-5