Abstract
Cervical cancer is the most common cancer found in Indian women. Two human papillomavirus (HPV) vaccines were approved for use in India in 2006; however, neither has become readily accepted. Physician attitudes and recommendations are crucial in the uptake of HPV vaccines among adolescent women in the USA; thus, we ought to investigate provider attitudes and practices related to HPV vaccination in India via a survey administered to 210 Indian physicians. Of the 210 physicians, 46 % were community physicians and 54 % were academic physicians. The correct response to HPV knowledge questions was identified around 50 % of the time in 6/11 questions. Only 47 % of the physicians knew that there was an HPV vaccine approved for use in India. Only 11 % and 15 % of physicians strongly agree that the HPV vaccine will lead to long-lasting immunity and has a safe side effect profile, respectively. A total of 30 % of those surveyed reported that they would recommend the HPV vaccine to their patients, while 73 % agreed that the cost of the HPV vaccine is a major barrier to acceptance. After multivariate analysis, there were two significant variables independently associated with a physician’s decision to recommend HPV vaccine. These variables were as follows: “whether the vaccine was freely available from the government sector” and “uncertainty about whether HPV must be persistent to cause cervical cancer vs not.” Given the lack of knowledge among practicing physicians in Mangalore, increasing the education about HPV infection and HPV vaccination towards health care providers has the potential to increase vaccine recommendations.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Human papillomavirus (HPV)-related disease burden is a major public health problem worldwide [1]. Most cervical and anogenital cancers are associated with HPV infection. High-risk HPVs 16 and 18 are the most common subtypes found in cervical cancer, with up to 70 % of cervical cancers found with infection by one or both of these subtypes [2]. Cervical cancer is the most common cancer found in Indian women, and annually, there are approximately 132,000 new cases and 74,000 deaths in India [3]. It has been reported that cervical cancer accounts for 26 % of all cancer cases in Indian women, as well as 23 % of cancer deaths among these women [4].
Two HPV vaccines were approved for use in India in 2006; however, neither has become readily accepted due to a variety of reasons including the following: cost, stigma, lack of knowledge, efficacy, and safety concerns [5, 6]. The safety concerns were highlighted by a report in 2010 which stated that four tribal women had died due to adverse events of the vaccine during the HPV vaccine demonstration project led by a global nongovernmental organization. This report was followed by a suspension of the HPV vaccine demonstration projects while the claims were investigated. Although these reports that the HPV vaccine caused deaths have been disproved, many people in India still associate the HPV vaccine with serious adverse effects due to the negative media coverage [7, 8]. Regardless, the Indian Academy of Pediatrics (IAP) added HPV to their list of recommended vaccinations in 2008 [9].
Physician attitudes and recommendations are crucial in the uptake of HPV vaccines among adolescent women in the USA and Canada. Multiple reports have stated that physician recommendations are the strongest influence for parents deciding whether to vaccinate their children [10–12]. In fact, recent data in the USA has shown that the HPV vaccine has reduced the prevalence of HPV (types 6, 11, 16, 18) by 56 % among females aged 14–19 since the vaccine was approved in 2006 [11]. This data follows the trend reported by Australian researchers who stated that after the national government-funded vaccination program was introduced in 2007, there was a significant decrease in HPV (types 6, 11, 16, 18) prevalence [13]. However, data is limited in terms of provider attitudes and practices related to HPV vaccination in India, and recommendations for routine vaccination remain controversial [14, 15].
At present, the HPV vaccine is only approved as an optional vaccination for girls aged 9–26 in India under the private sector and is not covered by the Government of India’s Universal Immunization Program (UIP). The Universal Immunization Program in India provides vaccinations for tuberculosis, diphtheria, pertussis, polio, hepatitis B, measles, and tetanus to pregnant women and children [5]. Since the HPV vaccine is only covered by the private sector, it is expensive costing 12,000 INR (approximately $200 US dollars) for the three doses [4]. When this is taken into consideration with the annual per capita income in India of 61,564 INR (2011–2012), about 20 % of an average income would have to be used for the vaccine. Most cases of cervical cancer in India are detected in the advanced stages due to a lack of an optimal screening program and access to care for women [14, 16, 17].
Previous studies have investigated the attitudes of parents and children to the vaccination in India; however, data is very limited on physicians’ attitudes to HPV vaccination [5, 17, 18]. There are very few quantitative studies found on HPV vaccination acceptance in low- and middle-income countries (LMIC) although this is where the majority of cases of cervical cancer are found [19]. Some of these previous studies have shown that parental acceptance was higher if a physician recommended immunization; parental decisions to vaccinate their adolescent children were influenced by various factors such as awareness of the serious consequences of HPV infection, vaccine efficacy, personal knowledge of someone with cancer, and whether they believed that their children were at risk for acquisition of HPV infection or developing cervical cancer [17, 19–22]. Thus, this study aimed to investigate the knowledge and attitudes of practicing physicians in India regarding HPV and the potential for routine HPV vaccine implementation in India for adolescents and young women aged 9–26 years for whom it is currently licensed. In particular, we were interested in whether there was a difference in the knowledge and attitudes between community and academic physicians in regard to HPV, and also, what factors were significantly associated with a physician’s intention to vaccinate.
In our study, we defined “community physicians” as those who did not have any affiliation with academic institutions (teaching hospitals—private or government) and instead are private practitioners. The community physicians are typically located in the more rural areas of the country and care for underserved populations compared to the academic physicians. One recent report from the state of Karnataka, South India, found that none of the women surveyed in a rural setting had heard about HPV [23]. Another study from North India found that urban residents had higher knowledge regarding HPV and cervical cancer compared to rural residents [24]. We hypothesized that the knowledge of academic physicians in regard to HPV would be higher than that of the community physicians and that the intention to recommend the vaccine would be lower than that found in the USA or Canada. This study was meant to help elucidate factors that may deter physicians in Southern India from recommending the HPV vaccine to their patients.
Materials and Methods
Study Design
A cross-sectional survey of physicians was conducted between June 2013 and July 2013 in Mangalore, India, and the surrounding areas. Mangalore is a coastal city in the state of Karnataka in southern India. Karnataka has a population of 61,130,704 people (2011 census) which makes up 5 % of the total population of India. Mangalore is the administrative headquarters of the district Dakshina Kannada which makes up 3 % of the Karnataka population. The literacy rate of this district is 84 %, well above the Karnataka state average of 68 % [25]. The academic physicians who were surveyed were located within this district, whereas most of the community physicians were in the surrounding districts.
Physicians practicing in the fields of pediatrics, obstetrics/gynecology, family medicine, internal medicine, and homeopathic medicine were approached and asked to complete a one-time 45-question survey. There were no financial or material incentives provided for participation in the survey. The physicians chosen represented two categories of physicians practicing in India: solely community-based practitioners and institutionally tied academic practitioners. A total of 300 physicians were approached at every type of medical practice, both urban and rural, in the Mangalore area without discrimination and asked if they were interested in participation; 210 agreed to participate (70 %). Since medical school is conducted in English in India, there were no language barriers between the physician and the interviewer. After obtaining informed consent, the self-administered questionnaire was provided to be completed. In order to prevent response bias, interviews made clear that participation in the study was anonymous and confidential. The study has been approved by the Medical Ethics Committee at K.S. Hegde Medical Academy in Mangalore, India, as well as by the Institutional Review Board at Wake Forest School of Medicine.
Questionnaire
The survey was prepared in English and developed based on previous surveys regarding HPV knowledge and attitudes [5, 10, 26–35]. There were 45 questions divided into five categories consisting of (1) demographics (11 questions), (2) basic HPV knowledge (11 questions), (3) HPV vaccine knowledge (10 questions), (4) attitudes towards HPV vaccine recommendations (9 questions), and (5) attitudes towards discussing sexuality with patients (4 questions). The questions were presented with multiple choices answers to choose from.
Study Variables
The main outcome variable that was targeted was whether the physician would recommend the HPV vaccine to his/her patient. This was assessed by a direct question asking whether they would recommend this vaccine to their patients, with the response options of “yes,” “no,” or “sometimes.” Other variables used in the analysis were those that could influence a physician’s decision to recommend the HPV vaccine to his patients. They include multiple-choice questions regarding demographics, basic HPV knowledge, HPV vaccine knowledge, attitudes towards HPV vaccine recommendations, and attitudes towards discussing sexuality with patients.
Statistical Analysis
Data is presented as numbers (percentages) for categorical variables, unless otherwise stated. For unadjusted analysis, differences in demographic characteristics and physician knowledge between community and academic physicians were assessed using the chi-square and Fisher’s tests. A stepwise regression method was used to select variables to be included in the multivariable models, with age and sex forced into the final model. Other covariates were retained based on their associations with the outcome variable (physician’s recommendation of HPV vaccine to patient) in this cohort and in prior studies. Logistic regression analysis was used to estimate the odds of a physician recommending the HPV vaccine to his patients, with adjustment for potential factors that may influence the physician’s decision. Analyses were performed using SAS 9.3 (SAS Institute, Cary, NC). A P value ≤0.05 was considered statistically significant.
Results
Demographics
A total of 210 physicians, 46 % of whom were community physicians, completed the 45-question survey. Table 1 summarizes the demographics from these 210 surveys by physician type (community vs academic). A total of 57 % of participants were between 35-49 years old, with slightly more males than females participating. The physicians have been practicing mostly between 10 and 29 years with more practicing in urban vs rural practices. Obstetricians and Gynecologists represented 34 % and 22 % of Academic and Community physicians, respectively (P < 0.0001).
Basic HPV Knowledge
Table 2 demonstrates the knowledge of HPV among both academic and community physicians. HPV was correctly identified as a DNA virus by 48 % of all physicians while only 20 % identified that there were over 100 strains of HPV. A total of 58 % of all physicians surveyed believed that a patient must have a persistent HPV infection to cause cervical cancer. The correct response to questions was identified only around 50 % of the time in 6/11 questions among both groups. The significant differences in the responses between academic and community physicians were present in 6/11 questions as shown in Table 2; the non-significant data is not shown. Interestingly, community physicians correctly answered four of these six questions more frequently than the academic physicians.
HPV Vaccine Knowledge and Opinions
The knowledge of physicians in regard to the HPV vaccine was surveyed by 12 questions, as summarized in Table 3. Only 47 % of the physicians knew that there was an HPV vaccine approved for use in India, while 51 % of these physicians thought that the HPV vaccine would be helpful and effective in preventing cervical cancer. In total, 11 and 15 % of physicians strongly agree that the HPV vaccine will lead to long-lasting immunity and has a safe side effect profile, respectively. In this section of the survey, 9 of the 12 questions had definite correct answers, while 3 of the questions were opinion-based. Of the 9 questions with definite correct answers, only 2 were answered correctly by more than 50 % of the respondents. There were statistically significant differences in the responses between academic and community physicians in 2 of the 12 questions as shown in Table 3; the non-significant data is not shown. In these two questions, the academic physicians correctly answered that there are two vaccines approved for use and that one of the licensed vaccines can protect against up to four HPV strains more frequently than the community physicians.
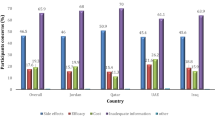
Attitudes Towards HPV Vaccine Recommendations
Fourteen questions were used to assess physicians’ attitudes towards HPV vaccination recommendations; the statistically significant questions are summarized in Table 4. Overall, 40 % of physicians strongly or somewhat agree that their colleagues would recommend the HPV vaccine, with 30 % reported that they would recommend the HPV vaccine to their own patients. Of the 14 % of respondents who said they would not recommend the vaccine, reasons included the following: cost (17 %), adverse side effects (7 %), doubt about efficacy (20 %), and not sure (48 %) among others. Only 31 % of physicians would recommend the HPV to their own children, while 26 % reported that they strongly or somewhat agreed that parents would accept the HPV vaccination for children under 14. A total of 40 % of physicians would recommend this vaccine to both female and male patients. There was a variable response in which specialty should be responsible for recommending this vaccine, with the highest percentage at 43 % believing it should be equal among pediatricians, internists, family practitioners, and OB/GYN physicians. Overall, 27 % of these physicians had been offered a continued medical education (CME) course on HPV (with 20 % attending), whereas 51 % of those who had not been offered a course were interested in one if it was available.
The cost of the HPV vaccine was thought to be a major barrier to its acceptance by 73 % of those surveyed. Overall, 75 % of the physicians were more likely to recommend the vaccine if it was freely available from the Government of India, while 53 % of physicians were still willing to recommend the vaccine if the patient was required to pay. There was a statistically significant difference between academic and community physicians in 4/12 questions as shown in Table 4. The academic physicians reported that they would not recommend the vaccine due to specific concerns such as cost, side effects, and efficacy, whereas the community physicians were not sure about why they would not recommend the vaccine, causing a statistically significant difference. However, the academic physicians were still more likely to recommend the vaccine even if patients were required to pay when compared the community physicians.
Attitudes Towards Discussing Sexuality with Patients
Four questions were used to assess the attitudes towards discussing sexuality with patients and are summarized in Table 5. Most physicians reported that they only discussed sexuality if the patient brings it up or if there is a specific problem (85 %). If the patient was under 18, 43 % of physicians discussed sexuality with the parents present, while 21 % discussed it with the patient alone. A total of 30 % of physicians thought that giving the HPV vaccine might make adolescents more promiscuous. Finally, 66 % of physicians thought that marketing the HPV vaccine as a cancer-preventing vaccine instead of a sexually transmitted infection-preventing vaccine would lead to higher acceptance. There was a statistically significant difference in responses by academic and community physicians in three out of four questions, which is shown in Table 5 The Academic Physicians were more likely to discuss sexuality with the patient alone, however also believed the vaccine could make patients more promiscuous more often than Community Physicians. Community Physicians did not believe that uptake would increase if the vaccine were marketed differently as much as the Academic Physicians did.
Multivariate Analysis
After multivariate analysis there were two significant variables that were independently associated with a physician’s decision to recommend HPV vaccine. These variable were: “whether the vaccine was freely available from the government sector” (P value 0.0098) and “uncertainty about whether HPV must be persistent to cause cervical cancer vs not” (P value 0.0001) (Table 6).
Discussion
The results of this study provide insight to the knowledge and attitudes that physicians in and around Mangalore, India, have in regard to HPV and the potential for an HPV vaccination implementation program. This group of physician participants has not previously been surveyed and suggests new ways to approach a routine HPV vaccination program in this country. Our study was focused on the overall knowledge and attitudes among physicians in Mangalore, Southern India, as well as investigating if any differences in knowledge and attitudes towards the HPV vaccine existed between academic and community physicians.
On a large scale, we found that the overall knowledge about HPV infection and vaccination is low among physicians in this region which is similar to reports from other regions of India [5, 19]. Several studies have shown that the acceptability of the HPV vaccine among parents and patients was high after explanation of HPV and its consequences [26, 29, 35]. However, we observed that many physicians in this district of India believed that most parents would not accept the HPV vaccination for children under 14 years old. Seventy-four percent of physicians surveyed were either neutral on the subject (30 %), somewhat disagreed (19 %), strongly disagreed (4 %), or were not sure (22 %) about parental acceptance of the vaccine. Importantly, there was no difference in the answers between community and academic physicians, implying that this may be a cultural barrier rather than an educational one.
A recent survey of 785 pediatricians from a national list of IAP members found that the pediatrician’s perceptions of HPV vaccine effectiveness and safety are significant predictors of HPV vaccine administration [6]. In this national survey of pediatricians, only 46 % report use of HPV vaccine routinely or selectively [6]. In the same study, pediatricians had a positive attitude towards HPV vaccine with over one half being of the opinion that the vaccine was safe whereas one third of those surveyed reported that the vaccine was effective.
These results should be considered in conjunction with the paper by Krupp et al. which surveyed physician knowledge in Mysore, India [5]. Their research was conducted in 2008 right after the IAP recommended routine use of the HPV vaccine among adolescents. In their paper, they found a low knowledge of HPV among physicians of varying specialties, similar to the results of our study. However, it is important to note that there has not been significant progress in the 5 years between these two studies. The impact of an HPV vaccination program will take years to realize, but it is imperative that this begin as soon as possible for the maximum effect. This must begin with education for physicians who can then disseminate accurate safety and efficacy data regarding HPV vaccine to their patients. We showed that there is a great interest for a continued medical education (CME) session on HPV information and vaccination.
It is also important to consider the results of our study with the recent paper by Pandey et al. which surveyed medical students at a premier medical school in close proximity to Mangalore [32]. Almost all of these students were well informed about HPV and its association with cervical cancer. The acceptance of the HPV vaccine among this group was 67.8 %. Our study demonstrates the impact that teaching has on future physicians’ knowledge and attitudes towards HPV. This further demonstrates that there is knowledge in the greater area around Mangalore about the importance of HPV vaccination which needs to be shared with the current practicing physicians through continued education.
Based on our study results, it is difficult to determine whether cost of the vaccine or issues surrounding physician recommendations are more important in determining HPV vaccine uptake in India. In general, although access to health insurance (self or employment-based financing) is on the rise in urban settings in India, out-of-pocket expenses are the primary mode of health care financing for most individuals both in urban and rural settings [36, 37]. The high cost of the HPV vaccine has been cited as a key barrier to vaccine uptake in some studies from India [18]. Strong advocacy to add the HPV vaccine to the Universal Immunization Program as well as physician education related to HPV, cervical cancer, and the benefits of vaccination must be addressed in order to increase vaccine uptake.
Our study was limited by a small sample size in a limited geographic region. Some of the non-significant findings may be attributed to the limited power of our analysis to detect a difference between the two groups of physicians. This study was a designed to be a small study in one region of Southern India; it will be important in the future to expand this research to a wider region of India to see if the results can be reproduced. We approached all clinics, hospitals, and other health care facilities in the area; however, there may be some bias in the response of physicians to the survey depending on what time and day we came to their place of work to conduct surveys.
Conclusions
Our study results provide insight on the knowledge and attitudes that physicians around Mangalore, India, have in regard to HPV and the potential for an HPV vaccination implementation program. This group of physician participants has not previously been surveyed and suggests new ways to approach a routine HPV vaccination program in India. Despite the general lack of knowledge among practicing physicians in Mangalore, it is promising that many physicians are interested in learning more about the subject. It will be important to consider factors that may influence a physician’s decision to recommend the HPV vaccine before a vaccination program can be started. It is important to begin increasing the knowledge of physicians in India about HPV in hopes of increasing the recommendation and acceptance of the vaccine among its vulnerable patients. Further studies with a larger sample size are needed to fully explore the knowledge, attitude, barriers, and practice of HPV vaccination among physicians in India.
References
Ferlay J et al (2010) Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer 127:2893–2917
Jemal A, et al. (2013) Annual report to the nation on the status of cancer, 1975-2009, Featuring the burden and trends in human papillomavirus (HPV)-associated cancers and HPV vaccination coverage levels. J Natl Cancer Inst.
Kaarthigeyan K (2012) Cervical cancer in India and HPV vaccination. Indian J Med Paediatr Oncol 33:7–12
Farhath SP, Vijaya PP, Mumtaj P (2013) Cervical cancer: is vaccination necessary in India? Asian Pacific J Cancer Prev 14:2681–2684
Krupp K et al (2010) Factors associated with intention-to-recommend human papillomavirus vaccination among physicians in Mysore, India. J Adolesc Health 46:379–384
Gargano LM et al (2013) Pediatricians’ perceptions of vaccine effectiveness and safety are significant predictors of vaccine administration in India. Int Health 5:205–210
Larson HJ, Brocard P, Garnett G (2010) The India HPV-vaccine suspension. Lancet 376:572–573
Sinha K (2010) Four deaths not due to flawed cervical cancer vaccine trial. The Times of India .
Consensus recommendations on immunization, 2008. Indian Pediatr 2008.45:635-648.
Duval B et al (2007) Vaccination against human papillomavirus: a baseline survey of Canadian clinicians’ knowledge, attitudes and beliefs. Vaccine 25:7841–7847
Markowitz L et al (2001) Reduction in human papillomavirus (HPV) prevalence among young women following HPV vaccination introduction in the United States, national health and nutrition examination surveys 2003-2010. J Infect Dis 208:385–393
Zimet GD (2005) Improving adolescent health: focus on HPV vaccine acceptance. J Adolesc Health 27:S17–S23
Tabrizi SN et al (2012) Fall in human papillomavirus prevalence following a national vaccination program. J Infect Dis 206:1645–1651
Nigam A et al. (2014) HPV vaccination in India: critical appraisal. ISRN Obstet Gynecol. 394595.
Das BC et al (2008) Prospects and prejudices of human papillomavirus vaccines in India. Vaccine 26:2669–2679
Saxena UC et al (2012) Evidence-based screening, early diagnosis and treatment strategy of cervical cancer for national policy in low- resource countries: example of India. Asian Pac J Cancer Prev 13:1699–1703
Madhivanan P et al (2014) Human papillomavirus vaccine acceptability among parents of adolescent girls: obstacles and challenges in Mysore, India. Prev Med 64:69–74
Belani HK et al (2014) Human papillomavirus vaccine acceptance among young men in Bangalore, India. Int J Dermatol 53:e486–e491
Tsu VD, Cernuschi T, LaMontagne DS (2014) Lessons learned from HPV vaccine delivery in low-resource settings and opportunities for HIV prevention, treatment, and care among adolescents. J Acquir Immune Defic Syndr 66:S209–S216
Trim K, Nagji N, Elit L, Roy K (2012) Parental knowledge, attitudes, and behaviors towards human papillomavirus vaccination for their children: a systematic review from 2001 to 2011. Obstet Gynecol Int. 92236.
Sam I, Wong L, Rampal S et al (2009) Maternal acceptance of human papillomavirus vaccine in Malaysia. J Adolesc Health 44:610–612
Brewer NT, Fazekas KI (2007) Predictors of HPV vaccine acceptability: a theory-informed, systematic review. Prev Med 45:107–114
Sasidharanpillai S, Bhat PV, Kamath V et al (2015) Knowledge, attitude and practices concerning human papilloma virus infection and its health effects among rural women, Karnataka, India. Asian Pacific J Cancer Prev 16:5053–5058
Hussain S, Nasare V, Kumari M et al (2014) Perception of human papillomavirus infection, cervical cancer and HPV vaccination in North Indian population. PLoS One 9:e112861
Census of India: size, growth, rate and distribution of population. Government of India: Ministry of Home Affairs 2011.
Carvalho NS et al (2009) Vaccinating against HPV: physicians’ and medical students’ point of view. Vaccine 27:2637–2640
Coleman MA, Levison J, Sangi-Haghpeykar H (2011) HPV vaccine acceptability in Ghana, West Africa. Vaccine 29:3945–3950
DiAngi YT et al (2011) A cross-sectional study of HPV vaccine acceptability in Gaborone, Botswana. PLoS One 6:e25481
Esposito S et al (2007) Pediatrician knowledge and attitudes regarding human papillomavirus disease and its prevention. Vaccine 25:6437–6446
Jaspers L et al (2011) Parental acceptance of human papillomavirus (HPV) vaccination in Indonesia: a cross-sectional study. Vaccine 29:7785–7793
Nnodu O et al (2010) Knowledge and attitudes towards cervical cancer and human papillomavirus: a Nigerian pilot study. Afr J Reprod Health 14:95–108
Pandey D et al (2012) Awareness and attitude towards human papillomavirus (HPV) vaccine among medical students in a premier medical school in India. PLoS One 7:1–5
Ragin CC et al (2009) Knowledge about human papillomavirus and the HPV vaccine--a survey of the general population. Infect Agent Cancer 4(Suppl 1):S10
Raley JC et al (2004) Gynecologists’ attitudes regarding human papilloma virus vaccination: a survey of fellows of the American College of Obstetrics and Gynecologists. Infect Dis Obstet Gynecol 12:127–133
Riedesel JM et al (2005) Attitude about human papillomavirus vaccine among family physicians. J Pediatr Adolesc Gynecol 18:391–398
Thomas KT, Sakthi VR (2011) Private health insurance in India evaluating emerging business models. J Health Manag 13:401–417
Roy K, Howard DH (2007) Equity in out-of-pocket payments for hospital care: evidence from India. Health Policy 80:297–307
Acknowledgments
We would like to thank all of the physicians who participated in this study and Nitte University for their support. We would also like to thank Ashwitha Fernandes for her language support without which this study would not have been possible.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Funding
Financial support was provided by the Infectious Disease Society of America Medical Scholars Program, the American Society for Tropical Medicine and Hygiene Benjamin Kean Fellowship, and the Wake Forest School of Medicine Pennell Pro Humanitate Vitae Fund. There are no financial conflicts of interests among the authors.
Rights and permissions
About this article
Cite this article
Canon, C., Effoe, V., Shetty, V. et al. Knowledge and Attitudes Towards Human Papillomavirus (HPV) Among Academic and Community Physicians in Mangalore, India. J Canc Educ 32, 382–391 (2017). https://doi.org/10.1007/s13187-016-0999-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13187-016-0999-0