Abstract
Traditional Chinese Medicine (TCM) includes both herbal remedies and non-herbal practices. Chinese cancer patients are particularly at high risk for herb–drug interactions. Providers, both primary care physicians and oncologists, frequently do not ask patients about TCM use, which has potentially dangerous consequences. This study describes an assessment of TCM use while undergoing conventional cancer treatment, among a cohort of Chinese immigrant cancer patients in New York City. The Immigrant Health and Cancer Disparities Service at Memorial Sloan–Kettering Cancer Center assists underserved cancer patients through a patient navigation program, the Cancer Portal Project. Six questions related to TCM are included in the existing Portal Needs Assessment Intake. Mandarin- or Cantonese-speaking Portal patients enrolled between January 2010 and May 2012 were surveyed. One hundred nine Chinese-speaking patients were enrolled in the Portal Project during the study period. Forty-six completed the TCM questions. Ninety-six percent preferred to speak Mandarin, Cantonese, or Fujianese in the healthcare setting. Thirty-nine percent (n = 18) of the 46 participants reported using TCM since being diagnosed with cancer. Nearly all (n = 16) who used TCM reported using herbal medicines. Ten TCM users did not describe sharing their use with Western doctors. Eight (44 %) of TCM users reported concurrently using TCM and conventional cancer treatment. Larger scale studies should further explore the concurrent use of TCM and conventional cancer treatment in this unique population. Future research should also address patient–provider communication related to the concurrent use of TCM and cancer treatment. This is also an important area of education for both patients and providers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
The use of complementary and alternative medicine (CAM), described as “health care practices and products that are not considered a part of conventional medicine due to insufficient evidence of their safety and efficacy,” has increased substantially in the USA [1]. Between the 2002 and 2007 National Health Interview Surveys, there has been a 14.2 % increase in use, from 25.7 to 29.4 % [1]. Asian Americans reported higher rates of CAM use (31.8 %) compared to other minority ethnic groups (African Americans—20.1 %; Hispanics—16.9 %) [1]. Among Chinese immigrant cancer patients in the West, use of CAM is as high as 47 % [2]. Traditional Chinese Medicine (TCM), a subset of CAM, is commonly used in East Asia as a complementary treatment among Chinese cancer patients receiving conventional treatment [3, 4]. TCM has a recorded history of more than 5,000 years, and includes a wealth of documented therapeutic resources; TCM encompasses both herbal remedies and a broad range of non-herbal practices and philosophies [3, 5]. TCM has been used by traditional Chinese practitioners for many years with proven efficacy [5]. Many patients use TCM to improve symptoms, enhance “vital energy” by restoring “balance,” boost immunity or detoxify, diminish conventional treatment side effects, use a less potentially harmful treatment than conventional treatment, regain a sense of control, and help accept death [3, 6, 7].
Several studies discuss TCM, especially the use of herbal medicines, within the broader category of CAM. In a study of CAM use among cancer patients from diverse ethnic groups identified through the Hawaii Tumor Registry, 24.7 % of 1,168 respondents reported use of at least one type of CAM since being diagnosed [8]. Twenty-five percent of Chinese patients reported CAM use, and were more likely to use herbs than any other ethnic group [8]. In Canada, Ferro et al. studied newly diagnosed Chinese cancer patients and found that 47 % used CAM; herbal remedies were most common (61 %) [2]. In a California study, using the regional tumor registry (operated by the Northern California Cancer Center), of the prevalence of concurrent use of conventional and alternative treatments for cancer by ethnicity (Chinese, Latino, White, Black), Lee et al. found that among 379 breast cancer patients, 48 % used at least one type of CAM and approximately one third used two types after being diagnosed [9]. Twenty-two percent of Chinese patients used herbal therapies [9]. Chinese patients were twice as likely to use this treatment modality compared to the other ethnic groups [9]. Forty-one percent of Chinese women had received chemotherapy and 17 % hormonal therapy in this study, although the specific overlap between herbal use and chemotherapy/hormonal use was not specified [9]. In a study of cancer pain among 170 Chinese cancer patients at an oncology practice in Manhattan's Chinatown, 11.2 % used Chinese herbal medicine for pain [10]. Sixty-five percent of patients in the study had received chemotherapy since diagnosis, but concurrent use of herbal medicine and chemotherapy was not detailed [10]. An earlier study in Taiwan described that 66 % of cancer patients took Chinese herbal medicine while receiving chemotherapy [5].
Many herbal remedies are metabolized by the hepatic P450 cytochrome system; the potential for herb–chemotherapy drug interactions is significant [3]. With the reported increased use of herbal remedies and the frequent lack of communication between patients and physicians regarding herb use (>90 %) [11], there is a growing risk of herb–anticancer drug interactions [12–16]. These can lead to substantial unexpected chemotherapeutic agent toxicities, and, just as concerning, potential undertreatment [17]. There is also risk for direct herb-related toxicities, including hepatic, renal, hematopoietic, cardiovascular, and neuropsychiatric [3]. Reported clinical herb–anticancer drug interactions include St. John's wort (Guan ye lian qiao) with irinotecan, a DNA topoisomerase I inhibitor used to treat advanced colorectal and lung cancer; St. John's wort with imatinib, a tyrosine kinase inhibitor used to treat Philadelphia-positive hematological malignancies; and garlic with docetaxel, a semi-synthetic taxane used to treat breast, lung, stomach, prostate, and head and neck cancers [12, 13]. Treatment with St. John's wort has been shown to decrease the plasma levels of the active metabolite of irinotecan, SN-38, by 42 % [14], and increase clearance of imatinib by 43 % [15]. Garlic has been shown to decrease the mean clearance of docetaxel in patients with metastatic breast cancer [16]. There is evidence from in vitro studies and animal models that Asian ginseng has immunostimulatory properties, which may interfere with the immunosuppressive effects of corticosteroids [18]. Cordyceps (dong chong xia cao), in studies conducted on human leukemic cell lines and animal models, has been shown to have immunoregulatory properties, and may similarly interact with corticosteroid treatment [18].
Chinese cancer patients are an understudied, underserved group with a high rate of varied cancers [19], at particularly high risk for herb–drug interactions. Despite high herb use, providers commonly do not ask patients about use, which has potentially dangerous consequences [9, 20]. In the study described above by Lee et al., only half of CAM users reported discussing use with their providers [9]. Among 198 Chinese primary care patients with high herb use, only 5 % had physicians who ever asked about use of CAM [20]. There is an expected future shortage of oncologists in the USA, as the cancer burden increases and the demand for oncology service grows [21]. The care of cancer patients during the active phase of treatment often requires the fulfillment of multiple, complex roles [21]. Primary care physicians (PCPs) already have an active role in cancer care, and their increasing role in cancer patient management is anticipated [21]. Klabunde et al. described a national survey of physicians caring for cancer patients (1,694 PCPs and 1,621 oncologists) conducted by the Cancer Care Outcomes Research and Surveillance Consortium [21]. The authors found that assessing patients for treatment preferences was the most commonly reported cancer care role in which PCPs participated (64.2 %) [21]. Asking patients about herbal medicine use in the context of a discussion about treatment preferences is a potentially critical opportunity for PCPs to reduce the risk of adverse herb–drug interactions.
This study describes an assessment of TCM use while undergoing conventional cancer treatment, among a cohort of Chinese immigrant cancer patients in New York City.
Design and Participants
The Immigrant Health and Cancer Disparities Service at Memorial Sloan–Kettering Cancer Center (MSKCC) assists underserved and minority cancer patients through an ongoing, individualized patient navigation/case management program, the Cancer Portal Project. The Portal Project provides cancer patients with social and economic assistance, including financial support, transportation assistance, legal advice, assistance with health insurance, food support and nutritional information, and referrals to cancer support and informational services [22]. The Portal Project is a service program implemented at 10 New York City hospital-based cancer clinics. The project received exemption from the MSKCC Institutional Review Board.
Six questions related to TCM are included in the existing Portal Needs Assessment Intake Form. Mandarin- or Cantonese-speaking Portal patients who were enrolled in the program between January 2010 and May 2012 were surveyed by bilingual staff. Staff completed the survey in person or administered the survey over the phone, if that was necessitated by the patient's schedule. The Intake Form includes items related to sociodemographics, preferred language for healthcare, years in the USA, and cancer diagnosis. The questions related to TCM queried patients about their use of TCM since being diagnosed with cancer, including the type of TCM used (i.e., traditional Chinese herbal medicines; traditional Chinese treatments such as acupuncture, acupressure, moxibustion), frequency of use, intended outcome of use, source of TCM (i.e., TCM doctor, TCM pharmacy, self “prescribed”), and whether use of TCM was shared with patients' Western medical doctors (i.e., medical oncologists, radiation oncologists, primary care physicians) and/or nurses. If Chinese herbs were used, patients were asked if they ever used herbs at the same time (same day or within 1 week) that they received cancer treatment (chemotherapy, radiation therapy, oral cancer medication, other Western cancer treatment i.e., hyperthermia, photodynamic therapy, laser therapy, gene therapy). Finally, patients were queried on whether they were ever advised not to use TCM by a Western doctor, and if they would be interested in learning more about TCM and potential interactions with cancer treatment, as well as potential toxicities due to TCM. Questions were developed based on prior qualitative work exploring the needs of Chinese immigrant cancer patients [23].
Descriptive analysis was conducted to examine sociodemographic characteristics, use of TCM and for what purposes, and use of Chinese herbs while undergoing conventional cancer treatment. Chi-square tests were performed to assess correlations between TCM use and sociodemographic factors.
Results
One-hundred and nine Chinese-speaking patients were enrolled in the Cancer Portal Project between January 2010 and May 2012. Forty-six completed the TCM questions. At the end of the Portal enrollment process, the remainder did not have time or could not be reached in follow-up if the TCM questions were not completed as part of the original intake, and one refused to complete the Intake Form. Sixty-one percent of TCM respondents were female. Eighty-nine percent were born in China, and 11 % in Malaysia. Sixty-seven percent had been living in the USA for 15 years or less. Ninety-six percent preferred to speak Mandarin, Cantonese, or Fujianese in the healthcare setting. Forty-six percent had less than a high school education. Seventy-eight percent were insured; among those insured, 58 % had Medicaid for Emergency Services. Forty-one percent had a PCP. The most common cancer diagnoses among participants were breast (41 %), gastric (13 %), head and neck (11 %), colorectal (9 %), and gynecological (9 %) (Table 1).
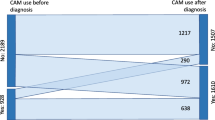
Thirty-nine percent (n = 18) of the 46 participants reported that they had used TCM since being diagnosed with cancer. Nearly all who used TCM reported using herbal medicine (n = 16) or “herbs and pills” (n = 1). One patient responded “don't know” to the type of TCM used. Most commonly reported herbs included lingzhi mushroom, cordyceps (dong chong xia cao), and ginseng. People who used TCM reported frequent use; 13 of the 18 respondents who used TCM reported using 1–2 times per day. Eleven reported they were currently using TCM. Most common reasons for using TCM included the following: to directly treat cancer (n = 5), to treat the side effects of cancer treatment (n = 4), and to boost the immune system/combat fatigue (n = 6). Most TCM users (n = 10) reported obtaining TCM from TCM pharmacies. Eight TCM users described sharing their use with Western medical doctors (four of whom were medical oncologists, one radiation oncologist, three missing type of doctor), eight reported not sharing use (one responded “don't know,” one refused). The eight TCM users who described not sharing TCM use with Western doctors reported that they did not see any reason to do so (n = 4), doctor did not ask (n = 2), doctor would not understand/doctor would disapprove (n = 1), doctor would not understand/hard to explain as doctor does not speak patient's language (n = 1) (Table 2).
Eight (44 %) of TCM users responded that they had concurrently used TCM (i.e., on the same day or within 1 week) of receiving conventional cancer treatment. Five patients reported taking TCM while receiving chemotherapy, either on the same day as chemotherapy or within 1–3 days (two of whom were also receiving radiation therapy and/or oral cancer medications). One patient did not know when he/she took TCM in relation to chemotherapy and radiation therapy, but took TCM “as needed” during those treatments. Two patients took TCM while taking oral cancer medications. Three of the eight patients who reported concurrent use of TCM and conventional treatment were advised by their physicians to discontinue TCM, two followed this advice to stop TCM, and one continued TCM use despite the advice (Table 2).
All participants were asked if they had ever been advised by a physician not to use TCM for any reason; 11 responded “yes,” and reasons they were given included that TCM would conflict with chemotherapy or radiation. Finally, all participants were queried on whether they would be interested in learning more information about TCM and potential interactions with cancer treatment, as well as potential toxicities; 48 % responded in the affirmative. Twenty-four percent were interested in a written brochure on the topic, 17 % in one-on-one information sessions, 15 % in lectures/group information sessions, and 11 % in online information.
There were no significant differences in the sociodemographic characteristics or type of cancer diagnosis between users and non-users of TCM.
Conclusions
In this assessment of TCM use among a cohort of Chinese immigrant cancer patients participating in an ongoing patient navigation program, we found a high rate of TCM use, nearly all of which was reported as the use of herbal medicines. Furthermore, while close to half of TCM users reported using TCM concurrently with conventional anticancer treatment, including chemotherapy, more than half of TCM users did not describe sharing their TCM use with their Western doctors. Among patients who did share TCM use with their Western doctors, none did so with a PCP. Less than a third of all participants reported ever being advised against TCM use by their physicians. There was also a high degree of interest in educational programs and initiatives on TCM, its potential interactions with cancer treatment, and its potential toxicities.
The current study provides important insight into the concurrent use of TCM and conventional cancer treatment. Two of the most commonly reported herbs in this assessment, cordyceps and ginseng, may interfere with the immunosuppressive activity of corticosteroids [18]. Corticosteroids are commonly used in cancer treatment regimens. This finding is therefore potentially significant for large numbers of cancer patients, with Chinese patients at particular risk given the high rates of TCM use in this population. There are also additional potential anticancer drug interactions with ginseng. American and Asian ginseng may increase the risk of rituximab-induced hypoglycemia, and may potentiate the monoamine oxidase inhibiting effect of procarbazine [18]. Evidence related to Siberian ginseng is conflicting, with some evidence suggesting that plasma levels of anticancer drugs that are substrates of the cytochrome P450 isozymes CYPA12, 2C9, and 3A4 may be increased due to inhibition of these isozymes, while other studies have found that Siberian ginseng is not likely to inhibit these isozymes in vitro [18].
This study was limited by its small sample size. Also, our sample was potentially biased as participants were surveyed from a cohort of patients already enrolled in a navigation program based at 10 hospital-based cancer clinics. Patients in our sample may have been significantly more tied into the Western health care system, by virtue of their establishment of their medical care at large medical centers. These patients may have been less likely to use TCM, or be more likely to encounter discouragement of TCM use from their physicians and nurses. Alternatively, given the lower likelihood of having a Chinese-speaking physician at a hospital-based clinic (i.e., versus an oncologist with a practice based in a Chinese immigrant neighborhood), patients may have been less likely to discuss TCM with their physicians, and the physicians may be less familiar with TCM and less likely to ask about its use, resulting in continued patient use and lack of communication about TCM. Future studies assessing TCM use among Chinese cancer patients should recruit from diverse clinical and community sites, including community-based oncologists and community cancer support organizations.
Larger scale studies should further explore the concurrent use of TCM and conventional cancer treatment in this unique population, and should delve further into the details of the specific herbs and anticancer drugs used, patterns of use, and reasons for use, as well as clinical observations (i.e., through chart review) of possible herb–anticancer drug interactions and herb-related toxicities. Future research should also address patient–provider communication related to concurrent use of TCM and conventional cancer treatment. This is also an important area of education for patients and providers, including PCPs. Programs should be developed to educate patients about herb–anticancer drug interactions and herb-related toxicities, and to improve patient understanding of herbs as having potentially significant biological effects, akin to other prescribed medications that should therefore be similarly discussed with providers. Patients should also be educated and empowered to actively participate in their medical care, including how to ask questions and communicate about complex issues or culturally specific practices such as TCM, in the interpreted medical encounter. Provider education is equally important; in particular, the inclusion of PCPs is essential and should not be overlooked. In the survey conducted by the Cancer Care Outcomes Research and Surveillance Consortium, over three quarters of PCPs reported fulfilling at least one of seven cancer care roles examined, mainly in a co-management capacity with oncologists [21]. The roles of PCPs and cancer specialists appeared to be complementary in this study [21]; educational initiatives should consider this pattern of care in educating both PCPs and cancer specialists about discussing TCM use with their patients. As PCPs most commonly reported their involvement in cancer care as the assessment of patients' treatment preferences [21], asking patients about their use of TCM could be a natural part of a dialogue on treatment. Educational initiatives should inform providers about the variety and intended purpose of TCM practices, herb–anticancer drug interactions and herb-related toxicities, and emphasize the importance of asking patients about TCM use and addressing concurrent TCM and anticancer drug use in a culturally responsive manner.
References
Su D, Li L (2011) Trends in the use of complementary and alternative medicine in the United States: 2002–2007. J Health Care Poor Underserved 22(1):296–310. doi:10.1353/hpu.2011.0002
Ferro MA, Leis A, Doll R, Chiu L, Chung M, Barroetavena MC (2007) The impact of acculturation on the use of traditional Chinese medicine in newly diagnosed Chinese cancer patients. Support Care Cancer 15(8):985–992. doi:10.1007/s00520-007-0285-0
Chiu J, Yau T, Epstein RJ (2009) Complications of traditional Chinese/herbal medicines (TCM)—a guide for perplexed oncologists and other cancer caregivers. Support Care Cancer 17(3):231–240. doi:10.1007/s00520-008-0526-x
Abdullah AS, Lau Y, Chow LW (2003) Pattern of alternative medicine usage among the Chinese breast cancer patients: implication for service integration. Am J Chin Med 31(4):649–658
Liu JM, Chu HC, Chin YH, Chen YM, Hsieh RK, Chiou TJ, Whang-Peng J (1997) Cross sectional study of use of alternative medicines in Chinese cancer patients. Jpn J Clin Oncol 27(1):37–41
Deng G, Cassileth BR, Yeung KS (2004) Complementary therapies for cancer-related symptoms. J Support Oncol 2:419–426
Gerber B, Scholz C, Reimer T, Briese V, Janni W (2006) Complementary and alternative therapeutic approaches in patients with early breast cancer: a systematic review. Breast Cancer Res Treat 95(3):199–209. doi:10.1007/s10549-005-9005-y
Maskarinec G, Shumay DM, Kakai H, Gotay CC (2000) Ethnic differences in complementary and alternative medicine use among cancer patients. J Altern Complement Med 6(6):531–538
Lee MM, Lin SS, Wrensch MR, Adler SR, Eisenberg D (2000) Alternative therapies used by women with breast cancer in four ethnic populations. J Natl Cancer Inst 92(1):42–47
Dhingra L, Lam K, Homel P, Chen J, Chang VT, Zhou J, Chan S, Lam WL, Portenoy R (2011) Pain in underserved community-dwelling Chinese American cancer patients: demographic and medical correlates. Oncologist 16(4):523–533. doi:10.1634/theoncologist.2010-0330
Saw JT, Bahari MB, Ang HH, Lim YH (2006) Potential drug–herb interaction with antiplatelet/anticoagulant drugs. Complement Ther Clin Pract 12(4):236–241. doi:10.1016/j.ctcp.2006.06.002
Yang AK, He SM, Liu L, Liu JP, Wei MQ, Zhou SF (2010) Herbal interactions with anticancer drugs: mechanistic and clinical considerations. Curr Med Chem 17(16):1635–1678
American Cancer Society. Guide to Cancer Drugs. 2012. http://www.cancer.org/treatment/treatmentsandsideeffects/guidetocancerdrugs/docetaxel?url=http%3A www.cancer.org/treatment/treatmentsandsideeffects/guidetocancerdrugs/docetaxel. Accessed May 2013
Mathijssen RH, Verweij J, de Bruijn P, Loos WJ, Sparreboom A (2002) Effects of St John's wort on irinotecan metabolism. J Natl Cancer Inst 94(16):1247–1249
Frye RF, Fitzgerald SM, Lagattuta TF, Hruska MW, Egorin MJ (2004) Effect of St John's wort on imatinib mesylate pharmacokinetics. Clin Pharmacol Ther 76(4):323–329. doi:10.1016/j.clpt.2004.06.007
Cox MC, Low J, Lee J, Walshe J, Denduluri N, Berman A, Permenter MG et al (2006) Influence of Garlic (Allium sativum) on the pharmacokinetics of docetaxel. Clin Cancer Res 12(15):4636–4640. doi:10.1158/1078-0432.ccr-06-0388
Meijerman I, Beijnen JH, Schellens JH (2006) Herb–drug interactions in oncology: focus on mechanisms of induction. Oncologist 11(7):742–752. doi:10.1634/theoncologist.11-7-742
Yap KY, See CS, Chan A (2010) Clinically relevant chemotherapy interactions with complementary and alternative medicines in patients with cancer. Recent Pat Food Nutr Agric 2(1):12–55
McCracken M, Olsen M, Chen MS Jr, Jemal A, Thun M, Cokkinides V, Deapen D, Ward E (2007) Cancer incidence, mortality, and associated risk factors among Asian Americans of Chinese, Filipino, Vietnamese, Korean, and Japanese ethnicities. CA Cancer J Clin 57(4):190–205
Wu AP, Burke A, LeBaron S (2007) Use of traditional medicine by immigrant Chinese patients. Fam Med 39(3):195–200
Klabunde CN, Ambs A, Keating NL, He Y, Doucette WR, Tisnado D, Clauser S, Kahn KL (2009) The role of primary care physicians in cancer care. J Gen Intern Med 24(9):1029–1036. doi:10.1007/s11606-009-1058-x
Gany F, Ramirez J, Nierodzick ML, McNish T, Lobach I, Leng J (2011) Cancer portal project: a multidisciplinary approach to cancer care among Hispanic patients. J Oncol Pract 7(1):31–38. doi:10.1200/JOP.2010.000036
Leng J, Lee T, Sarpel U, Lau J, Li Y, Cheng C, Chang MD, Gany F (2012) Identifying the informational and psychosocial needs of Chinese immigrant cancer patients: a focus group study. Support Care Cancer 20(12):3221–3229. doi:10.1007/s00520-012-1464-1
Acknowledgments
The authors gratefully acknowledge Michell Chang-Qui, Maria Xia, and Mei Hsuan Chen for their assistance with data collection and data entry for this study. This study was conducted with funding from NCI grant #U54-13778804-S2.
Conflict of Interest
None of the authors have any conflicts of interest
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Leng, J.C.F., Gany, F. Traditional Chinese Medicine Use among Chinese Immigrant Cancer Patients. J Canc Educ 29, 56–61 (2014). https://doi.org/10.1007/s13187-013-0542-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13187-013-0542-5