Abstract
Purpose
The Chinese immigrant community faces multiple barriers to quality cancer care and cancer survivorship. Psychosocial interventions can positively impact quality of life, anxiety, and distress in cancer patients. In this study, we explored the informational and psychosocial needs of Chinese cancer patients to inform the development of culturally targeted support and survivorship interventions.
Methods
We conducted four focus groups with a total of 28 Chinese cancer patients to elucidate their cancer informational and psychosocial needs. The groups were conducted using standard methodology and guided by community-based participatory research principles. Sessions were audio recorded, transcribed, and translated into English. The research team conducted the analysis.
Results
Frequently occurring themes included (1) the need for accurate information on cancer and treatment options, (2) the role of language barriers in accessing cancer care, (3) the role of food in cancer and the need for nutritional information, and (4) the role of Chinese medicine in cancer treatment. Participants expressed significant dissatisfaction with the amount, reliability, and/or comprehensibility of available information.
Conclusions
Support groups and programs should be developed to address participants’ needs for more information on cancer and its treatment. Programs should educate and empower patients on how to find further Chinese language information and resources and effectively communicate their questions and needs to providers in an interpreted encounter. System-level approaches should be implemented to ensure provision of interpretation services. Additionally, programs should incorporate the unique cultural needs of this population related to food/nutrition and Chinese medicine.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Each day, an average of 3,100 immigrants arrive in the U.S.A. where approximately 13 % of the population is foreign born [1, 2]. In the New York State alone, 22 % of the population is immigrant, 9 % of whom are Chinese, the largest of the Asian immigrant subgroups [3]. Of New York’s Chinese population, 74 % are immigrants and nearly 84 % (434,000) reside in New York City (NYC) [3].
While Asian-Americans are at lower risk for certain cancers, they have higher rates of gastric, liver, cervical, and nasopharyngeal cancers [4]. Asian-Americans/Pacific Islanders have higher stomach, liver, and cervical cancer mortality rates than non-Hispanic Whites and are the only major U.S. population group for whom the annual number of cancer deaths is greater than that for heart disease [5]. While disaggregated national data on the major Asian ethnic groups are not routinely available, in California, Chinese-Americans have higher rates of liver, colorectal, and lung cancer than other Asian groups, and Chinese women have the highest lung cancer mortality rate [5]. Breast cancer is the most commonly diagnosed cancer among Chinese women, and 5-year survival rates among Chinese immigrants have been shown to be lower than among U.S.-born Chinese women [6–8].
Cancer survivorship, an area of growing clinical and research importance, is defined as the physical, psychosocial, and economic issues related to cancer, from diagnosis through treatment and end-of-life care [9]. An increasing number of people are living many years after a cancer diagnosis; approximately 65 % of them are expected to live at least 5 years [10]. Stark inequalities continue to exist in the quality of life for minority cancer survivors both during and after treatment [11].
The Chinese immigrant community faces multiple barriers to both cancer care and a high quality of life in cancer survivorship. Stigma attached to cancer, misconceptions about cancer symptoms and severity, and overall limited knowledge about cancer and its treatment, combined with lack of knowledge about how to navigate health care systems, lack of resources to access cancer support groups, and linguistic, cultural, and financial barriers, make this group particularly vulnerable [11–16].
More than 45 % of NYC’s Chinese population is limited English proficient [17]. The inability to communicate in English often prevents Chinese immigrants from obtaining appropriate medical attention [14, 18]. Language and communication are especially crucial in effective delivery of cancer care, given that the information transferred from physician to patient is often complex and potentially distressing in nature [19, 20]. Cultural barriers, which often coexist with language barriers, play an important role in their own right. For Chinese patients diagnosed with cancer, cultural factors such as religious fatalism, concerns about distracting physicians from treating the disease, and the “desire to be good” have been cited as barriers to proper pain management [21, 22]. Suboptimal pain management can in turn contribute to lower quality of life [22]. Lin et al. also found that cultural concerns were accountable for reduced treatment seeking and participation in clinical trials among Chinese immigrants [23]. In addition, Chinese patients may often be passive in the health care system, as doctors are traditionally seen as authorities who should not be questioned or challenged [12]. These factors contribute to the overall reduced health literacy common among Asian-American immigrants [24, 25].
Approximately one-third of cancer patients with significant psychological distress are in need of psychological interventions [26]. It has been well documented that psychosocial interventions (behavioral therapy, educational therapy, psychotherapy, and support groups) can positively impact quality of life, anxiety, distress, and pain in patients with cancer [26–29]. Minorities, however, are less likely to participate in social support initiatives. This is likely due, in part, to a lack of interventions that address and incorporate minorities’ “social environments,” the importance of which is described by Guidry et al. [11]. There are limited data on the impact of Chinese support groups on psychosocial outcomes and quality of life [30, 31]. Chinese patients, for whom “losing face” may include loss of self-control in public, may find support groups with an educational focus especially useful in providing a safe distraction for emotional expression [32]. In a qualitative study of the experience of illness for Chinese women with breast cancer, Lam and Fielding demonstrated that women without visible physical changes would try to keep their illness a secret to avoid stigmatization rather than seek social support from peer groups [12]. For these women who lack support from their core social resources, support groups may be particularly valuable [12]. Education-based support groups have been demonstrated to be more effective than groups focused on peer discussion of positive and negative thoughts on improving both mental health and physical scores [33]. While similar studies among Chinese patients have not been conducted, the Virtual Community for Immigrants with Cancer demonstrated that Spanish-speaking patients participating in online support groups prefer to start their groups with cancer-related specific information [34]. This approach may make it easier for patients to express emotions in the context of the presented information [34].
This focus group study explored the needs of a diverse group of Chinese immigrant cancer patients in New York City. The primary objective was to gain knowledge of their informational and psychosocial needs that could be used to inform the development of culturally targeted education-based support and survivorship interventions.
Methods
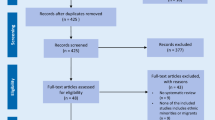
IRB approval was obtained. Focus groups were based on standard methodology for planning and designing the focus group study, developing a focus group guide, recruiting participants, selecting facilitators, and analyzing the results [35]. The study was guided by community-based participatory research principles [35, 36]. Community-based research is a collaborative method that equitably and actively engages community members, organizational representatives, and researchers in all phases of the research process [36]. In particular, community-based research builds on the strengths and resources within the community, promotes a colearning and empowering process that attends to social inequalities, and disseminates findings and knowledge gained to all partners [36]. Chinese survivors, community-based organizations, and health care providers serving Chinese immigrants with cancer contributed to the development, implementation, and analysis of the study. A key partner was the American Cancer Society (ACS) Asian Initiatives located in Flushing, Queens, the largest Chinese immigrant neighborhood in NYC. Focus group guide topic areas included the need for clinical cancer care information, the need for information on ancillary cancer care services, the need for general health care system information, and the need for emotional and social support. Each topic area included a set of questions, asked across all the groups. The topic related to the need for clinical cancer care information was the most lengthy (18 questions), 8 questions were asked related to ancillary care, 2 related to general health care, and 12 related to emotional and social support.
Two bicultural Mandarin- and Cantonese-speaking facilitators were trained in focus group methodology using a curriculum developed and tested with immigrant communities [35]. Participants were recruited from the community by a cancer support organization and through the surgical oncology clinic of a large NYC municipal hospital. Recruitment flyers and a telephone screening questionnaire were utilized. Participants were provided with an information sheet in Chinese describing the purpose of the focus groups and what the study would entail, and study staff responded to any questions, ensured that the presented information was understood, and verbally consented participants. To maintain complete anonymity of the participants, written consent was not obtained, as there was the perceived potential for legal, social, or economic risk in signing a consent form for any of the participants whose immigration status may have been undocumented. Inclusion criteria were (1) non-U.S. born, (2) of Chinese descent, (3) primary language not English, (4) proficiency in Mandarin or Cantonese, (5) age 21 through 80 years, and (6) diagnosis of cancer (any type).
Groups were held at ACS Asian Initiatives offices and at the NYC municipal hospital from where patients had been recruited. Each group interview was 90 min in length and conducted in Mandarin or Cantonese by trained facilitators and recorders. In addition to the facilitator, two recorders were present at each focus group to take detailed notes on the order of speakers and any significant nonverbal cues [37]. The Mandarin- and Cantonese-speaking groups were held separately, except for one mixed group with a trilingual facilitator who fostered discussion between the Mandarin- and Cantonese-speaking participants. Groups included patients of mixed cancer diagnoses but were single gender to encourage open discussion if sensitive issues were raised related to gender-specific diagnoses. Sessions were audio recorded and transcribed and were then translated into English and checked by a professional and community translator. The initial analysis was conducted by two of the authors (JL, TL), using inductive analysis techniques. Inductive analysis requires that categories, patterns, and themes come from the data; this iterative process then results in a coding scheme [38]. After the coding scheme was developed, the transcripts were reread and coded. The process of coding permitted reviewers to closely examine the prominent issues brought up in the focus groups as well as a chance to identify specific subtopics. A third author (FG) reviewed the codes. Results were discussed (JL, TL, FG), disagreements on coding were resolved, and key themes were elucidated. Each of the reviewers also selected quotations to illustrate the key themes.
Results
Four focus groups were conducted with Chinese cancer patients who were fluent in Mandarin, Fujianese, and/or Cantonese (Fujianese patients were also fluent in either Mandarin or Cantonese). A total of 28 patients participated. One group was held with women, and three groups were held with men. Patients’ age ranged from 38 to 79 (mean 57, standard deviation 10.1). Table 1 summarizes the participants’ demographic characteristics. All participants were immigrants from Asia, predominately China, Taiwan, and Hong Kong (89 %), and most commonly diagnosed with breast (25 %) or liver (32 %) cancer. Eighty-one percent of them were currently undergoing treatment. The most frequently occurring themes included the need for accurate cancer information, the need for information on treatment options, the role of language barriers in accessing cancer care, the role of food in cancer and the need for nutritional information, the role of Chinese medicine in cancer treatment, the burden of disease on the family, and the need for social, emotional, and spiritual support. Themes were similar between male and female participants, except that women more frequently described the need for social and emotional support.
The need for accurate cancer information
Across all groups, participants described searching and a desire for accurate information about cancer and its risks. Several participants described going online for information. Others described reading books, newspapers, clinic brochures, and obtaining information through cancer support organizations and by word-of-mouth. Of the eleven participants who spoke in some detail about their information-seeking behavior and/or informational needs, all but three expressed significant dissatisfaction with the amount, reliability, specificity, and/or comprehensibility of the information available to them.
Some felt there was too much available information, and it was impossible to know which information was accurate. Others felt there was no enough information: “I don’t understand anything, and I am confused, even apathetic. The doctor says let’s begin the treatment, and my mind is completely blank and utterly oblivious.” Another participant said: “Besides what the doctors told me, I had nothing to read. I went online to look myself, but it was all in English, which I don’t understand too clearly. So I don’t think that [this information] is really available.” Participants described drinks or certain foods being advertised to prevent or cure cancer and not knowing whether these could have an impact on the disease: “If medical professionals could provide patients with enough knowledge of what really does prevent and cure cancer, it’d be much better than whatever ideas [we hear] passed around by word of mouth.”
The need for information on treatment options
Many participants expressed a need for guidance in making decisions about treatment options and felt unable to challenge their doctors: “When I started to see a doctor and the doctor told me that I have to go through an operation and do chemotherapy, I basically had no other option. I had to choose between going through it and not going through it. I think that everyone basically has experienced this struggle, but at the end of course we submit to the doctor’s authority and carry on with the procedure…for us and medical treatment, we are completely in an ignorant state, we only can follow the doctor.” Participants expressed a desire for second opinions but also were often confused by having multiple doctors and did not know which doctors’ advice to follow.
The role of language barriers in accessing cancer care
The impact of language barriers was discussed by many participants in all groups. Language was felt to be a crucial issue. Participants discussed the role of language barriers in impeding participation in the treatment process and in situations where they were not receiving the care and attention they needed from the medical staff and had to advocate for themselves. While some participants described available and convenient interpreting services, many were not aware of interpreting services and described challenges in communicating with doctors and nurses. Many described bringing family members (especially children) along to act as interpreters. One participant described being asked to find his own interpreter and another described “bearing” pain and discomfort rather than coming to the hospital because of the inconvenience of having to find an interpreter to come with him. One patient related that while undergoing a PET scan, he had no interpreter: “When I was lying in the bed [for the PET scan], I couldn’t understand what the doctor was talking about. He was speaking English and I was speaking Chinese.”
Some described a preference for Chinese doctors and dissatisfaction with their current doctors. One explained, “My family doctor is a foreigner [American] and I think it’s hard to talk to him. If I had a Chinese doctor as my primary care doctor, then that would be best.” Another said, “We don’t understand our doctors. They are foreigners [Americans]. We can’t understand what they say. They don’t talk to us. They just type on their computers.”
The role of food in cancer and the need for nutritional information
Participants in all groups spoke extensively about food in relation to their disease. For example, some participants believed that they were infected with hepatitis B through food, while others thought that certain foods prepared by stir-frying or deep-frying cause cancer. Many wanted more information on what foods they should eat after being diagnosed, after chemotherapy, and to prevent recurrence. One participant said, “How [now that treatment is finished] do I maintain this condition now and not let the cancer recur? I still don’t know about this, and how would I know [find out] anything about it? They say that you should eat a lot of vegetables and don’t eat meat, but we are very ignorant when it comes to this and what this is all about. There’s nowhere to ask, either.” Others described similar questions and opinions. One participant explained: “I feel like eating is something that we can make a difference in. But everyone seems to have a different opinion on what one should eat after chemotherapy. I think this is the most important problem.” Another noted: “This is because really in the beginning the thing that has the most relevance to us is our diet, and so we really don’t know how to go about doing this.”
Despite questions about what to eat during and after cancer treatment, participants generally agreed that consuming more fresh fruits and vegetables, less meat, and fewer high-fat foods was beneficial to their health, particularly as cancer survivors. Several participants of both genders specifically talked about eating more vegetables because of their diagnosis and/or about their importance.
The role of Chinese medicine in cancer treatment
Participants in all groups discussed the role of Chinese medicine in general and during cancer treatment but had differing opinions on the extent of its usefulness. Of the ten total participants who spoke in some depth about Chinese medicine, six reported using both Chinese and Western medicine during their cancer treatment. These participants explained the importance of taking Chinese medicine to “help expel toxins” and to “condition the body a bit” after chemotherapy. Two of these participants said that they would not take Chinese and Western medicine at the same time but would space them out by several hours to avoid potential interactions.
Although four participants expressed hesitation or unwillingness to take Chinese medicine during cancer treatment, none of them rejected Chinese medicine outright. For example, one said that in China, there are more Chinese medicine doctors to choose from and their legitimacy is more easily established than in America. She said, “[Although] we want to go see Chinese medicine doctors to help us expel toxins…what if they don’t get it right [i.e., if they are not licensed or legitimate], then we get poisoned, right? So we don’t dare to do it because we’re scared of getting poisoned.”
One younger liver cancer patient, who described an unwillingness to take Chinese medicine during cancer treatment explained, “…in America…[we’re] more trusting of American doctors [laughs]. They’re pretty dependable—like with blood tests and that kind of thing; [but] there’s a little bit of speculation [involved] in Chinese medicine—they speculate a bit.”
Burden on the family
Several of the female participants described feeling as if they were a burden to their families. Chemotherapy was described as being a particularly difficult time for the family, and the cancer was experienced as “a burden on their minds, their finances, their material goods, and their kindness.” Furthermore, the burden was perceived to fall on “not just one person, [but] the whole family.” Participants also expressed concern for their families and the need for an understanding of how families of cancer patients feel. As one participant said, “How they face it [cancer] and how we face it is important, because cancer is a long-term struggle.” Participants felt that families needed to be included in and would be very willing to attend and support programs or activities. Some participants also described the need to find social support outside the family, both to relieve the strain on the family and to have the chance to interact with other patients with the same conditions. One participant described “annoying” her sisters by calling them frequently and the need to find someone to “chat with” when feeling particularly down, otherwise “It feels like you’re about to die and that’s a terrible feeling.”
The need for social, emotional, and spiritual support
Participants described a need for social, emotional, and spiritual support: “We are pretty drained after chemotherapy, psychologically and emotionally. If we have these friends, perhaps our days will be happier. What we need now is for these friends to all support each other.” Support groups were felt to be important: “Like the foreigners [Americans]—everybody who gets cancer meets up together to talk about their experiences.” Participants described the need to talk with others with cancer: “Because they [those without cancer] cannot sympathize if they haven’t been through it. Sometimes I have to stop myself from talking too much.” Others described the need for help in coping with the fear related to illness: “No one helps me with this fear that I have, who is going to help me?”
Participants described hobbies or activities that they perceived as being “good for [your] mind and body,” such as listening to music, walking outside, dancing, singing, chess, and socializing. Participants also described the importance of a positive attitude: “As for one’s spirit [mental wellbeing], be cheerful. I’ve said to my wife, I’m going to live for 500 years more [laughs].” Another participant described the importance of an integrated approach to cancer care: “Eat vegetables [not meat], combine [that] with exercise, your frame of mind—integrate all this…your emotions are the most important.” Participants also felt their doctors’ attitude was important: “As a doctor you need to give patients hope…if you don’t give him [us] hope, we will be totally crushed.”
Several participants mentioned a desire for more information about available social and financial services, and one explained, “Sometimes I think that when we need to find them [social workers] we don’t know where they are, and when they need to find us they don’t know where we are also…We can’t communicate.”
Discussion
This study highlights the needs and concerns of immigrant Chinese cancer patients. Interventions such as support groups and activities (i.e., exercise programs, nutrition seminars, social events) for Chinese patients and their families need to be provided. Participants in this study expressed several barriers to quality cancer care and the need for access to accurate information related to cancer, its treatment, and the role of nutrition and Chinese medicine in cancer.
The quality of the patient–provider interaction and communication should be addressed. In this study, participants described being unwilling to question their doctors, which led to a sense of powerlessness in making treatment decisions. Some of this perceived powerlessness was related to the notion that reliable information about treatment options was not available to them. Participants’ information preferences mirrored those of other cancer patient populations, who generally prefer as much information and decision-making participation as possible [39, 40]. Support groups and programs developed for this population should be responsive to participants’ stated needs for more information on cancer and its treatment. These programs should educate and improve patients’ self-efficacy for participation in treatment choices and decision-making, including teaching patients how to find further Chinese language information and resources and how to effectively communicate their questions, needs, and preferences to providers in an interpreted encounter. Programs should specifically target cultural barriers to greater self-efficacy, focusing on issues such as patients viewing doctors as authority figures, fatalism, and a fear of distracting physicians from treating their cancer [12, 21].
Improving providers’ knowledge and understanding of Chinese cancer patients’ cultural background and unique concerns and priorities, as well as the barriers they face to optimal cancer care, should also be addressed. This can be accomplished through requiring all providers to complete “cultural competency/responsiveness” training. Cultural competence/responsiveness in oncology encompasses the specific knowledge, attitudes, awareness, and clinical skills necessary for effective cross-cultural communication in the clinical setting [19]. Cultural competence/responsiveness can be taught through teaching and training and is critical in oncology where cultural differences in patients’ behaviors, values, preferences, and health beliefs can affect the threshold for seeking care, the recognition and communication of symptoms, the understanding of diagnostic, prognostic, and treatment information, the trust in health care providers, and the adherence to treatment regimens [19, 41–43].
Participants described numerous examples illustrating the magnitude of the impact of language barriers on accessing cancer care and cancer-related information. Many were unaware of the availability of interpreting services in hospitals. System-level approaches should be implemented, to ensure that all non-English speaking patients are made aware of and provided with trained interpreter services and translations of educational information and instructions for procedures.
Study results underscore several additional themes characterizing areas of particular importance to Chinese cancer patients. Support and survivorship interventions for this population should address the role of diet in cancer treatment and recovery, as participants in this study were dismayed by not being able to find accurate information on nutrition and cancer. Additionally, because many study participants described using Chinese herbal medicine concurrently with chemotherapy, both providers and patients should be educated about the risk of herb–medication interactions and how to enable safe concurrent use of Chinese and Western medications [44].
Participants voiced the central role of family in their illness, including worry about family members and the desire for inclusion of family in support initiatives. This is significant given recent research describing Chinese cancer patients’ anxiety about becoming a burden on the family compounding their own distress [45]. Filial piety, the central concept of Confucianism, refers to the idea that younger family members have an obligation to care for elder family members [46]. If adult children do not provide sufficient care for elderly parents, their behavior is considered shameful [46, 47]. In this study, however, we have described how filial piety can impose an additional worry for Chinese cancer patients. In developing interventions for this population, programs should be cognizant of the role of filial piety in the care arrangements for Chinese cancer patients and should be inclusive of family members.
The study’s limitations include a small sample size and potential sampling bias; the discussion could have represented the views of only a few but was strengthened by conducting multiple focus groups. However, the results present valuable information on the needs of this understudied group and parallel and expand upon the results found in the limited number of other studies that address the information and support needs of this population [48, 49]. Liu et al. studied hospitalized Chinese cancer patients and also found that patients had a significant need for informational and emotional support [49]. Huang et al., similar to our study, found that patients wanted to incorporate culture-specific treatments into their care, that family played a central role in patients’ care, and that there was a strong need for interpreters, as well as psychological and spiritual support [48]. Chiu focused on the spiritual resources of Chinese immigrants with breast cancer and found areas of importance that overlap with our study, as patients emphasized family, alternative therapies, and the usefulness of support groups, as well as the importance of including traditional Chinese cultural values, religion, art, prose, and literature [31]. These previous studies, in addition to our study, suggest that an overarching framework of cultural sensitivity, with particular attention to Chinese cultural norms, values, philosophies, traditional treatments, and the central role of the family, would contribute to the effectiveness of programs for this community. Results of this study present greater detail on the informational and psychosocial needs of Chinese immigrant cancer patients, in particular, highlighting the need for accurate information on cancer and treatment options, food and nutrition, and Chinese medicine in cancer treatment. These findings provide further groundwork for future research and the development of linguistically and culturally tailored support and survivorship interventions for this vulnerable population.
Conclusion
Chinese immigrant cancer patients described several areas of informational and psychosocial needs, including the need for accurate information on cancer and treatment options, the role of language barriers and the need for assistance in accessing cancer care, the role of food in cancer and the need for nutritional information, and the need for information related to the role of Chinese medicine in cancer treatment. Interventions should be developed at multiple levels: at the patient level, to educate and empower patients on how to find Chinese language information and resources and how to effectively communicate with providers; at the provider level, through cultural responsiveness training to improve cross-cultural communication; and at the system level, to ensure provision of interpretation services. Programs should incorporate the unique cultural concerns of this population related to food and nutrition, Chinese medicine, and the central role of family.
References
Camarota SA (2007) Immigrants in the United States, 2007: a profile of America’s foreign-born population. Center for Immigration Studies, Washington
Martin P, Midgley E (2010) Immigration in America 2010. Population Reference Bureau. http://www.prb.org/Publications/PopulationBulletins/2010/immigrationupdate1.aspx. Accessed March 2011
United States Census Bureau. American Community Survey (2006) S0201. Selected population profile in the United States, Chinese alone, New York City. United States Census Bureau. http://factfinder.census.gov. Accessed May 2011
McCracken M, Olsen M, Chen MS Jr, Jemal A, Thun M, Cokkinides V, Deapen D, Ward E (2007) Cancer incidence, mortality, and associated risk factors among Asian Americans of Chinese, Filipino, Vietnamese, Korean, and Japanese ethnicities. CA Cancer J Clin 57(4):190–205
Shavers VL, Brown ML (2002) Racial and ethnic disparities in the receipt of cancer treatment. J Natl Cancer Inst 94(5):334–357
Lee-Lin F, Menon U, Pett M, Nail L, Lee S, Mooney K (2008) Measuring breast cancer and mammography screening beliefs among Chinese American immigrants. West J Nurs Res 30(7):852–868. doi:10.1177/0193945908319247
Chuang SC, Chen W, Hashibe M, Li G, Zhang ZF (2006) Survival rates of invasive breast cancer among ethnic Chinese women born in East Asia and the United States. Asian Pac j cancer prev: APJCP 7(2):221–226
Deapen D, Liu L, Perkins C, Bernstein L, Ross RK (2002) Rapidly rising breast cancer incidence rates among Asian-American women. Int J Cancer 99(5):747–750. doi:10.1002/ijc.10415
Institute NC dictionary of cancer terms. http://cancer.gov/dictionary?CdrID=445089. Accessed May 2011
Reis L, Melbert D, Krapcho M (2011) SEER cancer statistics review, 1975–2005. http://seer.cancer.gov/csr/1975_2005. Accessed April 2011
Guidry JJ, Torrence W, Herbelin S (2005) Closing the divide: diverse populations and cancer survivorship. Cancer 104(11 Suppl):2577–2583. doi:10.1002/cncr.21251
Lam WW, Fielding R (2003) The evolving experience of illness for Chinese women with breast cancer: a qualitative study. Psycho-Oncology 12(2):127–140. doi:10.1002/pon.621
Ngo-Metzger Q, Massagli MP, Clarridge BR, Manocchia M, Davis RB, Iezzoni LI, Phillips RS (2003) Linguistic and cultural barriers to care. J gen intern med 18(1):44–52
Mui AC, Kang SY, Kang D, Domanski MD (2007) English language proficiency and health-related quality of life among Chinese and Korean immigrant elders. Health Soc Work 32(2):119–127
Liang W, Wang JH, Chen MY, Shibao F, Lee M, Schwartz MD, Pasick RJ, Mandelblatt JS (2008) Developing and validating a measure of Chinese cultural views of health and cancer. Health educ behav 35(3):361–375. doi:10.1177/1090198106294893
Yu MY, Hong OS, Seetoo AD (2003) Uncovering factors contributing to under-utilization of breast cancer screening by Chinese and Korean women living in the United States. Ethn Dis 13(2):213–219
MLA Language Map Data Center. Data center results: New York, New York. http://www.mla.org/map_data_results&state_id=36&place_id=51000&cty_id=. Accessed July 2011
Lai DW, Chau SB (2007) Predictors of health service barriers for older Chinese immigrants in Canada. Health Soc Work 32(1):57–65
Surbone A (2008) Cultural aspects of communication in cancer care. Support care cancer 16(3):235–240. doi:10.1007/s00520-007-0366-0
Thorne SE, Hislop TG, Armstrong EA, Oglov V (2008) Cancer care communication: the power to harm and the power to heal? Patient educ couns 71(1):34–40. doi:10.1016/j.pec.2007.11.010
Lin CC (2000) Barriers to the analgesic management of cancer pain: a comparison of attitudes of Taiwanese patients and their family caregivers. Pain 88(1):7–14
Wang XS, Cleeland CS, Mendoza TR, Engstrom MC, Liu S, Xu G, Hao X, Wang Y, Ren XS (1999) The effects of pain severity on health-related quality of life: a study of Chinese cancer patients. Cancer 86(9):1848–1855. doi:10.1002/(SICI)1097-0142(19991101)86:9<1848::AID-CNCR29>3.0.CO;2-M
Lin JS, Finlay A, Tu A, Gany FM (2005) Understanding immigrant Chinese Americans’ participation in cancer screening and clinical trials. J commun health 30(6):451–466
Nguyen GT, Bowman MA (2007) Culture, language, and health literacy: communicating about health with Asians and Pacific Islanders. Fam Med 39(3):208–210
Rudd R, Kirsch I, Yamamato K (2004) Literacy and health in America
Weis J (2003) Support groups for cancer patients. Support care cancer 11(12):763–768. doi:10.1007/s00520-003-0536-7
Lindemalm C, Strang P, Lekander M (2005) Support group for cancer patients. Does it improve their physical and psychological wellbeing? A pilot study. Support care cancer 13(8):652–657. doi:10.1007/s00520-005-0785-8
Kass S (1999) Breast-cancer intervention group aids physical healing, research finds. APA Monitor 30 (9)
Fallowfield L (1995) Psychosocial interventions in cancer. BMJ 311(7016):1316–1317
Mok BH (2001) Cancer self-help groups in China: a study of individual change, perceived benefit, and community impact. Small Group Res 32(2):115–132
Chiu L (2001) Spiritual resources of Chinese immigrants with breast cancer in the USA. Int J Nurs Stud 38(2):175–184
Shih FJ (1996) Concepts related to Chinese patients’ perceptions of health, illness and person: issues of conceptual clarity. Accid Emerg Nurs 4(4):208–215
Helgeson VS, Cohen S, Schulz R, Yasko J (1999) Education and peer discussion group interventions and adjustment to breast cancer. Arch Gen Psychiatry 56(4):340–347
Changrani J, Lieberman M, Golant M, Rios P, Damman J, Gany F (2008) Online cancer support groups: experiences with underserved immigrant Latinas. Prim Psychiatry 15(10):55–62
Krueger R, Casey MA (2008) Focus groups: a practical guide for applied research, 4th edn. Sage, Thousand Oaks
Israel BA, Schulz AJ, Parker EA, Becker AB (1998) Review of community-based research: assessing partnership approaches to improve public health. Annu Rev Public Health 19:173–202. doi:10.1146/annurev.publhealth.19.1.173
Kidd PS, Parshall MB (2000) Getting the focus and the group: enhancing analytical rigor in focus group research. Qual Health Res 10(3):293–308
Krueger RA (1994) Focus groups: a practicial guide for applied research. International Journal of Interpreter Education, 2nd edn. Sage, Thousand Oaks
Fallowfield L, Ford S, Lewis S (1995) No news is not good news: information preferences of patients with cancer. Psycho-Oncology 4(3):197–202
Cassileth BR, Zupkis RV, Sutton-Smith K, March V (1980) Information and participation preferences among cancer patients. Ann Intern Med 92(6):832–836
Betancourt JR (2003) Cross-cultural medical education: conceptual approaches and frameworks for evaluation. Acad Med 78:560–569
Betancourt JR, Green AR, Carrillo JE, Ananeh-Firempong OII (2003) Defining cultural competence: a practical framework for addressing racial/ethnical disparities in health and health care. Public Health Rep 188:293–302
Kagawa-Singer M (2003) A strategy to reduce cross-cultural miscommunication and increase the likelihood of improving health outcomes. Acad Med 78:577–587
McCune JS, Hatfield AJ, Blackburn AA, Leith PO, Livingston RB, Ellis GK (2004) Potential of chemotherapy-herb interactions in adult cancer patients. Support care cancer 12(6):454–462. doi:10.1007/s00520-004-0598-1
Lee J, Bell K (2011) The impact of cancer on family relationships among Chinese patients. J Transcult Nurs. doi:10.1177/1043659611405531
Smith C, Hung LC (2012) The influence of Eastern philosophy on elder care by Chinese Americans: attitudes toward long-term care. J Transcult Nurs 23(1):100–105
Nuyen A (2004) The contemporary relevance of the Confucian idea of filial piety. J Chin Philos 31(4):433–450
Huang X, Butow P, Meiser B, Goldstein D (1999) Attitudes and information needs of Chinese migrant cancer patients and their relatives. Aust N Z J Med 29(2):207–213
Liu JE, Mok E, Wong T (2005) Perceptions of supportive communication in Chinese patients with cancer: experiences and expectations. J Adv Nurs 52(3):262–270. doi:10.1111/j.1365-2648.2005.03583.x
Conflict of interest
This study had no specific funding. None of the authors have any conflicts of interest. The corresponding author has a full control of all primary data and agrees to allow the journal to review the data if requested.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Leng, J., Lee, T., Sarpel, U. et al. Identifying the informational and psychosocial needs of Chinese immigrant cancer patients: a focus group study. Support Care Cancer 20, 3221–3229 (2012). https://doi.org/10.1007/s00520-012-1464-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-012-1464-1