Abstract
Liver fibrosis is a major health problem that can lead to the development of liver cirrhosis and hepatocellular carcinoma. On the other hand, several antioxidants have been shown to possess protective effect against liver fibrosis. Therefore, in the present work, the effectiveness of curcumin, α-lipoic acid, and N-acetylcysteine in protecting against carbon tetrachloride (CCl4)-induced liver fibrosis as well as the mechanism(s) implicated in this protective effect was studied. The antioxidants used in this study resulted in hepatoprotective effect as evident by substantial decreases in collagen deposition in histopathological examinations in addition to significant decrease in serum levels of alanine aminotransferase, aspartate aminotransferase, gamma glutamyl transpeptidase, bilirubin, and transforming growth factor-alpha (TGF-α) as well as hepatic malondialdehyde concentration, with a concurrent increase in serum matrix metalloproteinase-13 (MMP-13) and hepatic reduced glutathione (GSH) levels as compared to CCl4 fibrotic group. In conclusion, curcumin, α-lipoic acid, and N-acetylcysteine protect rats against CCl4-induced liver fibrosis most possibly through their antioxidant activities and their capacities to induce MMP-13 and to inhibit TGF-α levels.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Liver fibrosis is a consequence of most chronic liver diseases such as hepatitis viral infection and autoimmune hepatitis. It is characterized by impaired liver function and increased production of extracellular matrix proteins, mainly collagens [1]. Carbon tetrachloride (CCl4), a well-known hepatotoxin, is widely used in laboratory animals to induce toxic liver injuries including fibrosis. CCl4 requires biotransformation to produce free radicals that eventually lead to membrane lipid peroxidation, and it has been established that free radicals and lipid peroxidation play a critical role in the pathogenesis of various hepatic disorders including hepatic fibrosis. Therefore, many antioxidants have been shown as potential hepatic antifibrotic agents [14, 21].
It has been established that curcumin, α-lipoic acid, and N-acetylcysteine exert multiple pharmacological actions that involve antioxidant activities and thus suppress fibrogenesis in rats with CCl4-induced liver injury [7, 16, 22]. However, their mechanism(s) of action are yet to be fully elucidated. Matrix metalloproteinases (MMPs) play an important role in tissue remodeling and repair in both physiological and pathological conditions including liver fibrosis [19]. MMP-13, the main interstitial collagenase in rodents, plays a critical role in mediating the regression of hepatic fibrosis [4]. On the other hand, Lee et al. [13] reported that transforming growth factor-alpha (TGF-α) induces activation of hepatic stellate cells which play a key role in the pathogenesis of hepatic fibrosis. Therefore, the present study was undertaken to study the antifibrotic effects of curcumin, α-lipoic acid, and N-acetylcysteine and to elucidate their possible mechanism(s) of action in CCl4-induced liver fibrosis in rats.
Materials and methods
Animals
Male Wistar rats weighing 180–200 g were used after 1 week for proper acclimatization to the animal house conditions (12 h lighting cycle and 25 ± 2°C temperature) and had free access to standard rodent chow and water. All experimental procedures were conducted according to the ethical standards approved by the Institutional Animal Ethics Committee guidelines for animal care and use, El-Minia University, Egypt.
Chemicals
Curcumin, α-lipoic acid, and N-acetylcysteine were purchased from Sigma–Aldrich Corp. (St. Louis, MO, USA). CCl4 was purchased from BDH/PROLABO Chemicals, England. All other chemicals were of analytical grade and were obtained from commercial sources.
Experimental procedures
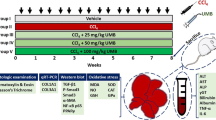
Animals were randomly divided into five groups of ten animals each. The first group served as the control group. The second group was intraperitoneally injected with a mixture of CCl4 (0.1 ml/100 g body weight) and olive oil (1:1, v/v) twice/week for 8 weeks to induce hepatic fibrosis as described by Fu et al. [6] with minor modifications. Groups 3–5 received curcumin (200 mg/kg; Fu et al. [6]), α-lipoic acid (30 mg/kg; Melhem et al. [15]), and N-acetylcysteine (300 mg/kg; Galicia-Moreno et al. [7]), respectively. The tested drugs were suspended in 0.5% aqueous solution of carboxymethyl cellulose and were administered orally daily 1 week before and 8 weeks concurrently with CCl4 injections. All groups received equivalent volumes of the above-used vehicles. Seventy-two hours after the last CCl4 injection, rats were sacrificed, and blood samples were collected and centrifuged at 3,000×g for 10 min to obtain clear sera. The liver was excised from each animal, and a slice was taken for histological examination. Liver samples were snap frozen in liquid nitrogen, stored at −80°C, and subsequently homogenized in cold potassium phosphate buffer (0.05 M, pH 7.4) for various biochemical analyses.
Biochemical analysis
Using commercially available UV/colorimetric kits, serum alanine aminotransferase (ALT), aspartate aminotransferase (AST), gamma glutamyl transpeptidase (GGT), and bilirubin (HUMAN GmbH, Germany) as well as hepatic glutathione (GSH) (Biodiagnostic, Egypt) levels were quantified according to the manufacturers' guidelines. Hepatic lipid peroxidation was determined as thiobarbituric acid-reacting substance and is expressed as equivalents of malondialdehyde (MDA), using 1,1,3,3-tetramethoxypropane as standard [3]. Serum MMP-13 and TGF-α (Uscn Life Science Inc., Wuhan, China) were determined using ELISA kits according to the manufacturer's instructions.
Histological examination
Liver tissue samples were fixed in 10% formalin, embedded in paraffin, sectioned, and stained with hematoxylin and eosin for histological examination and grading using light microscopy. Masson's trichrome stain was used to identify increases in liver collagenous tissue. To quantify the hepatic fibrosis, we used the Knodell index [12] with some modifications. At least five fields containing a central vein of each specimen were analyzed, and the microscopic examination was performed in a blind way.
Statistical analysis
The data are expressed as means ± SEM. Statistical analysis was performed by one-way ANOVA followed by Tukey–Kramar post analysis test for multiple comparisons with P < 0.05 being considered as statistically significant.
Results
Biochemical markers
Serum levels of ALT, AST, GGT, and bilirubin were measured as markers of liver injury. All three drugs, namely curcumin, α-lipoic acid, and N-acetylcysteine treatments significantly decrease CCl4-induced elevation in serum levels of the tested parameters (Table 1).
Histopathological analysis
Histological changes were screened to support the tested biochemical markers of liver injury. The histopathological results showed that the tested drugs ameliorated these changes. In the tested doses, N-acetylcysteine is more effective than curcumin and α-lipoic acid in restoring normal architecture (Fig. 1 and Table 2).
Effect of curcumin, α-lipoic acid, and N-acetylcysteine on carbon tetrachloride-induced histopathological changes in rat liver (×40). a Representative photomicrograph of normal liver tissue stained with hematoxylin and eosin. Notice normal appearance of hepatocytes (arrow); central vein is of normal diameter (asterisk) showing neither dilation nor congestion. b Liver tissue after exposure to carbon tetrachloride for 8 weeks; areas of coagulative necrosis are scattered in the liver lobule near to the central vein (arrow), hepatocytes showing vacuolated cytoplasm (arrowhead), and some apoptotic cells could be easily distinguished in the field (asterisks). Notice dilatation of the central vein and sinusoids with inflammatory cell infiltration. c Liver tissue after treatment with curcumin; general improvement of hepatic architecture could be observed, but some hepatocytes are still showing vacuolated cytoplasm (arrow), and others are apoptotic (arrowhead). Areas of necrosis are still observed (asterisks). d Liver tissue after treatment with α-lipoic acid; the appearance is better than the previous one, less number of vacuolated cells (arrow), disappearance of necrotic tissue, with little inflammatory infiltration (arrowhead). e Liver tissue after treatment with N-acetylcysteine; notice nearly complete recovery of hepatic tissue with scarce vacuolation and inflammatory infiltration
Pretreatment with curcumin, α-lipoic acid, or N-acetylcysteine effectively limits the development and progression of rat liver fibrosis induced by CCl4 as they improved the pattern of collagen distribution in hepatocytes. Once more in this respect, within the tested doses, N-acetylcysteine seems to be superior to curcumin and α-lipoic acid (Fig. 2 and Table 3).
Representative illustrations of rat liver tissues stained with Masson's trichrome for collagen (×40). a Normal liver tissue. Notice normal distribution of collagen (green color) around the sinusoids (arrow) and central vein (arrowhead). b Liver tissue after exposure to carbon tetrachloride for 8 weeks. Notice massive collagen depositions in the matrix especially around blood sinusoids (arrowhead) and around apoptotic hepatocytes (asterisk). c Liver tissue after treatment with curcumin; general improvement of hepatic architecture and decrease in the amount of collagen could be observed. d Liver tissue after treatment with α-lipoic acid; the appearance is better than the previous one with little amount of collagen deposition. e Liver tissue after treatment with N-acetylcysteine. Notice nearly complete recovery of hepatic tissue with pattern of collagen distribution back to normal
Hepatic MDA and GSH
Oxidative stress plays an important role in the development of hepatic fibrosis. So, MDA, the main final product of lipid peroxidation, was determined in rat liver to determine the membrane lipid oxidative damage. In addition, GSH, the most abundant thiol antioxidant in cells, was measured in rat liver. As shown in Fig. 3, treatment with all tested drugs significantly decreases hepatic MDA (Fig. 3a) with concurrent increases in hepatic GSH (Fig. 3b) levels as compared to CCl4 fibrotic group.
Effect of curcumin (Curc), α-lipoic acid (LA), and N-acetylcysteine (NAC) on hepatic malondialdehyde (a) and reduced glutathione (b) levels after 8 weeks of carbon tetrachloride (CCl 4 ) administration in rats. Data are the mean ± SEM of ten rats. *,°Significantly different from control and CCl4 groups, respectively, at P < 0.05
Serum MMP-13 and TGF-α
Figure 4 shows the effects of curcumin, α-lipoic acid, and N-acetylcysteine on serum levels of MMP-13 and TGF-α. Pretreatment with the tested drugs significantly increases MMP-13 (Fig. 4a) with concomitant decreases in TGF-α (Fig. 4b) levels compared with CCl4 fibrotic group.
Effect of curcumin (Curc), α-lipoic acid (LA), and N-acetylcysteine (NAC) on serum matrix metalloproteinase-13 (a) and transforming growth factor-α (b) levels after 8 weeks of carbon tetrachloride (CCl 4 ) administration in rats. Data are the mean ± SEM of ten rats. *,°,ªSignificantly different from control, CCl4, and NAC groups, respectively, at P < 0.05
Discussion
Hepatic fibrosis can lead to the development of hepatic cirrhosis with risk of liver failure and hepatocellular carcinoma [1]. In liver fibrosis, normal hepatic tissue is replaced with collagen-rich extracellular matrix. Within the tested doses, a comparison between the antioxidants used in this study indicates that they have different capacities to prevent collagen accumulation and to improve the histological architecture of the liver, N-acetylcysteine being the most effective. This is in agreement with the findings of Galicia-Moreno et al. [7] and Pereira-Filho et al. [17] who found that administration of N-acetylcysteine preserved the normal levels of collagen in CCl4-intoxicated rats. On the other hand, the development of CCl4-induced liver fibrosis is usually associated with oxidative stress and lipid peroxidation [14]. Bedossa et al. [2] reported that hepatocyte lipid peroxidation plays a major role in the regulation of collagen α1(I) gene expression and that it may be a link between hepatocyte injury and hepatic fibrosis. As shown in the present study, N-acetylcysteine, an antioxidant and GSH precursor, decreased hepatic lipid peroxidation and GSH depletion. GSH plays an important role in antioxidant defense directly through scavenging reactive oxygen species and indirectly through functioning as a cofactor of antioxidant enzymes [5].
Remodeling of fibrillar collagen in rodents has been widely ascribed to the action of MMP-13. The antioxidants used in the current study resulted in increase in serum MMP-13 levels. This result is supported by the findings of Pinlaor et al. [18] who found that curcumin reduces periductal fibrosis in liver fluke-infected hamsters after long-term treatment by a pathway including induction of tissue resorption via MMP-13 overexpression. Moreover, Fallowfield et al. [4] reported that resolution of CCl4-induced hepatic fibrosis was retarded in MMP-13-deficient mice. Furthermore, telmisartan, an angiotensin II type 1 receptor antagonist, prevented liver fibrogenesis and pre-neoplastic lesions by a mechanism involving an increase in MMP-13 expression [10]. In addition, Velasco-Loyden et al. [20] revealed that the aspartate salt of adenosine IFC305 suppresses the activation of hepatic stellate cells, the main extracellular matrix-producing cells in the fibrotic liver, by inhibiting the production of collagen α1(I) mRNA, and increasing the expression of MMP-13 mRNA, which may result in an important decrease of collagen deposition. Besides, collagen-I degradation is critical to hepatic stellate cell apoptosis and hepatocyte regeneration during recovery from liver fibrosis [8].
Various growth factors have been shown to play important roles in the development of liver fibrosis. The ability of the antioxidants used in this study to decrease serum TGF-α concentrations is in agreement with the findings of Lee et al. [13] who reported that hepatic stellate cell activation, a critical step in hepatic fibrogenesis, by TGF-α was blocked by antioxidants, such as d-α-tocopherol. In addition, Kato et al. [11] suggested that ethanol-induced TGF-α may contribute to the development of hepatic fibrosis in alcoholic liver diseases. Moreover, Ito et al. [9] reported that the antibiotic nitrofurazone induces hepatocyte proliferation with a pathway involving increase in TGF-α, and this increase was blocked by concomitant administration of N-acetylcysteine.
In conclusion, the antifibrotic effects of the drugs under investigation appear to stem from (1) their antioxidant activities as indicated by protection against increased lipid peroxidation and increased GSH contents and (2) their abilities to induce MMP-13 and to inhibit TGF-α levels. The rest of the studied biochemical and histopathological parameters indicate a status of structural and functional integrity of liver cells and provide further support to the suggestive mechanism of action.
References
Bataller R, Brenner DA (2005) Liver fibrosis. J Clin Invest 115:209–218
Bedossa P, Houglum K, Trautwein C, Holstege A, Chojkier M (1994) Stimulation of collagen alpha 1(I) gene expression is associated with lipid peroxidation in hepatocellular injury: a link to tissue fibrosis? Hepatology 19:1262–1271
Buege JA, Aust SD (1978) Microsomal lipid peroxidation. Methods Enzymol 52:302–310
Fallowfield JA, Mizuno M, Kendall TJ, Constandinou CM, Benyon RC, Duffield JS, Iredale JP (2007) Scar-associated macrophages are a major source of hepatic matrix metalloproteinase-13 and facilitate the resolution of murine hepatic fibrosis. J Immunol 178:5288–5295
Franco R, Schoneveld OJ, Pappa A, Panayiotidis MI (2007) The central role of glutathione in the pathophysiology of human diseases. Arch Physiol Biochem 113:234–258
Fu Y, Zheng S, Lin J, Ryerse J, Chen A (2008) Curcumin protects the rat liver from CCl4-caused injury and fibrogenesis by attenuating oxidative stress and suppressing inflammation. Mol Pharmacol 73:399–409
Galicia-Moreno M, Rodríguez-Rivera A, Reyes-Gordillo K, Segovia J, Shibayama M, Tsutsumi V, Vergara P, Moreno MG, Muriel P (2009) N-Acetylcysteine prevents carbon tetrachloride-induced liver cirrhosis: role of liver transforming growth factor-beta and oxidative stress. Eur J Gastroenterol Hepatol 21:908–914
Issa R, Zhou X, Trim N, Millward-Sadler H, Krane S, Benyon C, Iredale J (2003) Mutation in collagen-1 that confers resistance to the action of collagenase results in failure of recovery from CCl4-induced liver fibrosis, persistence of activated hepatic stellate cells, and diminished hepatocyte regeneration. FASEB J 17:47–49
Ito K, Kajikawa S, Nii A, Doi K (2005) Nitrofurazone-induced gene expressions in rat hepatocytes and their modification by N-acetylcysteine. Exp Toxicol Pathol 56:333–339
Jin H, Yamamoto N, Uchida K, Terai S, Sakaida I (2007) Telmisartan prevents hepatic fibrosis and enzyme-altered lesions in liver cirrhosis rat induced by a choline-deficient L-amino acid-defined diet. Biochem Biophys Res Commun 364:801–807
Kato J, Sato Y, Inui N, Nakano Y, Takimoto R, Takada K, Kobune M, Kuroiwa G, Miyake S, Kohgo Y, Niitsu Y (2003) Ethanol induces transforming growth factor-alpha expression in hepatocytes, leading to stimulation of collagen synthesis by hepatic stellate cells. Alcohol Clin Exp Res 27:58S–63S
Knodell RG, Ishak KG, Black WC, Chen TS, Craig R, Kaplowitz N, Kiernan TW, Wollman J (1981) Formulation and application of a numerical scoring system for assessing histological activity in asymptomatic chronic active hepatitis. Hepatology 1:431–435
Lee KS, Buck M, Houglum K, Chojkier M (1995) Activation of hepatic stellate cells by TGF alpha and collagen type I is mediated by oxidative stress through c-myb expression. J Clin Invest 96:2461–2468
Manibusan MK, Odin M, Eastmond DA (2007) Postulated carbon tetrachloride mode of action: a review. J Environ Sci Health C Environ Carcinog Ecotoxicol Rev 25:185–209
Melhem MF, Craven PA, Liachenko J, DeRubertis FR (2002) Alpha-lipoic acid attenuates hyperglycemia and prevents glomerular mesangial matrix expansion in diabetes. J Am Soc Nephrol 13:108–116
Min AK, Kim MK, Seo HY, Kim HS, Jang BK, Hwang JS, Choi HS, Lee KU, Park KG, Lee IK (2010) Alpha-lipoic acid inhibits hepatic PAI-1 expression and fibrosis by inhibiting the TGF-beta signaling pathway. Biochem Biophys Res Commun 393:536–541
Pereira-Filho G, Ferreira C, Schwengber A, Marroni C, Zettler C, Marroni N (2008) Role of N-acetylcysteine on fibrosis and oxidative stress in cirrhotic rats. Arq Gastroenterol 45:156–162
Pinlaor S, Prakobwong S, Hiraku Y, Pinlaor P, Laothong U, Yongvanit P (2010) Reduction of periductal fibrosis in liver fluke-infected hamsters after long-term curcumin treatment. Eur J Pharmacol 638:134–141
Rojkind M (1999) Role of metalloproteinases in liver fibrosis. Alcohol Clin Exp Res 23:934–939
Velasco-Loyden G, Pérez-Carreón JI, Agüero JF, Romero PC, Vidrio-Gómez S, Martínez-Pérez L, Yáñez-Maldonado L, Hernández-Muñoz R, Macías-Silva M, de Sánchez VC (2010) Prevention of in vitro hepatic stellate cells activation by the adenosine derivative compound IFC305. Biochem Pharmacol 80:1690–1699
Weber LW, Boll M, Stampfl A (2003) Hepatotoxicity and mechanism of action of haloalkanes: carbon tetrachloride as a toxicological model. Crit Rev Toxicol 33:105–136
Wu SJ, Tam KW, Tsai YH, Chang CC, Chao JC (2010) Curcumin and saikosaponin a inhibit chemical-induced liver inflammation and fibrosis in rats. Am J Chin Med 38:99–111
Conflict of interest
The authors declare that there are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Morsy, M.A., Abdalla, A.M., Mahmoud, A.M. et al. Protective effects of curcumin, α-lipoic acid, and N-acetylcysteine against carbon tetrachloride-induced liver fibrosis in rats. J Physiol Biochem 68, 29–35 (2012). https://doi.org/10.1007/s13105-011-0116-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13105-011-0116-0