Abstract
Percutaneous coronary intervention in patients with diabetes mellitus (DM) is associated with worse clinical outcomes; however, the long-term efficacy of sirolimus-eluting stents (SES) in diabetic patients remains uncertain. We evaluated 5-year clinical outcomes after SES implantation in 197 consecutive patients (85 in the DM group and 112 in the non-DM group), and 246 lesions (106 and 140, respectively). The primary end point was major adverse cardiac events (MACE) defined as cardiac death, nonfatal myocardial infarction, target lesion revascularization (TLR), stent thrombosis or admission for congestive heart failure. Diabetic patient characteristics included 32 % who used insulin. The risk of congestive heart failure was significantly higher [20.0 vs. 5.4 %, odds ratio (OR) 4.417, 95 % confidence interval (CI) 1.659 to 11.759, p = 0.003] in the DM group compared with the non-DM group; however, MACE did not occur significantly more often (27.1 vs. 16.1 %, p = 0.060). Multivariate logistic regression analysis showed that diabetes was associated with congestive heart failure (OR 4.715, 95 % CI 1.743 to 12.759, p = 0.002) and multivessel disease was associated with major adverse cardiac events (OR 2.709, 95 % CI 1.053 to 6.965, p = 0.039). The cumulative rates (%) of TLR were as follows: after 1 year; 5.9 versus 5.4, 2 years; 7.1 versus 5.4, 3 years; 9.4 versus 7.1, 4 years; 9.4 versus 8.9, 5 years; 9.4 versus 8.9 (p = 0.652) in the DM group and the non-DM group, respectively. Diabetic patients had worse long-term prognosis in terms of congestive heart failure than non-diabetic patients undergoing PCI, even with SES. TLR was performed steadily for up to 5 years of follow-up following the late catch-up phenomenon both in diabetic and non-diabetic patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Percutaneous coronary intervention (PCI) in patients with diabetes mellitus (DM) is associated with an increased risk of adverse clinical outcomes compared with those without DM [1–4]. A large cohort study demonstrated that patients with DM had a greater risk of major adverse cardiac events (MACE) even after sirolimus-eluting stent (SES) implantation compared to those without DM [5]. However, SES use in patients with DM reduced the extent of late luminal loss, suggesting a reduced risk of restenosis [6, 7], while SES reduced MACE among diabetic patients to a similar degree to that in non-diabetic patients [8]. Furthermore, the follow-up periods of the above reports were less than 3 years. Thus, longer-term follow-up data regarding efficacy and safety of SES in patients with DM are needed [9].
Therefore, we evaluated 5-year clinical outcomes after SES implantation in a series of consecutive patients with and without DM.
Methods
Patient population and intervention
We studied 549 consecutive patients who underwent PCI from August 2004 to April 2006. The study excluded patients with acute myocardial infarction (n = 147) diagnosed on the basis of chest pain of more than 30 min duration, ST segment elevation of more than 2 mm in two contiguous electrocardiographic (ECG) leads and more than a threefold increase in serum creatine kinase activity, and with unstable angina (n = 94) because no patients were treated with SES. Of the remaining patients (n = 308), we excluded patients treated with only plain old balloon angioplasty (n = 63) and implanted only a bare metal stent (n = 48). Finally, our study included 197 consecutive patients (85 with DM and 112 without DM) with 246 lesions who had received SES. No patients were treated with other types of drug-eluting stents. Patients were assigned to treatment with SES after discussion with the first operator and another 1 or 2 interventional cardiologists. Patients who received at least one SES were included in the analysis, regardless of whether they had received a bare metal stent at any time. SES had to be implanted in all lesions in patients who required stenting in multiple lesions simultaneously; the use of more than one stent per lesion was also allowed. Eligible patients had a history of stable or silent ischemia and presented with at least one lesion with a diameter stenosis of more than 75 %, or more than 50 % in the presence of ischemic signs with exercise ECG or scintigraphy (Tl) between a 2.25 and 4.50 mm reference vessel diameter, which is suitable for stent implantation. PCI was performed according to the current standard procedural guidelines. A successful procedure was defined as less than 25 % residual stenosis following the procedure. The study protocol was approved by the ethics committee at our institution. All patients gave written informed consent.
Adjunct drug therapy
Before or at the time of the procedure, patients received at least 100 mg of aspirin and 100 mg of ticlopidine twice a day. After the procedure, all patients were advised to continue taking aspirin lifelong and ticlopidine was prescribed for at least 12 months.
Quantitative coronary angiography and follow-up protocol
We assessed the initial and 8-month follow-up clinical and angiographic outcomes retrospectively. Baseline, postprocedural, and follow-up coronary angiograms were digitally recorded and all measurements were performed after the intracoronary administration of nitroglycerin. A contrast-filled nontapered catheter tip of 4F or 5F was used for calibration. Quantitative coronary angiography was performed from 2 orthogonal projections that well delineated the coronary artery of interest, without overlapping of side branches and with little foreshortening, using the Philips quantitative coronary analysis system (Philips Medical, The Netherlands). It was assessed by an interventional cardiologist or experienced personnel unaware of the patients with or without DM. We evaluated angiographic binary restenosis defined as in-stent restenosis of at least 50 % on follow-up angiography. Quantitative analysis was used to evaluate the stented area and the area that included the stented segment, as well as the 5 mm margins proximal and distal to the stent (defined as in-stent). All patients were asked to return for coronary angiography at 8 months after the procedure, or earlier if angina symptoms occurred.
Clinical outcomes over 5 years
The primary outcome measure for the present analysis was MACE (a composite of cardiac death, nonfatal myocardial infarction, target lesion revascularization (TLR), stent thrombosis or admission for congestive heart failure) assessed during a 5-year follow-up interval after SES implantation. TLR was considered to be driven by ischemia if the stenosis of the target lesion was more than 50 % on the basis of quantitative coronary angiography in the presence of ischemic signs or symptoms, or if there was a stenosis of more than 75 % even in the absence of ischemic signs or symptoms. Congestive heart failure was defined clinically as the presence of a third heart sound, a Killip class greater than 2, a Forrester subset of 2 or 4, dyspnea, or evidence of pulmonary congestion on chest radiographs [10]. The secondary outcome measure included the individual components of the primary outcome events, all cause death, target vessel revascularization and all PCI, including for other branches. Follow-up data were obtained from hospital charts or by interviewing the patients or referring physicians after 5 years.
Definitions
DM was diagnosed in all patients receiving active treatment with an oral hypoglycemic agent or insulin; for patients with a diagnosis of DM who were receiving dietary therapy alone, enrolment in the present study required documentation of an abnormal blood glucose level (≥126 mg/dl) after an overnight fast, an abnormal glycosylated hemoglobin (HbA1c) test (≥6.5 %) or an abnormal glucose-tolerance test (2 h ≥200 mg/dl) [11]. Data on other cardiovascular risk factors such as hypertension, dyslipidemia, smoking, and family history were reported by the patients themselves or taken from laboratory analysis.
Statistical analysis
Data are reported as the mean ± standard deviation. Baseline, lesion and angiographic characteristics were compared using Pearson’s χ2 test, Student’s t test or a non-parametric test (Mann–Whitney). The odds ratio (OR) and its 95 % confidence interval (95 % CI) were computed for outcome measures using univariate or multivariate logistic regression analysis. A p value of <0.05 was considered statistically significant. All statistical analyses were performed using a personal computer with the SPSS for Windows statistical package (SPSS Inc., Chicago, IL, USA).
Results
Baseline clinical data
A total of 197 patients and 246 lesions were treated with SES (Table 1). 85 patients, of whom 27 (32.0 %) required insulin (Table 2), and 106 lesions were diabetic. Although many baseline clinical and lesion variables were well balanced between the 2 groups, patients with DM had more often undergone previous coronary revascularization procedures (72.9 vs. 55.4 %, p = 0.011) (Table 1). Although we evaluated the results in patients with and without previous percutaneous coronary intervention separately, there were no significant differences with the results in the present study. There were no differences between the two groups before SES placement in terms of medications, laboratory findings on admission including renal function and left ventricular ejection fraction (54.2 ± 17.3 % vs. 51.4 ± 17.8 %) estimated by echocardiography and rate of complete revascularization (67.1 vs. 71.4 %) (Table 1).
Baseline lesions, angiographic and procedural data
Baseline lesion characteristics revealed a trend towards a smaller reference diameter in the DM group than that in the non DM group (2.13 ± 0.53 vs. 2.27 ± 0.52, p = 0.060) (Table 3). There was no significant difference in the ratio of de novo lesions (85.8 vs. 90.7 %). None of the results in the present study changed after exclusion of restenotic lesions. There were no significant differences between the two groups in patients who received bare metal stents in another branch (34.9 vs. 24.3 %) and in the same vessel (12.3 vs. 10 %) (Table 3). There were no significant differences between the two groups in the procedural characteristics such as final balloon size or maximal balloon pressure (Table 4). No cases were treated with a rotablator.
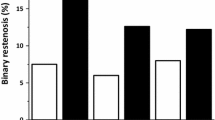
Eight-month follow-up data
Eight-month follow-up angiographic quantitative analysis, including late loss or binary restenosis, showed no significant differences between the 2 groups (Table 5). Furthermore, there were no significant differences between the two groups in the angiographic characteristics of restenotic lesions (Table 6).
Clinical outcomes over 5 years
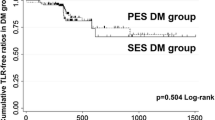
The cumulative incidence of the clinical outcomes over 5 years is listed in Fig. 1. The incidence of admission for congestive heart failure was significantly greater in the DM group than in the non DM group (20.0 vs. 5.4 %, OR 4.417, 95 % CI 1.659 to 11.759, p = 0.003). Kaplan–Meier analysis showed that the difference began to be recognized after 1 year (p = 0.0018) (Fig. 2). However, MACE did not occur significantly more often (27.1 vs. 16.1 %, p = 0.060) in the DM group compared with the non-DM group. Multivariate logistic regression analysis showed that DM was an independent predictor of admission for congestive heart failure (OR 4.715, 95 % CI 1.743 to 12.759, p = 0.002), but not for MACE, while multivessel disease was associated with MACE (OR 2.709, 95 % CI 1.053 to 6.965, p = 0.039) (Table 7). There were no significant predictors of late TLR beyond 1 year. The cumulative rates (%) of TLR were: after 1 year; 5.9 versus 5.4, 2 years; 7.1 versus 5.4, 3 years; 9.4 versus 7.1, 4 years; 9.4 versus 8.9, 5 years; 9.4 versus 8.9 (p = 0.652) in the DM group vs the non-DM group, respectively (Fig. 3). There were no significant differences between the two groups.
Clinical outcomes over 5 years. DM diabetes mellitus, CHF admission for congestive heart failure, MI non-fatal myocardial infarction, ST stent thrombosis, TLR target lesion revascularization, Late TLR target lesion revascularization beyond 1 year, TVR target vessel revascularization, PCI percutaneous coronary intervention, MACE major adverse cardiac events. Transverse bars in Forrest plots indicate 95 % confidence intervals. The incidence of admission for congestive heart failure was significantly greater in the DM group than in the non DM group
Discussion
The major findings of the present study were as follows. First, the patients with DM had a significantly greater risk of admission for congestive heart failure during the 5 years after SES implantation compared to those without DM. Second, there was no significant difference in terms of MACE between diabetic and non-diabetic patients. Finally, TLR was performed steadily up to 5 years of follow-up in patients both with and without DM, implying the late catch-up phenomenon occurred. Three randomized controlled trials (ISAR-DIABETES [12], REALITY [13] and SIRTAX [14]) involving a direct head to head comparison of SES with a paclitaxel-eluting stent (PES) in diabetic patients showed the superiority of SES with regard to late loss and in-segment binary restenosis over short term follow-up. However, DES-DIABETES [15] reported that the superiority of SES over PES in MACE over 2 years was attenuated between 2 and 4 years in diabetic patients. In the SIRTAX LATE trial [16], the clinical superiority of SES over PES at 1 year in MACE was also lost during 5-year follow-up, mainly driven by higher TLR in the SES group. The clinical superiority of SES over PES may be attenuated during long-term follow-up.
Identification of early and late TLR may provide an insight into the mechanism of the late catch-up phenomenon. This has been reported as follows: some smooth muscle cells are not entirely exposed [17], long-term inflammation [18], endothelial dysfunction [19], and progressive atherosclerosis at the margins [20]. The J-Cypher registry [21] reported that DM was an independent risk factor not for late TLR, but for early TLR, and that TLR was observed more frequently in off-label lesions. The incidence of TLR at 3-years in that study was similar to the present study. Late TLR may occur without a strong relation to diabetes.
We acknowledge some limitations in our study. First, the present study was a real world, but single center, non-randomized and retrospective study. Second, renal function, such as estimated by the glomerular filtration rate, was not estimated in patients with congestive heart failure. Third, the number of cases was low in both groups, so lower estimates could be influenced by chance, reducing the potential to increase the power and improve the precision of treatment efficacy and safety. Further studies on a larger number of patients are warranted.
Conclusions
We evaluated 5-year clinical outcomes after SES implantation in 197 consecutive patients with and without DM. The risk of congestive heart failure was significantly higher in the DM group compared with the non-DM group; however, major adverse cardiac events did not occur significantly more often. Target lesion revascularization was performed steadily up to 5 years of follow-up with the late catch-up phenomenon both in diabetic and non-diabetic patients.
References
Elezi S, Kastrati A, Pache J, Wehinger A, Hadamitzky M, Dirschinger J, et al. Diabetes mellitus and the clinical and angiographic outcome after coronary stent placement. J Am Coll Cardiol. 1998;32:1866–73.
Van Belle E, Perie M, Braune D, Chmait A, Meurice T, Abolmaali K, et al. Effects of coronary stenting on vessel patency and long-term clinical outcome after percutaneous coronary revascularization in diabetic patients. J Am Coll Cardiol. 2002;40:410–7.
Yamagata K, Kataoka Y, Kokubo N, Kasahara Y, Abe M, Nakajima H, et al. A 3-year clinical outcome after percutaneous coronary intervention using sirolimus-eluting stent and off-pump coronary artery bypass grafting for the treatment of diabetic patients with multivessel disease. Circ J. 2010;74:671–8.
Fukumoto A, Otsuji S, Takiuchi S, Ikushima M, Asano K, Terasoma K, et al. Comparison of real-world clinical outcomes between Cypher- and Taxus-eluting stents: GARA–GARA study. Cardiovasc Interv Ther. 2011;26:202–8.
Tada T, Kimura T, Morimoto T, Ono K, Furukawa Y, Nakagawa Y, et al. Comparison of three-year clinical outcomes after sirolimus-eluting stent implantation among insulin-treated diabetic, non-insulin-treated diabetic, and non-diabetic patients from j-cypher registry. Am J Cardiol. 2011;107:1155–62.
Dibra A, Kastrati A, Mehilli J, Pache J, Schuhlen H, von Beckerath N, et al. Paclitaxel-eluting or sirolimus-eluting stents to prevent restenosis in diabetic patients. N Engl J Med. 2005;353:663–70.
Sawai T, Miyahara M, Nakajima H, Nakamori S, Sakai M, Tamada H, et al. The impact of preprocedural hemoglobin A1c on the efficacy of sirolimus-eluting and paclitaxel-eluting stents. Cardiovasc Interv Ther. 2012;27:72–83.
Billinger M, Beutler J, Taghetchian KR, Remondino A, Wenaweser P, Cook S, et al. Two-year clinical outcome after implantation of sirolimus-eluting and paclitaxel-eluting stents in diabetic patients. Eur Heart J. 2008;29:718–25.
Kotani J, Ikari Y, Kyo E, Nakamura M, Yokoi H, Furuno K, Inui H, et al. Five-year outcomes of Cypher™ coronary stents: report from J-PMS Study. Cardiovasc Interv Ther. 2012;27:63–71.
Ito H, Maruyama A, Iwakura K, Takiuchi S, Masuyama T, Hori M, et al. Clinical implications of ‘no reflow’ phenomenon: a predictor of complications and left ventricular remodeling in reperfused anterior wall myocardial infarction. Circulation. 1996;93:223–8.
World Health Organisation Study Group. Diabetes mellitus. WHO Tech Rep Ser 1985;727:1–104.
Dibra A, Kastrati A, Mehilli J, Pache J, Schuhlen H, von Beckerath N, et al. Paclitaxel-eluting or sirolimus-eluting stents to prevent restenosis in diabetic patients. N Engl J Med. 2005;353:663–70.
Morice MC, Colombo A, Meier B, Serruys P, Tamburino C, Guagliumi G, et al. Sirolimus- vs paclitaxel-eluting stents in de novo coronary artery lesions: the REALITY trials: a randomized controlled trial. JAMA. 2006;295:895–904.
Billinger M, Beutler J, Taghetchian KR, Remondino A, Wenaweser P, Cook S, et al. Two-year clinical outcome after implantation of sirolimus-eluting and paclitaxel-eluting stents in diabetic patients. Eur Heart J. 2008;29:718–25.
Lee SW, Park SW, Kim YH, Yun SC, Park DW, Lee CW, et al. A randomized comparison of sirolimus- versus paclitaxel-eluting stent implantation in patients with diabetes mellitus. 4-year clinical outcomes of DES-DIABETES Trial. J Am Coll Cardiol Intv. 2011;4:310–6.
Räber L, Wohlwend L, Wigger M, Togni M, Wandel S, Wenaweser P, et al. Five-year clinical and angiographic outcomes of a randomized comparison of sirolimus-eluting and paclitaxel-eluting stents: results of the sirolimus-eluting versus paclitaxel-eluting stents for coronary revascularization LATE trial. Circulation. 2011;123:2819–28.
Cosgrave J, Corbett SJ, Melzi G, Babic R, Biondi-Zoccai GG, Airoldi F, et al. A late restenosis following sirolimus-eluting stent implantation. Am J Cardiol. 2007;100:41–4.
Virmani R, Guagliumi G, Farb A, Musumeci G, Grieco N, Motta T, et al. Localized hypersensitivity and late coronary thrombosis secondary to a sirolimus-eluting stent: should we be cautious? Circulation. 2004;109:701–5.
Higo T, Ueda Y, Oyabu J, Okada K, Nishio M, Hirata A, et al. Atherosclerotic and thrombogenic neointima formed over sirolimus drug-eluting stent: an angioscopic study. JACC Cardiovasc Imaging. 2009;2:616–24.
Aoki J, Nakazawa G, Tanabe K, Hoye A, Yamamoto H, Nakayama T, et al. Incidence and clinical impact of coronary stent fracture after sirolimus-eluting stent implantation. Catheter Cardiovasc Interv. 2007;69:380–6.
Nakagawa Y, Kimura T, Morimoto T, Nomura M, Saku K, Haruta S, et al. Incidence and risk factors of late target lesion revascularization after sirolimus-eluting stent implantation (3-year follow-up of the j-cypher registry). Am J Cardiol. 2010;106:329–36.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sato, T., Ono, T., Morimoto, Y. et al. Five-year clinical outcomes after implantation of sirolimus-eluting stents in patients with and without diabetes mellitus. Cardiovasc Interv and Ther 27, 189–195 (2012). https://doi.org/10.1007/s12928-012-0115-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12928-012-0115-2