Abstract
Major depressive disorder (MDD) is the leading cause of disability in the developed world, yet broadly effective treatments remain elusive. The primary aim of this pilot study was to investigate the efficacy of mindfulness-based cognitive therapy (MBCT) monotherapy, compared to sertraline monotherapy, for patients with acute MDD. This open-label, nonrandomized controlled trial examined a MBCT cohort (N = 23) recruited to match the gender, age, and depression severity of a depressed control group (N = 20) that completed 8 weeks of monotherapy with the antidepressant sertraline. The 17-item clinician-rated Hamilton Depression Severity Rating Scale (HAMD-17) was the primary outcome measure of depression to assess overall change after 8 weeks and rates of response and remission. The 16-item Quick Inventory of Depressive Symptomatology-Self Report (QIDS-SR16) was the secondary outcome measure to further assess depression severity. Both cohorts were demographically similar and showed significant improvement in depression ratings. No difference was found in the degree of change in HAMD-17 scores (t(34) = 1.42, p = 0.165) between groups. Secondary analysis showed statistically significant differences in mean scores of the QIDS-SR16 (t(32) = 4.39, p < 0.0001), with the MBCT group showing greater mean improvement. This study was limited by the small sample size and non-randomized, non-blinded design. Preliminary findings suggest that an 8-week course of MBCT monotherapy may be effective in treating MDD and is a viable alternative to antidepressant medication. Greater changes in the self-rated QIDS-SR16 for the MBCT cohort raise the possibility that patients derive additional subjective benefit from enhanced self-efficacy skills.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Major depressive disorder (MDD) is the number one cause of disability in developed countries and is projected to become the second cause of disability worldwide by 2020 (WHO 2001; Murray and Lopez 1996), yet broadly effective treatments remain elusive. The World Health Organization (WHO) Primary Care Study found that 60 % of patients treated with antidepressants still met criteria for depression after 1 year of treatment (WHO 2001). Only 30 % of individuals with MDD remit with one full trial of antidepressant medication and remission rates for successive trials are even lower (Rush et al. 2006). Moreover, there are well-documented problems with antidepressant adherence, side effects, drug interactions, cost, and personal preference (Thase et al. 2005). While existing psychotherapy treatments offer similar efficacy to medication for treatment of less severe MDD (Cuijpers et al. 2012), there are often significant barriers to access for patients wishing to pursue psychotherapy as a first-line treatment. These include cost, availability of trained psychotherapists, and time commitment (Cuijpers, et al. 2012). Therefore, development of cost effective, readily available, non-pharmacologic, evidence-based treatments is urgently needed.
Mindfulness-based cognitive therapy (MBCT) is a group-based, 8-week intervention that integrates mindfulness meditation with cognitive behavioral concepts. Its approach is distinct from cognitive behavioral therapy (CBT) in that it primarily focuses on the cultivation of effective methods to relate to depressive thoughts and feelings, rather than challenging or changing specific cognitions (Segal et al. 2002). MBCT was originally designed as an intervention to prevent relapse in individuals who have recovered from depression. It has demonstrated effectiveness when compared to routine clinical management (Godfrin and van Heeringen 2010; Ma and Teasdale 2004; Teasdale et al. 2000), and yields equivalent efficacy to maintenance antidepressants in preventing relapse (Kuyken et al. 2010a; Segal et al. 2010). More recently, several studies have investigated MBCT as an augmentative treatment for acute for depression. For example, Manicavasgar et al. (2011) compared MBCT and CBT in a population with MDD and found similar efficacy in both groups, although their work had the confounding effect of 57 % of their participants being on concurrent antidepressants. Omidi et al. (2013) found similar efficacy of CBT and MBCT in reducing depressive symptoms and superiority to medication alone, although 100 % of participants were on concurrent antidepressants. Hamidian et al. (2013) noted that augmentation with MBCT could improve outcomes in dysthymia compared to imipramine treatment alone. Chiesa et al. (2012) noted that in a sample of participants randomized to MBCT or psychoeducation, MBCT was more efficacious in reducing residual symptoms after initial antidepressant treatment. These studies followed works by Barnhofer et al. (2009) and Kingston et al. (2007) demonstrating that MBCT augmentation was more efficacious than treatment as usual (typically antidepressant management) in reducing the residual symptoms of chronic depression. Open label trials of MBCT augmentation of antidepressants for treatment-resistant depression showed effect sizes of 1.0 (Cohen’s D) in both Kenny and Williams (2007) and Eisendrath et al. (2008) hence making MBCT a realistically viable treatment to investigate as a stand-alone treatment for depression.
It’s believed that MBCT’s putative mechanisms of action include enhanced mindfulness (Kuyken et al. 2010b), improved emotional regulation (Arch and Craske 2006), increased self-compassion and acceptance (Kuyken et al. 2008), reduced rumination (Nolen-Hoeksema and Morrow 1991), and the expanded ability to “decenter” from one’s automatic thoughts and dysphoric feelings (Teasdale, et al. 2000). While defined in various ways, mindfulness primarily involves the intentional attention to one’s inner or outer environment in the present moment. “Decentering,” another key term used in the mindfulness literature, has been defined as the ability to view one’s thoughts and feelings as temporary mental events, as opposed to concrete reflections about oneself or others (Fresco et al. 2007). Through these emotion regulation mechanisms (i.e., mindfulness, self-compassion, rumination, decentering), MBCT also shows promise in reducing symptoms of anxiety, which commonly co-occur with depression (Finucane and Mercer 2006). Recent studies have suggested that increased mindfulness may produce biological changes identified through functional magnetic resonance imaging of the brain. Meditation may enhance executive control areas (e.g., the dorsolateral prefrontal cortex and dorsal anterior cingulate) and regulation of ventral affective processing areas (e.g., the amygdala and ventrolateral prefrontal cortex) (Koolschijn et al. 2009). While MBCT is a promising strategy to treat depression and reduce risk of relapse, further research into its efficacy and mechanisms, especially as compared to standard antidepressant treatment, is needed.
The primary aim of this pilot study was to investigate the efficacy of MBCT as a monotherapy for patients with acute phase MDD versus a matched sample treated with standard antidepressant management (ADM) with sertraline for 8 weeks, and to help estimate an MBCT effect size for use in designing further studies, as well as assess the feasibility of MBCT as a monotherapy for MDD. A further aim was to examine potential psychological mediators of treatment response among participants treated with MBCT.
Method
Participants
Recruitment for the MBCT trial was designed to match a cohort that previously participated in an open-label trial of sertraline monotherapy conducted in the same adult outpatient psychiatry clinic at the University of California, San Francisco (UCSF) Medical Center. A description and the results of that trial have been previously published (Rawdin et al. 2012). Neither the original cohort nor the second (MBCT) group underwent any other form of psychotherapy or pharmacotherapy during the acute treatment phase with either MBCT or ADM. The MBCT cohort was matched to the ADM cohort at baseline on a group level with respect to depression severity, mean age, and proportion of women, using a modified bin matching approach. The ADM cohort had initiated treatment 2 years earlier than the MBCT cohort commenced treatment. The MBCT cohort was completely enrolled and completed treatment within 6 months, making the lag-time between studies 2.0 years.
Twenty participants, aged 18 through 70, diagnosed with MDD, were enrolled in the ADM cohort. Twenty-three participants aged 18 through 60, diagnosed with MDD and matched on group mean baseline characteristics (depression severity, gender, and age) with the ADM group, were enrolled in the MBCT group. Candidates for both groups were recruited by fliers, Craigslist postings, and clinical referrals. Interested individuals were screened in a telephone interview. Those with depressive symptoms who were not currently taking antidepressant medications or receiving psychotherapy were invited for an in-person intake evaluation to determine eligibility. Participants gave written informed consent to participate in the studies, which were approved by the UCSF Committee on Human Research and were paid $300 (for the ADM group) and $210 (for the MBCT group) for completing treatment and the assessments.
Eligibility criteria based on depression symptoms for both studies was identical; participants were required to meet the Structured Clinical Interview for DSM-IV-TR Axis I (SCID-I/P) (First et al. 2002) criteria for MDD and to have a Hamilton Depression Severity Rating Scale (HAMD-17) score of 17 or greater. The SCID-I/P was utilized to assess major depressive episode (MDE) duration as well as number of previous episodes. Cognitive function was evaluated using the Mini-Mental Status Exam (Folstein et al. 1975). All instruments for both studies were administered by trained clinical research assistants or psychologists. Depressed individuals with psychosis or bipolar histories were excluded, although co-morbid anxiety disorders were allowed when the depression was considered to be the primary diagnosis. Individuals were also excluded for any of the following reasons: they (1) met SCID-I/P criteria for alcohol or substance abuse or dependence within 6 months of entering the study, (2) were at risk for self-injurious behaviors or suicide (i.e., endorsed a plan and intent), (3) were receiving individual or group psychotherapy and were not willing to discontinue for the 8-week acute treatment duration of the study, (4) did not have adequate English language comprehension, (5) were taking any psychotropic medications including antidepressants, antipsychotics, or mood stabilizers within 6 weeks prior to study entry (although low dose, short-acting sedative-hypnotics, as needed for sleep, were allowed a maximum of three times per week, but none within 1 week before assessments), or (6) had significant or unstable medical illnesses. Additionally, individuals were excluded from the MBCT study if they (1) had cognitive impairment, as defined by a score of <25 on MMSE, that would impair participation in MBCT. Recruitment and screening yielded 20 participants in the ADM group and 23 in the MBCT group who were enrolled into the respective studies.
Procedures and Measures
Participant screening for eligibility, baseline, and post-treatment interviews were completed in person at UCSF. Enrolled participants completed self-report measures online at a location of their choosing. Baseline assessments were conducted within 2 weeks prior to treatment commencement and post-treatment assessments occurred within 2 weeks of completing the 8-week intervention. The 17-item version of the HAMD-17 (Hamilton 1967) was the primary outcome measure of depression to measure overall change scores after 8 weeks as well as rates of response and remission. The 16-item Quick Inventory of Depressive Symptomatology-Self Report (QIDS-SR16) (Rush et al. 2003) was the secondary outcome measure of self-reported depression severity. Primary and secondary outcome instruments were administered pre-and post-treatment with treatment response for all instruments defined as scores ≥50 % decrease from baseline. Remission on the HAMD-17 and QIDS-SR16 was indicated by scores <8 and ≤5, respectively.
The MBCT cohort completed additional scales in order to measure potential post-treatment mediators of change, (i.e., mindfulness, self-compassion, decentering, and rumination). For this purpose, “mindfulness” was defined as the overall mean response rates on the self-report, 39-item Five Facet Mindfulness Scale (FFMQ) (Baer et al. 2006) which assesses mindfulness through five constructs: observing, describing, acting with awareness, non-judging of inner experience, and non-reactivity to inner experience. The 26-item Self-Compassion Scale (SCS) (Neff 2009), subdivided into six subscales: self-kindness, self-judgment, isolation, over-identification, common humanity, and mindfulness, was used to measure mean levels of self-compassion. Because the combined subscales of isolation and self-judgment have previously been demonstrated to play a mediating role in MBCT’s effect in relapse prevention (Van Dam et al. 2010), the version of the SCS which measures these factors was included. Rates of rumination and decentering were measured with the 20-item Experience Questionnaire (Fresco, et al. 2007) which is comprised of two subscales: rumination and decentering. Levels of rumination were also measured with the 22-item Ruminative Response Scale (Nolen-Hoeksema and Morrow 1991; Nolen-Hoeksema et al. 1993).
Treatment Course—MBCT
The structure and format of the mindfulness course followed the original 8-week MBCT manual created by Segal et al. (2002). The manual was adapted to cater to an acutely depressed patient population that often suffers from increased agitation, decreased attention span, and executive impairments (Avery and Silverman 1984). The guided sitting meditations were reduced from 40 to 25 min, while mindful movement exercises were increased from 15 to 25 min. Most of these adaptations were derived from our work with individuals suffering from treatment-resistant depression (Eisendrath et al. 2011). Participants met once weekly in groups of 8 to 12 participants for eight consecutive weeks. Each session lasted 2 h and 15 min and participants were asked to complete 45 min of meditation practice on each additional day of the week for 6 days. Participants recorded their homework practice, including the total amount of time spent doing exercises each week, in a journal that was reviewed prior to each session. Both groups were led by two licensed clinicians with advanced training in MBCT and who also have personal meditation practices. The course has key therapeutic elements which address mindfulness as follows:
-
1.
The body scan is a brief guided meditation that focuses participants’ attention on the present moment via awareness of bodily sensations.
-
2.
The 3-min breathing space is a brief meditation that focuses on the present moment through the awareness of breath.
-
3.
Mindful movement (stretching and walking) are exercises that allow participants to focus their attention on bodily sensations through movement.
-
4.
The guided sitting meditation encourages participants to cultivate a “decentered” awareness and objectivity.
Treatment Course—ADM
Participants in the ADM group were treated in an open-label manner with sertraline for 8 weeks, and were required to undergo at least a 6-week wash out period for any antidepressants taken prior to study enrollment. They could not be taking any other psychotropic medications. Sertraline dosing was based on clinicians’ judgment regarding and on efficacy and tolerability. Dosing began with 50 mg per day, increasing to a maximum of 200 mg per day, as tolerated and as warranted by clinical response. In two cases, the initial dose was lowered to 25 mg per day because of transient side effects. Medication compliance was monitored by pill counts and by plasma antidepressant levels at weeks 4 and 8 of treatment. The mean plasma concentration of (sertraline + N-desmethylsertraline) at week 4 was 46 ± 23 ng/ml; range 10–97 ng/ml, and at week 8 was 67 ± 37 ng/ml; range 10–146 ng/ml. All individuals had plasma concentrations within the range of published steady state concentrations for sertraline at therapeutic doses (Mauri et al. 2002), indicating good compliance with medication treatment.
Statistical Analysis
We used Pearson chi-square tests and t tests to compare the groups on demographic and depression and anxiety measures at baseline. For duration of MDE, we used a non-parametric test due to observed skew. T tests were used to compare the groups on mean change from baseline to week 8 on the HAMD-17 and the QIDS-SR16. The use of change scores allowed us to control for baseline variation. Next, we compared the two groups of study participants on the proportion who responded and those who met criteria for MDD remission. Finally, to identify measures that may mediate the change in depression over time in the MBCT group, we correlated the change in depression scores with the change in the scales of the four putative mediators: mindfulness, self-compassion, decentering, and rumination. Because the measures for these potential mediators were only available for the MBCT group, we were unable to complete a formal mediation analysis wherein a set of linear models tests whether the relationship of type of treatment received to outcome is accounted for the change in variable which, in turn, affects the outcome (MacKinnon 2008). Nonetheless, the potential mediators’ change score correlations with pre- to post-treatment change in HAMD-17 scores allows for some perspective regarding the factors’ roles.
Results
Five subjects in MBCT attended less than five treatment sessions and were considered “non-adherent/compliant.” Four of these individuals were lost to contact and did not complete the post-assessment, leaving 19 participants who were included in the MBCT group outcome analysis. One participant in the ADM group prematurely dropped out of the study due to clinical worsening, while one opted out due to scheduling constraints, and one was omitted from analysis after developing exclusion criteria (being diagnosed with diabetes) over the course of the study. This left 17 ADM participants for outcome analysis. There were no treatment specific adverse side effects leading to drop out in either group.
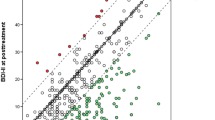
Demographic and clinical characteristics of enrolled participants are shown in Table 1. Comparison between the two groups indicated that they differed significantly only on education; the ADM group was more educated (p < 0.029). Table 2 displays the mean scores for the depression measures at baseline and post-treatment week 8 by group; it also displays the mean change scores along and associated t test p values. MBCT and ADM treatment were both associated with significant improvement in each of the outcome measures. No significant difference was found in the mean difference in primary outcome measure of degree of change in HAMD-17 scores (t(34) = 1.42, p = 0.165) between groups. This lack of statistical significance was maintained when education was added as a covariate (p = 0.10). There were significant differences in mean scores of the QIDS-SR16 t(32) = 4.39, p < 0.001), with the MBCT group showing greater mean improvement. There was no significant correlation between change in depression severity and number of depressive episodes. There was also no relationship identified between amount of homework reported and change in depression scores.
No differences were found (χ 2 (1) = 0.034, p = 0.853) in the proportion responding to treatment, with 47.8 % of the MBCT group and 45.0 % of the ADM group having end-of-treatment HAMD-17 scores over 50 % below their baseline level. Ten participants in the MBCT group and five participants in the ADM group responded to treatment with a 50 % or greater reduction in QIDS-SR16 scores but no statistically significant differences in these response rates were found between groups (χ 2(1) = 2.98, p = 0.084). There were also no significant differences in remission rates between the groups, with 42.1 % of the MBCT group and 41.1 % of the ADM group having HAMD-17 scores <8 at week 8 (χ 2 (1) = 0.003, p = 0.995). Four participants in the MBCT group were classified as having remitted on the QIDS-SR16 (score ≤5) and three individuals met this same criteria in the ADM group with no statistically significant between group difference found (χ 2 (1) = 0.114, p = 0.735).
Although a formal mediational analysis was not possible in our study, we investigated correlation of potential mediators to detect early signals for future randomized studies. The mean changes in the variables investigated as potential mediators in MBCT are shown in Table 3, as are the correlations between the change in the HAMD-17 score and the potential mediators as measured at baseline. Improvement in depression was related to increased non-reactive thinking (r = 0.57, p = 0.017). Because the n for these correlation analyses was 17 and statistical power is limited, we note several correlations >0.40 with p values of <0.10: decreased isolation, and increased decentering, observing, describing, and acting with awareness.
Discussion
This pilot study represents a preliminary investigation of MBCT as a stand-alone treatment for depression, furthering the literature of several studies that have investigated MBCT beyond its original origin as a therapy focused on preventing the relapse of depression (Barnhofer, et al. 2009; Hamidian, et al. 2013; Manicavasgar et al. 2011; Omidi, et al. 2013). The primary aim of the study was to assess the efficacy of depression treatment effects of MBCT and to compare them to those of ADM in untreated, acutely depressed individuals with MDD. Results showed that both open-label treatments were effective in reducing depressive symptom ratings. There were no statistically significant differences in rates of response, remission, or in decreases in depression severity between the two treatments on the HAMD-17. On the self-report QIDS-SR16, MBCT showed significantly greater improvement in depression severity.
Our correlational analyses of potential mediators must be interpreted cautiously due to the number of factors assessed simultaneously, thereby amplifying the possibility of type I errors. However, the facets of increased mindfulness as manifest by positive changes in non-reactive thinking, increased decentering, observing, describing and acting with awareness are consistent with the literature for the type of changes that occur with MBCT (Kuyken et al. 2010b). The ability of individuals to view their thoughts and emotions from a decentered perspective allows them to be less reactive. It also allows them to view thoughts as mental events and not proven facts. This ability is particularly important for depressed individuals prone to negative and catastrophizing ideas. The decreased sense of isolation that occurred may be particularly important and a benefit of group treatment with MBCT.
This study suggests that MBCT monotherapy may be a viable alternative as an acute treatment for depression. MBCT’s proven effectiveness to prevent depression relapse upon remission, contrasts with standard medication management for recurrent MDD, in which relapse prevention has been noted to last for only a relatively limited period after drug discontinuation (Dunlop et al. 2012; Glue et al. 2010). Furthermore, MBCT may be particularly well suited for individuals who are medication-averse, are troubled by side effects, or have difficulties with adherence; or conversely, for those individuals open to learning a useful skill set to manage their depression. Patients appear interested in such alternative approaches that enhance self-efficacy and offer skills to autonomously regulate dysphoric moods (Barnes et al. 2004). Although individuals are required to invest more time and energy in MBCT than in medication management during the first 8 weeks of treatment, studies indicate that MBCT may be cost effective in comparison to maintenance medications over time (Kuyken et al. 2010b; Shawyer et al. 2012).
Although this study is encouraging with respect to the effectiveness of MBCT, the results must be interpreted very cautiously since it is limited by being a non-randomized study with a small sample size that limits generalizability. The low power could have played a role in the inability to disprove the null hypothesis. The study was also limited by a lack of data with respect to independent factors, such as anxiety and disability, which can influence depression outcomes. While it’s not apparent that education was a demographic factor that impacted results, it is important to note that the two participant populations were not perfectly matched on a group level in that the ADM sample reported greater education levels. Moreover, the treatment cohorts were conducted at different times and while we do not believe there was a secular trend affecting prognosis, it is possible that this could have occurred. Finally, since the study represents an open trial, it is possible that the MBCT sample had a self-selection bias toward that treatment but the ADM sample may have had an offsetting bias toward medication management. These limitations and lack of randomization would be addressed in a full RCT. Similarly, the small sample size, imperfectly matched variables, such as the number of prior episodes and illness duration, would be alleviated in a full RCT, which we hope to address in our future work. In summary, MBCT may provide a psychotherapeutic option for the treatment of acute depression if supported by further randomized controlled trials. Because our results are preliminary, they suggest further investigation is indicated. Since MBCT is an established relapse prevention therapy, if it proves efficacious as a first-line treatment, it may offer significant secondary prevention benefits. With the pressing need to find depression treatments that work in the acute phase and prevent future episodes, additional research investigation is warranted.
References
Arch, J. J., & Craske, M. G. (2006). Mechanisms of mindfulness: emotion regulation following a focused breathing induction. Behaviour Research and Therapy, 44(12), 1849–1858. doi:10.1016/j.brat.2005.12.007.
Avery, D., & Silverman, J. (1984). Psychomotor retardation and agitation in depression. Relationship to age, sex, and response to treatment. Journal of Affective Disorders, 7(1), 67–76.
Baer, R. A., Smith, G. T., Hopkins, J., Krietemeyer, J., & Toney, L. (2006). Using self-report assessment methods to explore facets of mindfulness. Assessment, 13(1), 27–45. doi:10.1177/1073191105283504.
Barnes, P. M., et al. (2004). Complementary and alternative medicine use among adults: United States. Advance Data, 343, 1–19.
Barnhofer, T., Crane, C., Hargus, E., Amarasinghe, M., Winder, R., & Williams, J. M. (2009). Mindfulness-based cognitive therapy as a treatment for chronic depression: a preliminary study. Behaviour Research and Therapy, 47(5), 366–373. doi:10.1016/j.brat.2009.01.019.
Chiesa, A., Mandelli, L., & Serretti, A. (2012). Mindfulness-based cognitive therapy versus psycho-education for patients with major depression who did not achieve remission following antidepressant treatment: a preliminary analysis. Journal of Alternative and Complementary Medicine, 18(8), 756–760. doi:10.1089/acm.2011.0407.
Cuijpers, P., Reynolds, C. F., 3rd, Donker, T., Li, J., Andersson, G., & Beekman, A. (2012). Personalized treatment of adult depression: medication, psychotherapy, or both? A systematic review. Depression and Anxiety, 29(10), 855–864. doi:10.1002/da.21985.
Dunlop, B. W., Thase, M. E., Wun, C. C., Fayyad, R., Guico-Pabia, C. J., Musgnung, J., et al. (2012). A meta-analysis of factors impacting detection of antidepressant efficacy in clinical trials: the importance of academic sites. Neuropsychopharmacology, 37(13), 2830–2836. doi:10.1038/npp.2012.153 npp2012153.
Eisendrath, S. J., Delucchi, K., Bitner, R., Fenimore, P., Smit, M., & McLane, M. (2008). Mindfulness-based cognitive therapy for treatment-resistant depression: a pilot study. Psychotherapy and Psychosomatics, 77(5), 319–320. doi:10.1159/000142525.
Eisendrath, S., Chartier, M., & McLane, M. (2011). Adapting mindfulness-based cognitive therapy for treatment-resistant depression: a clinical case study. Cognitive Behavior Practice, 18(3), 362–370. doi:10.1016/j.cbpra.2010.05.004.
Finucane, A., & Mercer, S. W. (2006). An exploratory mixed methods study of the acceptability and effectiveness of mindfulness-based cognitive therapy for patients with active depression and anxiety in primary care. BMC Psychiatry, 6, 14. doi:10.1186/1471-244X-6-14.
First, M. B., Spitzer, Robert L, Gibbon Miriam, and Williams, Janet B.W. (2002). Structured clinical interview for DSM-IV-TR Axis I disorders, research version, Patient Edition. (SCID-I/P). Biometrics Research, New York State Psychiatric Institute, November
Folstein, M. F., Folstein, S. E., & McHugh, P. R. (1975). Mini-mental state. A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research, 12(3), 189–198.
Fresco, D. M., Moore, M. T., van Dulmen, M. H., Segal, Z. V., Ma, S. H., Teasdale, J. D., et al. (2007). Initial psychometric properties of the experiences questionnaire: validation of a self-report measure of decentering. Behaviour Therapy, 38(3), 234–246. doi:10.1016/j.beth.2006.08.003.
Glue, P., Donovan, M. R., Kolluri, S., & Emir, B. (2010). Meta-analysis of relapse prevention antidepressant trials in depressive disorders. The Australian and New Zealand Journal of Psychiatry, 44(8), 697–705. doi:10.3109/00048671003705441.
Godfrin, K. A., & van Heeringen, C. (2010). The effects of mindfulness-based cognitive therapy on recurrence of depressive episodes, mental health and quality of life: a randomized controlled study. Behaviour Research and Therapy, 48(8), 738–746. doi:10.1016/j.brat.2010.04.006.
Hamidian, S., Omidi, A., Mousavinasab, S. M., & Naziri, G. (2013). Comparison of the effect of mindfulness-based cognitive therapy accompanied by pharmacotherapy with pharmacotherapy alone in treating dysthymic patients. Iran Red Crescent Medical Journal, 15(3), 239–244. doi:10.5812/ircmj.8024.
Hamilton, M. (1967). Development of a rating scale for primary depressive illness. British Journal of Social & Clinical Psychology, 6(4), 278–296.
Kenny, M. A., & Williams, J. M. (2007). Treatment-resistant depressed patients show a good response to mindfulness-based cognitive therapy. Behaviour Research and Therapy, 45(3), 617–625. doi:10.1016/j.brat.2006.04.008.
Kingston, J., Chadwick, P., Meron, D., & Skinner, T. C. (2007). A pilot randomized control trial investigating the effect of mindfulness practice on pain tolerance, psychological well-being, and physiological activity. Journal of Psychosomatic Research, 62(3), 297–300. doi:10.1016/j.jpsychores.2006.10.007.
Koolschijn, P. C., van Haren, N. E., Lensvelt-Mulders, G. J., Hulshoff Pol, H. E., & Kahn, R. S. (2009). Brain volume abnormalities in major depressive disorder: a meta-analysis of magnetic resonance imaging studies. Human Brain Mapping, 30(11), 3719–3735. doi:10.1002/hbm.20801.
Kuyken, W., Byford, S., Taylor, R. S., Watkins, E., Holden, E., White, K., et al. (2008). Mindfulness-based cognitive therapy to prevent relapse in recurrent depression. Journal of Consulting and Clinical Psychology, 76(6), 966–978.
Kuyken, W., Byford, S., Byng, R., Dalgleish, T., Lewis, G., Taylor, R., et al. (2010a). Study protocol for a randomized controlled trial comparing mindfulness-based cognitive therapy with maintenance anti-depressant treatment in the prevention of depressive relapse/recurrence: the PREVENT trial. Trials, 11, 99. doi:10.1186/1745-6215-11-99.
Kuyken, W., Watkins, E., Holden, E., White, K., Taylor, R. S., Byford, S., et al. (2010b). How does mindfulness-based cognitive therapy work? Behaviour Research and Therapy, 48(11), 1105–1112. doi:10.1016/j.brat.2010.08.003.
Ma, S. H., & Teasdale, J. D. (2004). Mindfulness-based cognitive therapy for depression: replication and exploration of differential relapse prevention effects. Journal of Consulting and Clinical Psychology, 72(1), 31–40.
MacKinnon, D. P. (2008). Introduction to statistical mediation analysis. Ney York: Taylor & Francis Group.
Manicavasgar, V., Parker, G., & Perich, T. (2011). Mindfulness-based cognitive therapy vs cognitive behaviour therapy as a treatment for non-melancholic depression. Journal of Affective Disorders, 130(1–2), 138–144. doi:10.1016/j.jad.2010.09.027.
Mauri, M. C., Laini, V., Cerveri, G., Scalvini, M. E., Volonteri, L. S., Regispani, F., et al. (2002). Clinical outcome and tolerability of sertraline in major depression: a study with plasma levels. Progress in Neuro-Psychopharmacology & Biological Psychiatry, 26(3), 597–601.
Murray, C. J., & Lopez, A. D. (1996). Evidence-based health policy–lessons from the global burden of disease study. Science, 274(5288), 740–743.
Neff, K. D. (2009). The role of self-compassion in development: a healthier way to relate to oneself. Human Development, 52(4), 211–214.
Nolen-Hoeksema, S., & Morrow, J. (1991). A prospective study of depression and posttraumatic stress symptoms after a natural disaster: the 1989 Loma Prieta Earthquake. Journal of Personal and Social Psychology, 61(1), 115–121.
Nolen-Hoeksema, S., Morrow, J., & Fredrickson, B. L. (1993). Response styles and the duration of episodes of depressed mood. Journal of Abnormal Psychology, 102(1), 20–28.
Omidi, A., Mohammadkhani, P., Mohammadi, A., & Zargar, F. (2013). Comparing mindfulness based cognitive therapy and traditional cognitive behavior therapy with treatments as usual on reduction of major depressive disorder symptoms. Iran Red Crescent Medical Journal, 15(2), 142–146. doi:10.5812/ircmj.8018.
Rawdin, B. S., Mellon, S. H., Dhabhar, F. S., Epel, E. S., Puterman, E., Su, Y., et al. (2012). Dysregulated relationship of inflammation and oxidative stress in major depression. Brain, Behavior, and Immunity. doi:10.1016/j.bbi.2012.11.011.
Rush, A. J., Trivedi, M. H., Ibrahim, H. M., Carmody, T. J., Arnow, B., Klein, D. N., et al. (2003). The 16-Item Quick Inventory of Depressive Symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): a psychometric evaluation in patients with chronic major depression. Biological Psychiatry, 54(5), 573–583.
Rush, A. J., Trivedi, M. H., Wisniewski, S. R., Stewart, J. W., Nierenberg, A. A., Thase, M. E., et al. (2006). Bupropion-SR, sertraline, or venlafaxine-XR after failure of SSRIs for depression. New England Journal of Medicine, 354(12), 1231–1242. doi:10.1056/NEJMoa052963.
Segal, Z., Williams, J. M., & Teasdale, J. (2002). Mindfulness -based cognitive therapy for depression. New York: The Guilford press.
Segal, Z. V., Bieling, P., Young, T., MacQueen, G., Cooke, R., Martin, L., et al. (2010). Antidepressant monotherapy vs sequential pharmacotherapy and mindfulness-based cognitive therapy, or placebo, for relapse prophylaxis in recurrent depression. Archives of General Psychiatry, 67(12), 1256–1264. doi:10.1001/archgenpsychiatry.2010.168.
Shawyer, F., Meadows, G. N., Judd, F., Martin, P. R., Segal, Z., & Piterman, L. (2012). The DARE study of relapse prevention in depression: design for a phase 1/2 translational randomised controlled trial involving mindfulness-based cognitive therapy and supported self monitoring. BMC Psychiatry, 12, 3. doi:10.1186/1471-244X-12-3.
Teasdale, J. D., Segal, Z. V., Williams, J. M., Ridgeway, V. A., Soulsby, J. M., & Lau, M. A. (2000). Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. Journal of Consulting and Clinical Psychology, 68(4), 615–623.
Thase, M. E., Haight, B. R., Richard, N., Rockett, C. B., Mitton, M., Modell, J. G., et al. (2005). Remission rates following antidepressant therapy with bupropion or selective serotonin reuptake inhibitors: a meta-analysis of original data from 7 randomized controlled trials. Journal of Clinical Psychiatry, 66(8), 974–981.
Van Dam, N. T., Sheppard, S. C., Forsyth, J. P., & Earleywine, M. (2010). Self-compassion is a better predictor than mindfulness of symptom severity and quality of life in mixed anxiety and depression. Journal of Anxiety Disorders. doi:10.1016/j.janxdis.2010.08.011.
WHO (2001) Burden of mental and behavioral disorders. Geneva: WHO.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Eisendrath, S.J., Gillung, E., Delucchi, K. et al. A Preliminary Study: Efficacy of Mindfulness-Based Cognitive Therapy versus Sertraline as First-line Treatments for Major Depressive Disorder. Mindfulness 6, 475–482 (2015). https://doi.org/10.1007/s12671-014-0280-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12671-014-0280-8