Abstract
Mindfulness-based cognitive therapy (MBCT) was originally designed to prevent relapse in people who had recovered from depression, and many studies have proven its efficacy in this domain. People with treatment-resistant depression (TRD) may be maintaining their depression via a similar cognitive style to those who have recovered from depression and are vulnerable to relapse. Therefore, investigators have started to use MBCT to treat people with TRD. In this chapter, we outline the theoretical rationale for using MBCT to treat active depression, in particular TRD. We use a case study to illustrate modifications to the standard MBCT protocol that address challenges in treating people with TRD, such as decreased attentional control and debilitating negative thinking styles. Finally, we review the growing evidence base for the application of MBCT to treat TRD, and discuss practical considerations such as patient selection, group size, and format.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Mindfulness-based cognitive therapy
- Treatment-resistant depression
- Rumination
- Emotion regulation
- Self-compassion
- Experiential avoidance
- Meditation
The Case of Sofia
Sofia is a 54-year-old married woman who has been suffering from depressive symptoms to varying degrees since her adolescence. She was adopted at an early age and experienced sexual abuse by her adoptive father from the ages of 8–12. Despite persistent low mood and poor energy, Sofia was able to maintain steady work as a massage therapist until she experienced a worsening of her depressive symptoms 2 years ago. She is now on disability and spends her day watching TV. Her current symptoms include dysphoric mood, poor energy, difficulty concentrating, poor sleep, guilty ruminations, and passive suicidal ideation of “I wish I wouldn’t wake up tomorrow.”
Through the course of her treatment, Sofia has had at least 8 week trials of three mechanistically different antidepressants at therapeutic doses without remission of her symptoms. She discontinued several other antidepressants early due to sexual side effects , increased irritability, and fears of weight gain. She also suffers from chronic back pain of unknown etiology, and suffers from intermittent panic attacks. She has tried psychodynamic psychotherapy and CBT in the past but did not find them helpful. Specifically, she felt “no need to delve into the past” with psychodynamic psychotherapy, and felt like a “bad student” in CBT because she could not change her negative thoughts and often did not do the homework.
The Problem of Treatment-Resistant Depression
Sofia’s struggle with depression is unfortunately quite common. Depression is the number three cause of disability worldwide and the number one cause of disability in high-income countries [1]. Although definitions vary, the commonly held definition of treatment-resistant depression (TRD) is a failure to fully remit from depressive symptoms after two or more antidepressant trials [2, 3]. Thirty-five to fifty percent of all patients with depression may be treatment-resistant [4, 5]. TRD is associated with greater disability, morbidity, mortality, and health care costs than non-resistant depression [6, 7]. As such, it is a major public health concern.
Adding or switching medications is the strategy most commonly used for TRD. As illustrated in the STAR*D trial, this strategy has limited effectiveness, with only half of patients remitting after two full antidepressant trial , and lower remission rates for each subsequent treatment step [5]. After patients fail to remit using first-line medications, medications with higher side effect burden or risk may be used (such as tricyclic antidepressants and monoamine oxidase inhibitors), or more stigmatized and/or invasive treatment options may be utilized such as electroconvulsive therapy and vagal nerve stimulation.
Clearly, alternative approaches to treating TRD are needed. MBCT may be a low-cost, minimally invasive, and well-tolerated option for those with TRD.
Theoretical Rationale of MBCT for Treatment Resistant Depression
Use of MBCT for Prevention of Depressive Relapse
MBCT was originally designed to prevent depressive relapse in people who had recovered from a major depressive episode and were at risk of relapsing [8]. In this section, we review mechanisms by which MBCT may prevent depressive relapse, and then outline the rationale for using MBCT as an active treatment for people with TRD such as Sofia.
Numerous studies have found MBCT to be efficacious in relapse prevention [9–11]. A meta-analysis of six randomized-controlled trials (RCTs) with 593 total participants found that MBCT reduced the risk of relapse for patients with recurrent MDD by 34 % compared to treatment-as-usual (TAU) or placebo control, and the risk reduction increased to 43 % for patients with three or more previous episodes [12]. MBCT appears to be equivalent to maintenance medication for relapse prevention [13–15]. Gains from MBCT treatment were maintained over a 34-month follow-up period in one study [16] and 5-year follow-up period in another [17].
How does MBCT produce these results? The developers of MBCT postulated that people who had suffered from depression may react differently to sad mood states than people who had never been depressed, and then built the intervention based on this assumption. Teasdale [18] hypothesized that sad moods reactivate thinking styles associated with previous sad moods. This puts people who have been depressed in the past at risk of spiraling downward into another depressive episode. Several studies confirmed that when people who have experienced depression in the past feel sad, they are more likely to endorse dysfunctional thinking than those who have never been depressed [19, 20], and that people who display this reactivated dysfunctional thinking in response to sad mood are more likely to relapse into another depressive episode in the future [21, 22].
Mindfulness has been defined as the awareness that arises through paying attention on purpose in the present moment and nonjudgmentally [23]. Studies have confirmed that MBCT does in fact increase mindfulness, and that mindfulness skills may be the mediator of MBCT’s treatment effect [24, 25]. One study using EEG found that MBCT improved participants’ ability to shift their attention toward current moment experience and away from distracting stimuli during mild dysphoric states [26]. Another study with previously depressed participants found that after MBCT, participants showed less negative attentional bias; they showed a reduced facilitation of attention for negative information and a reduced inhibition of attention for positive information [27]. Mindfulness also encourages people to see the negative thoughts they experience as passing events of the mind that do not necessarily reflect reality. People may become less vulnerable to depressive relapse by being able to disengage from or “decenter” from negative thoughts and feelings [28, 29]. Mindfulness could thus lead to using less avoidance coping strategies [30], and could function as an exposure procedure to previously avoided aversive thoughts [31].
Applying MBCT to Treatment Resistant Depression
People with treatment-resistant depression may be maintaining their depression via a similar cognitive style that renders people who have recovered from depression vulnerable to relapse. Thus, several of the mechanisms that are thought to help prevent relapse may also help people who are actively depressed.
MBCT helps to decrease rumination [17, 32]. Nolen-Hoeksema defined ruminative responses to depression as “thoughts and behaviors that focus one’s attention on one’s depressive symptoms and the meaning of those symptoms” [33]. People often believe that ruminating about their symptoms will help them understand the causes of the depression better, and thus enable them to “fix” their mood. However, the depressive rumination often ends up paradoxically increasing sad mood [34]. Martin and Tesser [35] suggested that rumination is the result of discrepancies between an individual’s goals and the actual state of things. MBCT may decrease rumination by encouraging participants to adopt a more accepting mode of being, one that does not need to evaluate experience in order to reduce discrepancies [8, 36]. This increased acceptance could be particularly useful for people with treatment-resistant depression, who might be mired in depressive ruminations as treatment after treatment has failed to alleviate their symptoms.
Mindfulness may also enhance emotion regulation [37, 38]. Chiesa and collaborators [38] suggest that one of the ways that mindfulness training enhances emotion regulation is by modifying how “higher” brain regions such as the prefrontal cortex modulate the input to the “lower” emotion-generative system (such as the amygdala ) by actively reinterpreting emotional stimuli in a way that modifies their emotional impact [39]. This is similar to how cognitive behavioral therapy (CBT) has been postulated to exert its effect [40]. Mindfulness may also enhance emotion regulation by a direct reduction of reactivity in “lower” emotion-generative brain regions such as the amygdala, especially in long-term practitioners of mindfulness [41].
Self-compassion may be another mechanism by which MBCT treats active depression. Neff defines self-compassion as, “extending kindness and understanding to oneself rather than harsh self-criticism and judgment, seeing one’s experiences as part of the larger human experience rather than as separating and isolating, and holding one’s painful thoughts and feelings in balanced awareness rather than over-identifying with them” [42]. Kuyken and colleagues [43] found that increased self-compassion mediated MBCT’s ability to successfully prevent depressive relapse and also mediated the effect of MBCT on post-treatment symptoms of depression.
Going back to our case example of Sofia, she had failed many change-based strategies and her providers felt it would be beneficial for her to try an intervention focused on acceptance. Sofia did not like talking about her trauma history, and liked that the intervention would be present-focused and not necessitate delving into her painful past. Sofia also liked that while group participation was encouraged, if she were feeling particularly depressed or anxious, she could participate silently in the meditation s without needing to speak about her experience. She also had positive associations with the concept of mindfulness. Sofia knew friends who had a meditation practice who were not “sick” and thus found the concept of going to the group less stigmatizing. However she was skeptical that she’d be able to be “calm enough” to meditate. She was also concerned that her chronic pain would interfere with her ability to sit for long periods of time, and very worried that she would not be able to learn to meditate correctly.
Modifications of MBCT for Treatment-Resistant Depression
Despite the many indications that MBCT would be helpful in TRD, there are also unique challenges in treating this population [8, 44]. For one, it could be difficult to engage people with active depression. They may feel hopeless and may have low motivation to participate in group and do homework. They may have decreased ability to concentrate and attend to the teachings and exercises. Their negative thinking styles and self-criticism may make them believe they are “not meditating correctly” rather than being open to learning the new material. And given that they are actively depressed, the content of the present moment that they are being asked to focus on may be extremely painful. Accepting and allowing these negative thoughts and feelings could be a foreign and overwhelming concept. And finally, like Sofia, people with TRD are more likely to have comorbidities such as anxiety and physical pain [45, 46] that may interfere with their work in the group.
Eisendrath and colleagues [47, 48] have made several modifications to the MBCT manual developed by Segal et al. [8] to address these challenges. A summary of the modifications is listed in Table 12.1. Specific modifications are illustrated in detail using our case example of Sophia.
General Modifications
Throughout the 8 weeks of the group, the length of several group sitting meditation s were reduced from 30 min to 10–15 min to address the decreased attentional control and restlessness that is often experienced in depression. In addition, greater emphasis was placed on walking meditations and mindful movement/yoga. If participants suffered from physical limitations such as pain, instructors gave them suggestions for modification, for example sitting in a chair during the body scan instead of lying down. Given that several participants had a history of trauma , participants were given the choice of allowing their eyes to gently close or gazing softly a few feet in front of them if they were not comfortable closing their eyes in guided meditations. Similarly sitting in a chair rather than lying supine for a body scan may be preferred as less vulnerable.
The language instructors used was modified to address the change in focus from relapse prevention to treatment of active depression. For example, phrases like “when you become depressed,” were replaced with “the experience of depression for you right now.” The language was also modified from using commands like “close your eyes” to the present participle “closing your eyes” to help participants who might have difficulty with a more authoritative stance. See Table 12.2.
Going into MBCT, Sophia was of the mindset that if she actually let herself feel the full extent of her depression, she would sink further in it. Given that this is a natural and common way to think about depression, two exercises derived from Acceptance and Commitment Therapy (ACT) were added to the first session of MBCT to illustrate how and why people might want to relate differently to their depression. The ACT exercises helped to illustrate to participants why avoiding negative emotions and feelings may be counterproductive.
The Chinese Finger Cuff Exercise gave participants a physical metaphor for their psychological experience of depression [49]. Sophia and the other participants were given Chinese finger cuffs, asked to put their index fingers in them, and then asked to try to get out of the cuffs. When Sophia tried to pull her fingers out, the cuff tightened. She was then asked to try even harder, which made the cuff even tighter. She was then invited to push her fingers closer together, and she observed that the cuffs loosened up. This experience was then related to her depression. The perfectly natural method of trying to pull away from (or avoid) her depression had not worked in the past, and may have tightened depression’s grip on her. Somewhat counterintuitively, allowing herself to get in close with the depression may give her some “wiggle room” to live her life.
Another modification derived from ACT is the Quicksand Metaphor [49]. The group was asked what happens when people in quicksand struggle to get out. From watching movies, a group member responded that people sink even deeper when they struggle. We discussed how the best strategy when someone is in quicksand is actually to come into full contact with the quicksand by leaning back and floating in it.
In session 2, the standard Thoughts and Feelings exercise was paired with an added ACT exercise entitled Your Mind is Not Always Your Friend [50] to promote decentering from negative thoughts. Participants observed their own negative thoughts in the Thoughts and Feelings exercise, and were then invited to explore how the mind sometimes may not be helpful by (1) creating problems to worry about when there is nothing to worry about, (2) trying to solve problems that cannot be solved, (3) assigning blame, often to oneself, when a problem is detected. Sophia was invited to explore how actually engaging with her mind, and the negative thoughts it produces (as all minds do) may sidetrack her from doing what she values in life.
Another modification in Session 2 was the Black Dog Analogy that invited participants to think about their depression as something that they could react to in a number of different ways. Winston Churchill referred to his depressive states as the “black dog,” [51] and a depressed day as a day in which “the black dog has returned.” Participants were asked what their reaction to a black dog may be. Some people may be scared of a large black dog, but others may be curious about it. The exercise encouraged participants to consider different reactions to their depression, for example, recognizing that it may be a signal that something was not working in their lives that needed tending to. Sophia recognized that her “black dog” often returned when she was ignoring problems with her husband and consequently feeling more isolated from him.
In Session 3, while reviewing the home practice, Sophia talked about how angry she became when someone left their shopping cart haphazardly in the supermarket parking lot, and it rolled down and hit her car. She said that she could not stop thinking about how inconsiderate that person who left the cart was, and it ruined the rest of her day. This was a perfect lead-in to the Empty Boat Analogy. The group was told the story about a man on his boat who is awakened by the sound of another boat hitting his boat. When he comes up to the deck he is angry at the other boatman who hit him. When he looks more carefully at the other boat, he realizes that the other boat is empty and has merely drifted into his. The group discussed what impact this had on the boatman’s anger. Sophia saw how if she regarded the shopping cart incident as more neutral, versus being aimed at her, it diminished some of her anger. But she wondered how she could possibly view it that way in the heat of the moment. When the group was asked what Sophia might do, another group member suggested using a three minute breathing space the next time something like this occurred.
In Session 4, the Suffering Equation was used to continue to illustrate the drawbacks of experiential avoidance . The equation SUFFERING = RESISTANCE X PAIN was written on the board, where pain was described as physical or emotional pain such as depression [52]. Sophia and the other participants were told that pain is inevitable in life, which leads to a certain amount of suffering. But resisting the pain actually increases suffering. The group was asked if anyone could think of a situation in which resisting or avoiding something made the situation worse. Sophia said that she watched a lot of TV when she felt depressed to distract herself and avoid self-loathing feelings, and so that she would not “inflict” herself upon her loved ones. However in group discussion, she realized that this further isolated her, and admitted that watching TV all day made her feel even more worthless.
At this point, while Sophia was starting to be curious about what it would be like to relate to her depression differently, she wondered if not resisting her depression would be akin to giving up. This invited a discussion about acceptance versus resignation. Sophia found it helpful to think about how in Alcoholics Anonymous, members must first accept that they are “alcoholics” before they can change their actions. In a similar manner, relinquishing the struggle to escape depression may set the path for recovery.
The Donkey Standoff Exercise [53] was used in Session 5 to illustrate the concept of moving forward in life while still having symptoms of depression. Sophia was told of the difficulty of pulling a donkey by a rope directly in front of it, because the donkey will resist mightily. Instead, the way to get the donkey moving is to move alongside the donkey and look in the direction that you want to go. The group discussed the concept of moving forward in life alongside the depression, instead of resisting the depression fruitlessly or standing still in life waiting for the depression to completely disappear.
In Session 7, another modification that built on the black dog metaphor was used called the Frankenstein Exercise. This exercise was originally observed in a mindfulness-based stress reduction class. All the participants, including Sophia, were paired with other group members. Sophia played the role of “Frankenstein monster” in several scenarios, and then switched with her partner to take the role of “victim.” Frankenstein would come toward the victim, and then the victim could react to Frankenstein in several ways, just as participants could react to depression coming toward them in several ways. Sophia was asked what it felt like when she were instructed to freeze and cower in front of Frankenstein (submissive), sidestep Frankenstein (avoidant), forcefully hold Frankenstein at a distance (resistant), or come close to Frankenstein, hold his arm, and lead him in the direction she wanted to go (mindfully assertive). These scenarios were used to discuss how the mindfully assertive stance did not change the monster (depression), but allowed Sophia to start to take back control and direction in her life without needing to avoid or fight the depression. She did not need to wait for the depression to resolve before doing things in her life that she found meaningful.
Finally, in Session 8, the Self-Esteem Equation [54] was used to help participants understand the relationship between expectations, self-esteem, and depression. The equation “Self-Esteem = Achievements/Expectations” was written on the board and discussed. Sophia realized that she had unrealistic, unachievable expectations of herself. She had always thought that setting impossibly high goals of herself would be motivating. This equation helped her to understand that these impossible expectations actually undermined her self-esteem and caused her to sink further into depression, which then decreased her motivation to accomplish things. She was interested in coming up with more realistic goals for herself, such as finding part-time work in medical records and being more open about her feelings with her husband.
When sharing her overall experience with the group in Session 8, Sofia said she still found it hard to do sitting meditations, but was taking mindful walks and found the 3-min breathing spaces to be very helpful throughout the day. She said that she was starting to see how some of the negative things she thought about herself may just be “thoughts” and not “facts.” When she approached her self-talk this manner, she found it easier to not get stuck in these thoughts. As a result, she was spending more time with her husband and less time in front of the TV. Group members gave Sofia the feedback that she looked “lighter,” and Sofia acknowledged that she felt less depressed and more hopeful about the future.
Evidence of MBCT for TRD
There is a growing body of evidence that MBCT is an effective treatment for active depression [44, 55]. MBCT was better than Treatment As Usual (TAU) in patients with three or more episodes of depression [32], including those with a history of suicidal ideation [56]. When compared to active competitors, MBCT was shown to be equally effective to CBT [57, 58] and superior to a psycho-educational control group designed to be structurally equivalent to MBCT but excluding mindfulness meditation practice [25]. Improvements in depressive symptoms persisted through the 26-week follow-up period of one study [25] and for up to 5 years of follow-up in another [17].
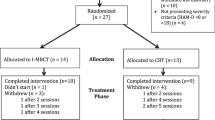
There are fewer studies of MBCT’s efficacy on TRD in particular. Kenny and Williams [59] studied the effects of MBCT on participants with continuing symptoms of depression despite treatment with antidepressant medication or CBT or both in a small sample of 50 participants. They reported a mean pre-MBCT Beck Depression Inventory (BDI) score of 24, versus a post-MBCT score of 14. In another small study, Eisendrath and colleagues [60] reported the results of MBCT augmentation of psychotherapy and medication treatment for 51 participants who were currently depressed and had failed to remit with at least two antidepressant trials. They reported a similar drop in BDI from 24 to 15.
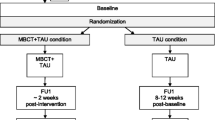
Eisendrath and colleagues [61] recently presented the results of a large randomized controlled trial (n=173) of MBCT versus a manualized active control for people with TRD. The control condition was the Health Enhancement Program (HEP) that includes physical activity, nutritional education, and music therapy [62]. They reported a significantly greater mean percent reduction in HAM-D in MBCT versus HEP (37 % versus 25 %, p = .01) and a significantly greater number of treatment responders (30 % versus 17 %, p = .029).
Mechanism of Change
As discussed earlier, many of the same mechanisms of change may be at play in the reduction in active depressive symptoms versus relapse prevention. Unfortunately, few studies have been done to study the mechanism of change in active depression . We can look to studies that reported on MBCT’s effect on residual symptoms of depression to provide some illumination on the topic.
Kuyken and colleagues [43] found that enhanced mindfulness and increased self-compassion mediated the effect of MBCT on post-treatment symptoms of depression in a population of patients with three or more depressive episodes who were in full or partial remission. A small RCT done with recurrently depressed patients, the majority of them in partial remission, showed that reductions in brooding (an aspect of rumination) and increases in mindfulness mediated the effects of MBCT on depressive symptoms [63]. Another RCT with patients with three or more previous depressive episodes, with and without a current depressive episode, found that effect on depressive symptoms were mediated by a decrease in worry and rumination, and an increase in the mindfulness skill “accept without judgment” [32]. Batink and colleagues [64] found that the effects of MBCT on residual symptoms of depression were mediated by changes in mindfulness skills and worry, but did not find rumination to be a mediator.
Another mechanism by which MBCT may reduce depressive symptoms is through increasing momentary positive emotions, which could lead to an “upward spiral” in affect and cognition [65]. In support of this theory, Geschwind and colleagues [66] found that MBCT compared to a waitlist control increased momentary positive emotions and reward from pleasant daily life activities for people with a history of MDD and current residual depressive symptoms. Batink and colleagues [64] found that changes in positive affect mediated 61 % of the effect of MBCT on residual depressive symptoms. And Garland and colleagues [65] found that MBCT enhanced momentary positive cognition, and appeared to strengthen the relationship between current positive affect and positive cognition the next day.
In terms of brain changes associated with MBCT, Eisendrath and colleagues [61] recently presented fMRI data regarding the effects of MBCT training compared to the aforementioned HEP control condition in a TRD population. Relative to HEP, during a working memory (WM) task, MBCT was associated with increased dorsolateral prefrontal cortex activation during WM encoding and maintenance and decreased ventrolateral activation during WM maintenance. In addition, in MBCT, but not in HEP, Hamilton Depression Rating Scale-17 improvement at 8 weeks was associated with enhanced regulation of amygdala activity during WM performance. Taken as a whole, these fMRI findings suggest MBCT has significant effects on brain circuitry that is associated with enhanced dorsolateral executive control mechanisms relative to ventral affective processing regions.
Practical Considerations of MBCT for TRD
Patient Selection
Overall, studies of MBCT have reported high adherence, low attrition rates, and no serious adverse events related to MBCT interventions [55]. Participants would be best served if they are able to tolerate a group format, can attend all eight weekly sessions, and are willing and able to do home practice.
Early studies suggested that MBCT was only effective in preventing depressive relapse for those with three or more episodes of depression [9, 67]. However a more recent study, albeit an open study, found that the number of previous episodes did not impact result when treating active depression, nor did the severity of depression [17]. Patients who have concurrent suicidal ideation may benefit from MBCT, in that their BDI scores have been shown to decrease with treatment [59]. However they may not experience a decrease in their suicidal ideation [56], and those with a history of suicide attempt were shown to have a higher dropout rate in MBCT trials [13].
MBCT may be particularly useful for depressed patients with psychiatric and physical comorbidities. For example, although results are mixed, many studies suggest MBCT may decrease anxiety [17, 24, 68, 69], making it an appealing treatment for TRD patients with comorbid anxiety. Patients with a history of childhood adversity may benefit more from MBCT than those who did not have childhood adversity [67, 70]. In addition, mindfulness in general has been linked to better physical and emotional functioning in those with chronic pain [71, 72].
Home Practice
Home Practice closely follows the MBCT manual recommendations [73]. Participants receive CDs or audio downloads of guided meditations (available through www.guilford.com/MBCT_materials) to practice with at home. Participants are encouraged to practice 6 days per week, approximately 45 min per day. In the TRD population, participants may find this amount of home practice especially daunting. Given that no clear relationship between total time of practice and clinical outcomes has been established in mindfulness-based interventions [17, 74], more emphasis may be placed on practicing shorter meditations, and utilizing 3 min breathing spaces throughout the day. Shortening the home practice to 30 min/day may be sufficient to sustain positive effects [17] and even 15 min a day may be effective for participants with mild to moderate depression [24] .
Group Size
The developers of MBCT created groups of around 12 people in their research [73]. Group size can vary depending on resources available, but generally should be no larger than 16 people.
Format
Groups run for 8 consecutive weeks, with 2.25 h per session. There are usually 2–3 facilitators per group. Of note, Pots and colleagues [24] adapted the intervention to run for 11 sessions with 1.5 h per session for people with mild to moderate depressive symptomatology.
Facilitator training: Facilitators should have training in psychotherapy, treatment of mood disorders, and have a familiarity with cognitive behavioral therapy. They should also have some familiarity with running groups. In addition, the developers of MBCT firmly believe that facilitators should have their own, ongoing mindfulness practice [73]. Their own practice helps facilitators to demonstrate and embody mindfulness for the group members, and clarifies facilitators’ own conceptions about pain, suffering, and acceptance [48]. Given that MBCT is asking participants with TRD to pay direct attention to experiences they would much rather avoid, the facilitators own familiarity and embodiment of this process is a key element to group success.
Summary/Conclusions
In summary, MBCT appears to be a safe and promising treatment for TRD with a growing evidence base. There are several challenges in treating patients with TRD, such as potential motivational and attentional deficits and multiple comorbidities. These challenges can be addressed with modifications to the original format, as outlined in this chapter and elsewhere [47, 48]. Despite the challenges, people with TRD may particularly benefit from this type of intervention, given that they are often ruminative with persistent self-critical thoughts [75].
The mechanisms by which MBCT may exert its effect are still being investigated. However several potential mediators such as increased self-compassion, decreased rumination, increased emotion regulation, and increased positive affect have been identified. It may be that several of these mediators contribute to the overall effect of the intervention. Globally, Chiesa [25] suggests that the benefits of mindfulness may be related to a “radical shift” in an individual’s attitude toward his or her own experience that leads him/her to “reperceive” in a more adaptive and less reactive way.
Identifying further neural correlates of MBCT treatment would be illuminating, especially given recent evidence that MBCT may exert its effects via circuitry involving regions such as the prefrontal cortex and the amgydala [38, 61]. So far, two EEG studies have yielded contradictory findings on MBCT’s effect on prefrontal alpha-asymmetry [26, 76]. If we better understand how MBCT affects brain circuitry, we might be able to predict which patients would benefit from the intervention the most. We also may be able to predict patient response based on genetics, although we are in the infancy of this research now. A recent study of patients with residual depressive symptoms suggested that gene variation (of an acetylcholine receptor and an opioid receptor) may moderate how MBCT boosts positive affect [77].
There are several areas of investigation that would help to clarify the potential mediators of MBCT’s effect, and could help target the intervention to those who would benefit the most from it. However, there is already a sound theoretical rationale for applying MBCT to TRD as well as a growing evidence base to support its use.
References
UN World Health Organization. World Report on Disability [Internet]. 2011. Accessed 15 Jun 2015. Available from http://www.who.int/disabilities/world_report/2011/report.pdf.
Trivedi MH, Rush AJ, Crismon ML, Kashner TM, Toprac MG, Carmody TJ, et al. Clinical results for patients with major depressive disorder in the Texas Medication Algorithm Project. Arch Gen Psychiatry. 2004;61(7):669–80.
Souery D, Papakostas GI, Trivedi MH. Treatment-resistant depression. J Clin Psychiatry. 2006;67:16–22.
Nemeroff CB. Prevalence and management of treatment-resistant depression. J Clin Psychiatry. 2007;68(8):17–25.
Rush A, Trivedi M, Wisniewski S, Nierenberg A, Stewart J, Warden D, et al. Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: a STAR* D report. Am J Psychiatr. 2006;163(11):1905–17.
Crown WH, Finkelstein S, Berndt ER, Ling D, Poret AW, Rush AJ, et al. The impact of treatment-resistant depression on health care utilization and costs. J Clin Psychiatry. 2002;63(11):963–71.
Greden JF. The burden of disease for treatment-resistant depression. J Clin Psychiatry. 2001;62 Suppl 16:26–31.
Segal Z, Williams JM, Teasdale J. Mindfulness-based cognitive therapy for depression: a new approach to preventing relapse. 1st ed. New York, NY: Guilford; 2002.
Teasdale JD, Segal ZV, Williams JM, Ridgeway VA, Soulsby JM, Lau MA. Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. J Consult Clin Psychol. 2000;68(4):615–23.
Bondolfi G, Jermann F, der Linden MV, Gex-Fabry M, Bizzini L, Rouget BW, et al. Depression relapse prophylaxis with Mindfulness-Based Cognitive Therapy: replication and extension in the Swiss health care system. J Affect Disord. 2010;122(3):224–31.
Godfrin KA, van Heeringen C. The effects of mindfulness-based cognitive therapy on recurrence of depressive episodes, mental health and quality of life: a randomized controlled study. Behav Res Ther. 2010;48(8):738–46.
Piet J, Hougaard E. The effect of mindfulness-based cognitive therapy for prevention of relapse in recurrent major depressive disorder: a systematic review and meta-analysis. Clin Psychol Rev. 2011;31(6):1032–40.
Kuyken W, Byford S, Taylor RS, Watkins E, Holden E, White K, et al. Mindfulness-based cognitive therapy to prevent relapse in recurrent depression. J Consult Clin Psychol. 2008;76(6):966–78.
Segal ZV, Bieling P, Young T, MacQueen G, Cooke R, Martin L, et al. Antidepressant monotherapy vs sequential pharmacotherapy and mindfulness-based cognitive therapy, or placebo, for relapse prophylaxis in recurrent depression. Arch Gen Psychiatry. 2010;67(12):1256–64.
Kuyken W, Hayes R, Barrett B, Byng R, Dalgleish T, Kessler D, et al. Effectiveness and cost-effectiveness of mindfulness-based cognitive therapy compared with maintenance antidepressant treatment in the prevention of depressive relapse or recurrence (PREVENT): a randomised controlled trial. Lancet. 2015;S0140–6736(14):62222–4. Internet article cited Jun 15 2015.
Mathew KL, Whitford HS, Kenny MA, Denson LA. The long-term effects of mindfulness-based cognitive therapy as a relapse prevention treatment for major depressive disorder. Behav Cogn Psychother. 2010;38(05):561–76.
Munshi K, Eisendrath S, Delucchi K. Preliminary long-term follow-up of mindfulness-based cognitive therapy-induced remission of depression. Mindfulness. 2013;4(4):354–61.
Teasdale JD. Cognitive vulnerability to persistent depression. Cognit Emot. 1988;2(3):247–74.
Miranda J, Persons JB. Dysfunctional attitudes are mood-state dependent. J Abnorm Psychol. 1988;97(1):76–9.
Miranda J, Persons JB, Byers CN. Endorsement of dysfunctional beliefs depends on current mood state. J Abnorm Psychol. 1990;99(3):237–41.
Segal ZV, Kennedy S, Gemar M, Hood K, Pedersen R, Buis T. Cognitive reactivity to sad mood provocation and the prediction of depressive relapse. Arch Gen Psychiatry. 2006;63(7):749–55.
Segal ZV, Gemar M, Williams S. Differential cognitive response to a mood challenge following successful cognitive therapy or pharmacotherapy for unipolar depression. J Abnorm Psychol. 1999;108(1):3–10.
Kabat-Zinn J. Mindfulness for beginners: reclaiming the present moment – and your life. Boulder, CO: Sounds True; 2011.
Pots WT, Meulenbeek PA, Veehof MM, Klungers J, Bohlmeijer ET. The efficacy of mindfulness-based cognitive therapy as a public mental health intervention for adults with mild to moderate depressive symptomatology: a randomized controlled trial. PLoS One. 2014;9(10):e109789.
Chiesa A, Castagner V, Andrisano C, Serretti A, Mandelli L, Porcelli S, et al. Mindfulness-based cognitive therapy vs. psycho-education for patients with major depression who did not achieve remission following antidepressant treatment. Psychiatry Res. 2015;226(2):474–83.
Bostanov V, Keune PM, Kotchoubey B, Hautzinger M. Event-related brain potentials reflect increased concentration ability after mindfulness-based cognitive therapy for depression: a randomized clinical trial. Psychiatry Res. 2012;199(3):174–80.
De Raedt R, Baert S, Demeyer I, Goeleven E, Raes A, Visser A, et al. Changes in attentional processing of emotional information following mindfulness-based cognitive therapy in people with a history of depression: Towards an open attention for all emotional experiences. Cogn Ther Res. 2012;36(6):612–20.
Fresco DM, Segal ZV, Buis T, Kennedy S. Relationship of posttreatment decentering and cognitive reactivity to relapse in major depression. J Consult Clin Psychol. 2007;75(3):447.
van der Velden A, Kuyken W, Wattar U, Crane C, Pallesen KJ, Dahlgaard J, et al. A systematic review of mechanisms of change in mindfulness-based cognitive therapy in the treatment of recurrent major depressive disorder. Clin Psychol Rev. 2015;37:26–39.
Chiesa A, Anselmi R, Serretti A. Psychological mechanisms of mindfulness-based interventions: what do we know? Holist Nurs Pract. 2014;28(2):124–48.
Baer RA. Mindfulness training as a clinical intervention: a conceptual and empirical review. Clin Psychol Sci Pract. 2003;10(2):125–43.
Van Aalderen J, Donders A, Giommi F, Spinhoven P, Barendregt H, Speckens A. The efficacy of mindfulness-based cognitive therapy in recurrent depressed patients with and without a current depressive episode: a randomized controlled trial. Psychol Med. 2012;42(05):989–1001.
Nolen-Hoeksema S. Responses to depression and their effects on the duration of depressive episodes. J Abnorm Psychol. 1991;100(4):569–82.
Nolen-Hoeksema S, Morrow J. Effects of rumination and distraction on naturally occurring depressed mood. Cognit Emot. 1993;7(6):561–70.
Martin LL, Tesser A. Some ruminative thoughts. Adv Soc Cognit. 1996;9:1–47.
Crane C, Winder R, Hargus E, Amarasinghe M, Barnhofer T. Effects of mindfulness-based cognitive therapy on specificity of life goals. Cogn Ther Res. 2012;36(3):182–9.
Arch JJ, Craske MG. Mechanisms of mindfulness: emotion regulation following a focused breathing induction. Behav Res Ther. 2006;44(12):1849–58.
Chiesa A, Serretti A, Jakobsen JC. Mindfulness: top–down or bottom–up emotion regulation strategy? Clin Psychol Rev. 2013;33(1):82–96.
Quirk GJ, Beer JS. Prefrontal involvement in the regulation of emotion: convergence of rat and human studies. Curr Opin Neurobiol. 2006;16:723–7.
Goldapple K, Segal Z, Garson C, Lau M, Bieling P, Kennedy S, et al. Modulation of cortical-limbic pathways in major depression: treatment-specific effects of cognitive behavior therapy. Arch Gen Psychiatry. 2004;61(1):34–41.
van den Hurk PAM, Janssen BH, Giommi F, Barendregt HP, Gielen SC. Mindfulness meditation associated with alterations in bottom-up processing: psychophysiological evidence for reduced reactivity. Int J Psychophysiol. 2010;78(2):151–7.
Neff KD. The development and validation of a scale to measure self-compassion. Self Identity. 2003;2(3):223–50.
Kuyken W, Watkins E, Holden E, White K, Taylor RS, Byford S, et al. How does mindfulness-based cognitive therapy work? Behav Res Ther. 2010;48(11):1105–12.
Strauss C, Cavanagh K, Oliver A, Pettman D. Mindfulness-based interventions for people diagnosed with a current episode of an anxiety or depressive disorder: a meta-analysis of randomised controlled trials. PLoS One. 2014;9(4):e96110.
Kornstein SG, Schneider RK. Clinical features of treatment-resistant depression. J Clin Psychiatry. 2001;62:18–25.
Bair MJ, Robinson RL, Eckert GJ, Stang PE, Croghan TW, Kroenke K. Impact of pain on depression treatment response in primary care. Psychosom Med. 2004;66(1):17–22.
Eisendrath S, Chartier M, McLane M. Adapting mindfulness-based cognitive therapy for treatment-resistant depression: a clinical case study. Cogn Behav Pract. 2011;18(3):362–70.
Sipe WE, Eisendrath SJ. Mindfulness-based cognitive therapy for treatment-resistant depression. In: Baer R, editor. Mindfulness-based treatment approaches: clinician's guide to evidence base and applications. 2nd edn. Elsevier; 2014. p. 61–76.
Hayes SC, Strosahl KD, Wilson KG. Acceptance and commitment therapy: an experiential approach to behavior change. New York: Guilford; 1999.
Zettle RD. ACT for depression: a clinician's guide to using acceptance & commitment therapy in treating depression. Oakland, CA: New Harbinger; 2007.
Johnstone M. Living with a black dog: his name is depression. Kansas City: Andrews McMeel; 2006.
Young S. Break through pain: a step-by-step mindfulness meditation program for transforming chronic and acute pain. Boulder, CO: Sounds True; 2004.
Luoma JB, Hayes SC, Walser RD. Learning ACT: an acceptance and commitment therapy skills-training manual for therapists. Oakland, CA: New Harbinger; 2007.
Eisendrath SJ. Psychiatric problems. In: Bongard F, Sue D, editors. Current critical care diagnosis and treatment. New York, NY: Lange Medical Books/McGraw Hill; 2002.
Chiesa A, Serretti A. Mindfulness based cognitive therapy for psychiatric disorders: a systematic review and meta-analysis. Psychiatry Res. 2011;187(3):441–53.
Barnhofer T, Crane C, Hargus E, Amarasinghe M, Winder R, Williams JM. Mindfulness-based cognitive therapy as a treatment for chronic depression: a preliminary study. Behav Res Ther. 2009;47(5):366–73.
Manicavasagar V, Perich T, Parker G. Cognitive predictors of change in cognitive behaviour therapy and mindfulness-based cognitive therapy for depression. Behav Cogn Psychother. 2012;40(02):227–32.
Omidi A, Mohammadkhani P, Mohammadi A, Zargar F. Comparing mindfulness based cognitive therapy and traditional cognitive behavior therapy with treatments as usual on reduction of major depressive disorder symptoms. Iran Red Crescent Med J. 2013;15(2):142–6.
Kenny M, Williams J. Treatment-resistant depressed patients show a good response to mindfulness-based cognitive therapy. Behav Res Ther. 2007;45(3):617–25.
Eisendrath SJ, Delucchi K, Bitner R, Fenimore P, Smit M, McLane M. Mindfulness-based cognitive therapy for treatment-resistant depression: a pilot study. Psychother Psychosom. 2008;77(5):319–20.
Eisendrath SJ. The practicing alternative techniques to heal depression study: a randomized controlled trial of mindfulness-based cognitive therapy for treatment-resistant depression with clinical and fmri effects. Findings presented at American Psychiatric Association Annual Meeting; Toronto; May 2015.
MacCoon DG, MacLean KA, Davidson RJ, Saron CD, Lutz A. No sustained attention differences in a longitudinal randomized trial comparing mindfulness based stress reduction versus active control. PLoS One. 2014;9(6):e97551.
Shahar B, Britton WB, Sbarra DA, Figueredo AJ, Bootzin RR. Mechanisms of change in mindfulness-based cognitive therapy for depression: preliminary evidence from a randomized controlled trial. Int J Cognit Ther. 2010;3(4):402–18.
Batink T, Peeters F, Geschwind N, van Os J, Wichers M. How does MBCT for depression work? Studying cognitive and affective mediation pathways. PLoS One. 2013;8(8):e72778.
Garland EL, Geschwind N, Peeters F, Wichers M. Mindfulness training promotes upward spirals of positive affect and cognition: multilevel and autoregressive latent trajectory modeling analysis. Front Psychol. 2015;6:15. Internet article accessed 15 Jun 2015.
Geschwind N, Peeters F, Drukker M, van Os J, Wichers M. Mindfulness training increases momentary positive emotions and reward experience in adults vulnerable to depression: a randomized controlled trial. J Consult Clin Psychol. 2011;79(5):618–28.
Ma SH, Teasdale JD. Mindfulness-based cognitive therapy for depression: replication and exploration of differential relapse prevention effects. J Consult Clin Psychol. 2004;72(1):31–40.
Kim YW, Lee SH, Choi TK, Suh SY, Kim B, Kim CM, et al. Effectiveness of mindfulness-based cognitive therapy as an adjuvant to pharmacotherapy in patients with panic disorder or generalized anxiety disorder. Depress Anxiety. 2009;26(7):601–6.
Piet J, Hougaard E, Hecksher MS, Rosenberg NK. A randomized pilot study of mindfulness‐based cognitive therapy and group cognitive‐behavioral therapy for young adults with social phobia. Scand J Psychol. 2010;51(5):403–10.
Williams JMG, Crane C, Barnhofer T, Brennan K, Duggan DS, Fennell MJ, et al. Mindfulness-based cognitive therapy for preventing relapse in recurrent depression: a randomized dismantling trial. J Consult Clin Psychol. 2014;82(2):275.
McCracken LM, Gauntlett-Gilbert J, Vowles KE. The role of mindfulness in a contextual cognitive-behavioral analysis of chronic pain-related suffering and disability. Pain. 2007;131(1):63–9.
Rosenzweig S, Greeson JM, Reibel DK, Green JS, Jasser SA, Beasley D. Mindfulness-based stress reduction for chronic pain conditions: variation in treatment outcomes and role of home meditation practice. J Psychosom Res. 2010;68(1):29–36.
Segal Z, Williams JM, Teasdale J. Mindfulness-based cognitive therapy for depression. 2nd ed. New York, Ny: Guilford; 2013.
Carmody J, Baer RA. How long does a mindfulness‐based stress reduction program need to be? A review of class contact hours and effect sizes for psychological distress. J Clin Psychol. 2009;65(6):627–38.
Moore RG, Garland A. Cognitive therapy for chronic and persistent depression. England, UK: John Wiley & Sons; 2003.
Barnhofer T, Duggan D, Crane C, Hepburn S, Fennell MJ, Williams JM. Effects of meditation on frontal alpha-asymmetry in previously suicidal individuals. Neuroreport. 2007;18(7):709–12.
Bakker J, Lieverse R, Menne-Lothmann C, Viechtbauer W, Pishva E, Kenis G, et al. Therapygenetics in mindfulness-based cognitive therapy: do genes have an impact on therapy-induced change in real-life positive affective experiences? Transl Psychiatry. 2014;4(4):e384.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Deen, S., Sipe, W., Eisendrath, S.J. (2016). Mindfulness-Based Cognitive Therapy for Treatment-Resistant Depression. In: Eisendrath, S. (eds) Mindfulness-Based Cognitive Therapy. Springer, Cham. https://doi.org/10.1007/978-3-319-29866-5_12
Download citation
DOI: https://doi.org/10.1007/978-3-319-29866-5_12
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-29864-1
Online ISBN: 978-3-319-29866-5
eBook Packages: MedicineMedicine (R0)