Abstract
Major depressive disorder is often chronic and characterized by relapse and recurrence despite successful treatments to induce remission. Mindfulness-based cognitive therapy (MBCT) was developed as a means of preventing relapse for individuals in remission using cognitive interventions. In addition, MBCT has preliminarily been found to be useful in treating active depression. This current investigation is unique in evaluating the long-term outcome of individuals with active depression who achieved remission with MBCT. Eighteen participants who achieved remission after an 8-week MBCT group were seen for evaluation at a mean follow-up interval of 48.7 months (SD = 10.2) after completing treatment. The current study shows that in these participants, the gains achieved after the initial treatment including remission of depression, decreased rumination, decreased anxiety, and increased mindfulness continued for up to 58.9 months of follow-up. The data suggest that all levels of depression from less recurrent and mild to more recurrent and severe were responsive to MBCT. The average number of minutes per week of continued practice in our cohort was 210, but the number of minutes of practice did not correlate with depression outcomes. MBCT's effects may be more related to regularity of practice than specific quantity. This study provides a preliminary exploration of MBCT's long-term effects, which can aid in future research with a typically chronic illness.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Major depressive disorder (MDD) is often chronic and characterized by relapse and recurrence despite successful treatments to induce remission. This course of depression often leads to individual disability as well as personal, familial, and societal suffering (Judd et al. 2000). As a result of this, many studies have focused on the prevention of relapse when considering the treatment of depression.
Interest has been growing in psychotherapy alternatives to long-term antidepressant prophylaxis. Cognitive–behavioral therapy (CBT) has been shown to be an effective adjunct to medications in relapse prevention (Fava and Ruini 2002; McPherson et al. 2005; Stimpson et al. 2002). Additionally, CBT has shown to be a viable treatment for medication-resistant depression (Fava et al. 1998; Fava et al. 1997). It is thought that cognitive therapies are effective in relapse prevention because following successful treatment of a depressive episode, they interfere with the mild depressive states that can reactivate the negative cognitive processing present during the prior depressive episode (Teasdale et al. 1995). Therefore, cognitive interventions to target that mild negative affect can help prevent escalating into more severe depressive states.
Mindfulness-based cognitive therapy (MBCT) was developed as a means of preventing relapse for individuals in remission by teaching mindfulness practices to increase awareness of cognitive patterns that increase the likelihood of or perpetuate depressive cycles (Godfrin and van Heeringen 2010; Ma and Teasdale 2004; Teasdale et al. 2000). MBCT is a treatment that integrates mindfulness meditation training with cognitive–affective processing (Teasdale and Barnard 1993; J. D. Teasdale 1993). It emphasizes changing the relationship with one's thoughts and feelings, thereby interrupting the downward spiral typical of a depressive episode (Segal et al. 2002; Teasdale et al. 1995), which is in contrast with CBT's focus on changing thought content. MBCT was specifically developed as a relapse prevention intervention as it emphasizes the daily practice of health-promoting behaviors such as mindfulness meditation and yoga and encouraging long-term engagement in these techniques (Segal et al. 2010). MBCT for treatment-resistant depression utilizes an adapted version of the original manual developed by Segal et al. (Segal et al. 2002) which describes eight 2.25-h sessions with themes that promote enhanced emotional regulation through increasing individual's nonjudgmental awareness of whatever is present. MBCT studies indicate that this intervention reduces relapse in patients with three or more previous episodes by approximately 50 % when compared to treatment as usual (Ma and Teasdale 2004) and appears to be equivalent to maintenance medication for relapse prevention (Kuyken et al. 2008; Segal et al. 2010).
As evidence for MBCT in the prevention of depressive relapses has been growing, there is a need for longer follow-up periods to assess the effects of MBCT both on relapse and depression levels. Currently, most studies have been limited to follow-up intervals of 15 months or less (Kuyken et al. 2008). Only one recent study surpassed that interval and showed that statistically significant decreases in depression severity from pre- to post-MBCT treatment were maintained over 34 months (Mathew et al. 2010).
Although designed for relapse prevention, MBCT has also been found to be effective in several open trials of active or residual depression (Eisendrath et al. 2008; Finucane and Mercer 2006; Kenny and Williams 2007). In a significant percentage of these patients, remission of depression has occurred with MBCT treatment. One trial has shown it to be equivalent to Cognitive–behavioral therapy (CBT) in the treatment of current depression (Manicavasgar et al. 2011).
This current investigation is unique in evaluating the long-term outcome of individuals with active depression who achieved remission with MBCT. The primary goal of this study was to examine depression levels and persistence of remission in patients who completed an 8-week MBCT group, achieved documented remission, and were seen for evaluation at a mean follow-up interval of 48.7 months (SD = 10.2) after completing treatment. In addition, levels of rumination, anxiety, and mindfulness were examined in order to explore the potential mechanisms underlying MBCT. For example, one study described rumination as prolonging the intensity of the negative mood, while distraction and acceptance decreased the intensity of the negative mood (Singer and Dobson 2007).
Method
Participants
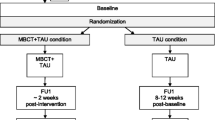
The participants of the study were adult outpatients at Langley Porter Psychiatric Hospital and Clinics (LPPH&C) at the University of California San Francisco, an urban setting, who completed a MBCT group between August 2006 and March 2009 and had an initial Beck Depression Inventory (BDI) score of greater than 10 prior to starting the group and 10 or less upon completion of the group, thereby achieving symptomatic remission. There is variability in the cut points on the BDI to define remission as some studies use a score of <12 as indicating remission (Riedel et al. 2010) and others use a score of <10 (Reeves et al. 2012). Based on our review of these studies, we adopted a score of 10 or less as defining remission. Of the initial 87 patients that participated in the MBCT group between those years, 33 met the remission criteria for the study. Of the 33 individuals, 18 agreed to participate in this study and come in for a follow-up interview (see Fig. 1). The study was approved by the university's institutional Committee on Human Research and has therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki. Written informed consent to complete the interview and questionnaires was obtained from the participants prior to starting the session.
Study Design
The study is an open examination of long-term clinical outcomes for patients with active depression who achieved remission in 8-week MBCT groups. Each participant was asked to come in to LPPH&C for an in-person follow-up interview by the researcher and complete an assessment battery including the following measures:
-
Beck Depression Inventory (BDI)-II: The BDI-II is a 21-item self-report instrument that is one of the most widely used instruments for measuring the severity of depression in clinical and research settings. Items are rated on a scale from 0 to 3, with higher scores reflecting more depressive symptoms (total score range = 0–63). Items include symptoms of depression such as hopelessness and irritability, cognitions such as guilt or feelings of being punished, as well as physical symptoms such as fatigue, weight loss, and lack of interest in sex (Beck et al. 1996).
-
Ruminative Response Scale (RRS): The RRS is a 22-item self-report instrument with high internal reliability with Cronbach’s alpha ranging from 0.88 to 0.92. It has high test–retest reliability. Items focus on the meaning of rumination, the subjective feelings related to depressed mood, symptoms, and causes and consequences of the ruminative thinking. High scores appear to be associated with a vulnerability factor to depression (Nolen-Hoeksema 2000; Roberts et al. 1998) as well as being able to predict depression severity in clinically depressed populations (Nolen-Hoeksema 2000).
-
State-Trait Anxiety Inventory (STAI): The STAI is a widely used 22-item self-report instrument designed to differentiate between the temporary condition of “state anxiety” (Y1) and the more general and long-standing quality of “trait anxiety” (Y2). The norms for anxiety levels in a depressed population are 54 for the state subscale and 53 for the trait subscale (Spielberger et al. 1970).
-
Freiburg Mindfulness Inventory (FMI): The FMI is a 30-item self-report scale that utilizes a single score. It was designed to measure mindfulness where knowledge of a Buddhist background of mindfulness cannot be expected (Buchheld et al. 2001). This was used to assess change in mindfulness pre- and post-MBCT. The following factors of mindfulness are included in the FMI: present moment attention, nonjudgmental and non-evaluative attitude towards self and others, openness to negative mind states, and process-oriented insightful understanding. Although newer measures are now available to measure mindfulness, the FMI was one of the more commonly available measures that were used early on when patient data in this study were first captured and utilized in follow-up for continuity and comparability over time.
-
Longitudinal Interval Follow-up Evaluation (LIFE) has been used to delineate depressive episodes over a period of time (Keller et al. 1987). A LIFE interview was conducted by the researcher (K.M.) to assess the longitudinal course of depression since completion of MBCT in these patients by collecting a detailed history of relapse episodes, as well as psychosocial, psychiatric, and treatment information history.
The follow-up scores on the BDI, RRS, STAI, and FMI measures were compared to their pre- and post-MBCT group scores. For the purpose of this study, we designed a 21-item follow-up interview script to verify previously recorded demographic information including a number of prior episodes of depression as well as past and present antidepressant medication use, alumni group attendance, mindfulness practice, and perceptions of usefulness of MBCT.
Statistical Analyses
Means, standard deviations, and percentages were computed to summarize the data. Scale means between independent groups (i.e., remitters vs. non-remitters and completers vs. non-completers) were compared using two-sample t tests and Pearson's chi-square test for percentages (e.g., percent employed). Dependent-sample t tests compared mean values of the remitters between assessment points, and Pearson correlation coefficients indexed the change in BDI scores, and the change on the other scales were estimated and tested.
Results
Table 1 displays demographic information that was collected from previous study records on all 87 participants of the MBCT groups between 2006 and 2009. Among this group, the age ranged between 24 and 81 years old, with 72 % of all participants being female. Prior to starting the MBCT group, 78 % of the patients were on an antidepressant medication. Of the 18 participants at follow-up, two were not on any antidepressants prior to the MBCT group, while six were not on any antidepressants by the time of follow-up. There was no significant difference in demographics between those who had remission of their depression following the 8-week MBCT group and those who did not. Among the remitters, there was no significant difference in demographics between those who came in for the follow-up interview (completers) versus those that did not come in (non-completers) except for race (100 % of the follow-up completers were Caucasian). Depression diagnoses were obtained by pre-treatment M.I.N.I. interviews (mood module) (Sheehan et al. 1998). Using this module, most study participants were diagnosed with MDD. Also, there was no significant difference in the number of lifetime depressive episodes—less than three episodes versus three or more episodes—(p = 0.52) or in severity of depression as measured by pre-BDI scores (p = 0.85) in remitters versus non-remitters. Table 2 displays the mean scores for each measure at the pre-treatment, post-treatment, and follow-up assessments for the 18 participants who attended the follow-up interview.
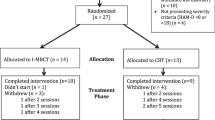
All five measures demonstrated a statistically significant change from pre- to post-. As seen in Fig. 2, depression scores as measured by the BDI significantly improved from pre- to post- (p <0.0001), and depression scores did not significantly change from post- to follow-up (p = 0.71). Similarly, state and trait anxiety as measured by the STAI, and rumination as measured by the RRS, significantly decreased from pre- to post- and did not significantly change from post- to follow-up. The mean rumination score continued to decrease, but the change was not significant. Mindfulness, as measured by the FMI, significantly increased from pre- to post- and did not significantly change from post- to follow-up. From the Pearson correlation coefficients, we noted that the change from pre- to post- and from post- to follow-up scores on the RRS and STAI was positively related, while the FMS inversely related in the same time frame with the BDI (see Table 3).
To investigate whether the participants' attitudes toward MBCT influenced their outcomes in terms of remission of their depression, end of MBCT treatment satisfaction scores on a scale of 1–10 (where 1 is least satisfied and 10 is most satisfied) were analyzed and showed no significant difference between the remitters and non-remitters (p = 0.71). Also, the analysis of the satisfaction scores in the completers versus non-completers indicated that satisfaction with the program did not appear to be a factor in the participants' decision to attend the follow-up interview (p = 0.78).
In order to gain a better understanding about potential mechanisms underlying MBCT’s long-term effects, the correlation of the minutes per week of continued practice in the remitters who completed the study and their scores on the measures was investigated. All participants except one had continued some form of mindfulness practice with an average time of 210 min per week (range 0–630 min per week). There was no statistically significant correlation between the minutes per week of continued practice and variability of their scores on the measures we tracked. The types of mindfulness activities that were practiced, on average, included 13 % body scan, 32 % sitting meditation, 19 % 3-min breathing space, and 35 % movement meditation (yoga, walking). Ten out of the 18 participants interviewed had attended at least one MBCT alumni group session since the completion of their treatment. MBCT alumni groups are once-monthly 1.5 h open groups that are free to “graduates” of MBCT. They serve as mini refreshers on mindfulness practices.
Finally, in reviewing the results of the LIFE interview, participants were not able to give a week-by-week or even month-by-month assessment of levels of depression according to the LIFE guidelines because of recall difficulties. Because of this, LIFE episode data were not analyzable. Most participants had difficulty in quantifying the number of depressive episodes they had experienced since completing MBCT. Seven participants of the 18 interviewed denied having any episodes of depression since completion of the group. One participant had relapses at the same frequency as she was having prior to the group. Notably, this participant was the one out of the 18 that did not do any form of mindfulness practice after completion of the group. The remaining ten participants had some depressive episodes since completion of the group; however, their perception was that the frequency of relapse was decreased, and the length of each episode was shorter than prior to the MBCT intervention.
Discussion
The current study shows that in those participants with significant depressive symptoms who had remission of their depressive symptoms upon completion of the MBCT group, the gains achieved including remission of depressive symptoms, decreased rumination, decreased anxiety, and increased mindfulness continued for up to 58.9 months of follow-up. These findings are consistent with prior research suggesting that MBCT is an effective treatment for current depression as well as for relapse prevention in depression. This study also suggests that for individuals who achieve remission with MBCT, the effects may persist, along with some continued practice, for at least 5 years. This is a longer follow-up period than previously studied.
Most of the participants in this study had greater than or equal to three lifetime episodes of depression prior to the MBCT treatment. However, an equal percentage of individuals with a history of less than three episodes as those with a history of three or more episodes remitted. Also, there was no significant difference in the pre-BDI scores among all of the MBCT group participants, meaning that depression severity was not a predictor of remission. This suggests that all levels of depression from less recurrent and milder symptoms (less than three episodes and lower BDI scores) to more recurrent and more severe symptoms (three or more episodes and higher BDI scores) were responsive to MBCT. This study, however, represents an open trial of MBCT and is in contrast to the randomized clinical trials, which showed MBCT to be effective in preventing relapse only for individuals with three or more episodes of depression (Godfrin and van Heeringen 2010; Ma and Teasdale 2004; Teasdale et al. 2000).
Although not found to be statistically significant, participants' rumination as measured by the RRS showed a continued decrease, and their mindfulness, measured by the FMS, showed a continued increase over the follow-up period. This correlational finding is consistent with a previous research that showed that less rumination was associated with lower depression levels (Bieling et al. 2012; Nolen-Hoeksema 2000; Ramel et al. 2004), and that enhanced mindfulness may facilitate less ruminative processing (Bieling et al. 2012; Birnie et al. 2010; Chambers et al. 2009; Ramel et al. 2004; Robins et al. 2012; Shapiro et al. 2008; Teasdale et al. 2000). Therefore, the inverse relationship of rumination and mindfulness in our participants suggest that increased mindfulness can decrease rumination and, in turn, reduce depression.
As there was no correlation between the number of minutes per week of continued practice in the remitters who completed the follow-up interview and the variability of the scores on the measures, this suggests that the amount of time spent doing formal mindfulness activities such as specific meditation or yoga practice is not obligatory to sustain remission. Although there is conflicting evidence about the importance of continuing practice on maintenance of meditation effects (Carmody et al. 2009), our study did not find such a correlation. As described in one previous study (Davidson et al. 2003), people may become more mindful in their everyday life leading to continued positive effects regardless of time put into formal practice. However, the average number of minutes per week of continued practice in our cohort was 210, which suggests that relatively modest regular practice (on average 30 min/day) may have contributed to this group's ability to sustain such positive effects.
There are several limitations in this study. Most notably, this is an uncontrolled, cross-sectional, retrospective analysis. With only 18 participants agreeing to come in for the follow-up interview, the sample size for the data is small. However, this did represent two thirds of the remitters whom we were able to contact. There may be a selection bias in that the individuals who agreed to participate may be favorably disposed towards their MBCT experience or perhaps be less depressed. Of note, however, these individuals rated the value of their MBCT experience similarly to their peers at the completion of MBCT. Given that 78 % of participants were female and 100 % of participants were Caucasian, it would have been useful to have a more diversified sample. The data were collected by participant recall after an extended period of time, and the instruments were all self-report to align with earlier versions given to participants of pre-MBCT. The duration of time since the MBCT group was not uniform and could have impacted some of the results. Nonetheless, even our minimum follow-up period of 31 months was much longer than that found in the most MBCT studies.
The difficulties in gathering data with the LIFE interview highlighted a weakness of this type of cross-sectional study. Patients have a difficult time recalling their illness course over an interval that averaged 48 months. It would have been preferable to have followed patients prospectively and at much shorter intervals to assess relapse rates. It was noteworthy that participants' inability to specify the number of episodes on the LIFE interview was in contrast to the general estimation (without the use of any structured instrument) of the number of episodes they had given prior to initiating MBCT. It has been shown in previous research that there are often significant errors in lifetime recall of depressive episodes (Simon et al. 1995). As the estimation of number of depressive episodes that had been gathered at entry into MBCT initially were based on patient estimation and not as carefully delineated, as is the case with the LIFE interview, it is difficult to say how accurate these estimations are. Nonetheless the subjective sense of our participants was that relapses had either stopped or become less frequent and less severe. The BDI scores certainly support that sense.
Despite the obvious limitations of this study, it provides a preliminary exploration of MBCT's long-term effects, which can aid in future research. Undoubtedly, a prospective long-term study with an appropriate control group would yield more specific data. This would allow a clearer picture of what factors may be mediating MBCT's effects and in fact, whether these effects can be distinctively attributable to MBCT. If these results are replicated in such studies, it would place greater importance on being able to specifically predict who responds best to MBCT to enhance personalized treatment of major depressive disorder.
References
Beck, A. T., Steer, R. A., & Brown, G. K. (1996). Manual for Beck Depression Inventory—II. San Antonio, TX: Psychological Corporation.
Bieling, P. J., Hawley, L. L., Bloch, R. T., Corcoran, K. M., Levitan, R. D., Young, L. T., et al. (2012). "Treatment-specific changes in decentering following mindfulness-based cognitive therapy versus antidepressant medication or placebo for prevention of depressive relapse": Correction to bieling et al. (2012). Journal of Consulting and Clinical Psychology, 80(3), 372.
Birnie, K., Garland, S. N., & Carlson, L. E. (2010). Psychological benefits for cancer patients and their partners participating in Mindfulness-Based Stress Reduction (MBSR). [Research Support, Non-U.S. Gov't]. Psycho-Oncology, 19(9), 1004–1009.
Buchheld, N., Grossman, P., & Walach, H. (2001). Measuring mindfulness in insiight meditation (Vipassana) and meditation-based psychotherapy. Freiburg: Peter Lang.
Carmody, J., Baer, R. A., Lykins, E. L. B., & Olendzki, N. (2009). An empirical study of the mechanisms of mindfulness in a mindfulness-based stress reduction program. Journal of Clinical Psychology, 65(6), 613–626.
Chambers, R., Gullone, E., & Allen, N. B. (2009). Mindful emotion regulation: an integrative review. Clinical Psychology Review, 29(6), 560–572.
Davidson, R. J., Kabat-Zinn, J., Schumacher, J., Rosenkranz, M., Muller, D., Santorelli, S. F., et al. (2003). Alterations in brain and immune function produced by mindfulness meditation. Psychosomatic Medicine, 65(4), 564–570.
Eisendrath, S. J., Delucchi, K., Bitner, R., Fenimore, P., Smit, M., & McLane, M. (2008). Mindfulness-based cognitive therapy for treatment-resistant depression: a pilot study. Psychotherapy and Psychosomatics, 77(5), 319–320.
Fava, G. A., & Ruini, C. (2002). Long-term treatment of depression: there is more than drugs. Recenti Progressi in Medicina, 93(6), 343–345.
Fava, G. A., Savron, G., Grandi, S., & Rafanelli, C. (1997). Cognitive-behavioral management of drug-resistant major depressive disorder. The Journal of Clinical Psychiatry, 58(6), 278–282. quiz 283-274.
Fava, G. A., Rafanelli, C., Grandi, S., Conti, S., & Belluardo, P. (1998). Prevention of recurrent depression with cognitive behavioral therapy: preliminary findings. Archives of General Psychiatry, 55(9), 816–820.
Finucane, A., & Mercer, S. W. (2006). An exploratory mixed methods study of the acceptability and effectiveness of mindfulness-based cognitive therapy for patients with active depression and anxiety in primary care. BMC Psychiatry, 6, 14.
Godfrin, K. A., & van Heeringen, C. (2010). The effects of mindfulness-based cognitive therapy on recurrence of depressive episodes, mental health and quality of life: a randomized controlled study. Behaviour Research and Therapy, 48(8), 738–746.
Judd, L. L., Akiskal, H. S., Zeller, P. J., Paulus, M., Leon, A. C., Maser, J. D., et al. (2000). Psychosocial disability during the long-term course of unipolar major depressive disorder. Archives of General Psychiatry, 57(4), 375–380.
Keller, M. B., Lavori, P. W., Friedman, B., Nielsen, E., Endicott, J., McDonald-Scott, P., et al. (1987). The longitudinal interval follow-up evaluation: a comprehensive method for assessing outcome in prospective longitudinal studies. Archives of General Psychiatry, 44(6), 540–548.
Kenny, M. A., & Williams, J. M. (2007). Treatment-resistant depressed patients show a good response to mindfulness-based cognitive therapy. Behaviour Research and Therapy, 45(3), 617–625.
Kuyken, W., Byford, S., Taylor, R. S., Watkins, E., Holden, E., White, K., et al. (2008). Mindfulness-based cognitive therapy to prevent relapse in recurrent depression. Journal of Consulting and Clinical Psychology, 76(6), 966–978.
Ma, S. H., & Teasdale, J. D. (2004). Mindfulness-based cognitive therapy for depression: replication and exploration of differential relapse prevention effects. Journal of Consulting and Clinical Psychology, 72(1), 31–40.
Manicavasgar, V., Parker, G., & Perich, T. (2011). Mindfulness-based cognitive therapy Vs cognitive behaviour therapy as a treatment for non-melancholic depression. Journal of Affective Disorders, 130(1–2), 138–144.
Mathew, K. L., Whitford, H. S., Kenny, M. A., & Denson, L. A. (2010). The long-term effects of mindfulness-based cognitive therapy as a relapse prevention treatment for major depressive disorder. Behavioural and Cognitive Psychotherapy, 38(05), 561–576.
McPherson, S., Cairns, P., Carlyle, J., Shapiro, D. A., Richardson, P., & Taylor, D. (2005). The effectiveness of psychological treatments for treatment-resistant depression: a systematic review. Acta Psychiatrica Scandinavica, 111(5), 331–340.
Nolen-Hoeksema, S. (2000). The role of rumination in depressive disorders and mixed anxiety/depressive symptoms. Journal of Abnormal Psychology, 109(3), 504–511.
Ramel, W., Goldin, P. R., Carmona, P., & McQuaid, J. R. (2004). The effects of mindulness meditation on cognitive processes and affect in patients with past depression. Cognitive Therapy and Research, 28(4), 433–455.
Reeves, G. M., Rohan, K. J., Langenberg, P., Snitker, S., & Postolache, T. T. (2012). Calibration of response and remission cut-points on the beck depression inventory-second edition for monitoring seasonal affective disorder treatment outcomes. Journal of Affective Disorders, 138(1), 123–127.
Riedel, M., Möller, H.-J., Obermeier, M., Schennach-Wolff, R., Bauer, M., Adli, M., et al. (2010). Response and remission criteria in major depression—a validation of current practice. Journal of Psychiatric Research, 44(15), 1063–1068.
Roberts, J. E., Gilboa, E., & Gotlib, I. H. (1998). Ruminative response style and vulnerability to episodes of dysphoria: gender, neuroticism, and episode duration. Cognitive Therapy and Research. Special Issue: Cognitive Processes and Vulnerability to Affective Problems, 22(4), 401–423.
Robins, C. J., Keng, S. L., Ekblad, A. G., & Brantley, J. G. (2012). Effects of Mindfulness-Based Stress Reduction on Emotional Experience and Expression: a randomized controlled trial. Journal of Clinical Psychology, 68(1), 117–131.
Segal, Z., Williams, J. M., & Teasdale, J. (2002). Mindfulness-Based Cognitive Therapy for depression. New York: The Guilford.
Segal, Z. V., Bieling, P., Young, T., MacQueen, G., Cooke, R., Martin, L., et al. (2010). Antidepressant monotherapy vs sequential pharmacotherapy and mindfulness-based cognitive therapy, or placebo, for relapse prophylaxis in recurrent depression. Archives of General Psychiatry, 67(12), 1256–1264.
Shapiro, S. L., Oman, D., Thoresen, C. E., Plante, T. G., & Flinders, T. (2008). Cultivating mindfulness: effects on well-being. Journal of Clinical Psychology, 64(7), 840–862.
Sheehan, D. V., Lecrubier, Y., Sheehan, K. H., Amorim, P., Janavs, J., Weiller, E., et al. (1998). The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. The Journal of Clinical Psychiatry, 59(Suppl 20), 22–33. quiz 34-57.
Simon, G. E., Vonkorff, M., Ustun, T. B., Gater, R., Gureje, O., & Sartorius, N. (1995). Is the Lifetime Risk of Depression actually increasing? Journal of Clinical Epidemiology, 48(9), 1109–1118.
Singer, A. R., & Dobson, K. S. (2007). An experimental investigation of the cognitive vulnerability to depression. Behaviour Research and Therapy, 45(3), 563–575.
Spielberger, C., Gorsuch, R. R., & Luchene, R. E. (1970). State-trait anxiety inventory. Palo Alto: Consulting Psychologists.
Stimpson, N., Agrawal, N., & Lewis, G. (2002). Randomised controlled trials investigating pharmacological and psychological interventions for treatment-refractory depression. systematic review. The British Journal of Psychiatry, 181, 284–294.
Teasdale, J. D. (1993). Emotion and two kinds of meaning: cognitive therapy and applied cognitive science. Behaviour Research and Therapy, 31(4), 339–354.
Teasdale, J., & Barnard, P. (1993). Affect, cognition and change: re-modelling depressive thought essays in cognitive psychology (p. 285). Hillsdale: Lawrence Erlbaum Associates, Inc.
Teasdale, J. D., Segal, Z., & Williams, J. M. (1995). How does cognitive therapy prevent depressive relapse and why should Attentional Control (Mindfulness) Training help? Behaviour Research and Therapy, 33(1), 25–39.
Teasdale, J. D., Segal, Z. V., Williams, J. M., Ridgeway, V. A., Soulsby, J. M., & Lau, M. A. (2000). Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. Journal of Consulting and Clinical Psychology, 68(4), 615–623.
Acknowledgments
Dr. Eisendrath’s work was supported by grant R01AT004572–01A1 968 from the National Center for Complementary and Alternative Medicine of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Munshi, K., Eisendrath, S. & Delucchi, K. Preliminary Long-Term Follow-up of Mindfulness-Based Cognitive Therapy-Induced Remission of Depression. Mindfulness 4, 354–361 (2013). https://doi.org/10.1007/s12671-012-0135-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12671-012-0135-0