Abstract
The aim of this paper was to determine the utility of high density porous polyethylene implants (HDPE) in a variety of facial skeletal deformities. Sixteen patients (age range 14–28 years) with facial deformities requiring skeletal defect reconstruction or augmentation, treated between January 2008 and December 2010. The follow-up of the patients ranged from 6 months to 2 years.The types of deformities and defects treated include: one patient each with hemifacial microsomia and nasal tip correction, two patients each with malar deformities and orbital floor reconstruction, three patients with paranasal deformities and mandibular hypoplasia and four patients with chin augmentation. A total of 24 implants were placed. The complications included infection and wound dehiscence in one patient. The implants were palpable extraorally in two patients. It is concluded that HDPE is an excellent alternative to autogenous grafts for facial skeletal augmentation. Its porous nature, excellent soft tissue growth and coverage are the advantages and disadvantages include its rigidity and sometimes it is palpable extraorally.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
High density porous polyethylene (HDPE) is an inert material, which is a type of porous polymer. It is hard and non-compressible. Zygomatic bone, mandibular angle, body and symphysis region, cranium, orbital floor are the common sites for augmentation. It is easily carved to create the desired shape. It has pores measuring 100–300 μm in diameter leading to rapid in growth of the tissue into its pores [1].
HDPE is available as a sterile implant in blocks, preformed anatomical shapes, and on a custom basis. It is biocompatible and well tolerated by surrounding tissue [2]. The porous structure of the medpore allows fibrovascularization which prevents its migration as well as infection [3].
The aim of this study was to see the versatility of the porous high density polyethylene implants for correction of various facial deformities as an augmentation and as an only graft material and to see post-operative outcome in terms of aesthetics and associated complications.
Patients, Materials and Methods
The study sample was derived from the population of patients who reported to the Datarkar Institute of Maxillofacial Surgery, Pratap Nagar, Nagpur, India between January 2008 and December 2010. Informed consent was obtained from all patients who were enrolled in the study after they received an explanation of the advantages and disadvantages of HDPE. A total of 24 implants were implanted with HDPE implants in 16 patients, out of which seven were males and nine were females and their age ranged from 14 to 28 years. The sites were one patient each with hemifacial microsomia and nasal tip correction, two patients each of malar deformities and orbital floor reconstruction, three patients each with paranasal deformities and mandibular hypoplasia and four patients of chin augmentation. All patients were seen at an interval of 3 months, 6 months and yearly, with minimal follow-up of 6 months. Patients were examined post-operatively and observed for implant infection, exposure, extrusion, and stability.
Surgical Technique
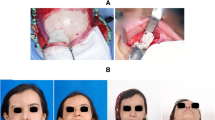
In this study we used the HDPE implants of Biopore. After complete history and clinical examination the treatment protocol for all the patients was decided. Patients were treated under general anesthesia. Extra oral approach was used in four patients, intraoral in nine patients and combined extra and intra oral approach in three patients. Adaptation of the HDPE was done whenever required by heating it in boiling saline and the carving with scalpel blade for desired thickness (Fig. 1). After cooling, medpore maintains the carved position. Primary fixation was achieved with the help of titanium screws or wires. Fixation of HDPE implants in 13 patients were carried out by using titanium screws, transosseous wiring used in one patient and in two patients implants were fixed to the recipient surface by tight suturing.
In 13 patients, 18 implants were fixed using titanium screw, one by using transosseous wiring. For the other two patients, a couple of implants has been done which is not very successful.
Case Presentation
Case 1
Patient presented with retruded chin (Fig. 2A). The defect was corrected using HDPE (Fig. 2B). The post-operative result is shown in (Fig. 2C).
Case 2
Patient presented with mandibular hypoplasia of left side of angle and body region (Fig. 3A). The defect was corrected using HDPE (Fig. 3B). The post-operative result is shown in (Fig. 3C).
Case 3
Patient presented with hemifacial microsomia (Fig. 4A). The deformity corrected by using HDPE (Fig. 4B). Figure 4C shows the post-operative result corrected facial deformity.
Case 4
Patient presented with cleft nasal deformity (Fig. 5A). HDPE implant was used for correction (Fig. 5B). Post-operative view showing corrected nasal deformity (Fig. 5C).
Case 5
The patient presented with orbital floor fracture (Fig. 6A). CT showed orbital floor fracture (Fig. 6B). Reconstruction was done using HDPE graft (Fig. 6C). Figure 6D shows the post-operative corrected deformity.
Results
All patients were kept under observation at an interval of 3, 6 months, and 1 year follow-up. The average follow-up in the study was a minimum of 6 months to 2 years. All patients were observed for improvement of facial esthetic, form and function by using Visual Analog Scale. All 16 patients showed significant improvement in facial esthetic. All implants were found to be fixed to the surrounding tissue at 3 months follow-up. Complications included infection and wound dehiscence in one patient, implant palpable extra orally in two patients. one implant was infected and removed after 4 weeks. The wound dehiscence was treated with resuturing after debridement under local anesthesia.
Discussion
The aim of this paper was to see the utility of HDPE (HDPE) implants in oral and maxillofacial surgery. The result suggests that HDPE is very useful in reconstructing the defects of maxillofacial region.
Since 1940, solid polyethylene has been used as a substitute for bone and cartilage [4]. In early 1970, HDPE was developed. It has high tensile strength, high biocompatibility, available in prefabricated shapes and has no reabsorption. According to Shanbag et al., HDPE has interconnecting network of pores which ranges from 160 to 368 μm and more than half of the pores are larger than 150 μm in diameter. This facilitates excellent tissue in growth [5]. Silicon can cause reabsorption of underlying bone while encapsulated and also can cause implant migration, which can be seen with almost all implants that do not promote tissue in growth [6].
Achieving the appropriate implant shape is a crucial step for a successful augmentation [7]. Although they are available in preformed shapes, the desired shape in the present study was achieved by soaking the HDPE in boiling saline and by carving with the help of scalpel blade. We recommend the soaking the HDPE in antibiotic solution before implantation, which is also supported by Frodel and Lee [8].
In our study, the maximum number of implants were augmented at chin (n = 4). Other authors in the literature also reported the chin as the most common site for facial implantation [5, 9]. Silicon chin implants were also used for chin augmentation but they cause underlying bone loss. The HDPE implant does not cause such reabsorption and also allows tissue growth [10].
Orbital wall defects have been reported to be repaired by various autogenous [11], alloplastic [12], allogenic [13] grafts and with the help of HDPE [14]. HDPE is well tolerated by orbital tissues and its porous structure is rapidly infiltrated by host tissue. In our study, we reconstructed the orbital floor defect in two patients and had no complications in the follow-up period. Rubin et al. [15], also reported low incidence rate of infection while using HDPE in orbital wall defect repair.
We placed HDPE in two cases in malar region; it is the ideal choice because of its tissue ingrowth nature. Silicone polymer can cause mobility and subsequently infection followed by rejection of the implant [16]. Nasal deformities were corrected in four patients using HDPE. It is reported that nasal dorsum has a higher complication rate than implants placed in areas which have more soft tissue coverage [17]. We did not find any complication in the follow-up period. Hypoplastic mandibles can be successfully augmented with the help of HDPE as proven by our study. We used screws and wires for fixation of HDPE, which is supported by other authors in the literature [18]. According to Frodel and Lee [8] in some cases, suture fixation is sufficient.
Conclusion
HDPE is an excellent alternative for facial contour repair. It allows tissue ingrowth into its pores which prevents its mobility. It is easy to shape and carve to the desired shape and size. The reabsorption rate of the graft is very rare as compared to autogenous bone graft. The donor site morbidity for harvesting the bone graft is avoided in this method of facial reconstruction. However, the graft may be extraorally palpable at some of the anatomical areas. The possibility of graft rejection is always there if it gets infected. The authors recommend the use of HDPE as a material of choice over autogenous bone graft for maxillofacial deformities and defects with due precautions and careful treatment planning. By chance if it fails, there is the option of autogenous bone graft, which is required in very few cases.
References
Yaremchuk MJ (2007) Facial skeletal augmentation with implants. In: Thome CH, Beasley RW, Aston SJ, Bartlett SP, Gurtner GC, Spear SL, (eds). Grabb and Smith’s plastic surgery. 5th edn. Philadelphia: Lippincott, pp 551–556
Sevin K et al (2000) Exposure of high-density porous polyethylene (Medpor®) used for contour restoration and treatment. Br J Oral Maxillofac Surg 38:144–149
Flood TR et al (1999) Randomized prospective study of the influence of steroids on postoperative eye opening after exploration of the orbital floor. Br J Oral Maxillofac Surg 37:510–511
Rubin LR (1983) Polyethylenes as a bone and cartilage substitute: a 32 year retrospective. In: Rubin LR (ed) Biomaterials in plastic surgery. CV Mosby, St Louis, pp 477–493
Shanbag A, Friedman HI, Augustine J, Von Recum AF (1990) Evaluation of porous polyethylene for external ear reconstruction. Ann Plast Surg 24:32–39
Wellisz T, Lawrence M, Jazayeri MA, Golshani S, Zhou ZY (1995) The effect of alloplastic implant onlays on bone in the rabbit mandible. Plast Reconstr Surg 96:957–963
Flowers RS (1991) Alloplastic augmentation of the anterior mandible. Clin Plast Surg 18:107
Frodel JL, Lee S (1998) The use of high-density polyethylene implants in facial deformities. Arch Otolaryngol Head Neck Surg 124:1219–1223
Bosse JP (1992) Clinical experience with the Medpor implant. Presented at the Canadian Society of Plastic Surgeons 46th Annual Meeting, London, Ontario, Canada, May 30
Lilla JA, Vistnes L, Jobe RP (1976) The long term effects of hard alloplastic implants when put on bone. Plast Reconstr Surg 59:14
Mathog RH (1983) Reconstruction of the orbit following trauma. Otolaryngol Clin North Am 16:585–607
Waite PD, Clanton JT (1988) Orbital floor reconstruction with lyophilized dura. J Oral Maxillofac Surg 46:727–730
Friesenecker J, Dammer R, Moritz M, Niederdellmann H (1995) Long-term results after primary restoration of the orbital floor. J Craniomaxillofac Surg 23:31–33
Shumrich KA, Kersten RC, Kulwin DR, Smith CP (1997) Criteria for selective management of the orbital rim and floor in zygomatic complex and midface fractures. Arch Otolaryngol Head Neck Surg 123:378–384
Rubin PAD, Bilyk JR, Shore JW (1994) Orbital reconstruction using porous polyethylene sheets. Ophthalmology 101:1697–1708
Friedman CD, Costantino PD (2002) Alloplastic materials for facial skeletal augmentation. Facial Plast Surg Clin N Am 10:325–333
Wellisz Tadeusz (1993) Clinical experience with the Medpor porous polyethylene implant. Aesth Plast Surg 17:339–344
Spector M, Flemming WR, Sauer BW (1995) Early tissue infiltrate in porous polyethylene implants into bone: a scanning electron microscope study. J Biomed Mater Res 9:537–545
Acknowledgments
Authors wish to thank Wendy Rash, RN, BSN, CEN for her support in grammatical corrections in the manuscript.
Conflict of Interests
None declared.
Ethical Approval
Taken.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rai, A., Datarkar, A., Arora, A. et al. Utility of High Density Porous Polyethylene Implants in Maxillofacial Surgery. J. Maxillofac. Oral Surg. 13, 42–46 (2014). https://doi.org/10.1007/s12663-012-0459-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12663-012-0459-2