Abstract
Background
Alloplastic materials in facial surgery have been used successfully for various applications in the reconstructive restoration or aesthetic augmentation of the facial skeleton. The objective of this study was to conduct a comprehensive systematic review of alloplastic implant materials utilized to augment the facial skeleton stratified by anatomical distribution, indication, specific material used, and respective outcomes.
Methods
A comprehensive systematic review on alloplastic facial implant data was conducted utilizing Medline/PubMed database. Articles were stratified by (1) anatomic localization in the face, as well as (2) alloplastic material.
Results
A total of 17 studies (n = 2100 patients, follow-up range = 1 month–27 years) were included. Overall, mersilene mesh implants were associated with the highest risk of infection (3.38%). Methyl methacrylate implants were associated with the highest rate of hematoma (5.98%). Implants placed in the malar region (2.67%) and frontal bones (2.50%) were associated with the highest rates of infection. Implants placed in the periorbital region were associated with the highest rate of inflammation (8.0%), explantation (8.0%), and poor cosmetic outcome (17.0%). Porous implants were shown to be more likely to potentiate infection than non-porous implant types.
Conclusions
Alloplastic facial implants are a reliable means of restoring facial symmetry and achieving facial skeletal augmentation with a relatively low complication profile. It is important for plastic surgeons to understand the relative risks for each type of implant to develop postoperative complications or poor long-term cosmetic results. Interestingly, porous implants were shown to be more likely to potentiate infection than non-porous implant types.
Level of Evidence III
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Facial implants are used in a variety of applications including post-traumatic reconstruction, correction of congenital abnormalities, and aesthetic augmentation or enhancement [1]. Commonly augmented facial sites include the nasal dorsum, malar eminence, and chin, in diverse applications that include rhinoplasty, orbital floor reconstruction, and augmentation of the facial skeleton [2]. While facial skeletal augmentation was traditionally achieved by utilizing autogenous bone grafts, advancements in materials engineering have allowed for the development of alloplastic materials better suited for certain surgical applications. These alloplastic facial implants offer a variety of advantages, including increased implant availability and the avoidance of donor-site morbidities seen with autogenous bone grafts such as scar alopecia and graft resorption [3]. The use of alloplastic facial implants may also offer the surgeon a number of advantages by avoiding difficulties in graft shaping that may result in increased surgical time and complexity [1].
Despite these advantages, alloplastic facial implants are not without their problems. Though a variety of implant material types exist, the ideal implant should possess a balance between structural integrity and pliability, and should be bioinert, to avoid inflammation [1, 2]. The absence of any one of these characteristics may result in complications which include postoperative infection or inflammation, graft explantation or migration, local hematoma or wound dehiscence, and ultimately poor cosmetic outcome. For example, implants made of porous materials such as porous high-density polyethylene (pHDPE) allow for the promotion of tissue ingrowth, but may also allow a site for bacteria to evade the host immune surveillance [2, 4]. Alternatively, uniformly solid implants that do not promote tissue growth may result in fibrotic encapsulation or migration of the implant [1]. For this reason, certain types of facial implants may be better suited based on procedure or anatomical site.
Though complications associated with alloplastic implants are well documented, studies have shown discrepancy regarding the rate of complications associated with certain implants [5,6,7,8]. A comprehensive analysis of facial implant complication rates and how they affect aesthetic outcome is essential. In this study, the authors conduct a systematic review and meta-analysis of pooled data of alloplastic implant materials utilized to augment the facial skeleton stratified by anatomical distribution, indication, specific material used, and respective outcomes.
Methods
Search Strategy
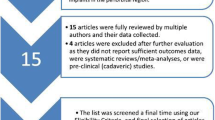
Two authors (first author and second author) independently conducted the electronic searches using Ovid Medline/PubMed database without timeframe limitations. Disagreements in regard to article identification and final selection for inclusion in this pooled analysis of the literature were resolved by the senior author. The following were used as either keywords or Medical Subject Headings (MeSH) in all combinations in the search strategy: [(alloplastic) AND face] and [(implant) AND (alloplastic) AND face]. The compiled reference lists were compared and reviewed for potential relevance. The bibliographies of included studies were also searched for articles not acquired through initial search queries. After all authors had completed systematic literature review, additional verification utilizing a medical librarian trained in systematic reviews was requested and received to ensure the most comprehensive review of all published studies meeting these criteria was performed. This study complied with the guidelines outlined in the Preferred Reporting Items for Systematic reviews and Meta-analyses (PRISMA). See Fig. 1 (flow chart).
Selection Criteria
Eligibility criteria included the following: clinical outcomes studies reporting data from alloplastic materials with anatomic localization in the face, including the zygoma, nose, mandible, orbit, frontal bone, maxilla, and glabella, for either reconstructive or aesthetic indications. Abstracts, presentations, non-English language papers, animal studies, non-clinical studies, ex vivo studies, reviews, meta-analyses, and single case reports were excluded.
Data Extraction and Processing
The extracted data included demographics, such as year of study, study design, country, follow-up duration, anatomical localization of alloplastic material, and surgical complications (including infection, inflammation, graft migration, need for explantation, hematoma, wound dehiscence, and cosmetic outcome). Data extraction from articles, tables, and figures was performed by one reviewer (second author) with accuracy of data entry confirmed by an additional reviewer (first author).
Analysis was designed to compare outcomes between (1) each alloplastic material studied and (2) different materials stratified by anatomical location in the face.
Results
A total of 2100 patients were featured in 17 case series [9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25] (follow-up range 1 month–27 years) (Table 1). The alloplastic implants analyzed were found to have an overall complication rate of 10.03% across all procedures and materials used. The most common overall complication was poor-reported aesthetic outcome with a pooled rate of 3.62%.
Overall, mersilene mesh implants were associated with the highest risk of infection (3.38%) followed by methyl methacrylate (2.43%) and silicone (1.58%). Methyl methacrylate implants were associated with the highest rate of hematoma (5.98%). Over half of all patients (21/41) requiring graft explantation received mersilene mesh implants; 12 received silicone implants. Migration was only reported in silicone and mersilene mesh implants. Only one patient with a silicone implant and two with Medpor implants were found to have postoperative wound dehiscence. Poor cosmetic outcomes had the highest rates respective to number of patients with Lactosorb, irradiated cartilage, and methyl methacrylate. The largest number of patients experiencing aesthetic complications was with methyl methacrylate (n = 28), followed by Medpor, mersilene mesh, and silicone (Table 2).
With regard to location, infection rates were highest in malar (2.67%), frontal (2.5%), and nasal (1.5%) implants in our analysis of pooled data from the literature. Inflammation was also reported in 13 (2.5%) patients with frontal implants. Orbital implants reported an 8% rate of inflammation and graft explantation. After orbital implant explantation, the next most common locations for explant were in nasal (2.38%) and mandibular (1.83%) implants. Migration was only noted as a complication in mandibular implants (1.08%), one of the less commonly reported complications overall. Implants placed in the frontal bone region reported a 6% (n = 32) likelihood of hematoma postoperatively. Wound dehiscence most often occurred with nasal implants (0.63%). The anatomic locations with the highest rates of poor aesthetic outcomes were orbital (17%), frontal (5.2%), and nasal (4.5%) (Table 3). Interestingly, porous implants were shown to be more likely to potentiate infection than non-porous implant types.
For completion, Supplemental Table 4 includes a listing of data collected from all case reports identified in the literature [26,27,28,29,30,31,32,33,34,35,36,37,38] as well as other case series that did not meet study inclusion criteria reporting outcomes in alloplastic facial implants, although we did not include these in our pooled data analysis.
See Figs. 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16 and 17 for illustrative examples of alloplastic facial implants commonly used in facial skeletal augmentation.
Discussion
Though autogenous bone transfer has long been utilized in a variety of applications involving facial reconstruction and aesthetic enhancement, limitations in tissue supply and associated morbidities such as graft resorption and scar alopecia have resulted in the development of a number of alloplastic implants [39]. As various types of alloplastic facial implants exist, factors that influence selection of alloplastic implant material include site and type of surgery, desired aesthetic outcome, and risk of complications. In this study, the authors performed a systematic review of alloplastic implant materials utilized in the face stratified by anatomical distribution, indication, specific material used, and respective outcomes.
To avoid excessive tissue inflammation, the ideal alloplastic implant should have excellent biocompatibility and should thus retain characteristics of the tissue it replaces or augments. The proper implant should therefore be non-allergenic, non-carcinogenic, and designed so that even in the setting of implant degradation, any associated breakdown products remain non-toxic [39]. However, even a well-tolerated alloplastic implant will function as a foreign body and thus evoke a response by the host. Soon after implantation, host proteins adhere to the surface of the implant, denature, and precipitate an inflammatory response characterized by local infiltration of inflammatory mediators and resultant collagen deposition on and around the implant [40]. Uncontrolled or persistent inflammatory response may result in further morbidity surrounding the implantation site. For example, silicone and methyl methacrylate implants have both been shown to cause significant bone resorption surrounding the site of implantation as well as thinning of the overlying skin [1, 41,42,43]. In one case series, 75% (n = 9/12) of silicone implants used for mandibular augmentation resulted in significant mandibular resorption [44]. This bone resorption is thought to be the result of a foreign body giant cell reaction that occurs between the implant and the bone, as well as, in the case of mandibular implants, pressure placed on the implant by the mentalis muscle. Due to the use of newer implants designed and placed to extend pressure over a greater anatomic surface area, significant bone resorption has become a less common complication though minimal self-limiting bone erosion continues to be a common result of the use of alloplastic implants [2]. Due to its significant inflammatory burden as well as other possible complications including extrusion, translucency and displacement, silicone is infrequently used for augmentation of facial areas other than the mandible, though solid silicone rubber, or Silastic, has been well documented in nasal augmentation procedures within Eastern societies [45,46,47]. In our review, silicone presented a minimal but not insubstantial inflammatory burden (0.33%; 1/443). Some reports state that methyl methacrylate has also been shown to cause significant bone resorption, though this is non-uniform with other reports crediting methyl methacrylate for its limited inflammatory potential [1, 39, 42, 48]. Methyl methacrylate was associated in this review with a relatively higher rate of inflammation (2.50%; n = 13/535). Lactosorb was also associated with a higher rate of inflammation (8%; n = 1/12), though this finding was limited to one study. More research is required to further elucidate the inflammatory potential of Lactosorb implants. Frontal implants were associated with an increased risk of inflammation (2.50%, n = 13/535) as well as poor overall cosmetic outcome (5.20%, n = 28/535). Inflammation and poor cosmetic outcome were also prevalent in orbital implants, though these findings were limited to one small case series.
Infection imposes a significant risk to early implant failure. Thus, the ideal implant should also maintain characteristics that limit invasion of the implant by microbial agents and maximize the host’s ability to combat infections that may arise [39]. Porous materials such as polytetrafluoroethylene, mesh-type materials, and hydroxyapatite are often used to design implants because they promote ingrowth of host tissue into the implant and may offer a decreased risk of implant migration [1, 4]. However, the presence of pores in the implant may also offer an increased risk of microbial invasion and resultant infection. Pore size is thought to be a determining factor for risk of infection. While a pore size of over 1 µm allows for the penetration of the pore by microbial substances, a pore size of over 50 µm is necessary for the penetration of the pore by host macrophages and other immune mediators. Thus, pore sizes between 1 and 50 µm may theoretically impose a more serious burden of infection as this would allow for invasion by bacterial mediators but not host immune cells [2, 39]. It is also thought that surface irregularity on the implant may confer additional energy that results in the increased adhesion of bacteria and other inflammatory mediators [2]. Disagreement exists whether porous implants potentiate infection over their solid counterparts [39, 49]. For example, reports have cited infection and inflammation as common complications associated with polytetrafluoroethylene implants, which feature microporous architecture composed of pores between 10 and 30 µm [45]. Conversely, it has also been reported that solid implants that do not promote tissue ingrowth, such as silicone, may increase risk of infection due to the formation of dead space between the graft and surrounding host tissues [50]. In our study, some, but not all, porous materials were associated with higher rates of infection. The alloplastic implant with the highest associated infection rate was mersilene resorbable mesh (3.40%, n = 18/533). Increased infection rate was also found in other porous materials such as methyl methacrylate (2.50%, n = 13/535), polytetrafluoroethylene (3%, n = 1/35), and Medpor (high-density polyethylene) (0.57%, n = 3/257). Though non-porous, silicone was associated with an infection rate of 1.67% (n = 7/443). In regard to location, the highest rate of infection was noted in patients receiving malar implants (2.67%, n = 3/123). The increased risk of complications associated with malar implants in comparison with other facial implants has been attributed to the observation that patients usually receive two malar implants, rather than the one implant obtained for, say, an isolated chin implant [2]. It has also been hypothesized that the thin wall of the anterior maxilla may provide a site of possible erosion of the implants, further increasing risk of infection [51].
Fixation of the implant is important for a number of reasons beyond maintaining aesthetic value. Continued movement of the implant within the tissue may cause continued tissue injury with resultant local inflammation and edema. Migration of the implant may also leave spaces between the implant and surrounding tissue that may serve as a space for hematoma, seroma, or microbial invasion and infection [2, 51]. The same porous characteristics thought to promote infection are also thought to promote fibrous ingrowth of host collagen into the implant, which lends to implant stability. Namely, the presence of pores greater than 50 µm in size allows for the migration of inflammatory mediators necessary for tissue ingrowth [39, 52]. If fibrous ingrowth does not occur, the implant can become encapsulated, which lends to easier migration of the implant within the tissue. Therefore, smooth non-porous implants such as silicone have been associated with higher rates of migration [42]. Other factors influencing migration within the tissue include implant shape and method of fixation [53]. In our review, migration was a relatively rare complication, but seen with both non-porous silicone (0.83%, n = 4/443) and porous mersilene resorbable mesh (0.75%, n = 4/533). Of note, migration was only seen as a complication in patients receiving mandibular implants (1.08%, n = 7/623), though reports reveal that migration may also be commonly associated with nasal implants [46]. Increased migration of mandibular implants may be a result of increased use of silicone materials within the area as well as increased influence of surrounding muscle on mandibular implants. More research may be required to elucidate the effects of porous architecture and on implant migration.
As with all systematic reviews, this study has several limitations. First, the cumulative outcomes analyzed were only as complete and accurate as each individual study included. Not all outcomes of interest were often available or mentioned despite large case volumes. Another limitation was the lack of large-volume studies across all implant types; thus, we felt that thorough statistical analyses could not be performed, as any conclusions drawn from such a deep statistical analysis would not be powered by the numbers reported. Additionally, while the primary objective of this particular study was to identify implant types which augment the bony skeletal features of the face, we recognize that there are other implants in the facial region (e.g., lip implants) which were not included in this analysis. Nevertheless, we feel that our study reports valuable pooled data, particularly pertaining to relative complication rates among material types and anatomic locations.
An important limitation of the reported results of this study is the relative quality and quantity of complications data published by our colleagues in all regions of the globe. For example, we are known that nasal implants are very often inserted for depressed middle vault defects in a diverse ethnic demographic; however, there are concerns that the accurate incidence of actual complications resulting from such implant placements may not be readily available in the primary literature for inclusion in this study. Thus, we must accept this as a weakness of our analysis based upon the paucity of literature available on complications.
It is a limitation of systematic review to adapt the language and categories that the included studies use. It is likely that more studies remain involving outcomes in alloplastic facial implants outside the scope of English language literature. Furthermore, there is a potential for bias in interpreting the data reported in each study, as it is possible that not all studies captured reliable comorbidity data or outcomes over a long period of time. Follow-up times are also a limitation of the study, as follow-up was limited to what the literature allows for follow-up measures. Also for this reason, we felt it prudent to avoid meta-analytic statistical measures to draw firm conclusions on the associations drawn from this study. Larger, randomized, multicenter studies are warranted to validate the associations found from this systematic review of the literature.
Conclusions
This study reaffirms that alloplastic facial implants are a reliable means of restoring facial symmetry and achieving facial skeletal augmentation with a relatively low complication profile across all implant types. The results of this systematic review indicated that some, but not all, porous materials were associated with higher rates of infection, a previously debated topic among surgeons. Furthermore, the results indicated migration to be a rarely reported complication of facial implant placement, equally reported in both porous and non-porous implant types. It is important for plastic surgeons to understand the relative risks for each type of implant to develop postoperative complications or poor long-term cosmetic results.
References
Frodel JL, Lee S (1998) The use of high-density polyethylene implants in facial deformities. Arch Otolaryngol Head Neck Surg 124(11):1219–1223
Cuzalina LA, Hlavacek MR (2009) Complications of facial implants. Oral Maxillofac Surg Clin N Am 21(1):91–104
Gear AJ, Lokeh A, Aldridge JH, Migliori MR, Benjamin CI, Schubert W (2002) Safety of titanium mesh for orbital reconstruction. Ann Plast Surg 48(1):1–9
Klawitter JJ, Bagwell JG, Weinstein AM, Sauer BW, Pruitt JR (1976) An evaluation of bone growth into porous high density polyethylene. J Biomed Mater Res 10(2):311–323
Winkler AA, Soler ZM, Leong PL, Murphy A, Wang TD, Cook TA (2012) Complications associated with alloplastic implants in rhinoplasty. Arch Facial Plast Surg 14(6):437–441
Wellisz T (1993) Clinical experience with the Medpor porous polyethylene implant. Aesthetic Plast Surg 17(4):339–3448273538
Türegün M, Sengezer M, Güler M (1998) Reconstruction of saddle nose deformities using porous polyethylene implant. Aesthetic Plast Surg 22(1):38–419456353
Romo T III, Sclafani AP, Sabini P (1998) Use of porous high-density polyethylene in revision rhinoplasty and in the platyrrhine nose. Aesthetic Plast Surg 22(3):211–2219618188
Ahn J, Honrado C, Horn C (2004) Combined silicone and cartilage implants: augmentation rhinoplasty in Asian patients. Arch Facial Plast Surg. 6(2):120–123
Bertossi D, Galzignato PF, Albanese M et al (2015) Chin microgenia: a clinical comparative study. Aesthet Plast Surg 39(5):651–658
Chang C, Kong WK (2014) Clinical effectiveness and safety of collagen sheet for dorsal augmentation in rhinoplasty. J Craniofac Surg 25(5):1852–1854
Demirkan F, Arslan E, Unal S, Aksoy A (2003) Irradiated homologous costal cartilage: versatile grafting material for rhinoplasty. Aesthetic Plast Surg 27(3):213–220
Erol OO, Enacar A (2003) Augmentation mentoplasty using a custom-design wire cage. J Craniofac Surg 14(6):884–892
Fanous N, Tournas A, Côté V et al (2017) Soft and firm alloplastic implants in rhinoplasty: why, when and how to use them: a review of 311 cases. Aesthetic Plast Surg 41(2):397–412
Gross EJ, Hamilton MM, Ackermann K, Perkins SW (1999) Mersilene mesh chin augmentation. A 14-year experience. Arch Facial Plast Surg. 1(3):183–189 (discussion 190)
Hollier LH, Rogers N, Berzin E, Stal S (2001) Resorbable mesh in the treatment of orbital floor fractures. J Craniofac Surg 12(3):242–246
Holmes AD, Lee SJ, Greensmith A, Heggie A, Meara JG (2010) Nasal reconstruction for maxillonasal dysplasia. J Craniofac Surg 21(2):543–551
Hopping SB, Joshi AS, Tanna N, Janjanin S (2010) Volumetric facelift: evaluation of rhytidectomy with alloplastic augmentation. Ann Otol Rhinol Laryngol 119(3):174–180
Lustica I, Velepic M, Cvjetković N et al (2001) Polymethyl-methacrylate implants in forehead and supraorbital arches reconstruction: retrospective study. Coll Antropol 25(Suppl):137–143
Niechajev I (2012) Facial reconstruction using porous high-density polyethylene (medpor): long-term results. Aesthetic Plast Surg 36(4):917–927
Nocini PF, Boccieri A, Bertossi D (2009) Gridplan midfacial analysis for alloplastic implants at the time of jaw surgery. Plast Reconstr Surg 123(2):670–679
Park DK, Song I, Lee JH, You YJ (2013) Forehead augmentation with a methyl methacrylate onlay implant using an injection-molding technique. Arch Plast Surg 40(5):597–602
Robiony M, Costa F, Demitri V, Politi M (1998) Simultaneous malaroplasty with porous polyethylene implants and orthognathic surgery for correction of malar deficiency. J Oral Maxillofac Surg. 56(6):734–741 (discussion 742)
Shadfar S, Farag A, Jarchow AM, Shockley WW (2015) Safety and efficacy of expanded polytetrafluoroethylene implants in the surgical management of traumatic nasal deformity. JAMA Otolaryngol Head Neck Surg 141(8):710–715
Yaremchuk MJ (2003) Improving aesthetic outcomes after alloplastic chin augmentation. Plast Reconstr Surg 112(5):1422–1432 (discussion 1433-4)
Alonso N, de Pochat VD, de Barros AR, Tavares LS (2013) Long-term complication after rhinoplasty using porous polyethylene implant: cutaneous fistula of the forehead. J Craniofac Surg 24(6):2176–2178
Bain CJ, Odili J (2012) Late infection of an alloplastic chin implant masquerading as squamous cell carcinoma. J Plast Reconstr Aesthet Surg 65(6):e151–e152
Emsen IM, Benlier E (2008) A new approach on reconstruction of frontonasal encephalomeningocele assisted with medpor. J Craniofac Surg 19(2):537–539
Eufinger H, Wehmöller M, Scholz M, Harders A, Machtens E (1999) Reconstruction of an extreme frontal and frontobasal defect by microvascular tissue transfer and a prefabricated titanium implant. Plast Reconstr Surg 104(1):198–203
Graham BS, Thiringer JK, Barrett TL (2001) Nasal tip ulceration from infection and extrusion of a nasal alloplastic implant. J Am Acad Dermatol 44(2 Suppl):362–364
Greene AK, Warren SM, McCarthy JG (2008) Onlay frontal cranioplasty using wire reinforced methyl methacrylate. J Craniomaxillofac Surg 36(3):138–142
Hoffmann C, Schuller-Petrovic S, Soyer HP, Kerl H (1999) Adverse reactions after cosmetic lip augmentation with permanent biologically inert implant materials. J Am Acad Dermatol 40(1):100–102
Pak MW, Chan ES, van Hasselt CA (1998) Late complications of nasal augmentation using silicone implants. J Laryngol Otol 112(11):1074–1077
Saray A (2003) Porcine dermal collagen (Permacol) for facial contour augmentation: preliminary report. Aesthetic Plast Surg. 27(5):368–375
Scolozzi P (2012) Maxillofacial reconstruction using polyetheretherketone patient-specific implants by “mirroring” computational planning. Aesthet Plast Surg 36(3):660–665
Stalder MW, St Hilaire H (2012) Immediate osseous genioplasty with Kirschner wire fixation for revision of infected alloplastic chin implant. J Craniofac Surg 23(5):e446–e447
Tieghi R, Consorti G, Clauser LC (2012) Contouring of the forehead irregularities (washboard effect) with bone biomaterial. J Craniofac Surg 23(3):932–934
Raghavan U, Jones NS, Romo T 3rd (2004) Immediate autogenous cartilage grafts in rhinoplasty after alloplastic implant rejection. Arch Facial Plast Surg 6(3):192–196
Quatela VC, Chow J (2008) Synthetic facial implants. Fac Plast Surg Clin N Am 16(1):1–10
Sclafani AP, Romo T III (2000) Biology and chemistry of facial implants. Facial Plast Surg 16(01):003–006
Dale EL, Sargent LA (2015) Bilateral erosion of malar implants into the maxillary sinuses. Plast Surg Case Stud 1(2):32–34
Wellisz T, Lawrence M, Jazayeri MA, Golshani S, Zhou ZY (1995) The effects of alloplastic implant onlays on bone in the rabbit mandible. Plast Reconstr Surg 96(4):957–963
Ren W, Wu B, Mayton L, Wooley PH (2002) Polyethylene and methyl methacrylate particle-stimulated inflammatory tissue and macrophages up-regulate bone resorption in a murine neonatal calvaria in vitro organ system. J Orthop Res 20(5):1031–1037
Peled IJ, Wexler MR, Ticher S, Lax EE (1986) Mandibular resorption from silicone chin implants in children. J Oral Maxillofac Surg 44(5):346–348
Peled ZM, Warren AG, Johnston P, Yaremchuk MJ (2008) The use of alloplastic materials in rhinoplasty surgery: a meta-analysis. Plast Reconstr Surg 121(3):85e–92e
Deva AK, Merten S, Chang L (1998) Silicone in nasal augmentation rhinoplasty: a decade of clinical experience. Plast Reconstr Surg 102:1230–1237
Graham BS, Thiringer JK, Barrett TL (2001) Nasal tip ulceration from infection and extrusion of a nasal alloplastic implant. J Am Acad Dermatol 44(2):362–364
Park DK, Song I, Lee JH, You YJ (2013) Forehead augmentation with a methyl methacrylate onlay implant using an injection-molding technique. Arch Plast Surg 40(5):597
Kiechel SF, Rodeheaver GT, Klawitter JJ, Edgerton MT, Edlich RF (1977) The role of implant porosity on the development of infection. Surg Gynecol Obstet 144(1):58–62
Lohuis PJFM, Watts SJ, Vuyk HD (2001) Augmentation of the nasal dorsum using Gore-Tex®: intermediate results of a retrospective analysis of experience in 66 patients. Clin Otolaryngol Allied Sci 26(3):214–217
Adams JR, Kawamoto HK (1995) Late infection following aesthetic malar augmentation with proplast implants. Plast Reconstr Surg 95(2):382–384
Staffel G, Shockley W (1995) Nasal implants. Otolaryngol Clin North Am 28(2):295–308
Rubin JP, Yaremchuk MJ (1997) Complications and toxicities of implantable biomaterials used in facial reconstructive and aesthetic surgery: a comprehensive review of the literature. Plast Reconstr Surg 100(5):1336–1353
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Human and Animal Rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed Consent
For this type of study, informed consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This study was supported in part by the Mayo Clinic Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Oliver, J.D., Eells, A.C., Saba, E.S. et al. Alloplastic Facial Implants: A Systematic Review and Meta-Analysis on Outcomes and Uses in Aesthetic and Reconstructive Plastic Surgery. Aesth Plast Surg 43, 625–636 (2019). https://doi.org/10.1007/s00266-019-01370-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-019-01370-0