Abstract
A number of experimental studies have reported that exposure to common, clinically used anesthetics induce extensive neuroapoptosis and cognitive impairment when applied to young rodents, up to 2 weeks old, in phase of rapid synaptogenesis. Propofol is the most used general anesthetic in clinical practice whose mechanisms of neurotoxicity on the developing brain remains to be examined in depth. This study investigated effects of different exposures to propofol anesthesia on Fas receptor and Fas ligand expressions, which mediate proapoptotic and proinflammation signaling in the brain. Propofol (20 mg/kg) was administered to 7-day-old rats in multiple doses sufficient to maintain 2-, 4- and 6-h duration of anesthesia. Animals were sacrificed at 0, 4, 16 and 24 h after termination of anesthesia. It was found that propofol anesthesia induced Fas/FasL and downstream caspase-8 expression more prominently in the thalamus than in the cortex. Opposite, Bcl-2 and caspase-9, markers of intrinsic pathway activation, were shown to be more influenced by propofol treatment in the cortex. Further, we have established upregulation of caspase-1 and IL-1β cytokine transcription as well as subsequent activation of microglia that is potentially associated with brain inflammation. Behavioral analyses revealed that P35 and P60 animals, neonatally exposed to propofol, had significantly higher motor activity during three consecutive days of testing in the open field, though formation of the intersession habituation was not prevented. This data, together with our previous results, contributes to elucidation of complex mechanisms of propofol toxicity in developing brain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A number of experimental studies have reported that exposure to common, clinically used anesthetics induce extensive cell death in the brain of young animals when applied during the phase of rapid synaptogenesis, during the first few weeks of life in rodents (Dobbing and Sands 1979; Jevtovic-Todorovic et al. 2003; Loepke and Soriano 2008; Jevtovic-Todorovic 2010). Recent retrospective clinical studies have revealed that children who received multiple anesthesia before the age of 4 had an increased risk of developing memory and learning disabilities later on in the life, which is in agreement with experimental animal studies (Wilder et al. 2009; Vutskits et al. 2012). Considering that annually just in the USA six million children under the age of 15 undergo anesthesia, this data indicates the ultimate need to elucidate mechanisms of anesthetics toxicity in developing brains (Servick 2014).
Propofol is an intravenous general anesthetic commonly used for the induction and maintenance of anesthesia in pediatric surgery. It is a powerful modulator of neuronal activity by potentiating inhibitory signaling through GABAA receptors and inhibiting excitatory signaling via NMDA receptors (Loepke and Soriano 2008; Alkire et al. 2008). The apoptotic cell death, one of the main anesthesia-induced neurotoxic effects observed in experimental studies, has been well documented on histopathological level for almost all common general anesthetics, including propofol (Ikonomidou et al. 1999; Jevtovic-Todorovic et al. 2003; Pesic et al. 2009; Bercker et al. 2009; Milanovic et al. 2010). Repeated exposure to propofol induces exposure-time-dependent neuronal cell loss and long-term neurocognitive deficits in neonatal rats (Yu et al. 2013). However, molecular mechanisms of propofol-induced apoptotic cell death are still not completely resolved. We and others have identified an activation of extrinsic apoptotic pathway triggered by increased TNFα expression and deprivation of neurotrophic factors accompanied by p75 receptor upregulation as possible mechanisms of propofol neurotoxicity (Pesic et al. 2009; Milanovic et al. 2010; Popic et al. 2012; Pearn et al. 2012; Milanovic et al. 2014; Popic et al. 2015). However, the potential role of other members of extrinsic apoptotic pathway, like Fas ligand and Fas death receptor cascade, as well as role of intrinsic apoptotic signaling represented by Bcl-2 family gene expression in propofol-mediated cell death has been neglected. In the light of the recent observation, it is of great importance that some anesthetic agents have less toxic effects on developing brain (Vutskits et al. 2012). Therefore, consequences of anesthesia administration are not only dependent on developmental stage, dose, concentration, and duration of anesthesia, but it is also agent specific (Fredriksson et al. 2007; Loepke and Soriano 2008; Vutskits et al. 2012). As the propofol is currently one of the most widely used anesthetics in clinical practice, and its administration is often followed by subsequent application of other, mostly volatile anesthetics, it is of essential importance to systematically assess the time- and dose-dependent effects of propofol on proapoptotic signaling in vivo.
Considering all this, the present study was undertaken to determine whether propofol exposures lasting 2-, 4- and 6-h could change the time profile of FasL and Fas receptors, the prototypic inducers of extrinsic cell death and downstream caspase-8 expression. Since the mitochondrial apoptotic pathway can be triggered intrinsically or with extrinsic pathway signals converging, we also examined the expression levels of Bcl-2 family members and caspase-9 after propofol anesthesia. As Fas/FasL system has been known to act as a mediator of inflammation in CNS pathology (Choi and Benveniste 2004) and as most recent studies point to the importance of inflammation in anesthetic toxicity, caspase-1, interleukine-1β (IL-1β) and activation of microglia (Cao et al. 2012; Tanaka et al. 2013; Ye et al. 2013; Shen et al. 2013), the focus of our study aims to determine if propofol anesthesia could interconnect pro-apoptotic and pro-inflammatory signaling in the developing brain. We also studied the cognitive processes that include attention and motor activity later in life (P35, P60) to assess long-term consequences of the propofol treatment. Importantly, novel findings accentuate the association between early exposure to general anesthesia and attention-deficit/hyperactivity disorder (Sprung et al. 2012).
Materials and Methods
Ethic Statement
All experimental procedures were in compliance with the EEC Directive (86/609/EEC) on the protection of animals used for experimental and other scientific purposes, and were approved by the Ethical Committee for the Use of Laboratory Animals of the Institute for Biological Research, University of Belgrade, and by the University of Virginia Animal Care and Use Committee, and were in accordance with the Guide for the Care and Use of LaboratoryAnimals (NIH).
Animals and Treatment
Seven-day-old (P7) male Wistar rats (average body weight 12–14 g) were used in all experiments. The procedures were designed to minimize the suffering of the animals and the number of rats used. Rat pups were separated from their mothers and placed in a temperature-controlled incubator set to an ambient temperature of 35–36 °C during anesthesia and first hour of recovery periods, after which they were returned to dam to feed. The treatment was performed by administration of propofol manufactured for intravenous human use (Recofol®; Schering Oy, Turku, Finland). Loss of the righting reflex served as an indicator of anesthetic-induced unconsciousness and sleeping time. A dose of 20 mg/kg that impaired the righting reflex for 43 ± 5 min was used.
Experimental Procedures
To prevent possible litter effects, a single pup from a litter was assigned to every single group of experimental rats mentioned at the appropriate points in this article. P7 rat pups (n = 92) were administered either 2, 4, or 6 bolus injections of 20 mg/kg of propofol intraperitoneally at 1 h intervals in order to achieve either 2-, 4-, or 6-h-long anesthesia (Milanovic et al. 2010). The animals were decapitated either immediately after cessation of the exposure times (designated as the 0 h time point), or after the recovery periods that lasted 4, 16 or 24 h following termination of propofol exposure (and are referred to as 4, 16, and 24 h time points, respectively). Control animals, separated from their mothers and received 2, 4, or 6 injections of physiological saline at the same intervals as propofol-treated littermates, were sacrificed at 0 h time point. The cortex and the thalamus from both hemispheres were isolated and frozen for subsequent use for RNA and protein analysis (n = 4 per group). Whole brains were isolated (n = 3 per group) for use in histological studies.
RNA Isolation, Reverse Transcription, and Semiquantitative PCR
Total RNA was isolated from the cortex and thalamus with TriZol (Invitrogen) reagent according to the manufacturer’s instructions. RNA concentrations were estimated by UV spectrophotometry, and RNA integrity was assessed by electrophoresis in a 1 % agarose gel.
Reverse transcription (RT) reactions were performed with 5 μg total RNA using oligo-(dT) primers and M-MLV Reverse Transcriptase according to the manufacturer’s instructions. One hundred ng of cDNA were used for each reaction. Primer sequences and PCR conditions are shown in Table 1. PCR reactions were performed in the GeneAmp1 PCR System 9700 (Applied Biosystems). All PCR reactions were performed from two independent RT reactions, with at least two repeats for each reaction. The PCR products were separated in 2 % agarose gels, stained with ethidium bromide, and photographed under UV light. Multi-Analyst/PC Software Image Analysis System (Bio-Rad Gel Doc 1000) was used for densitometry analysis.
Quantitative Real-Time Reverse Transcriptase Polymerase Chain Reaction (qRT-PCR)
The RT reactions were performed in 20 μl using a High-Capacity cDNA Archive Kit according to the manufacturer’s instructions. The reactions were carried out under RNase-free conditions at 25 °C for 10 min, and at 37 °C for 2 h. The cDNA was stored at −20 °C until further use. Relative quantification of caspase-8 was performed by real-time qPCR using the appropriate TaqMan assays(ID Rn00574069_m1, Applied Biosystems). GAPDH was included in every analysis as an endogenous control to correct for differences in inters assay amplification efficiency (ID Rn99999916_s1). Each sample was run in triplicate, and the mean values of each Ct were used for further calculations. Quantification was performed by the 2−∆∆Ct method (Livak and Schmittgen, 2001). The results obtained by qPCR were analyzed by RQ Study Add ON software for the 7000 v 1.1 SDS instrument (ABI Prism Sequence Detection System), with a confidence level of 95 % (p < 0.05).
Tissue Extracts and Western Blot Analysis
To obtain whole-cell extracts, the tissue was homogenized with a Dounce homogenizer in 10 vol (w/v) of lysis buffer (50 m M Tris–Cl pH 7.5, 150 mM NaCl, 1 % NP-40, 0.1 % SDS, 1 m M EDTA pH 8.0, 1 m M EGTA pH 7.2, 0.5 % Triton X-100) that contained a complete cocktail of phosphatase and protease inhibitors (Roche, Mannheim, Germany). The homogenates were sonicated and centrifuged at 16,000g at 4 °C for 30 min. The supernatants were collected and stored at −70 °C until use. Protein concentrations were determined by the bicinchonic acid micro-protein assay (Micro BCA Protein Assay Kit; Pierce Inc., Rockford, IL, USA) with albumin as standard.
Proteins (20–40 μg per lane) were separated by 10 % SDS polyacrylamide gel electrophoresis and transferred to nitrocellulose membranes (Amersham Bioscience, Otelfingen, Switzerland).The membranes were blocked at room temperature for 1 h in 3 % bovine serum albumin in Tris-buffered saline/0.1 % Tween 20 (TBS-T), followed by incubation for 2 h or overnight with primary antibodies. The immunoblots were processed with horseradish peroxidase-conjugated anti-rabbit (sc-2350, Santa Cruz) or anti-mouse antibodies (PO160, Dako) in TBS-T for 1 h at room temperature. Three washes with 0.3 % Tween-20 in Tris-buffered saline were performed between all steps. All blots were incubated with anti-β-actin or anti-GAPDH antibodies to correct for any differences in protein loading. Immunoreactivity was detected by enhanced chemiluminescence (ECL; Amersham Bioscience) after exposure on X-ray film. All films were densitometrically analyzed using the computerized image analysis program ImageQuant 5.0. The following antibodies were used: FasL (sc-6237), Fas (sc-716), Bcl-2 (sc-73820, caspase-8 (sc-7890), caspase-9 (sc-17784), GAPDH (sc-20357) all from Santa Cruz; Iba- 1 (019-19741) from Wako and β-actin (#A5316) from Sigma.
Histological Analysis and Immunofluorescence
After decapitation, brains were quickly removed and fixed in 4 % paraformaldehyde for 12 h. For cryoprotection, tissue was transferred into graded sucrose. Brains were frozen in 2-methyl butane and kept at −80 °C until sectioning on a cryotome. The brains were cut in coronal sections of 18-μm thickness and mounted on Superfrost® glass slides, dried for 12 h at room temperature, and stored at −20 °C until staining.
Normal goat serum (Sigma–Aldrich, Germany) was used for blocking of nonspecific labeling as 10 % solution in PBS. In order to estimate the activation state of glial cells, sections were incubated with primary antibodies for microglial marker: rabbit anti-Iba-1 (ionized calcium-binding adaptor molecule 1) antibody (WAKO, Japan) in 0.01 M PBS overnight at 4 °C. Following three washes in 0.01 M PBS, immune complexes were visualized with goat anti-rabbit IgG Alexa Fluor 488 (1:500; Invitrogen, Carlsbad, CA, USA), 2 h at room temperature. For the negative control, sections were incubated with appropriate secondary antibodies without the primary antibody. The sections were mounted in DAPI-mounting medium (VECTOR laboratories, USA) and examined under a Carl Zeiss Axiovert fluorescence microscope (Zeiss, Gottingen, Germany). All images were acquired with the 10× and 40× objectives.
Behavioral Tests
Regarding our previous findings about propofol anesthesia duration- and structure-dependent neurodegeneration (Milanovic et al. 2010), we opted to test long-term behavioral consequences of 6 h-long propofol exposure. Behavioral experiments were performed between 09:00 and 14:00 h. Animals neonatally exposed to propofol anesthesia (n = 6 per group) and control, saline injected animals (n = 6 per group) were habituated to experimental cages for three consecutive days (intersession activity) starting from age P35 (early adolescence in rats, Laviola et al. 2003). During each day, activity was detected for 30 min after the exposure of the animals to the open field cages (intrasession activity). After these tests at P35, the animals were tested again at P60.
Measurement of Motor Activity
The motor activity of rats was recorded individually for each animal in Opto-Varimex cages (Columbus Instruments, OH) that were linked online to an IBM-PC compatible computer. The open fields were placed in a light- and sound-attenuated room provided with indirect and homogenous illumination (150 lx in the centre of the open field arena). Each cage (44.2 × 43.2 × 20 cm) was equipped with 15 infrared emitters that were located on the x and y axes. An equivalent number of receivers were located on the opposite walls of the cage. Data were analyzed using Auto-Track software (Columbus Instruments). The Auto-Track interface collects data from the Opto-Varimex unit every 1/10th of a second and categorizes the activity. Locomotor activity was defined as a trespass of three consecutive photo-beams. Vertical activity was measured by recording the number of beams that were broken by rearing of the animal.
Statistical Analysis
Semi-quantitative evaluation of protein levels detected by Western immunoblotting was performed by densitometric scanning using the computerized image analysis program ImageQuant 5.0. The data are presented as percentages (mean ± SEM) relative to the control samples assumed to be 100 % (depicted by a black line on the graphs). Differences between the experimental groups were tested using Kruskal–Wallis nonparametric ANOVA with Mann–Whitney’s post-hoc U test (Statistica version 5.0; StatSoft, Tulsa, OK, USA). Significance was reported at p < 0.05.
The behavioral data obtained for the habituation sessions were presented as scores for 5-min periods within 30-min registration time (to view time-dependent changes in motor activity during intrasession habituation; mean), the summary for the first 5 min (as the period of most intensive exploratory activity; mean ± SEM) and the summary for the whole 30-min registration period (to assess total activities for defined period during three consecutive days of testing—intersession habituation; mean ± SEM). The data were analyzed by two-way analysis of variance (ANOVA) with propofol pretreatment and time (repeated measure) as factors. Subsequent comparisons were made using the Fisher LSD test.
Results
Propofol Induces Activation of FasL/Fas Death Receptor Proteins in P7 Rats
Seven-day-old rat pups, kept 2-, 4-, or 6-h under propofol-induced anesthesia, were sacrificed 0, 4, 16, and 24 h later. The first aim of the study was to examine the levels of protein expressions of Fas receptor and its ligand FasL in the cortex and thalamus by Western blot analysis.
In the cortex, there was a significant decrease of FasL protein level (by 35–40 % of control) immediately after termination of all anesthesia regimens, that were restored to control level 24 h later (Fig. 1a). In the thalamus, there was an early increase of FasL level (at 4 h time point, A + 4) following 2-h propofol anesthesia. Longer durations of anesthesia (4 and 6 h) induced elevation of FasL at later time points (up to 40 % at 16–24 h period, p < 0.05; Fig. 1b).
Time courses of Fas ligand and Fas receptor protein expressions after propofol exposures. The levels of FasL/Fas receptor protein expression were assessed by Western blot analysis of total protein extracts obtained from the cortex (a, c) and the thalamus (b, d) of P7 rats. The results are presented for animals at different recovery time points (0, 4, 16, and 24 h) after exposures to propofol anesthesia for 2-, 4-, and 6-h. A representative Western blots is shown with single protein bands corresponding to FasL/Fas receptor and β-actin, which served as an internal control of the protein load. Histograms represent protein levels expressed as a percentage relative to the control value obtained from five separate experiments. The results are mean ± SEM. *p < 0.05 vs. the control value, presented as a black line; # p < 0.05 between treatments
The expression profile of Fas receptor revealed stronger changes. In the cortex, alterations in Fas protein levels were time and anesthesia duration dependent, as seen inthe decreased Fas expression levels (around 50 % of control) after 2- and 4-h anesthesia dutarion at early time points, and increase detected after 6-h anesthesia at 0-and 24-hr time points (Fig. 1c). In the thalamus, expression levels of Fas receptor increased gradually, reaching peak at 24-h time point after termination of all three exposures to propofol (40–90 % increase above control level, p < 0.05; Fig. 1d).
Propofol Induced Caspase-8 mRNA and Proteins Expression
Caspase-8 is a downstream protein in FasL/Fas signaling cascade. The effect of propofol anesthesia on the caspase-8 mRNA and protein expression were investigated by qRT-PCR and Western blotting in the cortex and thalamus of P7 rats (Fig. 2).
Time courses of caspase-8 mRNA and protein expressions after propofol exposures. Caspase-8 mRNA expressions in the cortex (a) and the thalamus (b) of P7 rats after propofol anesthesia were examined by means of quantitative real-time qRT-PCR. The results are presented for animals at different recovery time points (0, 4, 16, and 24 h) after exposure to propofol anesthesia for 2, 4, and 6 h. Histograms represent mRNA levels expressed as the fold changes relative to the control value obtained from five separate experiments. The levels of caspase-8 protein expressions were determined by Western blot analysis of total protein extracts obtained from the cortex (c) and the thalamus (d). A representative Western blot is shown with a duplet protein bands (43/41 kDa fragment) corresponding to caspase-8 and β-actin, which served as internal controls of the protein load. Histograms represent protein levels expressed as a percentage relative to the control value obtained from five separate experiments. The results are mean ± SEM. *p < 0.05 vs. the control value, presented as a black line; # p < 0.05 between treatments
Quantification of the mRNA levels revealed significant changes of caspase-8 gene expressions in both structures examined (Fig. 2a, b). In the cortex, the most prominent changes were seen after 6-h anesthesia (Fig. 1a); time profile showed a biphasic pattern of alterations having peaks (60–80 % above control level) at 4 and 24 h after propofol exposure. In the thalamus, changes in caspase-8 mRNA levels were more vigorous and persistent after all three anesthesia regimens (Fig. 2b). Significant increases (up to 100 % above control level) were detected within 4–24 h time period after 2- and 4-h treatments, while 6-h treatment induced immediate elevation of caspase-8 mRNA (around 140 % above control) that lasted till the end of time period observed (Fig. 2b).
Effects of propofol anesthesia were analyzed at the levels of protein fragments p43/p41 that were generated after autocatalytic cleavage of procaspase-8 (p55/p53). Western blot analysis revealed structure-dependent expression of caspase-8 p43/p41 protein fragments (Fig. 2c, d). Thus, changes in the cortex were slight, and statistical significance was achieved only immediately after 2-h exposure, when decrease by 45 % of control was measured (p < 0.05; Fig. 2c). In the thalamus, both 4- and 6-h exposures to propofol led to significant upregulation of caspase-8 protein within 4–24 h time-frame (up to 52 % above control, p < 0.05; Fig. 2d). There were no significant changes in the levels of caspase-8 full-length (p-55/53) protein in either of structures (data not shown).
Effect of Propofol Treatment on Bcl-2 mRNA and Protein Expression
FasL/Fas-triggered extrinsic apoptotic signaling can be accompanied by activation of intrinsic apoptotic cascade in a caspase-8-dependent or -independent manner. Therefore, we sought to determine the effect of repeated injections of propofol on the levels of anti-apoptotic Bcl-2 mRNA and protein, the key member of intrinsic apoptotic pathway (Fig. 3).
Time-dependent changes in of Bcl-2 mRNA and protein expression. Bcl-2 mRNA expressions in the cortex (a) and the thalamus (b) of P7 rats after propofol anesthesia were examined by means of semiquantitative RT-PCR. The results are presented for animals at different recovery time points (0, 4, 16, and 24 h) after exposures to propofol anesthesia for 2, 4, and 6 h. Histograms represent mRNA levels expressed as the fold changes relative to the control value obtained from three separate experiments. The levels of Bcl-2 protein expressions were determined by Western blot analysis of total protein extracts obtained from the cortex (c) and the thalamus (d). A representative Western blot is shown with a single protein bands corresponding to Bcl-2 and β-actin, which served as internal controls of the protein load. Histograms represent protein levels expressed as a percentage relative to the control value obtained from five separate experiments (100 %). The results are mean ± SEM. *p < 0.05 vs. the control value, presented as a black line; # p < 0.05 between treatments
Propofol anesthesia influenced transcription of Bcl-2 gene in both examined structure (Fig. 3a, b). In the cortex, there was a significant downregulation of Bcl-2 gene expression (by 35–60 %) throughout 24-h time frame after all three exposures. Transient returning to basal level was detected only 16 h after shorter, 2- and 4-h treatments. In the thalamus, however, 2-h-long anesthesia did not affect Bcl-2 transcription until 24-h post-anesthetic point (decrease by 32 %, p < 0.05; Fig. 3b). Four- and six hours treatments produced decrease of Bcl-2 mRNA by 30–40 % in an anesthesia-duration- and time-dependent manner.
Western blot analysis revealed that Bcl-2 protein expression in the cortex had more pronounced changes than in the thalamus (Fig. 3c, d). A marked decrease (up to 50 % below the control, p < 0.05 l) in Bcl-2 abundance was detected immediately after termination of all three exposures in the cortex. That was followed by returning to control level at later times, except for 4-h exposure that remained decreased (by 40 % of control values, p < 0.05; Fig. 3d).
To extend the study, the expression levels of three additional, well-known markers of intrinsic pathway activation, Bcl-xl, Bad, and Bax, were analyzed at transcriptional level Supplementary Fig. 1). Anti-apoptotic Bcl-xL gene was slightly but significantly downregulated in the cortex 24 h following 2-h anesthesia and within 4 h after 6-h propofol anesthesia (Supplementary Fig. 1A). In the thalamus, the decline in Bcl-xL mRNA was detected immediately following termination of 6-h exposure (70 % of control level, p < 0.05) and 24 h after 2-h exposure (22 %, p < 0.05). As for the expression of pro-apoptotic genes, Bax and Bad PCR analysis revealed no significant changes of any of these, neither in cortex nor in thalamus following the all three anesthesia regimens (Supplementary Fig. 1C–F).
Propofol Induces Activation of Caspases-9 Protein Expression
Caspase-9 is apical caspase in mitochondrial (intrinsic) pathway of apoptosis. Western blot analysis revealed structure-specific pattern of caspase-9 expression seen as a decline in cortex and elevation in the thalamus. In the cortex, there was robust decrease in caspase-9 levels (to ~40 % of control value, p < 0.05) immediately after all three exposures to propofol (Fig. 4). Caspase-9 expressions recovered partially within 4–16 h following 2- and 4-h exposures, while significant and persistent decrease was detected at all time-points after 6-h exposure (Fig. 4a).
Time courses of caspase-9 protein expression levels in the cortex and the thalamus of P7 rats. Caspase-9 protein expressions in the cortex (a) and the thalamus (b) of P7 rats after 2-, 4-, and 6-h exposures to propofol. The results are presented for animals at different recovery time points (0, 4, 16, and 24 h) after exposures to propofol anesthesia. The levels of caspase-9 protein expression were assessed by Western blot analysis of total protein extracts obtained from the cortex and the thalamus. A representative Western blot is shown with a single protein bands corresponding to caspase-9 and β-actin, which served as internal controls of the protein load. Histograms represent protein levels expressed as a percentage relative to the control value obtained from five separate experiments. The results are mean ± SEM. *p < 0.05 vs. the control value, presented as a black line; # p < 0.05 between treatments
In the thalamus, no significant changes in caspase-9 were observed until later time points (Fig. 4b). Namely, at 16–24-h time period, 4- and 6-h exposures induced increase in the level of caspase-9 (~50 % above control. p < 0.05), while 2-h exposure had no effect (Fig. 4b).
Propofol Induced Caspase-1, Interleukin–1β mRNAs, and Activation of Microglial Cells
Caspase-1 is the best described inflammatory caspase involved in the processing of pro-IL-1β, a key inflammatory cytokine implicated to injury, disease, and infection (Denes et al. 2012). Therefore, we examined regional expression and temporal profiles of caspase-1 and IL-1β mRNA in response to propofol anesthesia.
Propofol treatment caused significant changes of caspase-1 mRNA expression in cortex and thalamus, as shown by using a semiquantitative RT-PCR (Fig. 5). In the cortex, the 2- and 4-h treatments led to a gradual increase of mRNA expression of the caspase-1, and the highest level has been detected in the A + 24 time points (57 % above the control, p < 0.05) (Fig. 5a). A 6-h treatment caused a more than double increase in caspase-1 gene expression immediately after termination of exposure that was followed by almost threefold increase at 16–24 h time period (Fig. 5a). In the thalamus, there was a pattern of caspase-1 gene expression similar to the one in the cortex, with highest levels (2–3.5-fold above control level) obtained at 16–24 hr time frame in a duration of anesthesia-dependent manner (Fig. 5b).
Time-dependent changes of the caspase-1 and IL-1β mRNA expressions of P7 rats after exposure to propofol anesthesia. Caspasa-1 mRNA expression levels in the cortex (a) and the thalamus (b) and IL-1β mRNA expression levels in the cortex (c) and thalamus (d) were examined by using semiquantitative RT-PCR The results are presented for animals at different recovery time points (0, 4, 16, and 24 h) after exposure to propofol anesthesia for 2, 4, and 6 h. Histograms represent mRNA levels expressed as the fold changes relative to the control value obtained from three separate experiments. The results are mean ± SEM. *p < 0.05 vs. the control value, presented as a black line; # p < 0.05 between treatments
Propofol treatment changed interleukin-1β gene expression in both structures (Fig. 5c, d). In the cortex, IL-12 was significantly increased within first 4 h after termination of all three anesthesia regimens (1.7–2.7-fold change above control, p < 0.05). Afterward, there was a transient return of IL-1β to the control level (at 16-h post-anesthesia), and trend toward increase was detected at 24-h time point Fig. 5c). In the thalamus, 2-h exposure induced change at 4 h post-anesthesia only, when twofold elevation above control level was measured. Four- and 6-h exposures to propofol induced peak in IL-1β gene expression immediately following termination of anesthesia, which were followed by decrease to control level or above it (for 6-h exposure at 16-h time point, p < 0.05) at 16–24 h time frame (Fig. 5d).
We next examined the potential of propofol anesthesia to stimulate microglial activation using staining by calcium-binding protein (Iba-1), which is a marker of microglial cells. Animals were exposed to propofol anesthesia for 6 h and were sacrificed after 24 h of recovery time. The most distinct microglial morphology during propofol treatment is appearance of cells displaying highly round-shaped amoeboid morphology with retracted processes and enlarged cell bodies (Fig 6). Following 6-h exposure to propofol, increased Iba-1- positive staining was detected mostly in retrosplenial cortex as well as in the laterodorsal thalamic nucleus The control samples of the cortex and thalamus exhibited a very low degree of microglia activation as revealed by a minimal number of Iba-1 stained cells. It was concluded that propofol anesthesia could induce activation of microglia in brain structures of P7 rats.
Representative images of propofol-induced microglia cells in the cortex and thalamus of P7 rats. Animals were exposed to propofol anesthesia for 6 h and were sacrificed after 24 h of recovery time. Brain sections from the cortex and thalamus were stained for the Iba-1 marker of microglial cells. At 24-h post propofol exposure, activated microglial cells display highly amoeboid and round-shaped morphology with retracted processes and enlarged cell bodies. The control samples of the cortex and thalamus exhibited a very low degree of microglial activation as revealed by small cell bodies and elongated distal ramified processes throughout the recovery period. Images are representative of three animals per experimental group. Scale bars 20 µm
Motor Activity of Rats Neonatally Exposed to Propofol Anesthesia During Habituation Testing at P35
Animals neonatally exposed to 6 h period of propofol anesthesia showed peculiar behavior during three consecutive days of habituation session as adolescents (P35), when compared to the age-matched control group (Fig. 7).
Motor activity of rats neonatally exposed to propofol anesthesia during habituation testing at P35. Results of locomotor and vertical activities were expressed as time-dependent changes during the intrasession habituation (a and d, respectively), the summary for the first 5 min as the period of the most intensive exploratory activity (b and e, respectively), and the summary for the whole 30-min registration period to assess intersession habituation (c and f, respectively). The mark asterisk denotes p < 0.05 vs. the same day of control group; hash denotes p < 0.05 vs. the first day of the same group (n = 6 per group)
Intrasession habituation was present in control and propofol-exposed groups at all days of testing regarding locomotor (Fig. 7a) and vertical activities (Fig. 7d). It was expressed through decrease of these activities during the time, representing adaptability of animals to the environment. When analyzing the first 5 min of registration period for both locomotor (Fig. 7b) and vertical (Fig. 7e) activities, statistical analysis revealed significant influence of propofol treatment [F(1, 10) = 22.745, p = 0.001 and F(1, 10) = 26.907, p < 0.001, respectively] and time [F(2, 20) = 7.396, p = 0.004 and F(2, 20) = 5.192, p = 0.017, respectively]. Compared to the control group, propofol-exposed animals showed increases in both activities during the first 5 min of testing on all 3 days examined (Fig. 7b, e, *p < 0.05). Post-hoc analysis also revealed significant decreases in locomotor and vertical activities during the 3rd day of the registration period compared to the 1st day (Figs. 7b, e, # p < 0.05) in both experimental groups. Statistical analysis of total locomotor and vertical activities for the 30-min registration period (Fig. 7c, f) confirmed significant influence of propofol treatment [F(1, 10) = 15.265, p = 0.004 and F(1, 10) = 8.231, p = 0.018, respectively] and time [F(2, 20) = 47.864, p = 0.001 and F(2, 20) = 10.707, p = 0.001, respectively]. For both experimental groups, decreases in the total locomotor (Fig. 7c) and vertical (Fig. 7f) activities during consecutive 3 days of testing (intersession habituation) were observed (# p < 0.05 vs. the first day of the same group), with significantly increased motor activities of animals neonatally exposed to propofol anesthesia in comparison with the control (*p < 0.05 vs. the same day of control group).
Motor Activity of Rats Neonatally Exposed to Propofol Anesthesia During Habituation Testing at P60
Tested as adults, rats neonatally exposed to 6 h period of propofol anesthesia still had specificities in motor behavior during three consecutive days of habituation.
Intrasession habituation was observed in control and propofol-exposed groups at all days of testing regarding locomotor (Fig. 8a) and vertical activities (Fig. 8d). When analyzing the first 5 min of registration period for both locomotor (Fig. 8b) and vertical (Fig. 8e) activities statistical analysis revealed significant influence of propofol treatment [F(1, 10) = 24.387, p = 0.004 and F(1, 10) = 15.682, p = 0.003, respectively]; factor time was significant only for locomotor activity (F(2, 20) = 4.775, p = 0.022). Compared to the control group, propofol-exposed animals showed increase in both activities during the first 5 min during the first two days of testing (Fig. 8b, e, *p < 0.05). Statistical analysis of total locomotor and vertical activities for the 30-min registration period (Fig. 8c, f) confirmed significant influence of propofol treatment [F(1, 10) = 6.631, p = 0.030 and F(1, 10) = 13.255, p = 0.005, respectively] and time [F(2, 20) = 32.972, p < 0.001 and F(2, 20) = 7.533, p = 0.004, respectively]. For both experimental groups, decreases in total locomotor (Fig. 8c) and vertical (Fig. 8f) activities during consecutive 3 days of testing (intersession habituation) were observed (# p < 0.05 vs. the first day of the same group), with significantly increased motor activities of animals neonatally exposed to propofol anesthesia in comparison to the control only during the first day of testing (Fig. 8c, f, *p < 0.05 vs. the same day of control group).
Motor activity of rats neonatally exposed to propofol anesthesia during habituation testing at P60. Results of locomotor and vertical activities were expressed as time-dependent changes during the intrasession habituation (a and d, respectively), the summary for the first 5 min as the period of the most intensive exploratory activity (b and e, respectively), and the summary for the whole 30-min registration period to assess intersession habituation (c and f, respectively). The mark asterisk denotes p < 0.05 vs. the same day of control group; hash denotes p < 0.05 vs. the first day of the same group (n = 6 per group)
Discussion
This study demonstrates that exposures to 2-, 4-, and 6-h-long propofol anesthesia induce expressions of proapoptotic and proinflammatory cytokine mRNAs and proteins in the cortical and thalamic structures of P7 rats. We established increased expressions of FasL/Fas death receptor and caspase-8, known markers of extrinsic apoptotic pathway, as well as changes in Bcl-2 and caspase-9 expressions, markers of the intrinsic apoptotic pathway activation. As elevated expression of Fas/FasL is often associated with an inflamed and degenerating brain, we also examined transcriptional expressions of pro-inflammatory caspase-1 and IL-1β mRNA concluding that their early increase may be involved in the detected microglial activation at 24-h after termination of propofol exposures. We also found long-term functional consequences of neonatal propofol treatment as P35 and P60 animals, which showed habituation to the open field, were clearly hyperactive throughout test periods.
In our previous work, we had clearly demonstrated that 2-, 4-, and 6 h-long exposures to propofol induced neuroapoptosis in cortex and thalamus of P7 rats and showed appearance of Fluoro-Jade positive cells immediately after termination of these three anesthesia durations, as well as 24 h later (Milanovic et al. 2010). We established that both caspase-3 and calpain proteases participate in neurodegeneration and proposed some potential mechanisms of propofol neurotoxicity in immature rat brain (Pesic et al. 2009; Milanovic et al. 2014; Popic et al. 2015; Pesic et al. 2015). Among other findings, we showed rapid and strong activations of TNFα and TNF receptors occurring within 4 h after prolonged propofol administration to P7. Also, propofol-induced neuroapoptosis can be partially triggered by neurotrophins misbalance leading to activation of p75 receptor signaling (Milanovic et al. 2014). Both TNF and p75 receptors belong to a family of TNF death receptors participating in degenerative and inflammatory processes in the CNS (Wajant et al. 2003; Choi and Benveniste 2004). As the role of Fas receptor, third remarkable member of TNF-death receptor family, and its ligand FasL had not been studied in the propofol-induced apoptosis, this study was undertaken to examine if Fas receptor and its ligand, FasL, contribute to neurodegeneration detected after 2, 4, or 6 h-exposures (Milanovic et al. 2010). The present data revealed that Fas/FasL show brain region-specific pattern of expression in immature rats after propofol treatment. We supposed that concomitant decline of Fas/FasL proteins’ expressions points to internalization of the Fas/FasL complex. FAS internalization that occurs 30–60 min after ligand binding was followed by rapid lysosomal degradation as was demonstrated in vitro (Algeciras-Schimnich et al. 2002). However, beside the termination of the signaling, the internalization may play a role in desensitization cells to extracellular signals, not only in the receptor and/or ligand recycling but also in localizations of receptor complex and downstream signaling molecules (as was reported for TNF complex; Wajant et al. 2003). Contrary to the cortex, increased expressions of Fas and FasL were detected early in the thalamus, and this finding is consistent with the results of the Yon et al. (2005) following application of anesthetic cocktail (midazolam, isoflurane, and nitrous oxide) that induced apoptosis in P7 animals.
To resolve possible implications of Fas/FasL changes, we next examined caspase-8 expression, the main downstream molecule in the extrinsic apoptotic pathway. Our observation that propofol upregulated caspase-8 mRNA confirms the effect of a single dose of propofol in P7 rats (Pešić et al. 2009), and reported transcriptional upregulation of caspase-8 after traumatic brain injury in humans (Zhang et al. 2003) and in rats (Beer et al. 2001). At protein level two isoforms of caspase-8 were detectable by Western blot, caspase-8a (55 kDa) and caspase-8b (53 kDa), that are processed in Death-Inducing Signaling Complex (DISC) to final active p18/p10 hetero-tetramer (Scaffidi et al. 1997; Lavrik et al. 2005). However, recent data indicate that caspase-8 does not have to be fully processed in order to acquire the enzymatic activity as the unprocessed enzyme p55/53, as well as first step cleaved p43/41 fragments may possess enzymatic activity too (Peter 2004; Thorburn 2004). Partially processed caspase-8 is bound to DISC and have limited approach to certain substrates (like receptor interacting protein, RIP), what might be of importance for some alternative functions of caspase-8 (Peter 2004). Although P43/41 isoforms are thought to recruit concomitantly to DISC and have similar pattern of activation (Scaffidi et al. 1997), it appears that they have different expression time profile after propofol anesthesia. Caspase-8 activation was more pronounced in the thalamus than in the cortex, which was expected, since the upstream signals, Fas/FasL and TNFα (Milanovic et al. 2014) were also changed in brain-region-dependent manner. It is well documented that the final step in caspase-dependent apoptosis provoked by different signals is the activation of caspase-3 that induces apoptotic fragmentation (Hengartner 2000). Caspase-8 can activate caspase-3 directly through death receptor pathway or indirectly by truncated Bid protein, the member of the pro-apoptotic Bcl-2 family, which initiates release of cytochrome c from mitochondria (Finucane et al. 1999; Reich et al. 2008).
Knowing that extrinsic apoptotic pathways can be performed simultaneously with converging intrinsic, we examined expression of Bcl-2 family members. We established that propofol anesthesia decreased transcription of anti-apoptotic Bcl-2 and Bcl-xL genes, while transcription of pro-apoptotic Bax and Bad was unaffected. Decline in the expression of Bcl-2 and Bcl-xl gene could be sufficient to misbalance in favor of pro-death signals, as demonstrated in different models of brain injury (Strauss et al. 2004; Perez-Navarro et al. 2005). Following propofol anesthesia caspase-9 zymogen level is persistently decreased in the cortex, which may suggest its proteolytic processing to the active forms. Considering also more prominent reduction in Bcl-2 protein level in the cortex, we could speculate that propofol activates intrinsic pathway in the cortex to a much greater extent than in the thalamus. However, it is not possible to make a direct conclusion on convergence of extrinsic to intrinsic pathway, as caspase-8-mediated truncation of Bid, Bcl-2 family protein (Elmore 2007; Villapol et al. 2007; Reich et al. 2008) was not studied herein.
Fas and TNF receptors, through RIP adapter protein, can activate caspase-1 which plays a key role in both apoptosis and inflammation in mammals (Wajant et al. 2003; Festjens et al. 2007). Cleavage of caspase-1 and generation of p20 active subunits lead to the proteolytic activation of pro-interleukin-1β into the mature and active cytokine (Denes et al. 2012). Several studies suggest that caspase-1 and IL-1β are involved in acute traumatic or ischemic brain or spinal cord injury as well as various neurodegenerative diseases (Clark et al. 1999; Friedlander 2000; Sifringer et al. 2007; Streit et al. 2014). In the present study, we demonstrated that propofol anesthesia upregulates transcription of caspase-1 and IL-1β genes in both structures. Their expression level is inversely correlated what can be explained by existing pools of both mRNA/proteins in the cells, fast translation of cytokines mRNA into proteins (like for TNFα; Wajant et al. 2003; Milanovic et al. 2010) and different dynamics of protein generation, as enzymes have ability to turn over many molecules of substrates at one time. Early upregulation of IL-1β expression, resembling the one ofTNFα mRNA (Milanovic et al. 2014), suggest that these cytokines might originate from neurons, in agreement with others who found cell-type-dependent cytokine production (Wu et al. 2012). However, as we observed an increasing trend in IL-1β expression 24 h after propofol anesthesia termination, especially in the cortex, we hypothesized that later wave of IL-1β may be due to subsequent activation of microglia. Microglial cells are the major components that mediate immune response and inflammation in the brain. Activated microglia play a critical role in neuroinflammation by releasing various inflammatory mediators, such as IL-1β, iNos, COX, TNF-α, and other cytokines, which may contribute to damage of neurons (Garden and Möller 2006; Lyman et al. 2014). Local inflammation directly interferes with the processes of memory consolidation, synaptic plasticity, and neurogenesis resulting in behavioral changes (Monje et al. 2003; Gemma et al. 2005). In the study of Cao et al. (2012), it was found that IL-1β may play a critical role in learning and memory, as widely used anesthetic isoflurane affected cognitive function of wild-type and not IL-1β-deficient mice. Recent in vivo and in vitro studies examining propofol toxicity report controversial data regarding inflammation and cognitive decline which may be consequences of different experimental designs and animal species used (Ye et al. 2013; Yu et al. 2013; Yang et al. 2014; Han et al. 2015).
In our model, we used novel object-recognition task (after retention delay of 1 h) and light–dark box tests to check cognitive and emotional consequences of propofol treatment, respectively, and they revealed no differences between control and the neonatally treated animals at P35 (data not shown). These results suggest that propofol-induced neurodegeneration has no long-term effects on short-term memory and anxiety, which has been hinted in previous studies (Karen et al. 2013). However, we revealed that animals previously exposed to 6-h-long propofol anesthesia have affected long-term memory, as assessed in habituation activities to the open field, which is nonaversive and nonassociative memory task. It has been suggested that intrasession habituation measures adaptability to the environment, whereas intersession habituation measures long-term memory to previous exposure (Bolivar 2009). Although findings in the field mainly accentuate learning-and-memory problems in animals neonatally exposed to general anesthesia (Han et al. 2015; Yu et al. 2013; Fredriksson et al. 2007), we found that propofol did not prevent formation of intersession habituation at P35. However, P35 animals had significantly higher exploratory activity compared to control littermates bringing up a proposal that hyperactivity could be an obstacle in reaching control-like memory score. This might be of significance in accordance with recent studies investigating the association between early exposure to general anesthesia and developmental or behavioral disorder (DBD), with ADHD as a major component (Tsai et al. 2015; Sprung et al. 2012). To the best of our knowledge, this is the first experimental evidence that rodents with prolonged exposure to propofol anesthesia during neonatal period (P7) exhibited hyperactivity during early adolescence (P35). This behavioral phenomenon persisted through to the young adulthood (P60), but in a more delicate form. The obtained results indicate that brain maturation (P35–P60 period) is a process that extensively encompasses natural removal of molecular/neurochemic causes of hyperactivity observed in adolescent rats. Since neuro-anatomic studies have described a massive synaptic pruning of dopamine receptors during adolescence in rodents (Laviola et al. 2003), it could be speculated that the affected function of dopaminergic receptors/system is in the base of observed phenomenon. Our previous work has already emphasized that this type of exposure of immature brain to propofol anesthesia during this critical phase of development provoked immediate changes in activity-dependent processes and synaptic adjustment. These changes influenced the brain capacity to integrate later developmental events and resulted in temporary altered response to acute psychotropic stimulation in adolescence (Pesic et al. 2015). In that sense, age-related molecular characterization of animals neonatally exposed to general anesthesia is of importance.
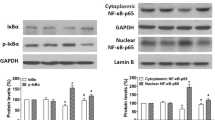
Although numerous literature data demonstrated the ability of anesthetics to induce morphological and functional injury in developing mammalian brain, many studies revealed the propofol might be an effective neuroprotective agent in the different models in vivo and in vitro (Tanaka et al. 2013; Ye et al. 2013; Zhang et al. 2011). However, some of these experimental paradigms were performed with concurrent noxious stimulation (stroke, trauma, seizure, inflammation) that had divergent patterns of neuronal activation and resulted in attenuation of the neuroapoptotic response (Fan et al. 2015 end references within). For example, nociceptive input into the sensory cortex can induce activation of neurons and microglia that may neutralize anesthetic-induced depression of neuronal and trophic activity, which is considered as a possible trigger of cell death (Liu et al. 2012). Propofol is similar in chemical structure to the active nucleus of antioxidants substances such as alpha-tocopherol (vitamin E), and it can directly scavenge ROS and inhibit free radical generation and lipid peroxidation to protect brain cells from oxidative stress implicated in many neurodegenerative disorders and brain dysfunction (Fan et al. 2015). A number of molecular events can be associated with propofol-mediated neuroprotection, including inhibition of ER stress response, repressed mitochondrial permeability transition pore, reduced glutamate concentration, NMDA response, Ca2+ increase, etc. (Zhang et al. 2012). It was shown that propofol protection can be achieved by activation and crosstalk between PI3P/AKT and JAK2/STAT pathways, as well as by activated MAPK/ERK cascade, through a very fast phosphorylation of signaling pathways (10–60 min) and translocation of transcription factors (up to 4 h) after propofol exposure (Shravah et al. 2014; Kidambi et al. 2010). Our studies in vivo showed also that propofol led to early activation of pro-survival Akt and ERK1/2 kinases, changed expression c-fos, and NfKb transcription factors, and might have suppressed the last step of apoptotic cascade inhibiting caspase-3 activity by XIAP overexpression (Milanovic et al. 2014; Popic et al. 2015). Altogether, in P7 and P14 propofol-anesthetized animals, we registered the same apoptotic and anti-apoptotic signaling pathways to be influenced, but mechanisms responsible for the dual effects and opposing outcomes (apoptosis at P7 and cell-survival at P14) still need to be resolved. Considering inevitability of anesthesia, a reasonable standpoint in the clinical settings would be to potentiate ability of anesthetics to induce intrinsic neuroprotective mechanisms by applying exogenous substances such as erythropoietin, melatonin, or omega-3 (Olsen and Brambrink 2013; Lei et al. 2012).
Notablly, it is still debatable whether neuronal cell loss is in relation with observed long-term impairment in learning and memory induced by some individual or mix of anesthetics. Stratmann et al. (2010) showed that in P7 rat brain, cell loss likely reflects severity of the treatment and cannot be causally linked to subsequent cognitive dysfunctions. Also, it needs to be determined if the absence of neuronal cell death does mean that surviving neurons are not impacted by anesthesia and function properly.
Taken together, we have found that propofol anesthesia activates Fas/FasL-mediated extrinsic and Bcl-2-dependent intrinsic apoptotic pathways, resulting in caspase-8 and caspase-9 activations, respectively. Moreover, we have established upregulation of caspase-1 and IL-1β cytokine transcriptions as well as subsequent activation of microglia,which could be potentially associated with brain inflammation. Behavioral data revealed that hyperactivity persists through adolescence and young adulthood, suggesting that neonatal propofol exposure changed at least some aspects of neurodevelopment. These data, together with our previous results, contribute to elucidation of complex mechanisms of propofol toxicity in developing brain (Fig. 9), with the aim to provide insight into signaling cascade in the search for the possible targets for neuroprotection.
Proposed mechanisms of propofol neurotoxicity in the developing brain. Propofol anesthesia activates TNF-, Fas- and p75-mediated apoptotic pathways and also decreases Bcl-2 expression, violating mitochondrial integrity. This causes activations of caspase-8 and -9, which activate executor-caspase-3. Propofol also increases Ca2+ concentration in the cytoplasm leading to activation of calpain, Ca2+-dependent protease. Early increase of cytokines expression brings microglia to an active state afterward. Finally, all these processes result in cell damage, apoptosis, and inflammation, which can be somewhat diminished by potential endogenous (Erk, Akt, and XIAP upregulation) neuroprotective mechanisms (Popic et al. 2015; Pesic et al. 2015; Milanovic et al. 2014; Popic et al. 2012; Milanovic et al. 2010; Pesic et al. 2009).
References
Algeciras-Schimnich A, Shen L, Barnhart BC, Murmann AE, Burkhardt JK, Peter ME (2002) Molecular ordering of the initial signaling events of CD95. Mol Cell Biol 22:207–220
Alkire MT, Hudetz AG, Tononi G (2008) Consciousness and anesthesia. Science 322:876–880
Andersen SL, Thompson AT, Rutstein M, Hostetter JC, Teicher MH (2000) Dopamine receptor pruning in prefrontal cortex during the periadolescent period in rats. Synapse 37:167–169
Beer R, Franz G, Krajewski S, Pike BR, Hayes RL, Reed JC, Wang KK, Klimmer C, Schmutzhard E, Poewe W, Kampfl A (2001) Temporal and spatial profile of caspase 8 expression and proteolysis after experimental traumatic brain injury. J Neurochem 78:862–873
Bercker S, Bert B, Bittigau P, Felderhoff-Müser U, Bührer C, Ikonomidou C, Weise M, Kaisers UX, Kerner T (2009) Neurodegeneration in newborn rats following propofol and sevoflurane anesthesia. Neurotox Res 16:140–147
Bolivar VJ (2009) Intrasession and intersession habituation in mice: from inbred strain variability to linkage analysis. Neurobiol Learn Mem 92(2):206–214
Brambrink AM, Evers AS, Avidan MS, Farber NB, Smith DJ, Martin LD, Dissen GA, Creeley CE, Olney JW (2012) Ketamine-induced neuroapoptosis in the fetal and neonatal rhesus macaque brain. Anesthesiology 116:372–384
Cao L, Li L, Lin D, Zuo (2012) Isoflurane induces learning impairment that is mediated by interleukin 1beta in rodents. PLoS One 7(12):e51431. doi:10.1371/journal.pone.0051431
Choi C, Benveniste EN (2004) Fas ligand/Fas system in the brain: regulator of immune and apoptotic responses. Brain Res Brain Res Rev 44:65–81
Clark RS, Kochanek PM, Chen M, Watkins SC, Marion DW, Chen J, Hamilton RL, Loeffert JE, Graham SH (1999) Increases in bcl-2 and cleavage of caspase-1 and caspase-3 in human brain after head injury. FASEB J 8:813–821
Denes A, Lopez-Castejon G, Brough D (2012) Caspase-1: is IL-1 just the tip of the ICEberg? Cell Death Dis 3:e338. doi:10.1038/cddis.2012.86
Dobbing J, Sands J (1979) The brain growth spurt in various mammalian species. Early Hum Dev 3:79–84
Elmore S (2007) Apoptosis: a review of programmed cell death. Toxicol Pathol 35:495–516
Fan W, Zhu X, Wu L, Wu Z, Li D, Huang F, He H (2015) Propofol:an anesthetic possessing neuroprotective effects. Eur Rev Med Pharmacol Sci 19:1520–1529
Festjens N, Vanden Berghe T, Cornelis S, Vandenabeele P (2007) RIP1, a kinase on the crossroads of a cell’s decision to live or die. Cell Death Differ 14:400–410
Finucane DM, Bossy-Wetzel E, Waterhouse NJ, Cotter TG, Green DR (1999) Bax-induced caspase activation and apoptosis via cytochrome c release from mitochondria is inhibitable by Bcl-XL. J Biol Chem 274:2225–2233
Fredriksson A, Ponten E, Gordh T, Eriksson P (2007) Neonatal exposure to a combination of N-methyl-d-aspartate and gamma-aminobutyric acid type A receptor anesthetic agents potentiates apoptotic neurodegeneration and persistent behavioral deficits. Anesthesiology 107:427–436
Friedlander RM (2000) Role of caspase 1 in neurologic disease. Arch Neurol 57:1273–1276
Garden GA, Möller T (2006) Microglia biology in health and disease. J Neuroimmune Pharmacol 1:127–137
Gemma C, Fister M, Hudson C, Bickford PC (2005) Improvement of memory for context by inhibition of caspase-1 in aged rats. Eur J Neurosci 22:1751–1756
Han D, Jin J, Fang H, Xu G (2015) long-term action of propofol on cognitive function and hippocampal neuroapoptosis in neonatal rats. Int J Clin Exp Med 8(7):10696–10704
Hengartner MO (2000) The biochemistry of apoptosis. Nature 407:770–776
Ikonomidou C, Bosch F, Miksa M, Bittigau P, Vöckler J, Dikranian K, Tenkova TI, Stefovska V, Turski L, Olney JW (1999) Blockade of NMDA receptors and apoptotic neurodegeneration in the developing brain. Science 283:70–74
Jevtovic-Todorovic V (2010) Developing brain and general anesthesia—is there a cause for concern? Med Rep 2:68. doi:10.3410/M2-68
Jevtovic-Todorovic V, Hartman RE, Izumi Y, Benshoff ND, Dikranian K, Zorumski CF, Olney J, Wozniak DF (2003) Early exposure to common anesthetic agents causes widespread neurodegeneration in the developing rat brain and persistent learning deficits. J Neurosci 23:876–882
Karen T, Schlager GW, Bendix I, Sifringer M, Herrmann R, Pantazis C, Enot D, Keller M, Kerner T, Felderhoff-Mueser U (2013) Effect of propofol in the immature rat brain on short- and long-term neurodevelopmental outcome. PLoS One 8(5):e64489. doi:10.1371/journal.pone.0064480
Kidambi S, Yarmush J, Berdichevsky Y, Kamath S, Fong W, SchianodiCola J (2010) Propofol induces MAPK/ERK cascade dependant expression of cFos and Egr-1 in rat hippocampal slices. BMC Res Notes 3:201
Kodama M, Satoh Y, Otsubo Y, Araki Y, Yonamine R, Masui K, Kazama T (2011) Neonatal desflurane exposure induces more robust neuroapoptosis than do isoflurane and sevoflurane and impairs working memory. Anesthesiology 115:979–991
Kubo K, Inada T, Shingu K (2011) Possible role of propofol’s cyclooxygenase-inhibiting property in alleviating dopaminergic neuronal loss in the substantia nigra in an MPTP-induced murine model of Parkinson’s disease. Brain Res 1387:125–133
Laviola G, Macri S, Morley-Fletcher S, Adriani W (2003) Risk-taking behavior in adolescent mice:psychobiological determinants and early epigenetic influence. Neurosci Biobehav Rev 27:19–31
Lavrik IN, Golks A, Krammer PH (2005) Caspases: pharmacological manipulation of cell death. J Clin Invest 115:2665–2672
Lei X, Guo Q, Zhang J (2012) Mechanistic insights into neurotoxicity induced by anesthetics in the developing brain. Int J Med Sci 13(6):6772–6799
Liu JR, Liu Q, Li J, Baek C, Han XH, Athiraman U, Soriano SG (2012) Noxious stimulation attenuates ketamine-induced neuroapoptosis in the developing rat brain. Anesthesiology 117:64–71
Livak KJ, Schmittgen TD (2001) Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods 25:402–408
Loepke AW, Soriano SG (2008) An assessment of the effects of general anesthetics on developing brain structure and neurocognitive function. Anesth Analg 106:1681–1707
Lyman M, Lloyd DG, Ji X, Vizcaychipi MP, Ma D (2014) Neuroinflammation: the role and consequences. Neurosci Res 79:1–12
Milanovic D, Popic J, Pesic V, Loncarevic-Vasiljkovic N, Kanazir S, Jevtovic-Todorovic V, Ruzdijic S (2010) Regional and temporal profiles of calpain and caspase-3 activities in postnatal rat brain following repeated propofol administration. Dev Neurosci 32:288–301
Milanovic D, Pesic V, Popic J, Tanic N, Kanazir S, Jevtovic-Todorovic V, Ruzdijic S (2014) Propofol anesthesia induces proapoptotic tumor necrosis factor-α and pro-nerve growth factor signaling as well as prosurvival Akt and XIAP expression in neonatal rat brain. J Neurosci Res 92:1362–1373
Monje ML, Toda H, Palmer TD (2003) Inflammatory blockade restores adult hippocampal neurogenesis. Science 302:1760–1765
Olsen EA, Brambrink AM (2013) Anesthesia for the young child undergoing ambulatory procedures: current concerns regarding harm to the developing brain. Curr Opin Anesthesiol 26:677–684
Pearn ML, Hu Y, Niesman IR, Patel HH, Drummond JC, Roth DM, Akassoglou K, Patel PM, Head BP (2012) Propofol neurotoxicity is mediated by p75 neurotrophin receptor activation. Anesthesiology 116:352–361
Perez-Navarro E, Gavaldà N, Gratacòs E, Alberch J (2005) Brain-derived neurotrophic factor prevents changes in Bcl-2 family members and caspase-3 activation induced by excitotoxicity in the striatum. J Neurochem 92:678–691
Pesic V, Milanovic D, Tanic N, Popic J, Kanazir S, Jevtovic-Todorovic V, Ruzdijic S (2009) Potential mechanism of cell death in the developing rat brain induced by propofol anesthesia. Int JDev Neurosci 27:279–287
Pesic V, Milanovic D, Popic J, Smiljanic K, Tesic V, Kanazir S, Jevtovic-Todorovic V, Ruzidijic S (2015) Neonatal propofol anesthesia modifies activity-dependent processes and induces transient hyperlocomotor response to d-amphetamine during adolescence in rats. Int J Devl neuroscience 47:266–277
Peter ME (2004) The flip side of FLIP. Biochem J 382:e1–e3
Popic J, Pesic V, Milanovic D, Todorovic S, Kanazir S, Jevtovic-Todorovic V, Ruzdijic S (2012) Propofol-induced changes in neurotrophic signaling in the developing nervous system in vivo. PLoS One 7(4):e34396. doi:10.1371/journal.pone.0034396
Popic J, Pesic V, Milanovic D, Loncarevic-Vasiljkovic N, Smiljanic K, Kanazir S, Ruzdijic S (2015) Induction of TNF-α signaling cascade in neonatal rat brain during propofol anesthesia. Int J Dev Neurosci 44:22–32
Reich A, Spering C, Schulz JB (2008) Death receptor Fas (CD95) signaling in the central nervous system: tuning neuroplasticity? Trends Neurosci 31:478–486
Scaffidi C, Medema JP, Krammer PH, Peter ME (1997) FLICE is predominantly expressed as two functionally active isoforms, caspase-8/a and caspase-8/b. J Biol Chem 272:26953–26958
Servick K (2014) Biomedical Research. Researchers struggle to gauge risks of childhood anesthesia. Science 346:1161–1162
Shen X, Dong Y, Xu Z, Wang H, Miao C, Soriano SG, Sun D, Baxter MG, Zhang Y, Xie Z (2013) Selective anesthesia-induced neuroinflammation in developing mouse brain and cognitive impairment. Anesthesiology 118:502–515
Shravah J, Wang B, Pavlovic M, Kumar U, Chen DDY, Luo H, Ansley DM (2014) Propofol mediates signal transducer and activator of transcription 3 activation and crosstalk with phosphoinositide 3-kinase/AKT. JAKSTAT 3(2):e29554
Sifringer M, Stefovska V, Endesfelder S, Stahel PF, Genz K, Dzietko M, Ikonomidou C, Felderhoff-Mueser U (2007) Activation of caspase-1 dependent interleukins in developmental brain trauma. Neurobiol Dis 25:614–622
Sprung J, Flick R, Katusic S, Colligan RC, Barbaresi WJ, Bojanic K, Welch TL, Olson MD, Hanson AC, Schroeder DR, Wilder RT, Warner DO (2012) Attention-deficit/hyperactivity disorder after early exposure to procedures requiring general anesthesia. Mayo Clin Proc 87(2):120–129
Stratmann G, Sall JW, May LDV, Loepke AW, Lee MT (2010) Beyond anesthetic properties: the effects of isoflurane on brain cell death, neurogenesis, and long-term neurocognitive function. Anesth Analg 110(2):431–437
Strauss KI, Narayan RK, Raghupathi R (2004) Common patterns of Bcl-2 family gene expression in two traumatic brain injury models. Neurotox Res 6:333–342
Streit W, Xue QS, Tischer J, Bechmann I (2014) Microglial pathology. Acta Neuropathol Commun. 2014(2):142. doi:10.1186/s40478-014-0142-6
Tanaka T, Kai S, Matsuyama T, Adachi T, Fukuda K, Hirota K (2013) General Anesthetics Inhibit LPS-Induced IL-1β Expression in Glial Cells. PLoS ONE 8(12):e82930. doi:10.1371/journal.pone.0082930
Thorburn A (2004) Death receptor-induced cell killing. Cell Signal 16:139–144
Tsai CJ, Lee CTC, Liang HY, Tsai PJ, Chen VCH, Gossop M (2015) Risk of ADHD after multiple exposures to general anesthesia: a nationwide retrospective cohort study. J Att Dis. doi:10.1177/1087054715587094
Villapol S, Acarin L, Faiz M, Castellano B, Gonzalez B (2007) Distinct spatial and temporal activation of caspase pathways in neurons and glial cells after excitotoxic damage to the immature rat brain. J Neurosci Res 85:3545–3556
Vutskits L, Davis PJ, Hansen TG (2012) Anesthetics and the developing brain: time for a change in practice? A pro/con debate. Paediatr Anaesth 22(10):973–980
Wajant H, Pfizenmaier K, Scheurich P (2003) Tumor necrosis factor signaling. Cell Death Differ 10:45–65
Wilder RT (2010) Is there any relationship between long-term behavior disturbance and early exposure to anesthesia? Curr opin Anaesthesia 23(3):332–336
Wilder RT, Flick RP, Sprung J, Katusic SK, Barbaresi WJ, Mickelson C, Gleich SJ, Schroeder DR, Weaver AL, Warner DO (2009) Early exposure to anesthesia and learning disabilities in a population-based birth cohort. Anesthesiology 110(4):796–804
Wu X, Lu Y, Dong Y, Zhang G, Zhang YY, Xu ZP, Culley DJ, Crosby G, Marcantonio ER, Tanzi RE, Xie Z (2012) The inhalation anesthetic isoflurane increases levels of pro-inflammatory TNF-α, IL-6 and IL-1β. Neurobiol Aging 33:1364–1378
Yang B, Liang G, Khojasteh S, Wu Z, Yang W, Joseph D, Wei H (2014) Comparison of neurodegeneration and cognitive impairment in neonatal mice exposed to propofol or isoflurane. PLoS One 9(6):e99171. doi:10.1371/journal.pone.0099171
Ye X, Lian Q, Eckenhoff MF, Eckenhoff RG, Pan JZ (2013) Differential general anesthetic effects on microglial cytokine expression. PLoS One 8(1):e52887. doi:10.1371/journal.pone.0052887
Yon JH, Daniel-Johnson J, Carter LB, Jevtovic-Todorovic V (2005) Anesthesia induces neuronal cell death in the developing rat brain via the intrinsic and extrinsic apoptotic pathways. Neuroscience 135:815–827
Yu D, Jiang Y, Gao J, Liu B, Chen P (2013) Repeated exposure to propofol potentiates neuroapoptosis and long-term behavioral deficits in neonatal rats. Neurosci Lett 534:41–46
Zhang X, Graham SH, Kochanek PM, Marion DW, Nathaniel PD, Watkins SC, Clark SB (2003) Caspase-8 expression and proteolysis in human brain after severe head injury. FASEB J 17:1367–1369
Zhang Y, Zhen Y, Dong Y, Xu Z, Yue Y, Golde TE, Tanzi RE, Moir RD, Xie Z (2011) Anesthetic propofol attenuates the isoflurane-induced caspase-3 activation and Aβ oligomerization. PLoS One 6(11):e27019. doi:10.1371/journal.pone.0027019
Zhang Y, Dong Y, Xu Z, Xie Z (2012) Propofol and magnesium attenuate isoflurane-induced caspase-3 activation via inhibiting mitochondrial permeability transition pore. Med Gas Res 2:20
Acknowledgments
This work was supported by the Grant ON173056 from the Ministry of Education, Science and Technological Development of the Republic of Serbia.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No conflict of interest to declare.
Electronic supplementary material
Below is the link to the electronic supplementary material.
12640_2016_9629_MOESM1_ESM.tif
Supplementary Figure 1. Time-dependent changes of Bcl-xL, Bax and Bad mRNA expression in the cortex (A) and the thalamus (B) of P7 rats after propofol anesthesia were examined by using semi-quantitative RT-PCR. The results are presented for animals at different recovery time points (0, 4, 16, and 24 hr) after exposure to propofol anesthesia for 2, 4, and 6 hr. Histograms represent mRNA levels expressed as the fold change relative to the control value (100%) obtained from three separate experiments. The results are mean ±SEM. *P<0.05 vs. the control value, presented as a black line; #P<0.05 between treatments. (TIF 1,156 kb)
Rights and permissions
About this article
Cite this article
Milanovic, D., Pesic, V., Loncarevic-Vasiljkovic, N. et al. The Fas Ligand/Fas Death Receptor Pathways Contribute to Propofol-Induced Apoptosis and Neuroinflammation in the Brain of Neonatal Rats. Neurotox Res 30, 434–452 (2016). https://doi.org/10.1007/s12640-016-9629-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12640-016-9629-1