Abstract
Deposition of amyloid-β (Aβ) peptides into specific encephalic structures has been pointed as an important event related to Alzheimer’s disease pathogenesis and associated with activation of glial cells, neuroinflammation, oxidative responses, and cognitive deficits. Aβ-induced pro-oxidative damage may regulate the activity of glutamate transporters, leading to reduced glutamate uptake and, as a consequence, excitotoxic events. Herein, we evaluated the effects of the pretreatment of atorvastatin, a HMG-CoA reductase inhibitor, on behavioral and biochemical alterations induced by a single intracerebroventricular (i.c.v.) injection of aggregated Aβ1–40 in mice. Atorvastatin (10 mg/kg/day, p.o.) was administered through seven consecutive days before Aβ1–40 administration. Aβ1–40 caused significant cognitive impairment in the object-place recognition task (2 weeks after the i.c.v. injection) and this phenomenon was abolished by atorvastatin pretreatment. Ex vivo evaluation of glutamate uptake into hippocampal and cerebral cortices slices showed atorvastatin, and Aβ1–40 decreased hippocampal and cortical Na+-dependent glutamate uptake. However, Aβ1–40 increased Na+-independent glutamate uptake and it was prevented by atorvastatin in prefrontal cortex slices. Moreover, Aβ1–40 treatment significantly increased the cerebrocortical activities of glutathione reductase and glutathione peroxidase and these events were blunted by atorvastatin pretreatment. Reduced or oxidized glutathione levels were not altered by Aβ1–40 and/or atorvastatin treatment. These results extend the notion of the protective action of atorvastatin against neuronal toxicity induced by Aβ1–40 demonstrating that a pretreatment with atorvastatin prevents the spatial learning and memory deficits induced by Aβ in rodents and promotes changes in glutamatergic and antioxidant systems mainly in prefrontal cortex.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alzheimer’s disease (AD) is characterized by neuronal death, memory loss, and progressive dementia and the histopathology consists of two known hallmarks: senile plaques formed from the aggregation of amyloid-β peptide (Aβ), and neurofibrillary tangles induced by tau hyperphosphorylation (Grundke-Iqbal 1986; Haass 2007). Currently, both fibrillar and soluble forms of low molecular weight of Aβ peptides are extensively studied and have been implicated in various cellular dysfunctions resulting in synaptotoxicity and neuronal cell death (Masters and Selkoe 2012).
During the progression of AD, many different types of neurons deteriorate, although there is a profound loss of forebrain cholinergic neurons, which is accompanied by a progressive decline in acetylcholine levels (Davies and Maloney 1976; Perry et al. 1977). Additionally, the glutamatergic neurotransmission is also affected in AD, probably initiating with a hypoactivity and then progressing to a hyperactivity of glutamatergic transmission associated with the severity of the disease (Schaeffer and Gattaz 2008).
In addition, excessive cholesterol levels in the brain also play important role in the development and progression of AD. It is noteworthy that Aβ aggregation and brain cholesterol metabolism seem to represent events that affect each other, since increased cholesterol levels play an important role in mediating Aβ aggregation and cholesterol-lowering agents, such as statins, have been suggested as potential preventive or therapeutic agents for AD (Longenberger and Shah 2011).
Statins are inhibitors of the enzyme 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase, thereby inhibiting cell synthesis of cholesterol and isoprenoids (Nelson and Cox 2000; Lee et al. 2008). Retrospective studies suggest that the prevalence of AD and vascular dementia is lower among patients taking statins (Jick et al. 2000; Wolozin et al. 2000). Atorvastatin, a member of statins family, is relatively more lipophilic and display a long half-life activity of HMG-CoA reductase inhibition when compared to other statins (Schachter 2005). Furthermore, the safety of high doses of atorvastatin has been demonstrated in adult humans (Waters 2005). Many studies have evaluated the pleiotropic effects of this statin, demonstrating its neuroprotective effects on diverse pathological conditions of the CNS (Piermartiri et al. 2009).
Studies have described a type of neuroinflammation induced by a single intracerebroventricular (i.c.v.) infusion of Aβ1–40 that mimics early phases of AD. Even though this acute infusion of this peptide in the brain of rodents is unable to induce all the pathological features of AD, it has been used as an experimental model for studying Aβ toxicity, which induces an inflammatory response associated with deficits in learning and memory (Medeiros et al. 2007; Prediger et al. 2007, 2008; Takeda et al. 2009; Piermartiri et al. 2010).
Of particular importance, we have shown that administration of atorvastatin (10 mg/kg, p.o.) for seven consecutive days after i.c.v. infusion of Aβ1–40 prevented hippocampal cell death, astrocytic glial fibrillar acidic protein (GFAP) and ciclooxigenase-2 increased expression, i.e., neuroinflammation and oxidative stress (Piermartiri et al. 2010), suggesting that statins not only prevent Aβ aggregation (Longenberger and Shah 2011), but also play protective effects by decreasing the toxicity induced by aggregated Aβ. However, this schedule of atorvastatin treatment (10 mg/kg, p.o., 7 days) after i.c.v. infusion of Aβ1–40 failed to improve spatial learning and impairments displayed by Aβ1–40-infused mice, although it was effective in preventing the neuronal degeneration (Piermartiri et al. 2010).
Other members of the statin family, such as fluvastatin, simvastatin, and pravastatin, have shown different effects regarding the intervention schedule against cognitive impairment induced by Aβ, due to prevention of cholinergic neuronal loss (Kurinami et al. 2008) or modulation of glutamatergic system (Tramontina et al. 2011). Therefore, in the present study, we investigated whether the pretreatment with atorvastatin is able to prevent the cognitive deficits induced by Aβ1–40 infusion in mice. Biochemical parameters related to the glutamate homeostasis, glutathione antioxidant system, and the acethylcolinesterase activity were also investigated in the hippocampus and prefrontal cortex in an attempt to elucidate potential mechanisms mediating atorvastatin-promoted neuroprotection.
Experimental Procedures
Animals
Male adult Swiss albino mice (3 months old/45–55 g) were kept on a 12-h light/dark cycle (light on at 07.00 a.m.) at a constant temperature of 22 ± 1 °C. They were housed in plastic cages with tap water and commercial food ad libitum. All procedures were carried out according to the institutional policies on animal experimental handling, designed to minimize suffering and limit the number of animals used and were approved by local Ethical Committee for Animal Research. All experiments were performed during the light phase (between 9:00 and 17:00 h) to avoid circadian variations.
Drug Treatment Protocol
Human Aβ1–40 (Tocris, Ellisville, MO, USA) was prepared as a stock solution at a concentration of 1 mg/ml in sterile 0.1 M phosphate-buffered saline (PBS) (pH 7.4) and aliquots were stored at −20 °C. Aβ solutions were aggregated by incubation at 37 °C for 4 days before use, as described previously (El Khoury et al. 1996). Previous analysis by transmission electronic microscopy showed that this Aβ1–40 preparation contains fibrils and protofibrils, in a mixture of low molecular weight species (Bicca et al. 2011). The Aβ1–40 peptide (400 pmol/mouse) or PBS (vehicle) was administered i.c.v. as previously described (Prediger et al. 2007, 2008; Piermartiri et al. 2010). Briefly, mice were anesthetized with isoflurane 0.96 % (0.75 CAM; Abbot Laboratórios do Brasil Ltda., RJ, Brazil) using a vaporizer system (SurgiVet Inc., WI, USA) and then gently restrained by hand for i.c.v. injections. The sterilization of the injection site was carried out using gauze embedded in 70 % ethanol. Under light anesthesia (i.e., just that necessary for loss of the postural reflex), the needle was inserted unilaterally 1 mm to the right of the midline point equidistant from each eye and 1 mm posterior to a line drawn through the anterior base of the eyes (used as external reference). A volume of 3 μl of Aβ1–40 or PBS solution was injected into the lateral ventricle, at the following coordinates from bregma: anteroposterior (AP) = −0.1 mm, mediolateral (ML) = 1 mm, and dorsoventral (DV) = −3 mm. The accurate placement of the injection site (needle track) was confirmed at the moment of dissection of the animals for the execution of biochemical experiments. Results from mice presenting any sign of cerebral hemorrhage were excluded from the statistical analysis (overall, less than 5 % of the total animals used).
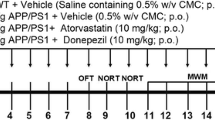
To study the putative modulation of atorvastatin on the molecular and behavioral changes induced by Aβ1–40, animals were treated orally (p.o.) with atorvastatin (Lipitor Atorvastatin calcium, Pfizer) 10 mg/kg/day, once a day during seven consecutive days (the last dose was administered 3 h before the i.c.v. administration of Aβ1–40 or PBS) (Piermartiri et al. 2010). Control animals were treated with vehicle (NaCl 0.9 %) orally for the same period. The treatment was done by the administration of 10 µl/g weight of the animal, both for the solutions of atorvastatin and saline. The experimental protocol of this study is summarized in Fig. 1.
Object-Place Recognition Task
Object-place recognition (OPR) task is based on the rodents natural behavior (novelty preference), an innate instinct that drives animals to learn about their environment (discrimination ratio). Additionally, it has been reported that the performance of this task is dependent on the hippocampus function (Binder et al. 2012). The OPR was performed in an apparatus consisting of an acrylic small chamber (25 cm × 25 cm × 40 cm). Before the experimental sessions, the animals were habituated to the experimental room for 90 min in dim light conditions. A light bulb was switched on during the experimental sessions. The light intensity was equal in the different parts of the apparatus. The objects were placed equidistant from two corners, 6 cm apart from the wall. Mice were placed individually into the chamber and performed the task for 5 min. In training sessions, two similar objects were utilized. In test sessions, performed 120 min later, one object was relocated to other corner of chamber. The objects employed were two LEGO® pieces presenting the same texture, size, shape, and color. The objects were not known to have any ethological significance for the mice. Discrimination ratio was expressed by the ratio TN/(TN + TF), (TN time spent exploring the novel place; TF time spent exploring familiar place), both in the training and test sessions. During the inter-trial interval, the objects were cleaned with 10 % ethanol solution to avoid odor cues. Exploration was defined by directing the nose to the object at a distance less than 2 cm and/or touching the object with the nose or forepaws. The time of exploration was measured by two blinded observers, with the use of chronometers. Animals that explored the objects less than 1.5 s in a session were excluded from the study.
Preparation and Incubation of Hippocampal and Prefrontal Cortex Slices
Eighteen days after the Aβ1–40 injection, animals (n = 5) were killed by decapitation, the brain was removed and the hippocampi and prefrontal cortex were rapidly dissected in ice-cold Krebs–Ringer bicarbonate buffer (KRB) of the following composition: 122 mM NaCl, 3 mM KCl, 1.2 mM MgSO4, 1.3 mM CaCl2, 0.4 mM KH2PO4, 25 mM NaHCO3, and 10 mM d-glucose. The buffer was bubbled with 95 % O2–5 % CO2 up to pH 7.4. Hippocampi and prefrontal cortex were sliced into 400-μm-thick transverse sections with a McIlwain tissue chopper, followed by transfer and separation into individual slices in an ice-cold KRB bath for 30 min.
Glutamate Uptake
Glutamate uptake was evaluated as previously described (Molz et al. 2005; Piermartiri et al. 2010). After preincubation of 30 min, slices were washed and then incubated for 15 min at 37° C in a Hank’s balanced salt solution (HBSS), composition in mM: 1.29 CaCl2, 136.9 NaCl, 5.36 KCl, 0.65 MgSO4, 0.27 Na2HPO4, 1.1 KH2PO4, and 5 HEPES. Uptake was assessed by adding 0.33 µCi/ml l-[3H]glutamate with 100 µM unlabeled glutamate in a final volume of 300 µl. Incubation was stopped immediately after 7 min by discarding the incubation medium, and slices were submitted to two ice-cold washes with 1 ml HBSS. Slices were solubilized by adding a solution with 0.1 % NaOH/0.01 % SDS and incubated overnight. Aliquots of slice lysates were taken for determination of the intracellular content of l-[3H]glutamate by scintillation counting. Specific high-affinity l-[3H]glutamate uptake (Na+-dependent uptake) was calculated as the difference between uptake obtained in the incubation medium as described above (total glutamate uptake) and uptake obtained with a similar incubation medium containing 133 mM choline chloride instead of NaCl and slices were previously washed in order to remove extracellular Na+ (Na+-independent uptake). Results were expressed as nmol of l-[3H]glutamate taken up per milligram of protein per minute.
Tissue Preparation for Measuring Acetylcholinesterase and Antioxidant Enzymes Activity
The animals were killed by decapitation, and the prefrontal cortex and hippocampus were removed. The hippocampi were sliced as previously described, and two hippocampal slices and the prefrontal cortex were homogenized (1:10 w/v) in HEPES buffer (20 mM, pH 7.0). The tissue homogenates were centrifuged at 3000×g, at 4 °C for 5 min and an aliquot of the low-speed supernatant was used for the determination of acetylcholinesterase (AChE) activity. Thereafter, the supernatants of the first centrifugation were further centrifuged at 16,000×g, at 4 °C for 20 min and the supernatants obtained were used for the determination of glutathione reductase (GR) and glutathione peroxidase (GPx) activities.
Acetylcholinesterase Activity
The AChE activity in the homogenates of hippocampus and prefrontal cortex was measured as previously described (Ellman et al. 1961), using acetylthiocholine iodide (0.6 mM) as a substrate. The rate of hydrolysis of acetylthiocholine iodide was measured at 412 nm through the release of the thiol compound (thiocholine), which produces the color-forming compound TNB after reaction with DTNB.
Antioxidant Enzymes Activity
The GR activity was measured using a NADPH reduction assay following the protocol developed by Carlberg and Mannervik (1985) using glutathione disulfide (GSSG) as substrate. GR activity was monitored by decrease in NADPH absorbance at 340 nm at 37 °C in a TECAN Genios Microplate Reader (Tecan Group Ltd., Männedorf, Switzerland). Results were based on a molar extinction coefficient for NADPH of 6.22 × 103 M−1/cm. The GPx activity was measured using an NADPH reduction assay following the technique of Wendel (1981). Tissue supernatant (200 μg protein) was added to a reaction mixture containing reduced glutathione, GR, and NADPH in phosphate buffer (pH 7.4). The reaction was initiated by adding tert-butyl hydroperoxide (1 mM), and the absorbance decrease at 340 nm was recorded at 37 °C in a TECAN Genios Microplate Reader (Tecan Group Ltd., Männedorf, Switzerland). The activity in the absence of the samples was subtracted. Results were based on a molar extinction coefficient for NADPH of 6.22 × 103 M−1/cm.
Enzymatic Measurement of Glutathione
Total glutathione (GSHt) and GSSG levels were determined according to the method of Sacchetta et al. (1986). Briefly, samples were homogenized 1:10 in a phosphate potassium (KPi) buffer 0.25 M with N-ethylmaleimide (NEM) 10 mM. After 15 min, perchloric acid (PCA) was added to a final concentration of 0.5 M for deproteinization, samples were centrifuged at 15,000×g for 5 min, and the supernatant was collected. NEM interacts with GSH, leaving GSSG to be measured. Therefore, to eliminate free NEM in the sample, pH was increased to 11 by the addition of 2 M KOH/0.3 M MOPS/0.5 M KPI, and the mixture was incubated on ice for 10 min. Finally, after adding sufficient PCA to neutralize the pH to 7, samples were centrifuged and the supernatant collected for further measurements. For the assay, a 96-well plate was used, containing 160 µl of reaction Mix (KPi 0.1 mM, EDTA 1 mM, DTNB 0.1 mM, NADPH 0.2 mM, H2O) and 30 µl of sample, and the assay was initiated by adding 10 µl of 5 U/ml GR. The absorbance was read for 5 min at 412 nm (37 °C) using a TECAN Genios Microplate Reader (Tecan Group Ltd., Männedorf, Switzerland). Kinetic changes in absorbance were converted to concentrations of GSHt and GSSG in μmol/g of tissue, using a standard curve.
Protein Content
The measurement of protein content was performed by the method of Lowry et al. (1951), using bovine serum albumin as standard.
Statistical Analysis
All values are expressed as mean ± SEM. The statistical evaluation of the results was carried out using two-way analysis of variance (ANOVA) with pretreatment and treatment as the independent variables. Following significant ANOVAs, multiple post hoc comparisons were performed using the Newman–Keuls test. The accepted level of significance for the tests was P < 0.05. All tests were performed using the Statistica® software package (Stat Soft Inc., Tulsa, OK, USA).
Results
Object-Place Recognition Task (OPR)
Mice were treated orally with atorvastatin (10 mg/kg/day), once a day during seven consecutive days. Three hours after the last atorvastatin administration, mice received the i.c.v. infusion of Aβ1–40 (400 pmol/mouse) or vehicle and were evaluated for behavioral performance in the OPR task after 14 days.
OPR is a task based on the rodent natural behavior and the innate instinct that drives animals to learn about their environment (discrimination ratio). The data of OPR were presented as discrimination ratio and the total time spent exploring both objects. In the training session, all animal groups showed the same level of performance in the task, spending around 50 % of the time exploring each object, indicating the interest of these animals by the novelty and lack of preference for a specific location of the objects. In the test session, it was observed that the control and atorvastatin groups explored 60 and 63 % of the time, respectively, the object that was relocated indicating learning about the environment. The animals infused with Aβ1–40 exhibit a cognitive deficit, spending about 50 % of their time exploring each one of the objects, indicating that they were not able to recognize the object placed in the familiar location. This cognitive deficit was prevented in the group where the animals infused with Aβ1–40 were previously treated with atorvastatin (64 % of time exploring the relocated object). It was also observed that atorvastatin per se did not affect the performance of mice in the OPR (Fig. 2a).
Effect of pretreatment with atorvastatin on cognitive deficits promoted by Aβ1–40 evaluated in the object-place recognition task in mice. The animals received a 7-day pretreatment with atorvastatin (10 mg/kg, p.o.) or saline and then a single i.c.v. infusion of Aβ1–40 (400 pmol/mouse) or PBS. Behavioral analysis was performed at the 14th day after Aβ1–40 infusion. Graphs represent the discrimination ratio in training and test sessions (a) and the total time (b) (in s) recorded for the objects exploration in the training and test sessions. The test session was performed 120 min after the training session. Results are presented as mean ± SEM (n = 14–21/group). Significant difference for discrimination ratio between training and test sessions, *P < 0.05, and significant difference for discrimination ratio in relation to all other groups in the test session, # P < 0.05 (two-way ANOVA followed by Newman–Keuls post hoc test). a Pretreatment [F(1,57) = 4.65, P < 0.05], treatment [F(1,57) = 1.76, P = 0.19], and interaction [F(1,57) = 0.79, P = 0.38]. b Pretreatment [F(1,56) = 0.001, P = 0.97], treatment [F(1,56) = 1.05, P = 0.31], and interaction [F(1,56) = 0.003, P = 0.95]
Considering the total time of exploration, it was observed that all groups showed a similar time of exploration for the two objects in both sessions. These results demonstrate that Aβ1–40 and atorvastatin or combination of both did not alter the interest of animals for the objects or their locomotion in the two sessions of this task (Fig. 2b).
Glutamate Uptake
Glutamate uptake was evaluated in an ex vivo assay in slices of prefrontal cortices and hippocampus obtained from mice pretreated with atorvastatin and infused with Aβ1–40. Glutamate uptake into prefrontal cortical (Fig. 3a) or hippocampal (Fig. 3b) slices was significantly reduced by atorvastatin pretreatment, Aβ1–40 infusion and also by atorvastatin plus Aβ1–40 treatment.
Evaluation of glutamate uptake into cortical and hippocampal slices from mice subjected to atorvastatin pretreatment and i.c.v. infusion of Aβ1–40. The animals received a 7-day pretreatment with atorvastatin (10 mg/kg, p.o.) or saline and a single i.c.v. infusion of Aβ1–40 (400 pmol/mouse) or PBS. Total l-[3H] glutamate uptake assay into prefrontal cortical (a) and hippocampal slices (b) was evaluated on the 18th day after Aβ1–40 infusion (n = 5/group). Na+-dependent and Na+-independent glutamate uptake in the prefrontal cortical (c) and hippocampal slices (d) were evaluated on the 18th day after Aβ1–40 infusion (n = 5/group). Results are presented as mean ± SEM. Significant difference from PBS control group, *P < 0.05, significant difference from Ator + Aβ1–40 group, # P < 0.05 (two-way ANOVA followed by Newman–Keuls post hoc test). a Pretreatment [F(1,15) = 14.15, P < 0.01], treatment [F(1,15) = 0.08, P = 0.77], and interaction [F(1,15) = 27.5, P < 0.01]. b Pretreatment [F(1,16) = 5.04, P < 0.05], treatment [F(1,16) = 7.15, P < 0.05], and interaction [F(1,16) = 3.14, P = 0.09]. c Pretreatment [F(1,12) = 14.75, P < 0.01], treatment [F(1,12) = 0.05, P = 0.82], and interaction [F(1,12) = 9.17, P < 0.05]. d Pretreatment [F(1,8) = 6.85, P < 0.05], treatment [F(1,8) = 0.89, P = 0.37], and interaction [F(1,8) = 0.91, P = 0.36]
In order to discriminate a putative effect of treatments on selective glutamate transporters, an Na+-independent glutamate transporters activity assay was performed. In cortical slices, a significant increase in the Na+-independent glutamate uptake was observed in Aβ1–40-treated mice when compared with that in atorvastatin plus Aβ1–40-treated mice (Fig. 3c). As observed in the total glutamate uptake, Na+-dependent glutamate uptake was reduced by atorvastatin or Aβ1–40 treatment.
In the hippocampus, a similar pattern was observed, although no statistical significant effect was revealed even on Na+-dependent or Na+-independent glutamate transport (Fig. 3d).
Acetylcholinesterase Activity
Another important system involved in memory and learning is the cholinergic system, which is extensively studied in Alzheimer’s disease and involved in the current treatment for patients suffering from this disease (García-Ayllón et al. 2011). In our study, we use two main brain regions involved in cognitive process to verify the activity of AChE, the enzyme responsible for degrading acetylcholine released into the synaptic cleft. The analysis of acetylcholinesterease activity either in the prefrontal cortex or in the hippocampus did not show any statistical difference among groups (Table 1).
Total Glutathione, Glutathione Disulfide Levels, Glutathione Reductase, and Peroxidase Activities
Another process that might exacerbate neuronal damage and consequent loss of synapses, leading to higher cognitive impairment in several neurodegenerative diseases, is the production of reactive oxygen species (ROS). Based on this principle, we analyzed the GSHt and its oxidized form (GSSG) levels as well as activity of the two antioxidant enzymes involved in the cycle of glutathione, GR, and GPx, that are responsible for detoxifying free radicals, reducing or preventing oxidative damage in the brain. Levels of GSHt, GSSG, and GR, GPx activities were evaluated in the prefrontal cortices and hippocampi of mice treated with atorvastatin and Aβ1–40. No significant difference was observed in the total (GSHt, Fig. 4a, b) and oxidized (GSSG, Fig. 4c, d) glutathione levels in the prefrontal cortex and hippocampus. The ratio between reduced glutathione and its oxidized form (GSH/GSSG) also did not show any changes (data not shown).
Evaluation of total glutathione (GSHt) and glutathione disulfide (GSSG) levels in prefrontal cortex and hippocampus of mice subjected to atorvastatin pretreatment and i.c.v. infusion of Aβ1–40. The animals received a 7-day pretreatment with atorvastatin (10 mg/kg, p.o.) or saline and a single i.c.v. infusion of Aβ1–40 (400 pmol/mouse) or PBS. The assays were performed on the 18th day after Aβ1–40 infusion (n = 5/group). Graphs represent the GSHt levels in the prefrontal cortex (a) and in the hippocampus (b) and GSSG levels in the prefrontal cortex (c) and in the hippocampus (d). Values are expressed as mean ± SEM (two-way ANOVA followed by Newman–Keuls post hoc test). a Pretreatment [F(1,16) = 0.17, P = 0.68], treatment [F(1,16) = 2.84, P = 0.11], and interaction [F(1,16) = 0.10, P = 0.74]. b Pretreatment [F(1,16) = 7.08, P < 0.05], treatment [F(1,16) = 0.02, P = 0.87], and interaction [F(1,16) = 0.02, P = 0.87]. c Pretreatment [F(1,16) = 0.07, P = 0.78], treatment [F(1,16) = 1.17, P = 0.29], and interaction [F(1,16) = 0.33, P = 0.57]. d Pretreatment [F(1,16) = 2.60, P = 0.12], treatment [F(1,16) = 0.01, P = 0.9], and interaction [F(1,16) = 0.93, P = 0.34]
GR activity assay in the prefrontal cerebral cortex of mice (Fig. 5a) showed a significant increase in the activity of this enzyme in the group infused with Aβ1–40, which was reversed in the group pretreated with atorvastatin. In the hippocampus (Fig. 5b), the group treated with atorvastatin plus Aβ1–40 had a significant increase in GR activity with respect to all other groups. Animals that received atorvastatin and animals infused with Aβ1–40 showed no differences from the control group.
Evaluation of glutathione reductase (GR) and glutathione peroxidase (GPx) activities in prefrontal cortex and hippocampus of mice subjected to atorvastatin pretreatment and i.c.v. infusion of Aβ1–40. The animals received a 7-day pretreatment with atorvastatin (10 mg/kg, p.o.) or saline and a single i.c.v. infusion of Aβ1–40 (400 pmol/mouse) or PBS. Enzymatic measurements were performed on the 18th day after Aβ1–40 infusion (n = 5/group). Graphs represent the GR activity in the prefrontal cortex (a) and in the hippocampus (b) and GPx activity in the prefrontal cortex (c) and in the hippocampus (d). Values are expressed as mean ± SEM. Significant difference from control group, *P < 0.05, significant difference from PBS control group, **P < 0.05, and significant difference from Aβ1–40 group, # P < 0.05 (two-way ANOVA followed by Newman–Keuls post hoc test). a Pretreatment [F(1,16) = 0.38, P = 0.54], treatment [F(1,16) = 16.38, P < 0.01], and interaction [F(1,16) = 6.82, P < 0.05]. b Pretreatment [F(1,16) = 6.28, P < 0.05], treatment [F(1,16) = 7.58, P < 0.05], and interaction [F(1,16) = 0.76, P = 0.39]. c Pretreatment [F(1,16) = 0.67, P = 0.42], treatment [F(1,16) = 3.16, P = 0.09], and interaction [F(1,16) = 8.82, P < 0.01]. d Pretreatment [F(1,16) = 0.79, P = 0.39], treatment [F(1,16) = 0.53, P = 0.47], and interaction [F(1,16) = 1.19, P = 0.29]
Regarding the enzymatic activity of GPx, it was observed that the Aβ1–40 group showed an increased activity of this enzyme and atorvastatin reversed the GPx activity to control levels in the prefrontal cortex (Fig. 5c). In the hippocampus, GPx activity showed no statistically significant difference among the groups (Fig. 5d).
Discussion
Our findings demonstrated that mice infused with Aβ1–40 display an impaired learning and loss of short-term memory in the OPR task, corroborating with other studies where amyloid peptides lead to cognitive deficits involving the hippocampus. Repeated pretreatment with atorvastatin for seven consecutive days prevents memory deficits induced by infusion of Aβ1–40. A previous study carried out in our laboratory showed that atorvastatin administered for 7 days after i.c.v. infusion of Aβ1–40 failed to reverse the deficits in spatial learning and memory in mice subject to the water maze task (Piermartiri et al. 2010). Other statins have also been shown to prevent cognitive deficits promoted by infusion of Aβ1–40, as the pretreatment with fluvastatin, in a water-finding task. However, the reversal of cognitive deficit induced by Aβ1–40 was not observed with a post-treatment with the same statin (Kurinami et al. 2008). Our data support the idea that different members of the statins family are able to prevent cognitive deficits in AD’s animal models and this prevention or reversal may also depend on the treatment schedule of these drugs.
The decrease in the cholinergic function is considered to be an important hallmark of AD (Auld et al. 2002). Our results showed no changes in AChE activity in the hippocampus and prefrontal cortex 18 days after infusion of Aβ1–40 neither in animals treated for seven consecutive days with atorvastatin. Many studies have compared elderly human brains presenting a diagnostic feature of early phases of AD with cognitive impairment of medium intensity with brains of patients in late stages of AD for cholinergic markers evaluation. It was observed that there was a reduction of cholinergic markers in patients in late stages of AD but not in those in the initial stages of the disease leading to the conclusion that cholinergic dysfunction may not occur until later stages of the disease (Davis et al. 1999; Tiraboschi et al. 2000). In our model, the animals begin to show cognitive dysfunction 7 days after administration of Aβ (Prediger et al. 2008) and our biochemical studies were conducted 18 days after the administration. Thus, a potential effect of Aβ toward the cholinergic system dysfunction may occur in later stages in our experimental model.
Previous studies have shown glutamatergic neurotransmission dysfunction in experimental models of AD (Piermartiri et al. 2010; Cassano et al. 2012). In transgenic 3XTg-AD mice, a decreased release of glutamate in the hippocampus and frontal cortex has been observed. A key issue seems to be the astrocytic involvement in the glutamatergic transmission in animal models of AD, since Aβ1–40 infusion leads to an increase in GFAP immunoreactivity in the hippocampus of mice, indicating a cytoskeletal reorganization of astrocytes as well as reduction in the immunoreactivity of the two main Na+-dependent glutamate transporters in astrocytes, GLAST and GLT-1, accompanied by reduced glutamate uptake (Piermartiri et al. 2010). To corroborate the idea that dysfunction of glutamatergic system is evoked by Aβ toxicity, we demonstrated that there is also a decrease in high-affinity Na+-dependent glutamate uptake in the prefrontal cortex which is still observed 18 days after Aβ1–40 infusion. However, atorvastatin pretreatment also decreased Na+-dependent glutamate uptake. The question why atorvastatin promoted a decrease in glutamate uptake per se is still unknown and under investigation in our laboratory. However, we have previously shown that the atorvastatin dose used in this experiment is not neurotoxic (Piermartiri et al. 2009, 2010). We have also assayed other parameters of glutamate transmission, such as glutamate release from hippocampal slices and glutamine synthetase activity, which were not altered in comparison to control groups with any treatment (data not shown).
Aiming to deeply investigate glutamate transport, it was observed that there was an increased Na+-independent glutamate uptake into cortical slices obtained from Aβ1–40-treated mice. Na+-independent glutamate transport is carried out mainly by cystine–glutamate exchanger (Xc− system), which is responsible for maintaining intracellular cysteine levels to glutathione synthesis (Aoyama et al. 2006). It is reasonable to suppose that an increased glutamate uptake by these carriers would lead to an increased release of cysteine, contributing to decrease in the rate-limiting substrate to glutathione synthesis. However, when evaluating glutathione levels, no significant reduction was observed in reduced (GSH) or oxidized glutathione (GSSG) levels. Experiments with chronic administration of atorvastatin in dogs have shown an increased GSH/GSSG ratio (Barone et al. 2011). A putative alteration in Xc− system expression is still an issue to be addressed, but our results clearly shown differential effects between the two cerebral regions studied.
Experimental and clinical studies indicate that oxidative stress plays a major role in the pathophysiology of AD (Butterfield and Lauderback 2002; Aluise et al. 2010; Sultana et al. 2011). Of particular importance, ROS can modulate Aβ deposition in AD by causing protein crosslinking (Mariani et al. 2005). It is also known that aggregation of Aβ stimulates the production of ROS (Tabner et al. 2005) and that antioxidant enzymes, such as those related to the glutathione antioxidant system, are affected by Aβ (Jhoo et al. 2004; Prediger et al. 2007). Our data show a significant increase in GR activity in the prefrontal cortex of mice on the 18th day after Aβ1–40 infusion and the pretreatment with atorvastatin reversed this increase. Conversely, Aβ1–40 infusion did not affect hippocampal GR activity at this time point, but the simultaneous treatment (atorvastatin plus Aβ) increased GR activity in this structure. Similarly, GPx activity also increased in the prefrontal cortex in response to Aβ1–40 infusion and the pretreatment with atorvastatin significantly blunted this increase. In the hipocampus, no significant effects were observed in GPx activity. Previous data from our group have shown an increase in GR activity in the prefrontal cortex of mice 24 h after the infusion of Aβ1–40 (Prediger et al. 2007). Our current finding shows that the increased cortical GR activity was still observed 18 days after Aβ1–40 infusion, suggesting a long-lasting response. Although the dissimilar effects of Aβ (and atorvastatin) toward hippocampal and cortico-cerebral glutathione-related enzymes suggest the likely occurrence of contrasting results, our findings corroborate literature data showing a differential modulation of these enzymes in both encephalic structures in response to different factors. Although the molecular mechanisms related to such differences between hippocampus and cerebral cortex are not yet understood, one might posit that the different neuronal constitution (referring not only to the different type of neurons, but also to the dissimilar receptors densities in a given neuronal type) likely contributes to the different responses observed. Furthermore, based on the critical role of astrocytes in maintaining the homeostasis of the antioxidant glutathione system in the central nervous system (Dringen and Hirrlinger 2003), the contribution of glial cells (Girardi et al. 2004) to the differential response in hippocampus and cerebral cortex cannot be ruled out.
It is noteworthy that both GPx and GR activities were increased in the prefrontal cortex of Aβ-treated mice and atorvastatin pretreatment abolished these increases. The simultaneous induction of both enzymes is an expected event since both enzymes are important to the detoxification of peroxides (Dringen et al. 2005). In fact, GR catalyzes the reduction of GSSG, which is generated when peroxides are reduced at the expense of reduced glutathione (GSH), in a reaction catalyzed by GPx. Evidence shows that up-regulation of GPx and GR occurs mostly via activation of the nuclear factor E2 p45-related factor 2 (Nrf2), which is stimulated under oxidant conditions (Thimmulappa et al. 2002). Nrf2 can activate transcription factors that interact with the antioxidant response element (ARE/EpRE) to initiate the transcription of target genes including GPx and GR (Itoh et al. 2003). Of note, genes with the ARE/EpRe sequence are induced by oxidants such as hydrogen peroxide (Rahman et al. 1996), whose production is stimulated by aggregated Aβ (Tabner et al. 2005). Based on the absence of Aβ-induced up-regulation of cortico-cerebral GPx and GR in animals pretreated with atorvastatin, one might suppose that this statin decreases the Aβ-induced production or increases the detoxification of ROS, which is in agreement with the pleiotropic effects of the statins (Barone et al. 2011; Butterfield et al. 2011).
In summary, we observed that i.c.v. Aβ1–40 infusion promotes cognitive impairments in mice subjected to OPR task, which was prevented by the pretreatment with atorvastatin. Glutamate uptake was reduced by Aβ1–40 or atorvastatin treatment. However, in the prefrontal cortex, Aβ1–40 increased Na+-independent glutamate uptake, an effect that deserves further investigation. The activity of AChE was not altered in any group indicating that the cholinergic system may be involved in later phases of the toxicity of Aβ1–40 peptide in our experimental protocol. Furthermore, we found that the Aβ1–40 causes an increase in GR and GPx activities in the prefrontal cortex of mice, both prevented by atorvastatin pretreatment. Therefore, atorvastatin pretreatment promoted an improvement in memory and learning deficits in mice undergoing infusion with Aβ1–40, which renders this drug as a promising molecule for further pharmacological studies on the search for therapeutic strategies to counteract the progression of AD.
Abbreviations
- Aβ:
-
Amyloid-β
- AD:
-
Alzheimer’s disease
- EAATs:
-
Excitatory aminoacids transporters
- GLAST, GLT-1:
-
Glial glutamate transporters
- GPx:
-
Glutathione peroxidase
- GR:
-
Glutathione reductase
- GSHt:
-
Total glutathione
- GSSG:
-
Oxidized glutathione
- HMG-CoA reductase:
-
3-Hydroxyl-3-methyl-glutaryl-coenzyme A reductase
- i.c.v.:
-
Intracerebroventricular
References
Aluise CD, Robinson RA, Beckett TL, Murphy MP, Cai J, Pierce WM, Markesbery WR, Butterfield DA (2010) Preclinical Alzheimer disease: brain oxidative stress, Abeta peptide and proteomics. Neurobiol Dis 39(2):221–228
Aoyama K, Suh SW, Hamby AM, Liu J, Chan WY, Chen Y, Swanson RA (2006) Neuronal glutathione deficiency and age-dependent neurodegeneration in the EAAC1 deficient mouse. Nat Neurosci 9(1):119–126
Auld DS, Kornecook TJ, Bastianetto S, Quirion R (2002) Alzheimer’s disease and the basal forebrain cholinergic system: relations to β-amyloid peptides, cognition, and treatment strategies. Prog Neurobiol 68:209–245
Barone E, Cenini G, Di Domenico F, Martin S, Sultana R, Mancuso C, Murphy MP, Head E, Butterfield DA (2011) Long-term high-dose atorvastatin decreases brain oxidative and nitrosative stress in a preclinical model of Alzheimer disease: a novel mechanism of action. Pharmacol Res 63(3):172–180
Bicca MA, Figueiredo CP, Piermartiri TC, Meotti FC, Bouzon ZL, Tasca CI, Medeiros R, Calixto JB (2011) The selective and competitive N-methyl-D-aspartate receptor antagonist, (-)-6-phosphonomethyl-deca-hydroisoquinoline-3-carboxylic acid, prevents synaptic toxicity induced by amyloid-β in mice. Neuroscience 192:631–641
Binder S, Baier PC, Mölle M, Inostroza M, Born J, Marshall L (2012) Sleep enhances memory consolidation in the hippocampus-dependent object-place recognition task in rats. Neurobiol Learn Mem 97(2):213–219
Butterfield DA, Lauderback CM (2002) Lipid peroxidation and protein oxidation in Alzheimer’s disease brain: potential causes and consequences involving amyloid-β-peptide associated free radical oxidative stress. Free Radic Biol Med 32:1050–1060
Butterfield DA, Barone E, Mancuso C (2011) Cholesterol-independent neuroprotective and neurotoxic activities of statins: perspectives for statin use in Alzheimer disease and other age-related neurodegenerative disorders. Pharmacol Res 64(3):180–186
Carlberg I, Mannervik B (1985) Glutathione reductase. Methods Enzymol 113:484–490
Cassano T, Serviddio G, Gaetani S, Romano A, Dipasquale P, Cianci S, Bellanti F, Laconca L, Romano AD, Padalino I, Laferla FM, Nicoletti F, Cuomo V, Vendemiale G (2012) Glutamatergic alterations and mitochondrial impairment in a murine model of Alzheimer disease. Neurobiol Aging 33(6):1121.e1–1121.e12
Davies P, Maloney AJ (1976) Selective loss of central cholinergic neurons in Alzheimer’s disease. Lancet 308(8000):1403
Davis KL, Mohs RC, Marin D, Purohit DP, Perl DP, Lantz M (1999) Cholinergic markers in elderly patients with early signs of Alzheimer’s disease. J Am Med Assoc 281:1401–1406
Dringen R, Hirrlinger J (2003) Glutathione pathways in the brain. Biol Chem 384(4):505–516
Dringen R, Pawlowski PG, Hirrlinger J (2005) Peroxide detoxification by brain cells. J Neurosci Res 79(1–2):157–165
El Khoury J, Hickman SE, Thomas CA, Cao L, Silverstein SC, Loike JD (1996) Scavenger receptor-mediated adhesion of microglia to beta-amyloid fibrils. Nature 382:716–719
Ellman GL, Courtney KD, Andres V Jr, Feather-Stone RM (1961) A new and rapid colorimetric determination of acetylcholinesterase activity. Biochem Pharmacol 7:88–95
García-Ayllón MS, Small DH, Avila J, Sáez-Valero J (2011) Revisiting the role of acetylcholinesterase in Alzheimer’s disease: cross-talk with P-tau and β-amyloid. Front Mol Neurosci 4(22):1–9
Girardi E, Ramos AJ, Vanore G, Brusco A (2004) Astrocytic response in hippocampus and cerebral cortex in an experimental epilepsy model. Neurochem Res 29(2):371–377
Grundke-Iqbal I (1986) Abnormal phosphorylation of the microtubule-associated protein tau (tau) in Alzheimer cytoskeletal pathology. Proc Natl Acad Sci USA 83:4913–4917
Haass C (2007) Soluble protein oligomers in neurodegeneration: lessons from the Alzheimer’s amyloid beta-peptide. Nat Rev Mol Cell Biol 8:101–112
Itoh K, Wakabayashi N, Katoh Y, Ishii T, O’Connor T, Yamamoto M (2003) Keap1 regulates both cytoplasmic-nuclear shuttling and degradation of Nrf2 in response to electrophiles. Genes Cells 8(4):379–391
Jhoo JH, Kim HC, Nabeshima T, Yamada K, Shin EJ, Jhoo WK, Kim W, Kang KS, Jo SA, Woo JI (2004) Beta-amyloid (1-42)-induced learning and memory deficits in mice: involvement of oxidative burdens in the hippocampus and cerebral cortex. Behav Brain Res 155(2):185–196
Jick H, Zornberg GL, Jick SS, Seshadri S, Drachman DA (2000) Statins and the risk of dementia. Lancet 356:1627–1631
Kurinami H, Sato N, Shinohara M, Takeuchi D, Takeda S, Shimamura M, Ogihara T, Morishita R (2008) Prevention of amyloid beta-induced memory impairment by fluvastatin, associated with the decrease in amyloid beta accumulation and oxidative stress in amyloid beta injection mouse model. Int J Mol Med 21(5):531–537
Lee J-K, Won J-S, Singh AK, Singh I (2008) Statin inhibits kainic acid-induced seizure and associated inflammation and hippocampal cell death. Neurosci Lett 440:260–264
Longenberger J, Shah ZA (2011) Simvastatin and other HMG-CoA reductase inhibitors on brain cholesterol levels in Alzheimer’s disease. Curr Alzheimer Res 8(4):434–442
Lowry OH, Rosebrough J, Farr AL, Randall RJ (1951) Protein measurement with the Folin phenol reagent. J Biol Chem 193:265–275
Mariani E, Polidori MC, Cherubini A, Mecocci P (2005) Oxidative stress in brain aging, neurodegenerative and vascular diseases: an overview. J Chromatogr B 827:65–75
Masters CL, Selkoe DJ (2012) Biochemistry of amyloid b-protein and amyloid deposits in Alzheimer disease. Cold Spring Harb Perspect Med. 2(6):a006262
Medeiros R, Prediger RD, Passos GF, Pandolfo P, Duarte FS, Franco JL, Dafre AL, Di Giunta G, Figueiredo CP, Takahashi RN, Campos MM, Calixto JB (2007) Connecting TNF-alpha signaling pathways to iNOS expression in a mouse model of Alzheimer’s disease: relevance for the behavioral and synaptic deficits induced by amyloid beta protein. J Neurosci 27(20):5394–5404
Molz S, Decker H, Oliveira IJL, Souza DO, Tasca CI (2005) Neurotoxicity induced by glutamate in glucose-deprived rat hippocampal slices is prevent by GMP. Neurochem Res 30:83–89
Nelson DL, Cox MM (2000) Lehninger principles of biochemistry, 3rd edn. Worth Publishers, New York, pp 799–814
Perry EK, Perry RH, Blessed G, Tomlinson BE (1977) Necropsy evidence of central cholinergic deficits in senile dementia. Lancet 1:189
Piermartiri TCB, Vandresen-Filho S, Herculano BA, Martins WC, Dal’agnolo D, Stroeh E, Carqueja CL, Boeck CR, Tasca CI (2009) Atorvastatin prevents Hippocampal cell death due to quinolinic acid-induced seizures in mice by increasing Akt phosphorylation and glutamate uptake. Neurotox Res 16(2):106–115
Piermartiri TCB, Figueiredo CP, Rial D, Duarte FS, Bezerra SC, Mancini G, De Bem AF, Prediger RDS, Tasca CI (2010) Atorvastatin prevents hippocampal cell death, neuroinflammation and oxidative stress following amyloid-β1-40 administration in mice: evidence for dissociation between cognitive deficits and neuronal damage. Exp Neurol 226(2):274–284
Prediger RD, Franco JL, Pandolfo P, Medeiros R, Duarte FS, Di Giunta G, Figueiredo CP, Farina M, Calixto JB, Takahashi RN, Dafre AL (2007) Differential susceptibility following beta-amyloid peptide-(1-40) administration in C57BL/6 and Swiss albino mice: Evidence for a dissociation between cognitive deficits and the glutathione system response. Behav Brain Res 177(2):205–213
Prediger RD, Medeiros R, Pandolfo P, Duarte FS, Passos GF, Pesquero JB, Campos MM, Calixto JB, Takahashi RN (2008) Genetic deletion or antagonism of kinin B(1) and B(2) receptors improves cognitive deficits in a mouse model of Alzheimer’s disease. Neuroscience 151(3):631–643
Rahman I, Bel A, Mulier B, Lawson MF, Harrison DJ, Macnee W, Smith CA (1996) Transcriptional regulation of gamma-glutamylcysteine synthetase-heavy subunit by oxidants in human alveolar epithelial cells. Biochem Biophys Res Commun 229(3):832–837
Sacchetta P, Di Cola D, Federlci G (1986) Alkaline hydrolysis of N-ethylmaleimide allows a rapid assay of glutathione disulfide in biological samples. Anal Biochem 154:205–208
Schachter M (2005) Chemical, pharmacokinetic and pharmacodynamic properties of statins: an update. Fundam Clin Pharmacol 19(1):117–125
Schaeffer EL, Gattaz WF (2008) Cholinergic and glutamatergic alterations beginning at the early stages of Alzheimer disease: participation of the phospholipase A2 enzyme. Psychopharmacology 198(1):1–27
Sultana R, Mecocci P, Mangialasche F, Cecchetti R, Baglioni M, Butterfield DA (2011) Increased protein and lipid oxidative damage in mitochondria isolated from lymphocytes from patients with Alzheimer’s disease: insights into the role of oxidative stress in Alzheimer’s disease and initial investigations into a potential biomarker for this dementing disorder. J Alzheimers Dis 24(1):77–84
Tabner BJ, El-Agnaf OM, Turnbull S, German MJ, Paleologou KE, Hayashi Y, Cooper LJ, Fullwood NJ, Allsop D (2005) Hydrogen peroxide is generated during the very early stages of aggregation of the amyloid peptides implicated in Alzheimer disease and familial British dementia. J Biol Chem 280(43):35789–35792
Takeda S, Sato N, Niisato K, Takeuchi D, Kurinami H, Shinohara M, Rakugi H, Kano M, Morishita R (2009) Validation of Aβ1–40 administration into mouse cerebroventricles as an animal model for Alzheimer disease. Brain Res 1280:137–147
Thimmulappa RK, Mai KH, Srisuma S, Kensler TW, Yamamoto M, Biswal S (2002) Identification of Nrf2-regulated genes induced by the chemopreventive agent sulforaphane by oligonucleotide microarray. Cancer Res 62(18):5196–5203
Tiraboschi P, Hansen LA, Alford M, Masliah E, Thal LJ, Corey-Bloom J (2000) The decline in synapses and cholinergic activity in asynchronous Alzheimer’s disease. Neurology 55:1278–1283
Tramontina AC, Wartchow KM, Rodrigues L, Biasibetti R, Quincozes-Santos A, Bobermin L, Tramontina F, Gonçalves CA (2011) The neuroprotective effect of two statins: simvastatin and pravastatin on a streptozotocin-induced model of Alzheimer’s disease in rats. J Neural Transm 118(11):1641–1649
Waters DD (2005) Safety of high-dose atorvastatin therapy. Am J Cardiol 96(5A):69–75
Wendel A (1981) Glutathione peroxidase. Methods Enzymol 77:325–333
Wolozin B, Kellman W, Ruosseau P, Celesia GG, Siegel G (2000) Decreased prevalence of Alzheimer disease associated with 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors. Arch Neurol 57:1439–1443
Acknowledgments
The research is supported by Grants from the Brazilian funding agencies: Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), Conselho de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), Financiadora de Estudos e Projetos – IBN-Net # 01.06.0842-00 (FINEP), and Instituto Nacional de Ciência e Tecnologia (INCT) for Excitotoxicity, and Neuroprotection. C.I.T., R.D.P. and M.F. are the recipients of CNPq productivity fellowship. W.C.M. is the recipient of CAPES Master scholarship and G.G.V. is the recipient of CAPES-PRODOC post-doctoral scholarship.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Martins, W.C., dos Santos, V.V., dos Santos, A.A. et al. Atorvastatin Prevents Cognitive Deficits Induced by Intracerebroventricular Amyloid-β1–40 Administration in Mice: Involvement of Glutamatergic and Antioxidant Systems. Neurotox Res 28, 32–42 (2015). https://doi.org/10.1007/s12640-015-9527-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12640-015-9527-y