Abstract
Embelia ribes is being used in Indian traditional herbal medicine for the treatment of mental disorders and as brain tonic. The present study was designed to investigate the protective effects of embelin from E. ribes on global ischemia/reperfusion-induced brain injury in rats. Transient global ischemia was induced by occluding bilateral common carotid arteries for 30 min followed by 24-h reperfusion. Neurological functions were measured using sensorimotor tests. Ischemia/reperfusion-induced neuronal injury was assessed by cerebral infarct area, biochemical and histopathological examination. Pretreatment of embelin (25 and 50 mg/kg, p.o.) significantly increased locomotor activity and hanging latency time and decreased beam walking latency when compared with ischemic control. The treatment also reduced significantly the lipid peroxidation and increased the total thiol content and glutathione-S-transferase activity in brain homogenates. The decreased cerebral infarction area in embelin-treated groups and histopathological observations confirmed the above findings. These observations suggested that embelin is a neuroprotective agent and may prove to be useful adjunct in the treatment of stroke.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Ischemic stroke accounts for 88% of all strokes and is associated with a high incidence of morbidity and mortality (Van der Worp and van Gijn 2007). Stroke has been ranked third most common cause of death worldwide and cerebrovascular diseases are considered second most frequent causes of deaths in the year 2020 (Huang and McNamara 2004). Hence, a major challenge that confronts medical researchers is the development of therapeutic agents, which prevent neuronal degeneration induced by ischemia, hypoxia and other traumatic insults to the CNS. Natural products probably represent an ideal source to develop safe and effective agents for the management of stroke and deserve scientific probe. Growing evidence supports the role of oxidative stress as one of the primary factors in brain injury mediated by cerebral ischemia and stroke (Landemmer and Harrison 2001). The brain is particularly vulnerable to oxidative stress because of its high rate of oxidative metabolic activity, intense production of reactive oxygen species (ROS) metabolites. ROS namely superoxide and hydroxyl free radicals, together with hydrogen peroxide have been proposed to cause neurotoxic effect and initiate a free radical-mediated chain reaction causing additional damage to diverse areas in the brain (Kondo et al. 1997). Therefore, oxidative injury could be one possible cellular cascade affecting all organs and tissues during ischemia.
Many antioxidants are reported to reduce ROS-mediated reactions and rescue neurons from ischemia/reperfusion-induced neuronal loss in animal models of cerebral ischemia (Gaur et al. 2009; Thiyagarajan and Sharma 2004).
Embelia ribes Burm. (Family: Myrsinaceae) is a medicinal plant used traditionally as anti-inflammatory to relieve rheumatism and fever (Kapoor et al. 1983). Its fruits are used as brain tonic, in the treatment of mental disorders, dyspnoea, diseases of the heart, etc. (Varier 2006). E. ribes is an important ingredient of a number of ayurvedic formulations in India (Pandey 1996; Vaidya-Arya 1999). Bhandari et al. (2002, 2007) have reported the dyslipidemic and antioxidant activity of ethanolic extract of E. ribes in streptozotocin-induced diabetes in rats. Its aqueous (Bhandari and Ansari 2008) and ethanolic extracts (Ansari and Bhandari 2008) were reported for their potent neuroprotective effects.
Embelin (2,5-dihydroxy-3-undecyl-1,4-benzoquinone, Fig. 1) is a naturally occurring alkyl substituted hydroxy benzoquinone and a major constituent from all the parts of E. ribes. Embelin reportedly possesses anti-inflammatory, analgesic (Chitra et al. 1994), antioxidant (Joshi et al. 2007), hepatoprotective (Dharmendra et al. 2009), wound healing (Kumara Swamy et al. 2009), antibacterial (Chitra et al. 2003), anticonvulsant (Mahendran et al. 2011) and antidiabetic (Mahendran et al. 2010) properties. Many quinones, thymoquinone (Al-Majed et al. 2006), idebenone (Nagaoka et al. 1989) and pyrroloquinoline quinine (Zhang et al. 2006) are known for their beneficial effects on cerebral ischemia. However, embelin has not been screened so far for its neuroprotective activity though the plant is traditionally used and scientifically proven as a neuroprotectant and antioxidant. Hence, in the present study we were interested to investigate the effect of embelin on transient global ischemia/reperfusion-induced neuronal damage in rats.
Materials and Methods
Isolation of Embelin from Embelia ribes
The berries of E. ribes were purchased from Abirami Botanicals, Tuticorin, Tamilnadu, India, and authenticated by Medicinal Plants Survey and Collection Unit, Ootacamund, Tamil Nadu, India, where a voucher specimen is preserved for further reference. Embelin was isolated according to our previously published protocol (Mahendran et al. 2011) and purity was matched with authentic sample.
Chemicals
1-Chloro-2,4-dinitrobenzene (CDNB) was obtained from Sigma–Aldrich, St. Louis, USA. Reduced glutathione (GSH), 5,5′-dithiobis-2-nitrobenzoic acid (DTNB), 2,3,5-triphenyltetrazolium chloride (TTC), thiobarbituric acid (TBA) and trichloroacetic acid (TCA) were purchased from Hi-Media Laboratories Pvt. Ltd., Mumbai, India. All the other chemicals used were of analytical grade.
Animals
Male Wistar rats (200–260 g) were obtained from the animal house of Sree Siddaganga College of Pharmacy, Tumkur, India, maintained under standard conditions (12 h light/dark cycle; 25 ± 3°C, 45–65% humidity) and had a free access to standard rat feed and water ad libitum. All the animals were acclimatized to laboratory conditions for a week before commencement of the experiment. The experiments were performed during the light portion between 08:00 and 12:00 am to avoid circadian influences. Animal studies were performed according to the prescribed guidelines of Committee for the Purpose of Control and Supervision of Experiments on Animals (CPCSEA), Government of India, India.
Preparation of Suspensions
Embelin was suspended in distilled water using Tween 80 (1% v/v). Two doses of embelin (25 and 50 mg/kg) were selected for administration by oral route based on our earlier study (Mahendran et al. 2010).
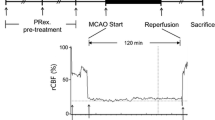
Ischemic Reperfusion Injury
Animals were divided into five groups of 6–10 rats each: Group I, sham-operated control received the vehicle (Tween 80, 1% v/v) (n = 6). Group II received embelin alone (50 mg/kg b.w.) and was subjected to sham operation (n = 8). Group III received vehicle and served as ischemic control (n = 10). Groups IV and V received embelin at 25 and 50 mg/kg b.w. (n = 10). All these treatments were given for 4 days orally by using oral gavage. On the fourth day, after 2 h of the above treatments, the animals of Groups III, IV and V were subjected to cerebral ischemia/reperfusion using the following procedure.
The animals were treated with atropine sulfate (0.5 mg/kg, i.p.) as preanesthetic medication and anesthetized with chloral hydrate (350 mg/kg, i.p.). Through a midline incision, a dissection was made between the sternocleidomastoid and the sternohyoid muscles parallel to the trachea and both common carotid arteries were exposed (Jingtao et al. 1999). Each carotid artery was freed from its adventitial sheath and vagus nerve, which were carefully separated and maintained. Ischemia was induced by occluding bilateral common carotid arteries (BCCA) with clamps for 30 min. Subsequently, both clamps were removed and both arteries were inspected for immediate reperfusion and the neck incision area was closed with stitches using suture. Sham control animals received the same surgical procedures, except the occlusion of BCCA. After 30 min of global ischemia, reperfusion was allowed for 24 h. After the completion of reperfusion period (24 h), the animals were assessed motor performance tests by the following neurological outcomes.
Locomotor Activity
The locomotor activity was recorded by using actophotometer (INCO Pvt. Ltd., Ambala, India). Before locomotor task, animals were placed individually in the activity meter for 2 min for habituation. Thereafter, locomotor activity was recorded using actophotometer for a period of 5 min (Kulkarni 1999).
Beam Walking Test
Beam walking test was used to evaluate gross vestibulomotor function. The apparatus consisted of a rod 120 cm in length and with a diameter of 2.3 cm. A wooden box (20 cm × 20 cm × 10 cm) was set at one end of the rod as a nest for motivating the animal to cross the beam. The apparatus was suspended 50 cm above a cushion, which protected the animals against fall injury. Rats were trained twice daily for 2 days before BCCA occlusion and assessed for motor coordination after 24 h of reperfusion. The time taken to traverse the beam was recorded. The cut-off time was taken as 120 s (Song et al. 2006; Yan et al. 2007).
Hanging Wire Test
This task was used to measure forelimb grip strength of the rats. In this test, animals were suspended by the forelimbs on a wire (45 cm long and 0.3 cm diameter) stretched between two posts 40 cm above a foam pillow. The time (s) until the animal fell was recorded. The cut-off time was taken as 90 s (Hunter et al. 2000).
Biochemical Estimations
After the motor performance tests, the animals (n = 4–8 from each group) were killed, brains were removed and homogenized in cold phosphate-buffered saline (10% w/v) and the suspension was centrifuged at 12000×g (Remi Motors Ltd., Mumbai, India) for 15 min at −4°C. The supernatant was used for the following biochemical analysis.
Measurement of Total Protein
The protein content of the brain homogenate was determined by Lowry’s method (Lowry et al. 1951) using bovine serum albumin as standard.
Measurement of Lipid Peroxidation
The extent of lipid peroxidation was measured by estimating the amount of malanodialdehyde (MDA) formed, as described by Akhtar et al. (2008). Briefly, to 0.1 ml homogenate, 1 ml of 10% (w/v) trichloroacetic acid (TCA) and 1 ml of 0.67% (w/v) thiobarbituric acid were added and placed in a boiling water bath for 30 min. Then the mixture was placed in crushed ice for 10 min followed by centrifugation at 4000×g for 10 min. The absorbance of the clear pink-colored supernatant was measured at 532 nm and the results were expressed as nmol MDA/mg protein.
Measurement of Total Thiols
The total thiol content was determined by the method described by Sedlak and Lindsay (1968), with slight modifications. To a mixture of 0.2 ml of homogenate and 0.36 ml of buffer, 0.04 ml of 10 mM DTNB and 1.5 ml of methanol were added and mixed well. The mixture was centrifuged at 1500×g for 5 min at −4°C. Then the intensity of the yellow color developed was measured at 412 nm and the results were expressed as nmol/mg protein.
Measurement of Glutathione-S-Transferase
Glutathione-S-transferase (GST) activity was measured as described by Habig et al. (1974). Briefly, 0.85 ml of Phosphate buffer (pH 7.4), 0.05 ml homogenate and 0.05 ml of 10 mM GSH were added, to which 0.05 ml of 1 mM CDNB was added to initiate the reaction. The rate of formation of GSH-CDNB complex was monitored for 5 min at 340 nm and the results were expressed as nmol of CDNB conjugate formed/min/mg protein.
Measurement of Brain Infarct Area
For the measurement of infarct area, two animals from each group were decapitated under deep anesthesia and the brains were removed and sliced coronally into 2-mm-thick sections, incubated in phosphate-buffered saline (pH 7.4) containing 2% of 2,3,5-triphenyltetrazolium chloride (TTC) for 30 min at 37°C and fixed in 10% neutral-buffered formalin overnight (Bederson et al. 1986; Fatehi-Hassanabad and Tasker 2011). The images of the stained sections were acquired using a high-resolution scanner, quantitatively analyzed by using Image J 1.43u software (NIH, USA) and expressed as a percentage of the total measured brain area.
Histopathological Studies
A section of the brain was fixed with 10% formalin, embedded in paraffin wax and cut into sections of 5-μm thickness. The sections were stained with hematoxylin and eosin dye for histopathological observations.
Statistical Analysis
The values were expressed as mean ± SEM. Statistical analysis was carried out by one-way analysis of variance (ANOVA) followed by Tukey post hoc test. P values <0.05 were considered as significant.
Results
Neurological Outcomes
In the sham control animals, the locomotor activity count and hanging latency time were found to be high and beam walking latency was low indicating the normal behavior of the animals. In the ischemic control animals, the locomotor activity and hanging latency time decreased significantly and beam walking latency was significantly increased indicating impairment of sensorimotor functions due to BCCA occlusion. The decrease in the locomotor count and hanging latency time was found to be 72.54 and 75.19%, respectively. Similarly, the increase in the beam walking latency was found to be 189.59%.
Pretreatment with different doses of embelin (25 and 50 mg/kg p.o.) for 4 days followed by ischemic reperfusion injury significantly increased (P < 0.05) the locomotor activity and hanging latency time and significantly decreased (P < 0.01) the beam walking latency periods towards the normal indicating the protective effect of embelin. The increase in the locomotor activity, hanging latency time and the decrease in beam walking latency when compared with ischemic control for the embelin 25 mg/kg treatment were found to be 200, 254.50 and 64.76%, respectively. These values for embelin 50 mg/kg treatment were found to be 260, 279.16 and 65.42%, respectively. Embelin 50 mg/kg pretreatment exhibited almost similar results to the sham control animals indicating complete reversal of ischemic damage. Embelin, when administered to sham-operated rats, showed slight reduction in the locomotor activity as well as hanging latency time. However, these were found to be insignificant indicating its safe nature (Table 1).
Biochemical Estimations
The level of MDA in BCCA occluded ischemic control rats was found to be 3.70 ± 0.42, a significant rise (P < 0.001) of about 141% when compared with 1.53 ± 0.07 of sham control animals. Pretreatment with embelin at 25 mg/kg followed by BCCA occlusion caused a significant reduction (P < 0.01) in the MDA levels to 1.85 ± 0.44 when compared with ischemic control animals. Embelin at 50 mg/kg significantly (P < 0.001) lowered this value to 0.75 ± 0.12, a value lower than the sham control indicating its potent neuroprotective effect (Fig. 2).
Ischemia for 30 min, significantly (P < 0.01) reduced the total thiol levels to 27.31 ± 1.15 compared with sham control (45.01 ± 4.95). The pretreatment with embelin at both the doses increased the total thiols to 37.54 ± 2.98 and 34.88 ± 3.60, respectively, when compared with ischemic control (Fig. 3). A significant reduction (P < 0.001) of around 51% in the GST activity was observed in ischemic control when compared with sham control. A significant increase (P < 0.001) in the enzyme level was found in the pretreatment of embelin at both the tested doses when compared with ischemic control. The increase is almost equivalent to sham control indicating the reversal of ischemic insult to normal levels (Fig. 4). However, the embelin-alone treatment caused a slight decrease in all the biochemical parameters which was non-significant.
Brain Infarct Area
The brain infarct area of ischemic control animals was found to be 21.08 ± 1.22%. The pretreatment with different doses of embelin at (25 and 50 mg/kg) significantly (P < 0.01) reduced the brain infarct area to 11.96 ± 0.19 and 8.61 ± 0.61%, respectively (Figs. 5, 6).
Histopathological Studies
The brain histology of sham control animal has showed normal appearance. Ischemic control animal brain exhibited increased glial density, presence of lymphocytes, edema, congested blood vessels and neuronal necrosis. The pretreatment with embelin at 25 mg/kg followed by ischemia showed increased glial density and edema, along with absence of lymphocytes, decreased congestion of blood vessels and neuronal necrosis. Embelin pretreatment at 50 mg/kg showed normal glial density, decreased edema, absence of lymphocytes, congestion of blood vessels and necrosis (Fig. 7).
Histopathological changes in brain of experimental rats. A, B Sham control and embelin alone, normal brain showing normal blood vessels and brain parenchyma. C Ischemic control showing congested blood vessels (a), neuronal necrosis (b) and increased lymphocyte infiltration. D Ischemia + embelin 25 mg/kg showing reduced congested blood vessels, lymphocytes and absence of necrosis. E Ischemia + embelin 50 mg/kg showing absence of necrosis and blood vessel congestion
Discussion
Bilateral common carotid artery (BCCA) occlusion is a well-known model used to study cerebral ischemia. BCCA occlusion causes reduction in blood flow to diverse regions of brain and contributes to associated behavioral and cognitive deficits (Tsuchiya et al. 1993; Martinez et al. 1997). In the present study, a significant decrease (72.54%) in locomotor activity and an increase (189.59%) in beam walking latency have been observed after ischemia reperfusion, which was reversed by embelin pretreatment (25 and 50 mg/kg p.o.) for 4 days. Similarly, global ischemia has been reported to cause significant decrease in grip and muscle strength of the limbs (Mukherjee et al. 2007; Rehni and Singh 2007). Consistent with this report, a significant increase in muscle strength and grip has been observed in embelin pretreatment at both the tested doses, suggesting the therapeutic potential of embelin against ischemic/reperfusion injury. A complete reversal of ischemic damage caused by BCCA occlusion was observed in animals pre-treated with higher dose of embelin.
Oxidative stress has been reported to play a major role in the ischemic reperfusion injury (Gaur et al. 2009; Al-majed et al. 2006; Nagaoka et al. 1989). The elevated MDA levels observed in the ischemic rats was significantly reduced in the embelin-pretreatment indicating its free radical scavenging effects. Ischemic injury to neurons depletes the total thiol content of the brain (Chandrashekhar et al. 2010). Rats pretreated with embelin at 25 and 50 mg/kg significantly increased the total thiol content when compared with ischemic rats. The pretreatment with embelin at both the doses restored the depleted GST activity in the brain homogenates induced by ischemia. These results are in agreement with the earlier reports of potent antioxidant activity of embelin (Dharmendra et al. 2009; Joshi et al. 2007).
TTC staining was used to assess the extent of cell death in brains subjected to ischemia/reperfusion (Fatehi-Hassanabad and Tasker 2011). The extent of infarction varies with different animal models of stroke. In the present study, approximately 20% of the total brain area was infarcted. This observation is consistent with an earlier report showing a relatively lesser (14–18%), but observable infarct area in global ischema/reperfusion-injured animals (Fatehi-Hassanabad and Tasker 2011). The pretreatment with embelin at both the doses showed comparatively less (9–12%) infarct lesion area indicating that embelin could protect the neurons from ischemic injury. The above results were further confirmed by histopathological studies, where the brain tissue of embelin-treated rats showed a reversal of the damage caused by ischemic reperfusion injury.
Hypoxic ischemic brain injury, carotid artery pathologies, asphyxiation and shock are a few age-related disorders seen frequently during cerebral ischemia (Gaur et al. 2009). Several plants including E. ribes and benzoquinone comprising phytochemicals exhibited potent neuroprotective effects and found to be useful in ischemia-related disorders (Bora and Sharma. 2010; Chandrashekhar et al. 2010; Ansari and Bhandari 2008; Al-Majed et al. 2006; Nagaoka et al. 1989; Zhang et al. 2006). Neuroprotection aimed at preventing ischemia/reperfusion injuries in transient global cerebral ischemia is an effective strategy in the treatment of stroke and related pathologies. Naringin, thymoquinone, idebenone and several other known antioxidants have shown protective effects against cerebral ischemia (Gaur et al. 2009; Al-majed et al. 2006; Nagaoka et al. 1989). The anticonvulsant effect of embelin in maximal electroshock and pentylenetetrazole-induced seizure was earlier reported by us (Mahendran et al. 2011). Several anticonvulsants have shown protection against ischemic/reperfusion-induced neuronal damage (Edmonds et al. 2001). Many benzoquinones are known to possess neuroprotective property in different animal models of ischemic brain injury (Al-Majed et al. 2006; Nagaoka et al. 1989; Zhang et al. 2006). Hence, these reports further supported the evidence of embelin having neuroprotective action.
In conclusion, embelin normalized the altered behavioral, biochemical and histopathological parameters in ischemic rats, suggesting the neuroprotective action of embelin. The possible mode of protection may be due its antioxidant and anticonvulsants properties. However, further research is warranted to elucidate the specific mechanism/s involved.
References
Akhtar M, Pillai KK, Vohora D (2008) Effect of thioperamide on oxidative stress markers in middle cerebral artery occlusion model of focal cerebral ischemia in rats. Hum Exp Toxicol 27:761–767
Al-Majed AA, Al-Omar FA, Nagi MN (2006) Neuroprotective effects of thymoquinone against transient forebrain ischemia in the rat hippocampus. Eur J Pharmacol 543:40–47
Ansari MN, Bhandari U (2008) Protective effect of Embelia ribes Burm on methionine induced hyperhomocysteinemia and oxidative stress in rat brain. Indian J Exp Biol 46:521–527
Bederson JB, Pitts LH, Germano SM, Nishimura MC, Davis RL, Bartkowski HM (1986) Evaluation of 2,3,5-triphenyltetrazolium chloride as a stain for detection and quantification of experimental cerebral infarction in rats. Stroke 17:1304–1308
Bhandari U, Ansari MN (2008) Protective effect of aqueous extract of Embelia ribes Burm fruits in middle cerebral artery occlusion-induced focal cerebral ischemia in rats. Indian J Pharmacol 40:215–220
Bhandari U, Kanojia R, Pillai KK (2002) Effect of ethanolic extract of Embelia ribes on dyslipidaemia in diabetic rats. Int J Exp Diab Res 3:159
Bhandari U, Jain N, Pillai KK (2007) Further studies on antioxidant potential and protection of pancreatic β-cells by Embelia ribes in experimental diabetes. Exp Diab Res 2007:1–6
Bora KS, Sharma A (2010) Neuroprotective effect of Artemisia absinthium L. on focal ischemia and reperfusion-induced cerebral injury. J Ethnopharmacol 129:403–409
Chandrashekhar VM, Ranpariya VL, Ganapaty S, Parashar A, Muchandi AA (2010) Neuroprotective activity of Matricaria recutita Linn against global model of ischemia in rats. J Ethnopharmacol 127:645–651
Chitra M, Sukumar E, Suja V, Devi CSS (1994) Antitumor, anti-inflammatory and analgesic property of embelin, a plant product. Chemotherapy 40:109–113
Chitra M, Devi CSS, Sukumar E (2003) Antibacterial activity of embelin. Fitoterapia 74:401–403
Dharmendra S, Ruchi S, Pahup S, Gupta RS (2009) Effect of embelin on lipid peroxidation and free radical scavenging activity against liver damage in rats. Basic Clin Pharmacol Toxicol 105:243–248
Edmonds HL, Jiang YD, Zhang Py, Shank R (2001) Topiramate as a neuroprotective in rat model of global ischemia-induced neurodegeneration. Life Sci 69:2265–2277
Fatehi-Hassanabad Z, Tasker RA (2011) Peroxisome proliferator-activated receptor-γ (PPAR-γ) activation confers functional neuroprotection in global ischemia. Neurotox Res 19:462–471 Epub 2010 Jun 4
Gaur V, Aggarwal A, Kumar A (2009) Protective effect of naringin against ischemic reperfusion cerebral injury: possible neurobehavioral, biochemical and cellular alterations in rat brain. Eur J Pharmacol 616:147–154
Habig WH, Pabst MJ, Jarkoby WB (1974) Glutathione S-transferases. The first enzymatic step in mercapturic acid formation. J Biol Chem 249:7130–7139
Huang Y, McNamara JO (2004) Ischemic stroke: acidotoxicity is a perpetrator. Cell 118:665–670
Hunter AJ, Hatcher J, Virley D, Nelson P, Irving E, Handubgham SJ et al (2000) Functional assessments in mice and rats after focal stroke. Neuropharmacology 39:806–816
Jingtao J, Sato S, Yamanaka N (1999) Changes in cerebral blood flow and blood–brain barrier in the gerbil hippocampal CA1 region following repeated brief cerebral ischemia. Med Electron Microsc 32:175–183
Joshi R, Kamat JP, Mukherjee T (2007) Free radical scavenging reactions and antioxidant activity of embelin: biochemical and pulse radiolytic studies. Chem Biol Interact 167:125–134
Kapoor VK, Chawla AS, Kumar M, Kumar P (1983) Anti-inflammatory agent in Indian laboratories. Indian Drugs 30:481–488
Kondo T, Reaume AG, Huang TT, Carlson E, Murakami K, Chen SF et al (1997) Reduction of CuZn-superoxide dismutase activity exacerbates neuronal cell injury and edema formation after transient focal cerebral ischemia. J Neurosci 17:4180–4189
Kulkarni SK (1999) Hand book of experimental pharmacology. Vallabh Prakashan, New Delhi, pp 117–119
Kumara Swamy HM, Krishna V, Shankarmurthy K, Abdul Rahiman B, Mankani KL, Mahadevan KM, Harish BG, Raja Naika H (2009) Wound healing activity of embelin isolated from the ethanol extract of leaves of Embelia ribes Burm. J Ethnopharmacol 109:529–534
Landemmer U, Harrison DG (2001) Oxidative stress and vascular damage in hypertension. Coronary Artery Dis 12:455–461
Lowry OH, Rosebrough NJ, Farr AL, Randal RJ (1951) Protein measurement with the Folin phenol reagent. J Biol Chem 193:265–275
Mahendran S, Maithili V, Badami S (2010) Evaluation of antidiabetic effect of embelin from Embelia ribes in alloxan induced diabetes in rats. Biomed Pharmacother; Epub 2010 Sep 20
Mahendran S, Thippeswamy BS, Veerapur VP, Badami S (2011) Anticonvulsant activity of embelin isolated from Embelia ribes. Phytomedicine 18:186–188
Martinez G, Di Giacomo C, Carnazza ML (1997) MAP2 synaptophysin immunostaining in rat brain and behavioral modifications after cerebral postischemic reperfusion. Dev Neurosci 19:457–464
Mukherjee PK, Ahamed KN, Kumar V, Mukherjee K, Houghton PJ (2007) Protective effect of biflavones from Araucaria bidwillii Hook in rat cerebral ischemia/reperfusion induced oxidative stress. Behav Brain Res 178:221–228
Nagaoka A, Suno M, Shibota M, Kakihana M (1989) Effects of idebenone on neurological deficits, local cerebral blood flow, and energy metabolism in rats with experimental cerebral ischemia. Arch Gerontol Geriatr 8:193–202
Pandey VN (1996) Pharmacological investigation of certain medicinal plants and compound formulations used in Ayurveda and Siddha. Central Council for Research in Ayurveda and Siddha, Yugantar Press, New Delhi, pp 370–376
Rehni AK, Singh N (2007) Role of phosphoinositide 3-kinase in ischemic postconditioning-induced attenuation of cerebral ischemia-evoked behavioral deficits in mice. Pharmacol Rep 59:192–198
Sedlak J, Lindsay R (1968) Estimation of total, protein-bound, and nonprotein sulfhydryl groups in tissue with Ellman’s reagent. Anal Biochem 25:192–205
Song YN, Li HZ, Zhu JN, Guo CL, Wang JJ (2006) Histamine improves rat rota-rod and balance beam performances through H2 receptors in the cerebellar interpositus nucleus. Neuroscience 140:33–43
Thiyagarajan M, Sharma SS (2004) Neuroprotective effect of curcumin in middle cerebral artery occlusion induced focal cerebral ischemia in rats. Life Sci 74:969–985
Tsuchiya M, Sako K, Yura S, Yonemasu Y (1993) Local cerebral glucose utilization following acute and chronic bilateral carotid artery ligation in Wistar rats: relation to changes in local cerebral blood flow. Exp Brain Res 95:1–7
Vaidya-Arya MR (1999) Sthaulya Cikitsa (treatment of obesity). In: A compendium of ayurvedic medicine, principles and practice. Sri Satyaguru Publication: A Division of Indian Book Centre, New Delhi, pp 335–339
Van der Worp HB, van Gijn J (2007) Clinical practice. Acute ischemic stroke. New Eng J Med 357:572–579
Varier PS (2006) Indian medicinal plants, a compendium of 500 species, vol 2. Orient Longman (Pvt) Ltd, Chennai, pp 368–371
Yan X, Wang S, Hou H, Ji R, Zhou J (2007) Lithium improves the behavioral disorder in rats subjected to transient global cerebral ischemia. Behav Brain Res 177:282–289
Zhang Y, Feustel PJ, Kimelberg HK (2006) Neuroprotection by pyrroloquinoline quinine (PQQ) in reversible middle cerebral artery occlusion in the adult rat. Brain Res 1094:200–206
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Thippeswamy, B.S., Nagakannan, P., Shivasharan, B.D. et al. Protective Effect of Embelin from Embelia ribes Burm. Against Transient Global Ischemia-Induced Brain Damage in Rats. Neurotox Res 20, 379–386 (2011). https://doi.org/10.1007/s12640-011-9258-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12640-011-9258-7