Abstract
Purpose
Tranexamic acid (TXA) reduces red blood cell transfusion in various orthopedic surgeries, yet the degree of practice variation in its use among anesthesiologists and surgeons has not been described. To target future knowledge transfer and implementation strategies, and to better understand determinants of variability in prophylactic TXA use, our primary objective was to evaluate the influence of surgical team members on the variability of prophylactic TXA administration.
Methods
This was a retrospective cohort study of all adult patients undergoing primary total hip arthroplasty (THA), hip fracture surgery, and spine fusion ± vertebrectomy at two Canadian hospitals between January 2014 and December 2016. We used Canadian Classification of Health Interventions procedure codes within the Discharge Abstract Database which we linked to the Ottawa Data Warehouse. We described the percentage of patients that received TXA by individual surgery, the specifics of TXA dosing, and estimated the effect of anesthesiologists and surgeons on prophylactic TXA using multivariable mixed-effects logistic regression analyses.
Results
In the 3,900 patients studied, TXA was most commonly used in primary THA (85%; n = 1,344/1,582), with lower use in hip fracture (23%; n = 342/1,506) and spine fusion surgery (23%; n = 186/812). The median [interquartile range] total TXA dose was 1,000 [1,000–1,000] mg, given as a bolus in 92% of cases. Anesthesiologists and surgeons added significant variability to the odds of receiving TXA in hip fracture surgery and spine fusion, but not primary THA. Most of the variability in TXA use was attributed to patient and other factors.
Conclusion
We confirmed the routine use of TXA in primary THA, while observing lower utilization with more variability in hip fracture and spine fusion surgery. Further study is warranted to understand variations in use and the barriers to TXA implementation in a broader population of orthopedic surgical patients at high risk for transfusion.
Résumé
Objectif
L’acide tranexamique (ATX) réduit la transfusion d’érythrocytes dans diverses chirurgies orthopédiques. Cependant, les variations de pratique quant à son utilisation parmi les anesthésiologistes et les chirurgiens n’ont pas été décrites. Afin de cibler les stratégies futures de transfert des connaissances et de mise en œuvre, et pour mieux comprendre les déterminants de la variabilité dans l’utilisation prophylactique d’ATX, notre objectif principal était d’évaluer l’influence des membres de l’équipe chirurgicale sur la variabilité de l’administration prophylactique d’ATX.
Méthode
Il s’agissait d’une étude de cohorte rétrospective de tous les patients adultes subissant une arthroplastie totale primaire de la hanche (ATH), une chirurgie de fracture de la hanche et une fusion intervertébrale ± vertébrectomie dans deux hôpitaux canadiens entre janvier 2014 et décembre 2016. Nous avons utilisé les codes de procédure de la Classification canadienne des interventions en santé dans la Base de données sur les congés des patients, que nous avons liée à la banque de données d’Ottawa. Nous avons décrit le pourcentage de patients qui ont reçu de l’ATX par chirurgie individuelle, les détails du dosage de l’ATX, et avons estimé l’effet des anesthésiologistes et des chirurgiens sur l’ATX prophylactique en réalisant des analyses de régression logistique multivariées à effets mixtes.
Résultats
Parmi les 3900 patients étudiés, l’ATX était le plus fréquemment utilisé lors d’une ATH primaire (85 %; n = 1344/1582), avec une utilisation plus faible lors de chirurgie de fracture de la hanche (23 %; n = 342/1506) et de chirurgie de fusion intervertébrale (23 %; n = 186/812). La dose totale médiane [écart interquartile] d’ATX était de 1000 mg [1000 à 1000], administrés dans 92 % des cas sous forme de bolus. Les anesthésiologistes et les chirurgiens ont ajouté une variabilité significative aux probabilités de recevoir de l’ATX lors d’une chirurgie de fracture de la hanche et de fusion, mais pas lors d’ATH primaire. La majeure partie de la variabilité dans l’utilisation d’ATX était attribuable aux facteurs liés au patient et à d’autres facteurs.
Conclusion
Nous avons confirmé l’utilisation de routine de l’ATX dans l’ATH primaire, tout en observant une utilisation moins répandue et plus variable lors de chirurgie de fracture de la hanche et de fusion intervertébrale. Une étude plus approfondie est nécessaire pour comprendre les variations d’utilisation et les obstacles à la mise en œuvre de l’ATX dans une population plus étendue de patients de chirurgie orthopédique à haut risque de transfusion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Red blood cell (RBC) transfusion rates among orthopedic surgeries vary widely, with lower rates among hip arthroplasty and higher rates in hip fracture and complex spine surgery.1,2,3,4 Strategies to mitigate perioperative RBC transfusion include preoperative correction of anemia, variation in surgical technique, intraoperative blood salvage, restrictive transfusion thresholds, and medications such as tranexamic acid (TXA).5,6,7
Tranexamic acid is an inexpensive and widely available medication that reversibly blocks lysine binding sites on plasminogen inhibiting plasmin formation and consequent fibrinolysis.8 Tranexamic acid has been shown to consistently reduce RBC transfusion in cardiac surgery, hip and knee arthroplasty, and trauma, where it is now incorporated into standard of care.5,9,10,11,12 Recent evidence syntheses suggest that TXA is effective in reducing transfusion in hip fracture surgery13,14,15 and spine surgery.16,17 In a recent meta-analysis evaluating a broader surgical population at high risk for RBC transfusion, TXA reduced the percentage of patients receiving transfused RBCs as well as the volume of transfused RBCs compared with placebo or usual care.18
Despite guidelines supporting the utilization of TXA to reduce transfusion in surgeries at increased risk for bleeding, real-world TXA use in orthopedic surgery has not been well described nor has the degree of practice variation in its use between anesthesiologists and surgeons.6 We studied how TXA use varies across orthopedic surgeries, and the influence of surgical team members on this variability. Understanding these determinants of practice variability will help inform and target future knowledge transfer and implementation strategies.
Methods
Study design, setting, and population
We completed a retrospective cohort study of all adult patients (≥ 18 yr of age) undergoing primary total hip arthroplasty (THA), hip fracture surgery, and spine fusion ± vertebrectomy at two hospitals in Ottawa, Ontario (Ottawa Hospital, Civic and General Campuses) between 1 January 2014 and 31 December 2016. These hospitals are tertiary care centres providing health services to approximately 1 million people. A formal policy or institutional guideline specific to TXA administration did not exist during the study period, nor was TXA stocked in the operating rooms. These orthopedic surgeries were chosen because they are high frequency surgeries (n > 150 per year) with higher rates of RBC transfusion (> 5%) and TXA utilization (> 10%) within the cohort.19 To prevent misclassification of surgery-specific rates of TXA utilization, we excluded patients with more than one surgery during their hospitalization. If a patient was re-admitted for another surgery during the study period (2014–2016), we evaluated only their initial hospital admission (Fig. 1).
Data sources
We obtained patient demographics, clinical, and administrative hospitalization data from the Discharge Abstract Database (DAD). The DAD uses standard International Classification of Diseases (ICD) coding for diagnoses and comorbidities, and Canadian Classification of Health Interventions (CCI) coding for surgical procedures. The DAD undergoes a continual process of data quality assurance and data validation.20 Transfusion, laboratory, and TXA data were obtained from the Ottawa Hospital Data Warehouse, which is a repository of clinical, laboratory, and health services information collected from the hospital’s information systems from both study institutions. Within the Ottawa Hospital Data Warehouse, TXA data were sourced from the Surgical Information Management System, a perioperative medical record which represents the medicolegal record for all surgical cases and is the gold standard for perioperative medication administration.
Study variables
We obtained patient demographics including age, sex, baseline comorbidities, most responsible diagnosis, and preoperative hemoglobin. Baseline comorbidities were evaluated using the Charlson comorbidity index.21 For the preoperative hemoglobin, we obtained the value drawn closest to the start of surgery, within the preceding four weeks. Surgical information, including type of procedure, date/time, surgical urgency (i.e., elective, urgent/emergent), and surgical team members (anesthesiologist, surgeon), was obtained from the DAD using standardized CCI procedure codes.22,23 The most responsible anesthesiologist was the anesthesiologist who started the surgical case. CCI procedure codes and ICD-10 diagnosis codes were used to define the orthopedic surgeries (eAppendix 1, Electronic Supplementary Material [ESM]).19 Total hip arthroplasty for osteoarthritis was evaluated separately, whereas THA for hip fracture was included in the hip fracture surgery group. Hip fracture surgery comprised THA (for hip fracture), hip hemiarthroplasty, and hip open reduction internal fixation (ORIF). To reflect transfusions attributable to perioperative bleeding, surgery-specific transfusion rates were defined based on RBC transfusions from the start of the surgery to seven days postoperative or hospital discharge, whichever occurred first. Prophylactic TXA administration was defined as intravenous TXA initiated within one hour before or after the start of surgery, with the intent to exclude cases where TXA was administered in response to surgical bleeding. Only prophylactic intravenous TXA use is considered in this paper.
Descriptive analysis of prophylactic TXA use
We described the percentage of patients who received intraoperative TXA by individual surgery, as well as specifics of TXA dosing (mg·kg−1·hr−1 and mg·hr−1) and administration. Baseline characteristics were summarized as means (standard deviation [SD]), medians [interquartile range (IQR)], or frequency (percent). We analyzed group differences in categorical or continuous data using Chi square and t tests. P values < 0.05 were considered significant. Sample sizes were not calculated as the primary intent of this analysis was descriptive, and the cohort was derived by convenience sampling. A data analysis and statistical plan was written and filed with our institutional review board before data were accessed.
Statistical analysis: evaluating the impact of surgical team members on variability of TXA administration
To estimate the effect of anesthesiologists and surgeons on prophylactic TXA utilization, we performed separate multivariable mixed-effects logistic regression analyses for primary THA, hip fracture surgery, and spinal fusion ± vertebrectomy. Our exposure of interest was the anesthesiologist and surgeon; the outcome was the administration of TXA. To account for patient and surgical risk, we adjusted for patient age, sex, comorbidities, preoperative hemoglobin, surgical urgency, hospital, and year. Patient age and preoperative hemoglobin were modelled using restricted cubic splines with five knots to allow for possible non-linear associations.24,25 For hip fracture surgery, the model was adjusted for the specific surgery subtypes, including THA (in patients with a diagnosis of hip fracture), hip hemiarthroplasty, and hip ORIF. Models were restricted to patients with data available for all covariates.
The exposures of interest, the anesthesiologist and surgeon, were included as random effects.26 The specific anesthesiologists and surgeons were considered randomly chosen exemplars from a hypothetical and infinite population of such practitioners. Rather than having a separate coefficient representing the association of TXA use with each specific individual (fixed effects), our mixed-effects model computes the spread, separately, across the hypothetical population of anesthesiologists and surgeons. Thus, the variance components express how widely TXA use ranges across anesthesiologists and across surgeons. To assess which of the two groups of practitioners account for more variation in TXA use, their variance components can be directly compared in magnitude.
To characterize the relative contributions of anesthesiologists, surgeons, and patient-level factors on variation in TXA administration, we used the random intercepts to calculate the variance partition coefficient (VPC) and the median odds ratio (OR) for the receipt of TXA.27 The VPC characterizes the proportion of variation attributable to the anesthesiologists, surgeons, patient factors, and other factors, and was calculated using the linear threshold model method. We used modified Wald P values to test if the variance was significantly different from zero.28 The median OR is a standardized measure of the variability in the odds of TXA use among surgeons or anesthesiologists. It represents the median amount by which the odds of TXA administration would change given two different anesthesiologists (or surgeons), one with a higher probability of TXA use, and one with a lower probability of TXA use. For example, a median OR of 1.75 suggests that the odds of TXA use is increased 1.75-fold (75% increase) when comparing two anesthesiologists on the same surgical case (same patient, same surgeon). Similarly, a median OR of 1.15 for anesthesiologists would mean that changing the anesthesiologist would typically result in a 15% increase in the odds of receiving TXA (same patient, same surgeon).
To more clearly illustrate how widely TXA use varies by anesthesiologist and surgeon, we plotted practitioner-specific estimated rates of TXA use for a hypothetical but typical patient, whose fixed effects covariate values were set to the mean or mode (for continuous or categorical variables) over the surgery-specific population. To examine anesthesiologists, we set the surgeon to the surgeon with the median predicted likelihood of TXA use; for surgeons, we used the median anesthesiologist. We then plotted these predicted likelihoods using a box-and-whisker plot.
Sensitivity analyses
As missing data were primarily limited to preoperative hemoglobin, the logistic regression models were performed using both single and multiple imputation for missing preoperative hemoglobin values. We performed single imputations assuming the missing hemoglobin values were: (a) the population mean, and (b) normal (120 g·L−1 for females, and 140 g·L−1 for males). To increase the generalizability of our findings, we conducted a separate logistic regression analysis that included all orthopedic and spine surgeries with TXA administration > 10%.
We conducted all analyses using SAS/STAT software (SAS version 9.4 for Windows; SAS Institute Inc., Cary, NC, USA). Multilevel models were specified and analyzed using the SAS command PROC GLIMMIX (SAS version 9.4 for Windows; SAS Institute Inc., Cary, NC, USA).
Results
Baseline characteristics
In two hospitals, we identified 3,900 patients undergoing primary THA, hip fracture surgery, or spine fusion ± vertebrectomy. Surgical urgency varied by surgery type; most THAs (98%) and spine fusion ± vertebrectomies (74%) were elective, whereas all hip fracture surgeries were urgent/emergent. The mean (SD) patient age was 68 (16) yr and 55% of patients were female. Preoperative hemoglobin values were available in 89% of the cohort; other study variables had near complete (> 99%) capture. Baseline demographics classified by surgery type are included in Table 1.
Overall, there were 121 anesthesiologists and 45 surgeons. Most physicians worked exclusively at one hospital (72% of anesthesiologists; 67% of surgeons). Among the primary THAs, there were 105 anesthesiologists and 16 surgeons. Among the hip fracture surgeries, there were 107 anesthesiologists and 37 surgeons. Among the spine fusion ± vertebrectomies, there were 72 anesthesiologists and 14 surgeons.
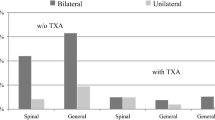
Description of prophylactic TXA use
The overall rate of prophylactic TXA administration was 48% (n = 1,872/3,900). Prophylactic TXA was administered preoperatively in 2% of patients (n = 44/1,872), with a mean (SD) administration time of 10 (12) min prior to surgery start. Tranexamic acid was administered intraoperatively in 98% of patients (n = 1,828/1,872), with a mean (SD) administration time of 28 (14) min after surgery start. Tranexamic acid was administered as an isolated bolus in 92% (n = 1,714/1,872), as an infusion in 2% (n = 31/1,872), and as a combined bolus and infusion in 7% (n = 127/1,872) of cases. Overall, the median [IQR] cumulative TXA dose was 1,000 [1,000–1,000] mg. Tranexamic acid use was most common in primary THA (n = 1,344/1,582; 85%), with lower utilization in hip fracture surgery (n = 342/1,506; 23%) and spine fusion ± vertebrectomy (n=186/812; 23%) (Table 1). Surgery-specific patient demographics are included in eAppendix 2 (ESM).
Evaluation of variability in prophylactic TXA administration by surgical team members
In our multivariable mixed-effects logistic regression models, anesthesiologists and surgeons added significant variability to the odds of receiving TXA in hip fracture surgery and spine fusion ± vertebrectomy, but not THA (eAppendices 3–6 [ESM]). In THA where TXA use is high, the variability of TXA use among anesthesiologists and surgeons was low. Conversely, in hip fracture surgery and spine fusion ± vertebrectomy where TXA use is lower, the variability in TXA use among anesthesiologists and surgeons was higher.
Among patients undergoing THA, most of the variation could be attributed to patient and other factors (VPC 92%), with some to anesthesiologists (6%), and less to surgeons (2%) (Fig. 2). The median OR for TXA administration was 1.6 among anesthesiologists and 1.3 among surgeons (Fig. 3). This means that for a given patient, their median odds of receiving TXA would differ by 1.6-fold depending on the anesthesiologist they receive care from, and by approximately 1.3-fold depending on the surgeon who performs their surgery. Among patients undergoing hip fracture surgery, 12% of the variation in TXA use was attributable to the anesthesiologist, 10% to the surgeon, and 78% to patient and other factors. The median OR for TXA administration was 2.0 among anesthesiologists and 1.8 among surgeons performing hip fracture surgery. Lastly, among patients undergoing spinal fusion ± vertebrectomy, 19% of the variation in TXA use was attributable to the anesthesiologist, 13% to the surgeon, and 68% to patient-specific factors. The median OR for TXA use was 2.5 among anesthesiologists and 2.1 among surgeons performing spinal fusion ± vertebrectomy.
Median odds ratios (OR) of TXA administration for primary THA, hip fracture surgery and spine fusion ± vertebrectomy. The median OR is a standardized measure of the variability in the odds of TXA use among surgeons or anesthesiologists. It represents the median amount by which the odds of TXA administration would change given two different anesthesiologists (or surgeons), one with a higher probability of TXA use, and one with a lower probability of TXA use. TXA = tranexamic acid
Practitioner-specific estimated rates of TXA use for a hypothetical but typical patient undergoing each of the three surgeries are included in Fig. 4. For a typical THA patient, the likelihood of TXA use varied by anesthesiologist with a median [IQR] predicted probability of 0.84 [0.82–0.85], and by surgeon with a median [IQR] predicted probability of 0.85 [0.84–0.85] (Fig. 4). For a typical hip fracture surgery patient, the likelihood of TXA use varied by anesthesiologist with a median [IQR] predicted probability of 0.30 [0.26-0.37], and by surgeon with a median [IQR] predicted probability of 0.30 [0.27–0.36]. Lastly, for a typical spine fusion patient, the likelihood of TXA use varied by anesthesiologist with a median [IQR] predicted probability of 0.16 [0.13–0.24], whereas the likelihood of TXA use varied by surgeon with a median [IQR] predicted probability of 0.14 [0.12–0.20].
Practitioner-specific estimated rates of TXA use for a hypothetical, but typical patient, whose fixed effects covariate values were set to the mean or mode (for continuous or categorical variables) over the surgery-specific population. To examine anesthesiologists, we set the surgeon to the surgeon with the median predicted probability of TXA use; for surgeons, we used the median anesthesiologist. TXA = tranexamic acid
The variability among surgical team members was consistent when the models were run with imputation of preoperative hemoglobin, and when the impact of anesthesiologist and surgeon were evaluated in a broader population of orthopedic and spine surgeries. As a post-hoc sensitivity analysis, model estimates did not appreciably change when we excluded care providers who worked at both the General and Civic campuses.
Discussion
In our cohort, TXA use was highest in primary THA, with lower utilization in hip fracture surgery and spine fusion ± vertebrectomy. Most of the variability was related to patient and other factors. There was little variability in TXA use among anesthesiologists and surgeons in primary THA, with more substantial practice variability in the other two surgeries.
The high utilization (85%) and low variability of TXA use in THA reflects the substantial evidence supporting TXA efficacy and cost-effectiveness in this surgery.9,29,30 As most of the variability in TXA use was related to patient and other factors, this could appropriately reflect risk-adapted clinical decision-making based on differing patient characteristics. Overall, this suggests the supportive recommendations for routine TXA use from multiple American orthopedic society guidelines have been effectively translated into clinical practice and incorporated into standard of care.31
In hip fracture and spine fusion surgeries, lower utilization and substantial variability in TXA use among surgical team members could reflect explicit anesthesiologist or surgeon preference for TXA administration, variations in surgical technique between surgeons, or the surgeon-specific case composition. Recently, randomized data have been published supporting the ability of TXA to reduce RBC transfusion in hip fracture13,14,15,32 and complex spine surgeries,18,33,34 although the certainty surrounding safety (i.e., thrombosis) is less clear. The underreporting of thrombotic complications and limited durations of follow-up in trials may have underestimated the true incidence of thromboembolic complications in an elderly population at particularly increased risk.18 Future randomized trials powered for important safety endpoints are needed prior to routine adoption.
Strengths of our study include the use of high-fidelity data sets that reliably capture patient demographics, surgical information, and TXA administration across a healthcare system that cares for more than 1 million people. We have addressed a knowledge gap by describing not only the rates of TXA use across different orthopedic surgeries but also how the use varies across surgical team members. To the best of our knowledge, this has never been previously reported.
Limitations of this study include the incomplete ascertainment of preoperative hemoglobin, which could be related to perioperative guidelines that advocate for reduced routine bloodwork prior to surgery.35 To further understand the impact of this missing data, sensitivity analyses were planned a priori and performed with various imputation techniques, none of which significantly altered the results. We evaluated variability in TXA use among care providers from 2014 to 2016, which may not reflect recent TXA utilization practices. We were unable to evaluate the impact practitioner characteristics and training, nor the potential impact of trainees on TXA administration. Topical TXA was not explicitly captured, although this reflects institutional practice as topical administration was uncommonly used, if at all, during the study period. Though representative of a large referral population, our logistic regression models were limited to two Ottawa hospitals; an expanded evaluation of TXA utilization in additional centres could be beneficial.
In our cohort, prophylactic TXA was routinely used in primary THA, with little variation in use by anesthesiologists and surgeons. In hip fracture surgery and spine fusion, the prophylactic use of TXA was lower and more variable. Further study is warranted to understand the determinants of TXA practice variation and barriers to TXA implementation in a broader population of orthopedic surgical patients at high risk for RBC transfusion.
References
Verlicchi F, Desalvo F, Zanotti G, Morotti L, Tomasini I. Red cell transfusion in orthopaedic surgery: a benchmark study performed combining data from different data sources. Blood Transfus 2011; 9: 383-7.
Mitchell MD, Betesh JS, Ahn J, Hume EL, Mehta S, Umscheid CA. Transfusion thresholds for major orthopedic surgery: a systematic review and meta-analysis. J Arthroplasty 2017; 32: 3815-21.
Vuille-Lessard E, Boudreault D, Girard F, Ruel M, Chagnon M, Hardy JF. Red blood cell transfusion practice in elective orthopedic surgery: a multicenter cohort study. Transfusion 2010; 50: 2117-24.
Ponnusamy KE, Kim TJ, Khanuja HS. Perioperative blood transfusions in orthopaedic surgery. J Bone Joint Surg Am 2014; 96: 1836-44.
Ferraris VA, Brown JR, Despotis GJ, et al. 2011 update to the Society of Thoracic Surgeons and the Society of Cardiovascular Anesthesiologists blood conservation clinical practice guidelines. Ann Thorac Surg 2011; 91: 944-82.
American Society of Anesthesiologists Task Force on Perioperative Blood Management. Practice guidelines for perioperative blood management: an updated report by the American Society of Anesthesiologists Task Force on Perioperative Blood Management. Anesthesiology 2015; 122: 241-75.
Freedman J. The ONTraC Ontario program in blood conservation. Transfus Apher Sci 2014; 50: 32-6.
Levy JH, Koster A, Quinones QJ, Milling TJ, Key NS. Antifibrinolytic therapy and perioperative considerations. Anesthesiology 2018; 128: 657-70.
Moskal JT, Capps SG. Meta-analysis of intravenous tranexamic acid in primary total hip arthroplasty. Orthopedics 2016; 39: e883-92.
He P, Zhang Z, Li Y, Xu D, Wang H. Efficacy and safety of tranexamic acid in bilateral total knee replacement: a meta-analysis and systematic review. Med Sci Monit 2015; 21: 3634-42.
Shakur H, Roberts I, Bautista R, et al. Effects of tranexamic acid on death, vascular occlusive events, and blood transfusion in trauma patients with significant haemorrhage (CRASH-2): a randomised, placebo-controlled trial. Lancet 2010; 376: 23-32.
Landoni G, Lomivorotov V, Silvetti S, et al. Nonsurgical strategies to reduce mortality in patients undergoing cardiac surgery: an updated consensus process. J Cardiothorac Vasc Anesth 2018; 32: 225-35.
Xiao C, Zhang S, Long N, Yu W, Jiang Y. Is intravenous tranexamic acid effective and safe during hip fracture surgery? An updated meta-analysis of randomized controlled trials. Arch Orthop Trauma Surg 2019; 139: 893-902.
Zhang P, He J, Fang Y, Chen P, Liang Y, Wang J. Efficacy and safety of intravenous tranexamic acid administration in patients undergoing hip fracture surgery for hemostasis: a meta-analysis. Medicine (Baltimore) 2017; https://doi.org/10.1097/MD.0000000000006940.
Farrow LS, Smith TO, Ashcroft GP, Myint PK. A systematic review of tranexamic acid in hip fracture surgery. Br J Clin Pharmacol 2016; 82: 1458-70.
Li G, Sun TW, Luo G, Zhang C. Efficacy of antifibrinolytic agents on surgical bleeding and transfusion requirements in spine surgery: a meta-analysis. Eur Spine J 2017; 26: 140-54.
Winter SF, Santaguida C, Wong J, Fehlings MG. Systemic and topical use of tranexamic acid in spinal surgery: a systematic review. Global Spine J 2016; 6: 284-95.
Houston BL, Uminski K, Mutter T, et al. Efficacy and safety of tranexamic acid in major non-cardiac surgeries at high risk for transfusion: a systematic review and meta-analysis. Transfus Med Rev 2020; 34: 51-62.
Houston BL, Fergusson DA, Falk J, et al. Evaluation of transfusion practices in noncardiac surgeries at high risk for red blood cell transfusion: a retrospective cohort study. Transfus Med Rev 2020; https://doi.org/10.1016/j.tmrv.2020.08.001.
Juurlink D, Preyra C, Croxford R, et al. Canadian Institute for Health Information Discharge Abstract Database: a validation study. Institute for Clinical Evaluative Sciences; 2006. Available from URL: https://www.ices.on.ca/~/media/Files/Atlases-Reports/2006/CIHI-DAD-a-validation-study/Full-report.ashx (accessed December 2020).
Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 2005; 43: 1130-9.
Canadian Institute for Health Information. Canadian Classification of Health Interventions (CCI) - Alphabetical Index 2015. Available from URL: https://www.cihi.ca/sites/default/files/cci_volume_four_2015_en_0.pdf (accessed December 2020).
Canadian Institute for Health Information. Canadian Coding Standards for Version 2018 ICD-10-CA and CCI. Ottawa, ON: CIHI; 2018. Available from URL: https://secure.cihi.ca/free_products/CodingStandards_v2018_EN.pdf (accessed December 2020).
Marrie RA, Dawson NV, Garland A. Quantile regression and restricted cubic splines are useful for exploring relationships between continuous variables. J Clin Epidemiol 2009; 62(511–7): e1.
Harrell F. Regression Modeling Strategies: With Applications to Linear Models, Logistic Regression, and Survival Analysis. New York, NY: Springer; 2001 .
Snijders T, Bosker R. Multilevel Analysis: An Introduction to Basic and Advanced Multilevel Modeling. London: Sage; 2002 .
Merlo J, Chaix B, Ohlsson H, et al. A brief conceptual tutorial of multilevel analysis in social epidemiology: using measures of clustering in multilevel logistic regression to investigate contextual phenomena. J Epidemiol Community Health 2006; 60: 290-7.
Austin PC, Wagner P, Merlo J. The median hazard ratio: a useful measure of variance and general contextual effects in multilevel survival analysis. Stat Med 2017; 36: 928-38.
Lopez-Picado A, Barrachina B, Remon M, Errea M. Cost-benefit analysis of the use of tranexamic acid in total replacement hip surgery. J Clin Anesth 2019; 57: 124-8.
Fillingham YA, Ramkumar DB, Jevsevar DS, et al. The efficacy of tranexamic acid in total hip arthroplasty: a network meta-analysis. J Arthroplasty 2018; 33(3083–9): e4.
Fillingham YA, Ramkumar DB, Jevsevar DS, et al. Tranexamic acid use in total joint arthroplasty: the clinical practice guidelines endorsed by the American Association of Hip and Knee Surgeons, American Society of Regional Anesthesia and Pain Medicine, American Academy of Orthopaedic Surgeons, Hip Society, and Knee Society. J Arthroplasty 2018; 33: 3065-9.
Xie J, Hu Q, Huang Q, Chen G, Zhou Z, Pei F. Efficacy and safety of tranexamic acid in geriatric hip fracture with hemiarthroplasty: a retrospective cohort study. BMC Musculoskelet Disord 2019; https://doi.org/10.1186/s12891-019-2670-5.
Kim KT, Kim CK, Kim YC, et al. The effectiveness of low-dose and high-dose tranexamic acid in posterior lumbar interbody fusion: a double-blinded, placebo-controlled randomized study. Eur Spine J 2017; 26: 2851-7.
Shakeri M, Salehpour F, Shokouhi G, et al. Minimal dose of tranexamic acid is effective in reducing blood loss in complex spine surgeries: a randomized double-blind placebo controlled study. Asian Spine J 2018; 12: 484-9.
Feely MA, Collins CS, Daniels PR, Kebede EB, Jatoi A, Mauck KF. Preoperative testing before noncardiac surgery: guidelines and recommendations. Am Fam Physician 2013; 87: 414-8.
Author contributions
All authors contributed to the conception and design of the manuscript. Brett L. Houston, Emily Krupka, Iris Perelman, Alan Tinmouth, and Anna Blankstein contributed to data acquisition. Brett L. Houston, Allan Garland, Robert Balshaw, and Ryan Zarychanski contributed to data analysis. Brett L. Houston drafted the manuscript, and all authors contributed to manuscript review.
Disclosures
None.
Funding statement
This research was funded by the Manitoba Medical Service Foundation. AFT receives salary support and Brett L. Houston, Daniel I. McIsaac, Allan Garland, Alan Tinmouth, Alexis F. Turgeon, Rodney H. Breau, Dean A. Fergusson, and Ryan Zarychanski receive operating support from CIHR. Ryan Zarychanski is the recipient of the Lyonel G Israels Professorship in Hematology at the University of Manitoba.
Editorial responsibility
This submission was handled by Dr. Philip M. Jones, Deputy Editor-in-Chief, Canadian Journal of Anesthesia.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Houston, B.L., Fergusson, D.A., Falk, J. et al. Variation in prophylactic tranexamic acid administration among anesthesiologists and surgeons in orthopedic surgery: a retrospective cohort study. Can J Anesth/J Can Anesth 68, 962–971 (2021). https://doi.org/10.1007/s12630-021-01939-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-021-01939-x