Abstract
Purpose
This study investigated whether quantitative sensory testing (QST) with thermal stimulations can quantitatively measure the characteristics of an ultrasound-guided interscalene brachial plexus block (US-ISB).
Methods
This was a prospective randomized trial in patients scheduled for arthroscopic shoulder surgery under general anesthesia and US-ISB. Participants and observers were blinded for the study. We assigned the study participants to one of three groups: 0.5% levobupivacaine 15 mL, 0.5% levobupivacaine 15 mL with 1:200,000 epinephrine, and 0.75% ropivacaine 15 mL. We performed thermal QST within dermatomes C4, C5, C6, and C7 before infiltration and 30 min, six hours, ten hours, and 24 hr after performing the US-ISB. In addition, we used QST, a semi-objective quantitative testing method, to measure the onset, intensity, duration, extent, and functional recovery of the sensory block. We also measured detection thresholds for cold/warm sensations and cold/heat pain.
Results
Detection thresholds for all thermal sensations within the ipsilateral C4, C5, C6, and C7 dermatomes increased rapidly (indicating the development of a hypoesthetic state) and reached a steady state after 30 min. This lasted for approximately ten hours and returned to normal detection thresholds by 24 hr. There were no differences detected between the three groups at 24 hr when we compared warm sensation thresholds on one dermatome. Visual inspection of the pooled results per dermatome suggests the ability of QST to detect clinically relevant differences in block intensity per dermatome.
Conclusions
Quantitative sensory testing can be useful as a method for detecting the presence and characteristics of regional anesthesia-induced sensory block and may be used for the evaluation of clinical protocols. The three local anesthetic solutions exhibited a similar anesthetic effect. The results support the use of QST to assess block characteristics quantitatively under clinical research conditions. This trial was registered at Clinicaltrals.gov, NCT02271867.
Résumé
Objectif
Cette étude avait pour objectif de déterminer si les tests sensoriels quantitatifs (QST) avec stimuli thermiques pouvaient mesurer de façon quantitative les caractéristiques d’un bloc interscalénique du plexus brachial réalisé sous échoguidage (US-ISB).
Méthode
Il s’agit d’une étude randomisée prospective réalisée auprès de patients devant subir une chirurgie arthroscopique de l’épaule sous anesthésie générale et US-ISB. Aux fins de l’étude, les participants et les observateurs étaient en aveugle. Nous avons attribué les participants à l’un de trois groupes : 15 mL de lévobupivacaïne 0,5 %, 15 mL de lévobupivacaïne 0,5 % avec de l’épinéphrine 1: 200 000, et 15 mL de ropivacaïne 0,75 %. Nous avons réalisé des QST thermiques au niveau des dermatomes C4, C5, C6 et C7 avant l’infiltration et 30 min, six heures, dix heures et 24 heures après réalisation du US-ISB. De plus, nous avons utilisé le QST, une méthode de test quantitatif semi-objective, afin de mesurer le délai d’action, l’intensité, la durée, l’étendue et la récupération fonctionnelle du bloc sensitif. Nous avons également mesuré les seuils de détection des sensations de froid/chaleur et de douleur au froid/à la chaleur.
Résultats
Les seuils de détection de toutes les sensations thermiques au sein des dermatomes ipsilatéraux C4, C5, C6 et C7 ont rapidement augmenté (indiquant l’apparition d’un état d’hypoesthésie) et se sont stabilisés après 30 min. Cet état a duré environ dix heures et, à 24 h, les seuils de détection étaient à nouveau normaux. Aucune différence n’a été détectée entre les trois groupes à 24 h lorsque nous avons comparé les seuils de sensation de chaleur au niveau d’un dermatome. L’inspection visuelle des résultats groupés par dermatome laisse penser que le QST pourrait détecter les différences pertinentes d’un point de vue clinique en matière d’intensité du bloc par dermatome.
Conclusion
Les tests sensoriels quantitatifs peuvent être utiles pour détecter la présence et les caractéristiques d’un bloc sensitif induit par l’anesthésie régionale; ces tests peuvent être utilisés pour évaluer les protocoles cliniques. Les trois solutions d’anesthésiques locaux ont eu un effet anesthésique semblable. Les résultats appuient l’utilisation des QST pour évaluer les caractéristiques d’un bloc de façon quantitative dans des conditions de recherche clinique. Cette étude a été enregistrée au www.clinicaltrials.gov, NCT02271867.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Several improvements in clinical practice of peripheral nerve blocks (PNB) have been introduced over the last decade, including the routine use of ultrasound (US). Numerous studies have emphasized the advantages of US, including reduced block onset time, control of the spread of local anesthetic (LA), and the use of smaller volumes of LA.1-6
There are several challenges to address in order to bring about further improvement in the quality of PNB. One challenge is to determine if we can further reduce LA concentrations and still produce a block of sufficient duration and antinociceptive intensity. Another challenge requires objective and reliable identification of the optimal anesthetic solutions and injection sites to achieve postoperative analgesia with the use of a single-injection block. Use of novel methods should help to address the challenges of objectively assessing PNBs.
With this in mind, we considered using thermal quantitative sensory testing (QST), a method frequently applied to assess chronic pain syndromes.7,8 The rationale for using QST to assess a block is to draw on a reliable repeatable technique to obtain a gradual and objective measurement of the intensity of a sensory block over time.7,9 By contrast, traditional sensory testing techniques, such as pinprick, touch, cold sensation, and motor block, applied in previous studies are more subjective, less discriminatory between different fibres and nociceptors, not gradual, and can depend on the intensity of their application.10-12 Cold sensation (CS) by ether application is the most frequently used clinical evaluation of sensory impairment after regional analgesia, but CS examines only A-δ fibres, not C fibres.13 Pinpricks stimulate A-δ fibres, C fibres, and unencapsulated free nerve endings and mechanoreceptors. These mechanoreceptors are activated not only by noxious stimuli but also by pressure and stretch, both of which stimulate adjacent cells.14
Thermal QST, a computer-operated threshold system, uses contact heat and cold stimulations delivered by a contact thermode. This methodology has gained wide acceptance in the evaluation of chronic pain conditions involving dysfunction of cutaneous small fibres. With the availability of normative data, studies have implemented standardized QST protocols that apply age- and sex-matched reference values.7,15 This technique is useful in the detection and follow-up of various types of small-fibre neuropathies characterized by the impairment of the thinly myelinated A-δ and unmyelinated C fibres.8
The purpose of the present report is to describe block characteristics as measured by QST for the benefit of researchers who may consider using this measurement technique in their own research or clinical practice.
Methodology
The local ethical committee gave their approval (approval no. 9/25/113). for this single-centre prospective randomized double-blind study. We conducted the study at Antwerp University Hospital from July 2009 to August 2010 in accordance with the recommendations of good clinical practice. Inclusion criteria for the study were adult patients scheduled for diagnostic and therapeutic shoulder arthroscopy, with or without decompression. Exclusion criteria included patients with contraindications to the study drugs or interscalene brachial plexus block, those with diabetes mellitus or peripheral neuropathy, or those receiving chronic analgesic therapy. An anesthesiologist assessed patients during the preoperative consultation, and if patients met the inclusion and exclusion criteria and signed the informed consent form, they could enroll in the study. Patients stopped using all analgesics 12 hr before surgery, and all patients included in this study protocol received lorazepam (1 mg) orally as a premedication.
Randomization technique
The patients were randomly assigned to receive an ultrasound-guided interscalene brachial plexus block (US-ISB) with one of three LA solutions. An independent researcher who was not involved in patient care during the study procedure prepared sealed envelopes to allocate the participants randomly to one of the three study groups. The randomization technique for this study did not involve use of strata or blocks.
A research assistant entered sex, age, and dermatome data into the TSA-II - NeuroSensory Analyzer (Medoc Ltd., Ramat Yishai, Israel) before the first test. The analyzer’s software uses sex, age, and dermatome to identify corresponding normative values for the different thermal thresholds.7,16 Patients with initial QST findings indicating the presence of hyper- or hypo sensory phenomena were excluded from participation.
We then assigned patients randomly to one of three experimental conditions: 0.5% levobupivacaine (0.5% LBup), 0.5% levobupivacaine with 1/200,000 epinephrine (0.5% LBupEpi), or 0.75% ropivacaine (0.75% Rop) (Fig. 1). We used low-volume high-concentration long-acting LA for maximal duration of analgesic effect via a single-injection ISB.17,18 The blinded researcher then selected a sealed envelope and gave the envelope to the unblinded study team member. The unblinded member of the study team prepared the medication in a room adjacent to the operating theatre. Patients, the independent data recorder, and the physician performing the ISB were unaware of the LA solution used. We then recorded QST parameters - warm sensation (WS), CS, heat pain (HP), and cold pain (CP) - at different time points after the LA injection.
Quantitative thermal testing
We performed thermal QST within dermatomes C4 through C7 in the following manner: We first placed the thermal analyzer thermode and fixed the device in position with a band on the dermatomes to be tested. The device induces a serial change in temperature starting at a baseline of 32°C. Changes in the intensity and direction of the current flow (Peltier principle) result in ascending or descending changes in the surface temperature of the test thermode at a rate of 1°C·sec−1 for non-noxious sensations and 1.5°C·sec−1 for painful stimulations. Patients set threshold values by pressing a button when they detect a change in temperature or pain (method of limits). Detection thresholds for non-noxious CS and WS (representing A-δ fibres and C fibres, respectively) are recorded first. Detection thresholds for CP and HP (both representing A-δ and C fibres) are subsequently documented. To avoid skin injury, increases and decreases in temperature are stopped at 50.5°C for HP and 0°C for CP.
We performed the thermal QST one hour before US-ISB and then 30 min, six hours, ten hours, and 21-24 hr after LA infiltration. We also performed sensory testing in the contralateral C5 dermatome, which served as an intra-participant control. We obtained five measurements for CS/WS and three measurements for CP/HP at every dermatome and used the mean of the measurements for each sensation/pain. The controls used in this protocol included the measured thresholds of all ipsilateral dermatomes before performing the US-ISB and all thresholds of the unblocked contralateral C5 dermatome at every interval. We determined the WS/CS and HP/CP detection thresholds by applying the reaction-time inclusive method of limits. Each patient served as their own control; individual baseline values were substitute reference ranges for the normative data available for these tests. We assessed the effect of applying regional anesthesia by an evaluation of the differences in detection thresholds for these non-noxious thermal stimuli. We expressed the degree of hypoesthesia as a change in the detection threshold from baseline (32°C) to maximal level (50.5°C for WS and 0°C for CS).7,15 Following each QST, we evaluated the degree of motor block using a validated three-point modified Bromage scale.19
The need for and timing of rescue medication were also part of the evaluation of clinical parameters for block efficacy, and we noted both in the medical records. The rescue medication consisted of paracetamol 1 g iv and ketorolac 30 mg iv. Quantitative sensory testing was performed for all patients one hour before infiltration in the four ipsilateral (C4, C5, C6, C7) dermatomes and the contralateral (C5) dermatome. We based the measurement time points in our patient population on full recovery of cognitive function after attaining general anesthesia using short-acting anesthetics. Data from the left and right sides of the body were combined for absolute reference data.7
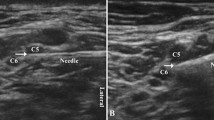
Regional anesthesia technique
An US-ISB was performed with an injection at the level of the emerging C5 nerve root. Under sterile conditions, we used a 12-MHz Logiq e linear probe (GE, USA) and a 22G Stimuplex® needle (BBraun, Germany) in an in-plane needle approach. We localized the C5 root by recognizing the transverse processes of C7, C6, and C5, and then, we slowly injected 15 ml of the LA with the needle positioned lateral to the C5 root. When necessary, we repositioned the needle medial to the C5 root to optimize the spread anteriorly.
General anesthesia technique
The second QST was performed 30 min after the US-ISB, followed by induction of general anesthesia. A standardized induction consisted of propofol 2-3 mg·kg−1, fentanyl 3 μg·kg−1, and rocuronium 0.5 mg·kg−1, followed by sevoflurane maintenance. We conducted noninvasive blood pressure, electrocardiogram, and SpO2 monitoring before induction and at regular intervals after intubation. In addition, capnography continued until the end of the procedure. Supplemental opioid increments were administered when the pre-induction blood pressure increased by > 25%.
Statistical analysis
A preliminary study showed the possibility of finding a difference of 5.5°C between any two groups at a single time point and a single dermatome. This would entail using a desired power of 0.90, a significance criterion of 0.05 (two-tailed), and a standard deviation (SD) of 4.8°C with a sample size of at least 13 patients per group (StatsToDo Trading Pty Ltd). We therefore limited the statistical analysis for the between-group analysis to a predefined single time point (24 hr post injection), on a single dermatome (C5), for a single test (WS). We applied the analysis of variance test for this comparison. We reported continuous normally distributed variables as mean (SD) and the non-normally distributed variable, time to rescue medication, as median (interquartile range [IQR]). Statistical analyses were performed using Prism 6.0e for Mac (GraphPad Software, Inc. USA). Normality was confirmed by applying the D’Agostino-Pearson omnibus test for normality to the residuals of the model.
Outcome parameters
The primary outcome parameter was the measurement of gradual changes in block characteristics (evaluating changes in cutaneous somatosensation) along the adjacent roots of the injection site in an ISB. Our secondary goal was to determine the feasibility of using QST to assess various LA block characteristics, such as onset, intensity, duration, and functional recovery, by measuring sensory detection thresholds in the relevant dermatomes. As a third outcome parameter, we wanted to investigate the feasibility of using QST to evaluate the presence of a sensory block, given that the application of regional anesthesia increases the detection thresholds for non-noxious stimuli. We defined feasibility as a standardized technique using useful signals to measure the intensity (with low variability) of PNB in all patients under research conditions and not in a routine clinical setting.
There was insufficient power in our study design to show differences between LA solutions at different assessment intervals.
In order to analyze changes in block characteristics over time for multiple dermatomes with adequate precision, we would require far larger groups of patients because of the multiplicity of testing. We therefore chose to report the obtained data but refrain from further statistical analysis regarding time-dependent changes. Data were pooled per dermatome to report between-dermatome differences.
Results
We randomly assigned 52 patients to three groups (Fig. 1) and excluded seven patients during the study period before we reached our sample of 45 patients. Patient demographics were similar across the three groups (Table 1). The QST results prior to injection were within the age-, sex- and dermatome-specific normative ranges for all 45 patients.7,15
The changes in mean (SD) detection thresholds in C5 were as follows:
-
Group LBup [CS, 24.4°C (6.5) to 7.4°C (11.5) and WS, 39.4°C (3.1) to 48.8°C (3.2)];
-
Group LBupEpi [CS, 26.3°C (2.8) to 4.4°C (9.3) and WS, 38.1°C (1.1) to 49.1°C (3.8)];
-
Group Rop [CS, 24.9°C (4.4) to 5.7°C (9.4) and WS 38.7°C (2.6) to 49.2°C (3.0)].
Table 3 (available as an Electronic Supplementary Material) itemizes all recorded mean values for each drug, dermatome, and time point.
Fig. 2 (WS and CS in C5) and Fig. 3 (WS and CS in C7) present the different detection thresholds for the three solutions displaying the block characteristics over time, including the block intensity. We observed these changes at 30 min, and they lasted up to ten hours after injection. The mean (SD) CS and WS thresholds [CS, 5 (40)%; WS, 28 (60)%] did not differ more than 50% from the baseline-corrected values in the C7 dermatome (Fig. 3); thus, an adequate (i.e., clinically relevant) sensitive block was likely not achieved in this dermatome. Nevertheless, the observed changes in the detection threshold still suggest the presence of a certain degree of hypoesthesia. Fig. 5 and Fig. 6 (available as an Electronic Supplementary Material) show changes in the CP and HP thresholds over time for C5 and C7, respectively.
Time course of neurosensory changes at the C5, ipsilateral and contralateral, dermatome for the three anesthetic solutions (0.5% LBup, 0.5% LBupEpi, and 0.75% Rop) measured with quantitative sensory testing (mean, standard deviation [SD]) in detection thresholds for cold sensation and warmth sensation. The increases in thresholds are significant as compared with pre-injection thresholds (P < 0.05). Contralateral measurements (displayed in open non-filled shapes) served as intra-subject control and did not differ significantly from the baseline temperature sensation detection thresholds. Detection thresholds between the three local anesthetics (both ipsilateral and contralateral) did not differ significantly. LBup = levobupivacaine; LBupEpi = levobupivacaine with 1/200,000 epinephrine; Rop = ropivacaine
Time course of neurosensory changes at the ipsilateral C7 and contralateral C5 dermatomes for the three anesthetic solutions (0.5% LBup, 0.5% LBupEpi and 0.75% Rop) measured with quantitative sensory testing [mean, standard deviation (SD)] in detection thresholds for cold sensation and warmth sensation. Increases in thresholds are significant as compared with pre-injection thresholds (P < 0.05). Contralateral measurements (displayed in open non-filled shapes) served as intra-subject control and did not differ significantly from the baseline temperature sensation detection thresholds. Detection thresholds between the three local anesthetics (both ipsilateral and contralateral) did not differ significantly. LBup = levobupivacaine; LBupEpi = levobupivacaine with 1/200,000 epinephrine; Rop = ropivacaine
At 24 hr following injection of LA, the mean (SD) differences between the initial (Pre) and last measured values (24 hr) in C5 were as follows:
-
Group LBup [WS, −1.3 (5.1)°C and CS, −1.3 (5.2)°C];
-
Group LBupEpi [WS, −2.7 (5.8)°C and CS, 0.7 (3.9)°C];
-
Group Rop [WS, −3.5 (1.2)°C and CS, 1.2 (4.8)°C].
Differences in WS thresholds on C5 were not statistically different for the three groups 24 hr after injection (P = 0.215), indicating a similar degree of sensory nerve blockade for the three LA solutions at that time point.
Visual inspection of the data in Figs. 2 and 3 suggested no differences between the three groups at all time points. We therefore pooled the results for the three drugs to assess differences in block intensity between dermatomes. The changes in thresholds (pooled results for the three LA) were pronounced at C5. The mean (SD) changes in detection threshold values (hypoesthesia) were WS, 16.6 (9.2)°C and CS 26.6 (16.9)°C at six hours. At C7, the mean (SD) changes for WS and CS were 5.2 (11.1)°C and 1.6 (12.8)°C, respectively. The variable change detected at both dermatomes suggests the ability of QST to detect clinically relevant differences in block intensity (Table 2).
After the QST at 30 min, motor block was complete (Grade 2) in 43 patients (Fig. 4). A decreased (Grade 1) motor response was observed in two patients. Motor block lasted for at least ten hours in all patients, except one patient treated with 0.5% LBup. The median [IQR] time before the patients requested rescue medication was 12.5 hr [9.25 −16.8]. The elapsed time at rescue analgesia did not differ significantly across the three groups.
Time course of changes in intensity of motor block after regional anesthesia. Motor block was assessed using the three-point modified Bromage scale. A score of 2 means no motor block, while a score of 1 means decreased motor strength and a score of 0 means complete motor block with an inability to move. Data are displayed as mean [standard deviation (SD)]
Discussion
The findings of this study show that QST may be useful in detecting the presence of a regional anesthesia-induced somatosensory block and in evaluating the characteristics over time. The detection thresholds for non-noxious thermal sensations, WS, and CS continued to increase after 30 min, indicating that the maximal block was not yet achieved, the LA solution was still spreading, or both. The peak effect, measured as a maximum threshold at six and ten hours, suggests a steady-state block with maximal effect of LA. During this period, the block was sufficient, and patients asked for rescue medication only when a regression of the block had occurred.
There is an increased role for QST in the assessment of A-δ and C fibre function in diverse acute and chronic pain conditions. This is applicable in the quantitative assessment of PNBs in a clinical research setting by selective measurement of A-δ and C fibre sensory nerve function. Its primary advantage is the lack of activation of complementary sensations like vibration, stretch, and pressure. Nevertheless, concerns of reliability and the complexity of assessment have limited the broader application of QST in the clinical setting.7,20-22
Complete temperature discrimination remained possible at all time points regardless of the depth of the motor block. This finding may indicate the presence of an incomplete ISB, an incomplete sympathetic block, or a combination of both. The sympathetic fibres originating from the cervical sympathetic chain and present in the arterial vascular wall are not blocked by an ISB.
Due to the proximity of the different roots in the interscalene region and through the application of the QST protocol, we were able to measure a gradual decrease in the extent of the block with distance from the injection site (C5), particularly in C7 where we measured a less deep block. These differences provided an estimate of the effect of spread of the anesthetic solutions as well as the speed of block onset in every root. This effect is likely more pronounced when using lower volumes of LA solutions.
The time course of the noxious detection thresholds was similar to that of the non-noxious detection thresholds, but the QST software automatically limits the noxious detection thresholds at a certain temperature to avoid burn or frostbite lesions (50.5°C and 0°C). When high concentrations of LA solutions are used, HP and CP reach those cut-off thresholds, making pain thresholds less important in the evaluation of these blocks. In addition, the highly variable activation of A-δ and C fibres determines the CP thresholds; this activation differs significantly across patients, making CP less reliable.9,23 Nevertheless, a comparison of the reliable HP thresholds is possible when examining the roots at the distance of C5 (Figs 5 and 6; available as Electronic Supplementary Material).
At 24 hr, the motor block was in regression but still present. Resolution of the sensory block, as measured by thermal QST, appeared to precede resolution of the motor block. There was no significant difference between the different experimental groups. We can attribute these effects to the decrease over time in the LA concentration in situ, with a faster recovery of sensory fibres than large motor fibres.24
Comparing the ipsilateral vs the contralateral C5 dermatome was mandatory not only to obtain in-patient reference data (because QST is region-specific and absolute data are not available) but also to exclude an eventual systemic effect of LA.7 Moreover, the low variability between these contralateral thresholds clearly shows the reliability and reproducibility of QST and confirms the feasibility of using QST under research conditions, our tertiary outcome.
We did not include pinprick as a reference measurement because thermal QST prior to pinprick induces increased mechanical perception, and repeated mechanical stimulation leads to habituation mechanisms, thereby lowering mechanical thresholds.7,25
Several practical considerations limit widespread use of QST at the bedside. Quantitative sensory testing is reliable only when following a rigorous methodological protocol necessitating verbal instructions to the patient and implementation of the technical procedure.7,20 Patient cooperation and attention are necessary to garner adequate responses to the stimuli, challenging the use of QST during the perioperative period, among patients receiving sedatives, and at night. The development of hypersensitivity and conditioning to repeated stimuli limits the number of potential QST values.20,23,26 Quantitative sensory testing is time-consuming, requiring a mean (SD) of 33 (9) min for each assessment in our study. Finally, the applied method of limits should be a reaction-time inclusive method, thereby resulting in higher physiological detection thresholds.27 Reaction-time exclusive methods, such as the method of levels, are even more time-consuming (extending the duration of testing up to 60-80 min per patient), excluding their application in clinical research projects.27
As an alternative to thermal QST protocols, the Neurometer®, a current perception threshold (CPT®) device, applies electric current perception thresholds to assess nerve function after LA administration;28,29 however, this option exhibits less reliability and considerably more variability than thermal QST. Furthermore, patients detect thermal stimuli more easily than CPT stimuli.30,31 Finally, this method is only a semi-objective test in that it requires subjective feedback from patients regarding the detection of electrical stimulation.
This study has several limitations. The intervals between the QST episodes were several hours in length, which may have resulted in missing subtle differences in the onset and resolution of the block. Because full patient cooperation and attention are necessary for adequate responses to the stimuli, we based the measurement time points in our patient population on full recovery of cognitive function after general anesthesia and avoided measurement time points during normal sleep. This requirement prohibited the application of QST during the perioperative period and at night. In the present study, we tested long-acting LA solutions with recovery of the block during the night. This approach allowed us to compare the different graphs and the time to rescue medication. The practical limitations described above as well as the possible development of hypersensitivity and conditioning by repeated thermal stimuli limited the potential number of QST values for an assessed patient.20,23,26
This study shows that reducing the volumes of LA, a current practice in US-ISB, results in a more selective block. The intensity of the block is optimal at C5 when we inject the LA solution around the C5 root, as for shoulder surgery, but the intensity decreases when measured at the adjacent roots. Future studies should address the potential for a reduction in LA volume and block duration without a reduction in analgesia and patient comfort.
In conclusion, the use of QST enabled a comparison of the onset, intensity, and duration of LA block among clinically applied anesthetic drugs. Furthermore, this study highlights the importance of the site of injection on the intensity of sensory block. These objective measures may assist future clinical research, but routine clinical use in the perioperative period awaits the development of less time-consuming assessment protocols.
References
McNaught A, Shastri U, Carmichael N, et al. Ultrasound reduces the minimum effective local anaesthetic volume compared with peripheral nerve stimulation for interscalene block. Br J Anaesth 2011; 106: 124-30.
Gautier P, Vandepitte C, Ramquet C, DeCoopman M, Xu D, Hadzic A. The minimum effective anesthetic volume of 0.75% ropivacaine in ultrasound-guided interscalene brachial plexus block. Anesth Analg 2011; 113: 951-5.
Gray AT, Laur JJ. Regional anesthesia for ambulatory surgery: where ultrasound has made a difference. Int Anesthesiol Clin 2011; 49: 13-21.
Harper GK, Stafford MA, Hill DA. Minimum volume of local anaesthetic required to surround each of the constituent nerves of the axillary brachial plexus, using ultrasound guidance: a pilot study. Br J Anaesth 2010; 104: 633-6.
Kapral S, Greher M, Huber G, et al. Ultrasonographic guidance improves the success rate of interscalene brachial plexus blockade. Reg Anesth Pain Med 2008; 33: 253-8.
Renes SH, Rettig HC, Gielen MJ, Wilder-Smith OH, van Geffen GJ. Ultrasound-guided low-dose interscalene brachial plexus block reduces the incidence of hemidiaphragmatic paresis. Reg Anesth Pain Med 2009; 34: 498-502.
Rolke R, Baron R, Maier C, et al. Quantitative sensory testing in the German Research Network on Neuropathic Pain (DFNS): standardized protocol and reference values. Pain 2006; 123: 231-43.
Lauria G. Small fibre neuropathies. Curr Opin Neurol 2005; 18: 591-7.
Felix ER, Widerstrom-Noga EG. Reliability and validity of quantitative sensory testing in persons with spinal cord injury and neuropathic pain. J Rehabil Res Dev 2009; 46: 69-84.
Eadie MJ, Scott AE, Lees AJ, Woodward M. William Gowers: the never completed third edition of the ‘Bible of Neurology’. Brain 2012; 135: 3178-88.
Mulholland RC. Sir William Gowers 1845-1915. Spine (Phila Pa 1976) 1996; 21: 1106-10.
Gowers WR. A Manual of Diseases of the Nervous System. London: J. & A. Churchill; 1886 .
Hansson P, Backonja M, Bouhassira D. Usefulness and limitations of quantitative sensory testing: clinical and research application in neuropathic pain states. Pain 2007; 129: 256-9.
Adriaensen H, Gybels J, Handwerker HO, Van Hees J. Response properties of thin myelinated (A-delta) fibers in human skin nerves. J Neurophysiol 1983; 49: 111-22.
Yarnitsky D, Sprecher E. Thermal testing: normative data and repeatability for various test algorithms. J Neurol Sci 1994; 125: 39-45.
Magerl W, Krumova EK, Baron R, Tolle T, Treede RD, Maier C. Reference data for quantitative sensory testing (QST): refined stratification for age and a novel method for statistical comparison of group data. Pain 2010; 151: 598-605.
Casati A, Putzu M. Bupivacaine, levobupivacaine and ropivacaine: are they clinically different? Best Pract Res Clin Anaesthesiol 2005; 19: 247-68.
Burlacu CL, Buggy DJ. Update on local anesthetics: focus on levobupivacaine. Ther Clin Risk Manag 2008; 4: 381-92.
Bromage PR. Mechanism of action. In: Bromage PR, editor. Epidural Analgesia. Philadelphia: WB Saunders; 1978. p. 119-59.
Heldestad V, Linder J, Sellersjo L, Nordh E. Reproducibility and influence of test modality order on thermal perception and thermal pain thresholds in quantitative sensory testing. Clin Neurophysiol 2010; 121: 1878-85.
Defrin R, Ohry A, Blumen N, Urca G. Sensory determinants of thermal pain. Brain 2002; 125: 501-10.
Wilder-Smith OH, Tassonyi E, Crul BJ, Arendt-Nielsen L. Quantitative sensory testing and human surgery: effects of analgesic management on postoperative neuroplasticity. Anesthesiology 2003; 98: 1214-22.
Moloney NA, Hall TM, O’Sullivan TC, Doody CM. Reliability of thermal quantitative sensory testing of the hand in a cohort of young, healthy adults. Muscle Nerve 2011; 44: 547-52.
Gokin AP, Philip B, Strichartz GR. Preferential block of small myelinated sensory and motor fibres by lidocaine: in vivo electrophysiology in the rat sciatic nerve. Anesthesiology 2001; 95: 1441-54.
Grone E, Crispin A, Fleckenstein J, Irnich D, Treede RD, Lang PM. Test order of quantitative sensory testing facilitates mechanical hyperalgesia in healthy volunteers. J Pain 2012; 13: 73-80.
Backonja MM, Walk D, Edwards RR, et al. Quantitative sensory testing in measurement of neuropathic pain phenomena and other sensory abnormalities. Clin J Pain 2009; 25: 641-7.
Sunnergren O, Brostrom A, Svanborg E. How should sensory function in the oropharynx be tested? Cold thermal testing: a comparison of the methods of levels and limits. Clin Neurophysiol 2010; 121: 1886-9.
Radwan IA, Saito S, Goto F. High-concentration tetracaine for the management of trigeminal neuralgia: quantitative assessment of sensory function after peripheral nerve block. Clin J Pain 2001; 17: 323-6.
Liem EB, Joiner TV, Tsueda K, Sessler DI. Increased sensitivity to thermal pain and reduced subcutaneous lidocaine efficacy in redheads. Anesthesiology 2005; 102: 509-14.
Lowenstein L, Jesse K, Kenton K. Comparison of perception threshold testing and thermal-vibratory testing. Muscle Nerve 2008; 37: 514-7.
Tsui BC, Shakespeare TJ, Leung DH, Tsui JH, Corry GN. Reproducibility of current perception threshold with the Neurometer((R)) vs the Stimpod NMS450 peripheral nerve stimulator in healthy volunteers: an observational study. Can J Anesth 2013; 60: 753-60.
Acknowledgement
The authors thank Dr. Kristien Wouters for her assistance with the statistical analyses.
Editor’s note
Data sharing: original, de-identified, data are available on request from the corresponding author. Please contact Dr. Sermeus at: luc.sermeus@uza.be
Disclosure of funding
Departmental resources funded this study - Department of Anesthesiology, Antwerp University Hospital, University of Antwerp, Edegem, Belgium.
Conflicts of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author contributions
Luc A. Sermeus conceived and coordinated the study. Luc A. Sermeus, Guy H. Hans, and Margaretha B. Breebaart helped conceive the study design. Luc A. Sermeus and Margaretha B. Breebaart performed the blocks. Luc A. Sermeus analyzed the quantitative sensory testing results and wrote the manuscript. Guy H. Hans performed the quantitative sensory testing interpretation, analyzed the data, and edited various versions of the manuscript. Tom Schepens assisted in reviewing and editing the different versions of the manuscript and significantly contributed to the statistical analysis. Nathalie M.-L. Bosserez and Carine J. Smitz performed the quantitative sensory testing. Guy H. Hans and Nathalie M.-L. Bosserez helped draft the manuscript. Nathalie M.-L. Bosserez presented the abstract. Carine J. Smitz collected data. Marcel P. Vercauteren and Margaretha B. Breebaart critically read the various versions of the manuscript.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sermeus, L.A., Hans, G.H., Schepens, T. et al. Thermal quantitative sensory testing to assess the sensory effects of three local anesthetic solutions in a randomized trial of interscalene blockade for shoulder surgery. Can J Anesth/J Can Anesth 63, 46–55 (2016). https://doi.org/10.1007/s12630-015-0505-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-015-0505-x