Abstract
This randomized double-blind controlled trial compared the block characteristics of three low-dose local anesthetics at different roots in an ultrasound-guided interscalene block, using thermal quantitative sensory testing for assessing the functioning of cutaneous small nerve fibres. A total of 37 adults scheduled to undergo shoulder arthroscopy were randomized to receive 5 mL of either 0.5% levobupivacaine with and without epinephrine 1/200,000 or 0.75% ropivacaine in a single-shot interscalene block. Thermal quantitative sensory testing was performed in the C4, C5, C6 and C7 dermatomes. Detection thresholds for cold/warm sensation and cold/heat pain were measured before and at 30 min, 6, 10 and 24 h after infiltration around C5. The need for rescue medication was recorded. No significant differences between groups were found for any sensation (lowest P = 0.28). At 6 h, the largest differences in sensory thresholds were observed for the C5 dermatome. The increase in thresholds were less in C4 and C6 and minimal in C7 for all sensations. The analgesic effect lasted the longest in C5 (time × location mixed model P < 0.001 for all sensory tests). The time to rescue analgesia was significantly shorter with 0.75% ropivacaine (P = 0.02). The quantitative sensory findings showed no difference in intensity between the local anesthetics tested. A decrease in block intensity, with minimal changes in pain detection thresholds, was observed in the roots adjacent to C5, with the lowest block intensity in C7. A clinically relevant shorter duration was found with 0.75% ropivacaine compared to the other groups. Trial registration NCT 02691442.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Ultrasound guidance (USG) has optimized the performance of peripheral nerve blocks (PNB) by increasing the success rate and decreasing complications [1]. One of the main advantages when using ultrasound-guided regional anesthesia (UGRA) is, as Barrington et al. demonstrated, a reduction of local anesthetic (LA) volume and thereby a decreased incidence of local anesthetic systemic toxicity (LAST) [2]. Another advantage of UGRA when performing an interscalene block (ISB) is a possible decrease in phrenic nerve palsy [3].
Furthermore, with UGRA, the exact site of injection can be determined and the spread of the LA solution around the targeted nerve can be visualized [4]. In the case of an Interscalene block (ISB) for shoulder surgery, the targeted root is C5 or the superior trunk before the suprascapular nerve, which innervates the upper part of the shoulder joint, branches out of the brachial plexus. The inferior, lateral and anterior structures of the joint are innervated by the axillary nerve branching out of the posterior cord. There are also contributions from the subscapular nerve branch of the posterior cord and from the lateral pectoral nerve branch of the lateral cord, and all these nerves originate from the C5 and C6 roots [5].
Pain after shoulder surgery can be a serious problem. The reason for this is the richly innervated joint. A-δ and C-fibres directly transmit continuous deep somatic pain, whereas reflex A-α stimulation at the same spinal cord segments results in severe muscle spasm in the peri-articular region [6,7,8,9]. Adequate pain relief seems crucial for early rehabilitation and a single shot ISB seems to be the technique of choice [10]. Over the past decade, many studies have emphasized a reduction in LA volumes in ISB and the subsequent reduction in hemi-diaphragmatic paresis [3, 11, 12]. The primary goal of a PNB is to provide adequate pre- and/or post-operative pain relief with minimal side effects and/or complications. The downsides of reducing LA volumes in a single-injection ISB include the possibility of a shortened block duration and a reduction in anti-nociceptive intensity and extent. Traditional techniques to evaluate sensory effects of nerve blocks, e.g., pinprick tests, are not gradual, mostly subjective, can depend on the intensity of the application and are less discriminatory between different fibres. We therefore used the novel and repeatable technique of thermal quantitative sensory testing (QST) to objectively, reliably and gradually assess the anti-nociceptive intensity, duration, and extension of the applied nerve block [13]. QST applies thermal stimuli, such as cold (CS) and warm sensations (WS), cold-induced pain (CP) and heat-induced pain (HP), to assess the functioning of small fibres, specifically A-δ and C-polymodal nociceptors responsible for thermal sensation and pain detection and its transmission to the spinal cord and central nervous system, in a semi-objective and reproducible manner [14, 15]. QST has been used to evaluate small nerve neuropathies caused by drugs [16]. The rational to use QST to measure the effects of local anesthetics was the fact that they can be considered to cause a reversible neuropathy and this can be measured with QST [13]. QST has several advantages: it is a graded evaluation due to the quantifiable responses and provides objective evaluation compared to the classical clinical examination. Unlike the evaluation of neuropathies in chronic pain, there is no gold standard for the evaluation of RA. Comparison of the QST method with known techniques, such as pinprick, is impossible for several reasons; pinprick assessment would influence successive measurements, and repeated mechanical stimulation induces increased mechanical perception and leads to habituation mechanisms, thereby lowering mechanical thresholds [14, 17].
Generally, when comparing potency of the different long acting LAs, previous studies suggest a decreasing rank: racemic bupivacaine > levobupivacaine > ropivacaine. This difference seems more evident when using lower concentrations [18]. Previous studies comparing bupivacaine with ropivacaine or levobupivacaine were done with higher volumes [19,20,21,22,23]. Most studies carried out before the era of US, which now make it possible to consistently inject at a similar location in the plexus. Few studies have been performed with low volumes [3, 11]. Moreover, none of these studies used QST for evaluation.
2 Methodology
Approval for this single-centre, prospective, randomized, double-blind study was obtained from the local Ethical Committee (no. 10/45/315). The study was performed in a University Hospital from December 2010 through April 2014. This study was performed in accordance with the recommendations of good clinical practice. Adult patients scheduled for diagnostic and therapeutic shoulder arthroscopy were eligible. Patients with contraindications to non-steroidal anti-inflammatory drugs (NSAIDs) or ISB and those with diabetes mellitus, peripheral neuropathy or receiving chronic analgesic therapy (analgesics for > 3 weeks) were excluded. An anesthesiologist assessed the patients during the pre-operative consultation; if the patient met the inclusion and exclusion criteria and signed the informed consent form, they were enrolled in the study. Patients stopped using all analgesics 12 h before surgery. Lorazepam (1 mg) was administered orally as premedication in every patient included in this study protocol.
2.1 Randomization technique
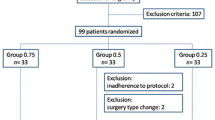
After providing their written informed consent, the patients were randomly assigned to receive an ultrasound-guided interscalene brachial plexus block (US-ISB) with one of three LA solutions. Sealed envelopes, prepared by an independent researcher who was never involved in the patient care during the study procedure, randomly allocated the participants to one of the three study groups: 0.5% LBup (0.5% levobupivacaine), 0.5% LBupEpi (0.5% levobupivacaine with 1/200,000 epinephrine), or 0.75% Rop (0.75% ropivacaine) (Fig. 1). The randomization technique for this study did not involve the use of stratification or blocks.
A blinded research nurse entered the patients’ gender, age and dermatome data in the thermal sensory analyser before the first test. The software of the QST-analyser (Win TSA 5.32, Medoc Ltd., Ramat Yishai, Israel) used gender, age and dermatome to identify the corresponding normative values for the different thermal thresholds [14, 24]. Patients with initial QST findings indicating the presence of hyper- or hypo-sensory phenomena were excluded from participation.
The sealed envelope was given to the unblinded study group member, who prepared the medication in a room adjacent to the operating theatre. Patients, the independent data recorder and the physician performing the ISB were unaware of the LA solution used.
We used low-volume, high-concentration, long-acting LA for maximal duration of the analgesic effect via a single-injection ISB [18, 25]. We then recorded the QST parameters, including WS, CS, HP, and CP, at different time points after the LA injection.
2.2 Quantitative thermal testing
Thermal QST (TSA-II—NeuroSensory Analyser, Medoc Ltd., Ramat Yishai, Israel) was performed within dermatomes C4 through C7. The thermode was placed and fixed in position with a band on the dermatomes to be tested and induced a gradual change in temperature starting at a baseline of 32 °C. Changes in the intensity and the direction of the current flow (Peltier principle) resulted in ascending or descending changes in the surface temperature of the test thermode at a rate of 1 °C/s for non-noxious sensations and 1.5 °C/s for painful stimulations. Patients set threshold values by pressing a button when they detected a change in temperature or pain (method of limits). Detection thresholds for non-noxious cold and warm sensations (representing A-δ fibres and C-fibres, respectively) were recorded first. Detection thresholds for cold and heat pain (both representing A-δ and C-fibres) were subsequently documented. To avoid skin injury, increases and decreases in temperature were stopped for pain sensations at 50.5 °C for heat and 0 °C for cold.
Thermal QST was performed 1 h before US-ISB (baseline recording) and then 30 min, 6, 10, and 21–24 h after LA infiltration. Sensory testing was also performed in the contralateral C5 dermatome, which served as an intra-participant control. Five measurements were obtained for CS/WS and three measurements for CP/HP at every dermatome. The means of the measurements for each sensation/pain were used. The controls used in this protocol included the measured thresholds of all ipsilateral dermatomes before performing the US-ISB and all thresholds of the unblocked contralateral C5 dermatome at every interval. We determined the WS/CS and HP/CP detection thresholds by applying the reaction-inclusive method of limits. Individual baseline values were determined pre-block, and the contralateral C5 QST values served as reference values during each time point. The effect of applying regional anesthesia (RA) was assessed by evaluating the differences in detection thresholds for these non-noxious thermal stimuli. The degree of hypoesthesia was expressed as a change of the detection threshold between the baseline (32 °C) and maximal level (50.5 °C for WS and 0 °C for CS) [14, 26].
In addition, the timing of rescue medication was part of the evaluation as a clinical parameter to measure block efficacy. Since the patient did not receive specific guidelines concerning use of rescue medication, the need for, the timing of rescue analgesic medication as the VAS were noted in the medical records. The rescue medication consisted of 1 g of intravenous (IV) paracetamol and 30 mg of IV ketorolac. Measurement time points in our patient population were based on full recovery of cognitive function after general anesthesia using short-acting anesthetics. Data from the left and right sides of the body were combined for absolute reference data [14]. Patient demographics and medications were also noted. Assessment of motor block was derived from the technique described by Bromage on a three-point scale. A score of 2 means no motor block, while a score of 1 means decreased motor strength and a score of 0 means complete motor block with an inability to move [13, 27].
2.3 Regional anesthesia technique
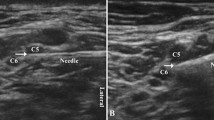
An US-ISB was performed with an injection at the level of the emerging fifth cervical nerve root by a single physician (LS, > 3000 US-guided blocks before starting this study). Under sterile conditions, a linear 18-MHz US-transducer (Focus 400, BK Ultrasound, Herlev, Denmark) and a 22G needle (Sonoplex 50 mm, Pajunk, Geisingen, Germany) were used in an in-plane needle, peri-plexus approach. We performed a peri-plexus approach to avoid subepineural injection, which could damage the root and/or influence our results [28, 29].
The C5 root was localized by identifying the transverse processes of C7, C6 and C5. The needle was positioned lateral and inferior to the C5 root, where 5 mL of the LA was slowly injected after aspiration for blood detection and avoiding intravascular injection.
2.4 General anesthesia technique
General anesthesia was induced after the second QST test, which was performed 30 min after the ISB. A standardized induction using 2 to 3 mg/kg propofol, 3 µg/kg fentanyl and 0.5 mg/kg rocuronium for endotracheal intubation was followed by sevoflurane maintenance. NIBP, ECG, SpO2 and CO2 were monitored before induction and at 5-min intervals after intubation until the end of the procedure. Supplemental opioid increments were administered when the pre-induction blood pressure increased by > 25%.
2.5 Outcome parameters
The objective of this study was to compare the block characteristics, such as onset, intensity and duration when a low volume of various LA solutions was injected for ISB. In particular, our primary outcome parameter was to assess differences between the groups for QST measurements at C5.
We further aimed, as a secondary outcome, to observe the difference in evolution of QST thresholds over time between the groups and the locations, which is translated as the interaction term group by time and location by time in a statistical model. Finally, we aimed to compare the time to first administration of supplemental analgesia, our third outcome.
2.6 Power analysis
Based on the findings of the previous studies we anticipated a difference of 5 °C in thermal threshold between study groups with a deviation of at least 4 °C. To find such a difference at one dermatome, at a certain time point, 10 patients per group are needed, to achieve a power of 80% with a type 1 (a) error of 0.05 (PASS). With this sample size, and the same assumption of a difference of 5 °C in at least one dermatome at one of the measured time points, we tested for an interaction effect between time and group in a mixed effects model with 80% power and type I error 0.05 (GLIMMPSE) [30]. The correlation between measurements of the same individual is assumed to be 0.6, with a decay rate of 0.1.
2.7 Statistical analysis
Data are reported as the means and standard deviations, when normally distributed, and otherwise as medians with lower and upper quartiles. Categorical variables are summarized as numbers and percentages. For the comparison of the time to rescue medication [and the visual analogue score (VAS) score at that time] in the three groups, the Kruskal–Wallis and pairwise Mann–Whitney U tests were used. The number of patients with motor blocks was compared between the groups using the Fisher exact test.
Because the increases and decreases in temperature were stopped at 0 °C for CS and CP and at 50.5 °C for WA and HP, the detection thresholds were left- and right-censored, respectively. For these data, we used the non-linear mixed model described by Thiébaut [31]. This model assumes that sensation and pain thresholds are normally distributed, while incorporating censoring below 0 °C or above 50.5 °C. Correlation between measurements in the same subject was taken into account by adding a nested random intercept for each subject’s location within the time point. The fixed effects in this model included categorical time, group and location. Initially, all two- and three-way interactions were added, and a stepwise reduction procedure was applied based on the Akaike information criteria (AIC). In this way, in all four models (CS, WS, CP, HP), the fixed effects could be reduced to time, group, location and interaction between time and location.
Statistical analyses were performed using SAS 9.2 (SAS Institute, Cary, North Carolina, USA). P < 0.05 was considered as statistically significantly different.
3 Results
A total of 37 patients were randomized. Seven patients were excluded, including 4, due to pre-existing abnormal QST findings measured pre-procedure and 3, due to conversion from arthroscopy to open rotator cuff repair surgery. Thirty subjects completed the study without untoward reactions (Fig. 1: CONSORT Flow Diagram).
The study subjects’ demographic parameters are displayed in Table 1.
The mixed model shows differences over time at C5 for all measured QST parameters (CS, WS, CP, HP) supporting the effectiveness of the RA technique with this small LA volume.
Differences between the dermatomes (C4, C5, C6, C7) were observed (PLocation < 0.001), demonstrating the selectivity for nerve roots with this small dose of LA solution. 6 h after injection, the largest differences in sensory thresholds (CS and WS) could be observed at the C5 dermatome (Figs. 2, 3). [Graphics of all neurosensitive/nociceptive responses are available as Supplemental Material (Additional File 2)].
Cold sensation. Time course of the neurosensory changes in detection thresholds for the cold sensation (Temperature in °C) in the different dermatomes for the three anesthetic solutions (0.5%Bup, 0.5%BupEpi, 0.75%Rop) measured with quantitative sensory testing (mean, standard deviation). The increases in thresholds are significant as compared to pre-injection thresholds (Ptime < 0.001, post-hoc differences versus baseline < 0.05 for all locations). Detection thresholds between the three local anesthetics did not differ significantly (Pgroup 0.70)
Warm sensation. Time course of the neurosensory changes in detection thresholds for the warm sensation (Temperature in °C) in the different dermatomes (C4, C5, C6, C7) for the three anesthetic solutions (I = 0.5%Bup, II = 0.5%BupEpi, III = 0.75%Rop) measured with quantitative sensory testing (mean, standard deviation). The increases in thresholds are significant as compared to pre-injection thresholds (Ptime < 0.001, post-hoc differences versus baseline < 0.05 for all locations). Detection thresholds between the three local anesthetics did not differ significantly (Pgroup 0.30)
P values were calculated separately for time in between injection and QST measurement, (Ptime), cervical root (Plocation) and drug group (Pgroup) or a combination of these factors. The analgesic effect lasted the longest in C5 (Ptime × location < 0.001 for all sensory tests). This result demonstrates that root-specific blockade was established when injecting a small volume of LA solution in close proximity to the nerve root. No significant differences were observed between the study drug groups for any sensation (lowest Pgroup = 0.28). Furthermore, the sensory effect was similarly spread among dermatomes for all three drugs (Pgroup × location = 0.05 for HP, Pgroup × location > 0.27 for the other tested sensations, therefore group x location was not included in the final model). This result indicates equality in sensation and thus reveals no difference in anti-nociceptive effects of the three tested study drugs.
Differences were observed between the time points, i.e., the intensity of the block changed over the time course of the 24-h study period (Ptime < 0.001) and varied for different locations (Ptime × location < 0.001). As indicated in the figures the thresholds at different time points per location reveal no differences for contralateral C5 dermatomes, and only small differences for C7, while large differences are observed for C4, C5 and C6. Differences in the change in analgesic intensity were similar for each study drug (WS Ptime × group = 0.03; CS, HP, CP: Ptime × group = NS, therefore time × group was not included in the final model). The three-way interaction time × location × group was not significant in the four models (Ptime × location × group > 0.21). All mixed model values of nerve blockage effects over time, per dermatome and per study group are available as Supplemental Material (Additional File 1).
The time to the first need for supplemental analgesia, as requested by the patient, ranged from a median of 8 h 28 min (IQR 6 h 15–10 h 50) for 0.75%Rop to a median of 11 h 50 min (IQR 10 h 52–12 h 50) for 0.5%LBupEpi; the median time for patients receiving 0.5%LBup was 11 h 20 min (IQR 8 h 30–13 h 38). The difference between 0.75%Rop and 0.5%LBupEpi was significant (P = 0.02). The median VAS score for pain did not differ between the three study groups (P = 0.12) (Table 2).
4 Discussion
Thermal QST enables the assessment of RA-induced somatosensory block, and particularly the block characteristics over time, by separately testing the small fibres responsible for nociception. Using QST methods, we could map the course of the US-ISB, including its intensity, duration and root selectivity. The three study drugs tested showed comparable nerve blocking effects in terms of intensity. Our results demonstrated the utility of cervical root-specific nerve blockade with a small volume of LA.
QST can quantitatively measure RA-induced somatosensory block over time. This technique, which is used to evaluate neuropathies in chronic pain by objectively measuring abnormalities in the functioning of the cutaneous somatosensory small fibres, was used to gradually determine the effects of an ISB on different roots by measuring the effects on their respective dermatomes [13, 32]. This quantitative, semi-objective approach is in sharp contrast to evaluation techniques that are commonly used in clinical settings, such as the pinprick and cold sensation with ether methods. Since QST is far more precise and less subjective than pinprick methods, it is possible to relate differences in sensory thresholds recorded by this technique to clinically significant outcome parameters such as patient comfort, or the need for rescue analgesic drugs [32, 33]. As a result, predefined thresholds can be used to reliably calculate sample sizes for future research. Currently applied outcome parameters such as the VAS and opioid/rescue analgesic consumption measures are indirect, subjective and surrogate markers for peripheral nerve block characteristics and therefore require larger sample sizes to filter out subject-related and investigator-related biases.
Using QST and following strict methodological protocols, we could indirectly and reliably assess the functionality of small fibres, particularly the A-δ and C-polymodal nociceptors responsible for thermal sensation and pain detection, as well as their transmission to the spinal cord and central nervous system [14, 15]. Defrin et al. suggested that pain quality and thresholds are related to the simultaneous activation of both nociceptive and non-nociceptive pathways, as well as the interactions between them, and that the quality of nociception is determined by central neurons integrating the information arriving from these two pathways, and this conduction system can be evaluated with thermal QST [34, 35].
In a previous study that used the same psycho-physical testing methodology, we suggested the importance of the injection site for the intensity of the block in different nerve roots. Even with high volumes, we could measure a difference in block intensity with differences in the injection site [13].
Our results did not indicate any significant difference in the block characteristics of the LA solutions we studied in the C5-dermatome. However, reducing the volume of injected LA emphasized the importance of the role of the injection site; when injecting a volume of 5 mL of LA around C5, we obtained a more selective block of this root, with a smaller increase in thresholds in the closest C4 and C6 and with no increases in thresholds in C7, more distant from the injection site. As shown in Figs. 2 and 3, the results for CS and WS in C5 at 10 h seem to reflect a shorter duration of action for 0.75%Rop in this time window, although the difference was not statistically significant. Due to the interval of several hours between QST measurements, the exact recovery time point may not have been observed. In addition, in the 0.75%Rop group, the time to supplemental analgesia was significantly shorter, and pairwise tests showed a difference when comparing 0.5%LBupEpi with 0.75%Rop (P = 0.02), indicating a shorter duration of action for 0.75%Rop [18, 36]. The shorter time to rescue medication in the 0.75%Rop (mean 8h28) may have influenced the QST measurements of the 10 h- and “post”-time points in this group. A faster ceiling in the sensation thresholds of the adjacent roots of C5 is observed in the 0.5% LBup group without repercussion on the pain thresholds.
We measured a difference in intensity among the various adjacent roots, demonstrating the importance of the injection site in obtaining a high quality and long-lasting analgesic block. More specifically, in the case of shoulder surgery, small volumes need to be injected near C5 or the superior trunk. The reduced sensations thresholds as measured by QST at C6 seems to have no effect on the analgesic efficacy, as experienced by the patients and as reflected in the pain thresholds of C6, which are proportionally less reduced (Additional File 2). We have no clear explanation for the finding of a different threshold after 0.5% Bupi on C6 (see Figs. 2, 3). The reduced block intensity in C6 could be a reason for the faster recovery and shorter duration of low-volume ISB for shoulder surgery. The expedited recovery may be perceived as pain at the time of ISB recovery, but does not reflect inadequate analgesia at peak effect time (Additional File 2). Moreover, an injection of a low volume of LA in a more distal ISB approach could miss the suprascapular nerve and considerably reduce the analgesic effects in the upper part of the shoulder joint [37]. The rationale for adding epinephrine to a low dose of levobupivacaine (When starting this study, Ropivacaine was already known to have intrinsic vasoconstrictive properties [38, 39]) was to look for any change in analgesic effect. Whether the effect of epinephrine with long-acting LA is simply due to a decreased systemic uptake, leading to a greater effect, or because of any analgesic property of epinephrine itself, is not exactly known. In an ISB local spread could reach the substantia gelatinosa of the spinal cord and have an effect on alpha-2-adrenoreceptors. Even if these effects are minimal with long acting LA solutions and low volumes probably have less spread to the epidural space, this has never been tested with QST [40,41,42,43].
4.1 Limitations
The principle limitation of this study is the small number of patients recruited. Our study compares three low doses of LA solution for their analgesic effects following shoulder arthroscopy. In the patients studied, we were unable to show any significant difference in neurosensitive/nociceptive responses between the LAs, even if subtle differences are likely to exist. In order to statistically demonstrate any differences in block characteristics large sample sizes would have been required [44]. Such samples would exceed available resources—investigators are limited by both resources and time. We selected our population carefully using rigid inclusion criteria to reduce patient variability. In addition, such studies expose the patients to certain risks, even if the RA blocks are performed by an experienced skilled clinician. This raises ethical concerns if sufficient numbers are to be included for the sake of demonstrating statistical significance, especially if the clinical relevance of this is questionable.
Only a clinical difference in duration could be demonstrated.
Second, the standardized protocol and the time(-lapse) needed to perform the evaluation with QST limits the method’s utility in clinical practice. QST is a time-consuming and labour-intensive technique for assessing the analgesic effects of local anesthetics and is therefore likely limited to a research setting.
Third, since multiple evaluations with QST might induce hypersensitivity and conditioning the number of tests are limited. Moreover, as patient cooperation and attention are mandatory for QST, these tests are quite impossible during normal sleep periods, resulting in a lack of data during recovery of the block [15, 45, 46].
Despite these limitations, in a specific setting, QST could allow accurate predictions of adequate sample sizes when designing studies in this field of research.
5 Conclusion
We performed a selective ultrasound-guided interscalene blockade of one nerve root, namely C5, with 5 mL of different long-lasting LA formulations with a measured reduced blockade of the adjacent roots. We found no differences between LAs in the QST pattern at C5. As reflected by QST at 10 h (CS), 0.75%Rop showed a clinically relevant difference in block duration when compared to the other LAs (Figs. 2, 3). A reduction in block intensity and the faster recovery in C6 could be the reason for the shorter duration of clinical analgesia for shoulder arthroscopy. QST measurements suggest that we cannot reduce the volumes of LA indefinitely without an effect on clinical pain relief. Moreover, the knowledge of anatomy and the interpretation of sono-anatomy should help determine the exact injection site when using low volumes of LA to produce the desired analgesia.
Availability of data
Data sharing: original, de-identified, data are available upon request.
References
Kapral S, Greher M, Huber G, Willschke H, Kettner S, Kdolsky R, Marhofer P. Ultrasonographic guidance improves the success rate of interscalene brachial plexus blockade. Reg Anesth Pain Med. 2008;33(3):253–8.
Barrington MJ, Kluger R. Ultrasound guidance reduces the risk of local anesthetic systemic toxicity following peripheral nerve blockade. Reg Anesth Pain Med. 2013;38(4):289–97.
Renes SH, Rettig HC, Gielen MJ, Wilder-Smith OH, van Geffen GJ. Ultrasound-guided low-dose interscalene brachial plexus block reduces the incidence of hemidiaphragmatic paresis. Reg Anesth Pain Med. 2009;34(5):498–502.
Plante T, Rontes O, Bloc S, Delbos A. Spread of local anesthetic during an ultrasound-guided interscalene block: does the injection site influence diffusion? Acta Anaesthesiol Scand. 2011;55(6):664–9.
Aszmann OC, Dellon AL, Birely BT, McFarland EG. Innervation of the human shoulder joint and its implications for surgery. Clin Orthop Relat Res. 1996(330):202–7.
Bonica JJ. Importance of effective pain control. Acta Anaesthesiol Scand Suppl. 1987;85:1–16.
Cousins MJ: John J. Bonica distinguished lecture. Acute pain and the injury response: immediate and prolonged effects. Reg Anesth. 1989;14(4):162–79.
Bonica JJ. Postoperative pain. 2 ed. Vol. 1. Philadelphia: Lea & Febiger; 1990.
Bonica JJ. Anatomic and physiologic basis of nociception. 2 ed. Vol. 1. Philadelphia: Lea & Febiger; 1990.
Borgeat A, Ekatodramis G, Kalberer F, Benz C. Acute and nonacute complications associated with interscalene block and shoulder surgery: a prospective study. Anesthesiology. 2001;95(4):875–80.
Gautier P, Vandepitte C, Ramquet C, DeCoopman M, Xu D, Hadzic A. The minimum effective anesthetic volume of 0.75% ropivacaine in ultrasound-guided interscalene brachial plexus block. Anesth Analg. 2011;113(4):951–5.
McNaught A, Shastri U, Carmichael N, Awad IT, Columb M, Cheung J, Holtby RM, McCartney CJ. Ultrasound reduces the minimum effective local anaesthetic volume compared with peripheral nerve stimulation for interscalene block. Br J Anaesth. 2011;106(1):124–30.
Sermeus LA, Hans GH, Schepens T, Bosserez NM, Breebaart MB, Smitz CJ, Vercauteren MP. Thermal quantitative sensory testing to assess the sensory effects of three local anesthetic solutions in a randomized trial of interscalene blockade for shoulder surgery. Can J Anaesth. 2016;63(1):46–55.
Rolke R, Baron R, Maier C, Tolle TR, Treede RD, Beyer A, Binder A, Birbaumer N, Birklein F, Botefur IC, et al. Quantitative sensory testing in the German research network on neuropathic pain (DFNS): standardized protocol and reference values. Pain. 2006;123(3):231–43.
Heldestad V, Linder J, Sellersjo L, Nordh E. Reproducibility and influence of test modality order on thermal perception and thermal pain thresholds in quantitative sensory testing. Clin Neurophysiol. 2010;121(11):1878–85.
Lauria G. Small fibre neuropathies. Curr Opin Neurol. 2005;18:591–7.
Grone E, Crispin A, Fleckenstein J, Irnich D, Treede RD, Lang PM. Test order of quantitative sensory testing facilitates mechanical hyperalgesia in healthy volunteers. J Pain. 2012;13(1):73–80.
Casati A, Putzu M. Bupivacaine, levobupivacaine and ropivacaine: are they clinically different? Best Pract Res Clin Anaesthesiol. 2005;19(2):247–68.
Casati A, Borghi B, Fanelli G, Cerchierini E, Santorsola R, Sassoli V, Grispigni C, Torri G. A double-blinded, randomized comparison of either 0.5% levobupivacaine or 0.5% ropivacaine for sciatic nerve block. Anesth Analg. 2002;94(4):987–90. (table of contents).
Casati A, Borghi B, Fanelli G, Montone N, Rotini R, Fraschini G, Vinciguerra F, Torri G, Chelly J. Interscalene brachial plexus anesthesia and analgesia for open shoulder surgery: a randomized, double-blinded comparison between levobupivacaine and ropivacaine. Anesth Analg. 2003;96(1):253–9. (table of contents).
Eroglu A, Uzunlar H, Sener M, Akinturk Y, Erciyes N. A clinical comparison of equal concentration and volume of ropivacaine and bupivacaine for interscalene brachial plexus anesthesia and analgesia in shoulder surgery. Reg Anesth Pain Med. 2004;29(6):539–43.
Kaur A, Singh RB, Tripathi RK, Choubey S. Comparision between bupivacaine and ropivacaine in patients undergoing forearm surgeries under axillary brachial plexus block: a prospective randomized study. J Clin Diagn Res. 2015;9(1):UC01–6.
Borgeat A, Ekatodramis G, Blumenthal S. Interscalene brachial plexus anesthesia with ropivacaine 5 mg/mL and bupivacaine 5 mg/mL: effects on electrocardiogram. Reg Anesth Pain Med. 2004;29(6):557–63.
Magerl W, Krumova EK, Baron R, Tolle T, Treede RD, Maier C. Reference data for quantitative sensory testing (QST): refined stratification for age and a novel method for statistical comparison of group data. Pain. 2010;151(3):598–605.
Burlacu CL, Buggy DJ. Update on local anesthetics: focus on levobupivacaine. Ther Clin Risk Manag. 2008;4(2):381–92.
Yarnitsky D, Sprecher E. Thermal testing: normative data and repeatability for various test algorithms. J Neurol Sci. 1994;125(1):39–45.
Bromage PR. Mechanism of action. Philadelphia: WB Saunders; 1978:119–59.
Szerb JJ, Greenberg JL, Kwofie MK, Baldridge WH, Sandeski RE, Zhou J, Wong K. Histological confirmation of needle tip position during ultrasound-guided interscalene block: a randomized comparison between the intraplexus and the periplexus approach. Can J Anaesth. 2015;62(12):1295–302.
Spence BC, Beach ML, Gallagher JD, Sites BD. Ultrasound-guided interscalene blocks: understanding where to inject the local anaesthetic. Anaesthesia. 2011;66(6):509–14.
Kreidler SM, Muller KE, Grunwald GK, Ringham BM, Coker-Dukowitz ZT, Sakhadeo UR, Baron AE, Glueck DH. GLIMMPSE: online power computation for linear models with and without a Baseline Covariate. J Stat Softw 2013, 54(10).
Thiebaut R, Jacqmin-Gadda H. Mixed models for longitudinal left-censored repeated measures. Comput Methods Programs Biomed. 2004;74(3):255–60.
Hansson P, Backonja M, Bouhassira D. Usefulness and limitations of quantitative sensory testing: clinical and research application in neuropathic pain states. Pain. 2007;129(3):256–9.
Reinhart DJ, Wang W, Stagg KS, Walker KG, Bailey PL, Walker EB, Zaugg SE. Postoperative analgesia after peripheral nerve block for podiatric surgery: clinical efficacy and chemical stability of lidocaine alone versus lidocaine plus clonidine. Anesth Analg. 1996;83(4):760–5.
Defrin RO, Ohry A, Blumen N, Urca G. Sensory determinants of pain. Brain. 2002;125:501–10.
Wilder-Smith OHT, Crul E, Ben JP, Arendt-Nielsen L. Quantitative sensory testing and human surgery: effects of analgesic management on postoperative neuroplasticity. Anesthesiology. 2003;98:1214–22.
Smet I, Vlaminck E, Vercauteren M. Randomized controlled trial of patient-controlled epidural analgesia after orthopaedic surgery with sufentanil and ropivacaine 0.165% or levobupivacaine 0.125%. Br J Anaesth. 2008;100(1):99–103.
Burckett-St Laurent D, Chan V, Chin KJ. Refining the ultrasound-guided interscalene brachial plexus block: the superior trunk approach. Can J Anaesth. 2014;61(12):1098–102.
Ivani G. Ropivacaine: is it time for children? Paediatr Anaesth. 2002;12(5):383–7.
Goveia CS, Magalhaes E. Ropivacaine in peribulbar anesthesia - vasoconstrictive properties. Rev Bras Anestesiol. 2010;60(5):495–512.
Soetens FM, Soetens MA, Vercauteren MP. Levobupivacaine-sufentanil with or without epinephrine during epidural labor analgesia. Anesth Analg. 2006;103(1):182–6. (table of contents).
Sinnott CJ, Cogswell IL, Johnson A, Strichartz GR. On the mechanism by which epinephrine potentiates lidocaine’s peripheral nerve block. Anesthesiology. 2003;98(1):181–8.
Rosenberg PH, Heinonen E. Differential sensitivity of A and C nerve fibres to long-acting amide local anaesthetics. Br J Anaesth. 1983;55(2):163–7.
Niemi G. Advantages and disadvantages of adrenaline in regional anaesthesia. Best Pract Res Clin Anaesthesiol. 2005;19(2):229–45.
Wittes J. Sample size calculations for randomized controlled trials. Epidemiol Rev. 2002;24(1):39–53.
Moloney NA, Hall TM, O’Sullivan TC, Doody CM. Reliability of thermal quantitative sensory testing of the hand in a cohort of young, healthy adults. Muscle Nerve. 2011;44(4):547–52.
Backonja MM, Walk D, Edwards RR, Sehgal N, Moeller-Bertram T, Wasan A, Irving G, Argoff C, Wallace M. Quantitative sensory testing in measurement of neuropathic pain phenomena and other sensory abnormalities. Clin J Pain. 2009;25(7):641–7.
Acknowledgements
Assistance with the study: Mrs. Annick Leroy for reviewing the statistical analysis. This manuscript has been edited by American Journal Experts.
Funding
Financial support and sponsorship: resources were provided from the Department of Anesthesiology only.
Author information
Authors and Affiliations
Contributions
LS conceived the study, participated in its design and coordination, performed the blocks, analyzed the QST results and wrote the manuscript. GH helped conceive the study design, performed the QST interpretation, helped in the analysis of the data, assisted in manuscript drafting and edited the various versions of the manuscript. TS helped in the analysis of the data, assisted in writing and reviewed the manuscript. SM assisted in writing and reviewing the manuscript. KW performed the statistical analysis. MB helped conceive the study design and performed a critical reading. CS performed QST testing and collected data. MV critically read the various versions of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Additional file 1
: All mixed model values of nerve blockage effects over time, per dermatome and per study group. Statistical methodology and P-values of the within/between-subject effects in the censored mixed effects model. (DOCX 73 KB)
Additional file 2
: Graphics of all neurosensitive/nociceptive responses. Time course of the neurosensory changes in detection thresholds for all sensations, Cold & Warm Sensation and Cold & Heat Pain (Temperature in °C) in the different dermatomes (C4, C5, C6, C7) for the 3 anesthetic solutions (0.5%Bup, 0.5%BupEpi, 0.75%Rop) measured with quantitative sensory testing (mean, standard deviation). The increases in thresholds are significant as compared to pre-injection thresholds. Detection thresholds between the 3 local anesthetics did not differ significantly. (DOCX 436 KB)
Rights and permissions
About this article
Cite this article
Sermeus, L.A., Schepens, T., Hans, G.H. et al. A low dose of three local anesthetic solutions for interscalene blockade tested by thermal quantitative sensory testing: a randomized controlled trial. J Clin Monit Comput 33, 307–316 (2019). https://doi.org/10.1007/s10877-018-0150-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-018-0150-3