Abstract
Objectives
The incidence of refeeding syndrome (RFS) in older patients is not well-known. The aim of the study was to determine the prevalence of known risk factors for RFS in older individuals during hospitalization at geriatric hospital departments.
Design and setting
342 consecutive older participants (222 females) who admitted at acute geriatric hospital wards were included in a cross-sectional study. We applied the National Institute for Health and Clinical Excellence (NICE) criteria for determining patients at risk of RFS. In addition, Mini Nutritional Assessment Short Form (MNA®-SF) was used to identify patients at risk of malnutrition. Weight and height were assessed. The degree of weight loss was obtained by interview. Serum phosphate, magnesium, potassium, sodium, calcium, creatinine and urea were analyzed according to standard procedures.
Results
Of 342 older participants included in the study (mean age 83.1 ± 6.8, BMI range of 14.7–43.6 kg/m2), 239 (69.9%) were considered to be at risk of RFS, in which 43.5% and 11.7% were at risk of malnutrition and malnourished, respectively, according to MNA-SF. Patients in the risk group had significantly higher weight loss, lower phosphate and magnesium levels. In a multivariate logistic regression analysis, low levels of phosphate and magnesium followed by weight loss were the major risk factors for fulfilling the NICE criteria.
Conclusion
The incidence of risk factors for RFS was relatively high in older individuals acutely admitted in geriatric hospital units, suggesting that, RFS maybe more frequent among older persons than we are aware of. Patients with low serum levels of phosphate and magnesium and higher weight loss are at increased risk of RFS. The clinical characteristics of the older participants at risk of RFS indicate that these patients had a relatively poor nutritional status which can help us better understand the potential scale of RFS on admission or during the hospital stay.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Refeeding syndrome (RFS) is a life-threatening complication which arises as a result of over-rapid or unbalanced nutritional support after a period of starvation or fasting (1, 2). This potentially lethal condition has been characterized as a clinical complex, which includes fatal shifts in fluid and electrolytes associated with metabolic abnormalities in malnourished patients or starved individuals undergoing refeeding whether orally, enterally or parenterally (1). The clinical symptoms of RFS cover a wide spectrum of conditions include fluid retention with peripheral oedema, congestive heart failure, cardiac arrhythmia, respiratory compromise, delirium, encephalopathy and other severe organ dysfunctions (3, 4). RFS usually arises within 2 to 5 days of starting to refeed (3, 5).
It is generally agreed that prevention, careful patient monitoring and management of RFS by the multidisciplinary nutrition team may help to mitigate RFS complications (5, 6). According to the guidelines of the National Institute for Health and Clinical Excellence (NICE) (7), for patients at high risk for RFS, nutrition repletion of energy should be started slowly, and then can be progressively increased to provide adequate nutrition demands over four to seven days (3-5). Using this strategy, a recent randomized clinical trial in 13 hospital intensive care units demonstrated a higher overall survival time and lower mortality in critically ill adults (8). In addition, correction of plasma electrolytes (i.e. phosphate, magnesium, potassium and sodium) and fluid imbalance along with refeeding as well as vitamin and trace-element deficiencies (i.e. thiamine) are recommended (3, 4).
Although, several risk factors for development of RFS have been identified, one of the predominant risk factor of the RFS is hypophosphatemia (2, 3). Prevalence of hypophosphatemia in patients at risk of RFS is high (9, 10). In a prospective cohort study of a heterogeneous group of intensive care unit (ICU) patients, Marik and Bedigian have shown that 34% of patients experienced refeeding hypophosphatemia soon after feeding was started (9). In another study of 106 cancer patients, the incidence of hypophosphatemia was 25% (10). Although this is important to emphasize, there are several causes of hypophosphatemia which are not necessarily associated to RFS (5). Other biochemical abnormalities of RFS are common comprising severely low serum electrolytes concentration of magnesium and potassium, disorders of sodium and fluid balance and thiamine deficiency (11, 12). In addition, acute and chronic malnutrition are the most important clinical risk factors for RFS. Hise et al (13) and Morley et al. (14) estimated that the prevalence of malnutrition in older hospitalized patients is between 30 to 50% and 35 to 65%, respectively.
Since there is no universally accepted definition of RFS, it is not surprising that the incidence of RFS is unknown and varies in different studies as wide as 0.4 – 34% (1, 4, 6). Hence, the guidelines of the NICE criteria are recognized as a useful tool for screening and identifying patients at high risk of developing RFS (7). In one recent study of 178 internal medicine patients, 97 patients (54%) were considered to be at risk of RFS and 14 patients actually developed RFS (11). However, the authors of that study applied NICE criteria for determining people at risk of RFS and they took hypophosphatasemia as the main indicator for the presence of this syndrome.
RFS has been confirmed in those with chronic alcoholism, individuals with anorexia nervosa, oncology patients receiving chemotherapy and depleted patients with acute illness (15-17). In addition, more specifically, the fast growing populations of hospitalized older subjects are known to be considered at high risk of RFS due to many underlying comorbidities and high prevalence of malnutrition as a consequence of dementia, dysphagia, depression and others (18-20). In one case-control study of hospitalized patients older than 65 years, Kagansky et al. reported that about 14.1% of 2307 older patients had hypophosphatemia compatible with the RFS on average on day 10 of hospitalization (21). In addition, other studies have found low serum phosphate and magnesium levels amongst older hospitalized patients (18, 22). RFS can be considered as a common reason of low serum phosphate and magnesium levels in older individuals due to significant overlap between risk factors for hypophosphatemia and hypomagnesemia and those for RFS (18).
On the other hand, RFS is likely underdiagnosed in older hospitalized persons and those in long-term care facilities due to nonspecific initial symptoms among this population (18, 23). Although pathophysiology of RFS has evolved, the potential dangers of refeeding and understanding the circumstances under which RFS arises in fragile older adults are less well known (24). Older patients often suffer from multi-comorbidity that overlaps with the typical symptoms of RFS which impairs the early recognition of RFS (24, 25). Whenever patients with RFS are not properly treated, the consequences can be fatal. Accordingly, identifying patients prone to RFS is essential due to minimizing its occurrence and avoiding mortality and morbidity related with this phenomenon (26).
Therefore, the aims of this study were i) to determine the prevalence of risk factors for RFS according to NICE criteria in older hospitalized patients aged 60-100 years and ii) to demonstrate the major clinical risk factors of RFS among this population.
Subjects and Methods
Study design and subjects
The study population consisted of 342 older participants (222 women and 120 men), aged between 60 and 100 years with a body mass index (BMI) range of 14.7–43.6 kg/m2 who consecutively hospitalized between July 2015 and February 2016. This cross-sectional study was performed at six different geriatric hospital departments in Germany. Exclusion criteria were age < 60 years, missing or withdrawn consent of the patients, hypercalcemia and hyperparathyroidism. The study protocol had been approved by the ethical committee of Friedrich-Alexander-University, Erlangen-Nürnberg.
NICE criteria have been applied for determining persons at high risk of RFS in all patients acutely admitted (Table 1) and subjects were grouped into two categories according to the guideline. First, subjects with at least one or more of the major parameter of NICE criteria were considered as positive NICE I. Second, subjects with two or more of the minor parameter of NICE criteria were considered as positive NICE II. In addition, Mini Nutritional Assessment Short Form (MNA®-SF) was used to identify patients at risk of malnutrition (27). Further, weight was measured without shoes and with light clothing at an accuracy of 0.01 kg and height was assessed to the nearest 0.5 cm at time of hospital admission. The degree of weight loss (WL) was obtained by interview. The medication histories at time of hospital admission were obtained either through interview or from the medication lists of the general practitioner.
Laboratory methods
Blood tests were performed on the day of admission at each hospital clinical chemistry laboratory and serum phosphate, magnesium, potassium, sodium, calcium, creatinine and urea were analyzed according to standard procedures. Serum phosphate level < 0.8 mmol/l was defined as hypophosphatemia as well as serum magnesium and potassium levels < 0.70 mmol/l and 3.5 mmol/l were considered as hypomagnesemia and hypokalemia, respectively.
Statistical analysis
The statistical analysis was performed with SPSS statistical software (SPSS Statistics for Windows, IBM Corp, Version 23.0, Armonk, NY, USA). Continuous variables are expressed by their means and standard deviations (SDs). Categorical variables are expressed as n (%). Differences between females and males and between patients at refeeding risk and not at refeeding risk were analyzed by using an unpaired t test in normally distributed variables. Categorical variables were compared by the Chi square test or the Fisher’s exact test, as appropriate. Multivariate logistic regression analyses were performed for identifying the clinical parameters that were independent risk factors for RFS (28). The independent variables included in the model were those variables that were significantly associated with NICE-refeeding risk criteria as dependent variable in univariate analysis: initial body weight, BMI, WL during first to six months, serum phosphate, magnesium and potassium levels, diuretics, no significant nutrition intake, antiacids and insulin therapy. The Hosmer and Lemeshow test were calculated for the goodness-of-fit of the logistic regression model. All tests were 2-tailed, and P<0.05 was accepted as the limit of significance.
Results
Baseline characteristics and laboratory data of study participants stratified by sex are presented in Table 2. Of 342 old participants, 65% of subjects were women. The age range was between 60 and 100 years. Women were significantly younger than men. According to MNA-SF, in total study population, the prevalence of the patients at risk of malnutrition and malnourished subjects were 44.7% and 11.1%, respectively.
The study population showed a wide BMI range with no sex differences (P=0.916). Compared with women, men had significantly higher actual body weight, height as well as WL during first, second, third and sixth months (WL ranged from 0 to 17.3% in females compared to range from 0 to 20.5% in males at sixth months; P <0.01). In addition, BMI less than 16 kg/m2 and 18.5 kg/m2 were observed in 1.2 % and 5.0% of the study population, respectively. There were no significant differences in all laboratory data between sexes, except for creatinine with lower values in females than males (P <0.01). In total population, 51 participants (14.9%) had hypophosphataemia of which 33 were females. Furthermore, prevalence of hypomagnesaemia and hypokalemia were 16.7% (57 subjects) and 10.8% (37 subjects), respectively (Table 2).
Diagnostic work-up for identifying patients at risk for RFS according to the guidelines of the NICE criteria in total study population are shown in Table 3. Using the criteria NICE I and NICE II (Table 1), diagnosis of risk factors for RFS was confirmed in 168 participants (49.1%) and 173 participants (50.6%), respectively. Based on NICE I, no significant nutritional intake for > 10d (21.3%) followed by hypomagnesaemia (16.7%) and hypophosphataemia (14.9%) were the most common risk factors of RFS. By contrast, diuretics (55.8%), no significant nutritional intake for > 5d (40.9%), and antiacids (39.5%) were the major determinants of risk factors for RFS according to NICE II. In addition, 32.2% of study participants (110 subjects) were at risk for RFS according to both criteria concurrently. With regards to this overlap, 69.9% of total study population (239 subjects) was considered to be at risk of RFS (Table 3).

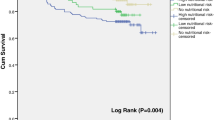
Descriptive characteristics and laboratory data of the study participants stratified by NICE criteria for determining people at high risk of RFS are given in Table 4. According to the NICE I and NICE II, patients at risk of RFS had significantly higher WL during the last 6 months (P < 0.01) than the patients not at risk of RFS, with no differences in age and BMI. In addition, based on MNA-SF, the prevalence of malnourished subjects was higher in refeeding risk groups compared to not at risk of RFS. Of 239 of older patients at risk of RFS, 43.5% and 11.7% were at risk of malnutrition and malnourished, respectively. Moreover, lower mean serum phosphate, magnesium and potassium levels were seen in patients at risk of RFS (Figure 1, P < 0.001), as expected considering the NICE I criteria.
A multivariate logistic regression analysis was performed for identifying the clinical parameters that were the important independent risk factors for RFS according to the NICE guideline (Table 5). Low levels of phosphate and magnesium followed by WL (in 3 months) were the major independent predictors for risk of RFS. In addition, low levels of potassium, diuretics and no significant nutrition intake were the other independents determinants for risk of RFS. Furthermore, age and gender do not impact the risk factors in NICE criteria (age, P=0.750; gender, P=0.840).
Discussion
The majority of older hospitalized patients are frail with several concomitant chronic conditions (29-32). Previous studies have shown the increased prevalence of multi-comorbidity with age (31, 32). RFS represents a potentially fatal condition which is considered to be a serious clinical problem, particularly, in the population of hospitalized older patients (1, 18). The actual prevalence of RFS is debatable possibility due to the absence of accepted diagnostic criteria, differences in definition used, study design and sample size (2, 9, 33). In addition, the incidence or risk of RFS is not well-known among geriatric patients because of significant overlap which exists between the symptoms of RFS and the symptoms of multi-comorbidity, resulting in poor recognition of RFS in older subjects. Accordingly, due to the lack of reliable RFS incidence data, preventing or minimizing its occurrence and identifying the high risk patients are crucial (4, 34).
To the best of our knowledge, there are very few studies exploring the incidence or risk of RFS in older patients acutely admitted to the geriatric hospital wards. As shown here and in previous studies (35, 36), many of older patients are malnourished or at risk of malnutrition, and therefore require nutrition therapy. When the risk of RFS is not properly identified or treated, this may lead to replacement of risk of malnutrition with risk of RFS. In this study, according to the NICE criteria, 69.9 % of the older patients were at risk of RFS suggesting that RFS maybe more frequent among geriatric patients than we are currently aware of. The high prevalence of risk factors found in the current study is in accordance with the recent study of internal medicine patients, in which 54% of participants were considered to be at risk of RFS (11). As reported by the National Confidential Enquiry into Patient Outcome and Death (NCEPOD) (37), 19% of those patients who meet the NICE risk criteria are expected to develop RFS. The recent study by Kraaijenbrink indicated that 14% of patients at risk of RFS actually developed the syndrome (11). Concurrently, Rio et al. found only a 1% prevalence of RFS among all hospital patients started on artificial nutrition (2). However, the incidence or risk of RFS depends on the degree of malnutrition and the feeding strategy which can therefore not be compared between studies.
In addition, our study demonstrates that older individuals at risk of RFS had significantly higher WL followed by lower levels of serum phosphate and magnesium. These data indicate that the refeeding risk group was in a relatively poor nutritional state that might assist in understanding the potential scale of RFS. Nutritional problems are numerous in geriatric patients and sometimes misdiagnosed (34, 38). Previous studies of hospitalized older subjects reported that 20% - 65% of this population experience nutritional deficiencies (36, 38-40) and the incidence of malnutrition in long-term care facilities is considered to be 30% - 60% (41). In a hospital based study of 32,837 patients, Imoberdof et al. (35) found that approximately one in five patients were severely undernourished or to be at risk of undernutrition and the risk was directly associated with age (age<45 y: 8%; 45-64 y: 11%; 65-84 y: 22%; >85 y: 28%). In the current study, in total study population, prevalence of the patients at risk of malnutrition and malnourished subjects were 63.1% and 31.9%, respectively. Consequently, the multi- morbidity and the relatively high age of our study participants may explain the higher number of the patients at risk of RFS.
Furthermore, hypomagnesemia and hypophosphatemia were common findings in our study population. About 16.7 % and 14.9 % of the patients were found to have hypomagnesemia and hypophosphatemia, respectively. The incidence of hypophosphatemia in our study population was similar with the 14.1% rate reported in a case-control study of older hospitalized patients (21) and almost half the rate (29%) reported in a cohort study of older hospitalized women (22). When a multivariate model was performed in our study, low levels of phosphate and magnesium followed by WL were the major independent risk factors for fulfilling the NICE criteria. However, hypophosphatemia is the hallmark of RFS, but its presence in our older patients is not necessarily meant that RFS would develop, since there are other possible reasons for low phosphate levels (18, 21). Recently Kraaijenbrink et al. found that of all 97 older patients at risk of RFS, 14 patients developed hypophosphatemia and consequently RFS (11).
Some limitations to the present study should be discussed. We did not address the real occurrence of RFS and it is not clear how many of the older patients at risk of RFS actually developed the syndrome. In addition, development of electrolyte disturbances over time and any type of nutritional therapy have not been assessed in our study. Therefore, future research is needed to provide detailed information of this syndrome and its occurrence in older patients to ascertain the best preventative strategies.
Conclusion
RFS is underestimated and is probably often underdiagnosed in a large proportion of geriatric patients with multiple comorbidities those who suffer from malnutrition and nutritional difficulties for several consecutive days (11, 34, 42). This study found that prevalence of risk factors for RFS is relatively high in older patients acutely admitted in geriatric hospitals, suggesting that, RFS maybe more frequent among older adults than we are aware of.
In this study, the clinical characteristics of the patients at risk of RFS, especially the associations of RFS with WL, hypophosphatemia, hypomagnesemia and other risk factors suggest that many of these older patients maybe are at increased risk of developing RFS. These findings revealed that the older patients at risk of RFS had a relatively poor nutritional state which may help the early identification of high-risk older individuals on admission or during the hospital stay and allow us to develop novel strategies in order to minimize risk of RFS among these patients. Our results indicate the need for better recognition and monitoring of hospitalized older patients at risk for the development of RFS.
Acknowledgments: With thanks to the working group on nutrition and metabolism of the German Geriatric Society (GGS) for the idea and discussion of the study design.
Conflicts of interest: The authors declare no conflict of interest.
Financial disclosure: The study received no financial support.
Ethical standard: The authors declare that the study procedures comply with current ethical standards for research involving human participants in Germany. The study protocol had been approved by the ethical committee of Friedrich-Alexander-University, Erlangen-Nürnberg.
Author contributions: The study was designed by all authors. Data were obtained by RW, IC, IG, CM, MKM and HPW. Statistical analysis was performed by MP. MP, DV and RW prepared the manuscript. All authors read and approved the final manuscript.
References
Solomon SM, Kirby DF. The refeeding syndrome: a review. JPEN Journal of parenteral and enteral nutrition. 1990;14(1): 90–7.
Rio A, Whelan K, Goff L, Reidlinger DP, Smeeton N. Occurrence of refeeding syndrome in adults started on artificial nutrition support: prospective cohort study. Bmj Open. 2013;3(1).
Mehanna HM, Moledina J, Travis J. Refeeding syndrome: what it is, and how to prevent and treat it. Brit Med J. 2008;336(7659): 1495–8.
Crook MA, Hally V, Panteli JV. The importance of the refeeding syndrome. Nutrition (Burbank, Los Angeles County, Calif). 2001;17(7-8):632–7.
Crook MA. Refeeding syndrome: Problems with definition and management. Nutrition (Burbank, Los Angeles County, Calif). 2014;30(11-12):1448-55.
Mehanna H, Nankivell PC, Moledina J, Travis J. Refeeding syndrome -awareness, prevention and management. Head Neck Oncol. 2009;1:4.
National Institute for Health and Care Excellence: Clinical Guidelines [Internet]. London: National Institute for Health and Care Excellence (UK);. 2003-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK11822/.
Doig GS, Simpson F, Heighes PT, Bellomo R, Chesher D, Caterson ID, et al. Restricted versus continued standard caloric intake during the management of refeeding syndrome in critically ill adults: a randomised, parallel-group, multicentre, single-blind controlled trial. Lancet Resp Med. 2015;3(12): 943–52.
Marik PE, Bedigian MK. Refeeding hypophosphatemia in critically ill patients in an intensive care unit -A prospective study. Arch Surg-Chicago. 1996;131(10): 1043–7.
Gonzalez Avila G, Fajardo Rodriguez A, Gonzalez Figueroa E. [The incidence of the refeeding syndrome in cancer patients who receive artificial nutritional treatment]. Nutricion hospitalaria. 1996;11(2): 98–101.
Kraaijenbrink BVC, Lambers WM, Mathus-Vliegen EMH, Siegert CEH. Incidence of refeeding syndrome in internal medicine patients. Neth J Med. 2016;74(3): 116–21.
Fernandez Lopez MT, Lopez Otero MJ, Alvarez Vazquez P, Arias Delgado J, Varela Correa JJ. Refeeding syndrome. Farmacia hospitalaria: organo oficial de expresion cientifica de la Sociedad Espanola de Farmacia Hospitalaria. 2009;33(4): 183–93.
Hise ME, Kattelmann K, Parkhurst M. Evidence-based clinical practice: dispelling the myths. Nutrition in clinical practice: official publication of the American Society for Parenteral and Enteral Nutrition. 2005;20(3): 294–302.
Morley JE. Pathophysiology of anorexia. Clinics in geriatric medicine. 2002;18(4):661-+.
Cumming AD, Farquhar JR, Bouchier IA. Refeeding hypophosphataemia in anorexia nervosa and alcoholism. British medical journal (Clinical research ed). 1987;295(6596): 490–1.
Telfer N, Persoff M. The Effect of Tube-Feeding on the Hydration of Elderly Patients. Journals of Gerontology. 1965;20(4): 536–43.
Boateng AA, Sriram K, Meguid MM, Crook M. Refeeding syndrome: Treatment considerations based on collective analysis of literature case reports. Nutrition (Burbank, Los Angeles County, Calif). 2010;26(2): 156–67.
Henderson S, Boyce F, Sumukadas D, Witham MD. Changes in Serum Magnesium and Phosphate in Older Hospitalised Patients-Correlation with Muscle Strength and Risk Factors for Refeeding Syndrome. J Nutr Health Aging. 2010;14(10): 872–6.
McMinn J, Steel C, Bowman A. Investigation and management of unintentional weight loss in older adults. Bmj-Brit Med J. 2011;342:d1732.
Bamia C, Halkjaer J, Lagiou P, Trichopoulos D, Tjonneland A, Berentzen TL, et al. Weight change in later life and risk of death amongst the elderly: the European Prospective Investigation into Cancer and Nutrition-Elderly Network on Ageing and Health study. J Intern Med. 2010;268(2): 133–44.
Kagansky N, Levy S, Koren-Morag N, Berger D, Knobler H. Hypophosphataemia in old patients is associated with the refeeding syndrome and reduced survival. J Intern Med. 2005;257(5): 461–8.
Sumukadas D, Jenkinson F, Witham MD. Associations and consequences of hypophosphataemia in older hospitalised women. Age and ageing. 2009;38(1): 112–5.
Dominguez LJ, Barbagallo M, Lauretani F, Bandinelli S, Bos A, Corsi AM, et al. Magnesium and muscle performance in older persons: the InCHIANTI study. American Journal of Clinical Nutrition. 2006;84(2): 419–26.
Khan LUR, Ahmed J, Khan S, MacFie J. Refeeding Syndrome: A Literature Review. Gastroent Res Pract. 2011;2011.
Hearing SD. Refeeding syndrome -Is underdiagnosed and undertreated, but treatable. Brit Med J. 2004;328(7445): 908–9.
Tresley J, Sheean PM. Refeeding Syndrome: Recognition Is the Key to Prevention and Management. Journal of the American Dietetic Association. 2008;108(12): 2105–8.
Rubenstein LZ, Harker JO, Salva A, Guigoz Y, Vellas B. Screening for undernutrition in geriatric practice: Developing the Short-Form Mini-Nutritional Assessment (MNA-SF). J Gerontol a-Biol. 2001;56(6):M366–M72.
Campbell M. Multiple logistic regression models—what are they? Midwifery. 2004;20(3): 236–9.
Karlamangla A, Tinetti M, Guralnik J, Studenski S, Wetle T, Reuben D. Comorbidity in older adults: Nosology of impairment, diseases, and conditions. J Gerontol a-Biol. 2007;62(3): 296–300.
Marengoni A, Winblad B, Karp A, Fratiglioni L. Prevalence of chronic diseases and multimorbidity among the elderly population in Sweden. American journal of public health. 2008;98(7): 1198–200.
Wolff JL, Starfield B, Anderson G. Prevalence, expenditures, and complications of multiple chronic conditions in the elderly. Archives of internal medicine. 2002;162(20): 2269–76.
Guralnik JM. Assessing the impact of comorbidity in the older population. Annals of epidemiology. 1996;6(5): 376–80.
Zeki S, Culkin A, Gabe SM, Nightingale JM. Refeeding hypophosphataemia is more common in enteral than parenteral feeding in adult in patients. Clinical Nutrition. 2011;30(3): 365–8.
Coutaz M. Delirium in malnourished elderly subjects: Could it be refeeding syndrome? European Geriatric Medicine. 2016;7(5): 434–7.
Imoberdorf R, Meier R, Krebs P, Hangartner PJ, Hess B, Staubli M, et al. Prevalence of undernutrition on admission to Swiss hospitals. Clinical Nutrition. 2010;29(1): 38–41.
Elmstahl S, Persson M, Andren M, Blabolil V. Malnutrition in geriatric patients: a neglected problem? Journal of advanced nursing. 1997;26(5): 851–5.
Outcome NCEiP, Stewart JAD, Outcome NCEiP, Staff D. A Mixed Bag: An Enquiry Into the Care of Hospital Patients Receiving Parenteral Nutrition: National Confidential Enquiry into Perioperative Deaths; 2010.
Wells JL, Dumbrell AC. Nutrition and aging: assessment and treatment of compromised nutritional status in frail elderly patients. Clinical interventions in aging. 2006;1(1): 67–79.
Sullivan D, Lipschitz D. Evaluating and treating nutritional problems in older patients. Clinics in geriatric medicine. 1997;13(4):753.
Hall K, Whiting SJ, Comfort B. Low nutrient intake contributes to adverse clinical outcomes in hospitalized elderly patients. Nutrition reviews. 2000;58(7): 214–7.
Rudman D, Feller AG. Protein-Calorie Undernutrition in the Nursing-Home. Journal of the American Geriatrics Society. 1989;37(2): 173–83.
Viana Lde A, Burgos MG, Silva Rde A. Refeeding syndrome: clinical and nutritional relevance. Arquivos brasileiros de cirurgia digestiva: ABCD = Brazilian archives of digestive surgery. 2012;25(1): 56–9.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pourhassan, M., Cuvelier, I., Gehrke, I. et al. Prevalence of Risk Factors for the Refeeding Syndrome in Older Hospitalized Patients. J Nutr Health Aging 22, 321–327 (2018). https://doi.org/10.1007/s12603-017-0917-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-017-0917-0