Abstract
Background
Malnutrition among older adults plays an important role in clinical and functional impairment.
Aims
The aim of our study was to evaluate all parameters of Mini-Nutritional Assessment (MNA), according to the nutritional status and to define the risk factors that may cause at risk of malnutrition and malnutrition in more detail.
Methods
One thousand outpatients aged 65 years or older who underwent the Comprehensive Geriatric Assessment (CGA) were included the study.
Results
A total of 1000 patients (men vs women; 27.1% vs 72.9%), of whom the mean age was 74.30 ± 8.28, were enrolled. We found that 6.6% of patients were malnourished, 31.6% of patients were at risk of malnutrition and 61.8% of patients were well-nourished. The mean MNA score was 23.71 ± 4.19. In patients with malnourished subgroup, the parameters that cause the most loss of points were self-perception of health (87.9%), protein intake (86.4%) and taking at least 3 medications per day (77.3%). At the risk of malnutrition subgroup, protein intake (86.7%), self-perception of health (74.7%) and taking at least 3 medications per day (65.2%) were the three parameters that cause the most loss of points.
Discussion
In the at-risk and malnourished subgroups, perception of health status, protein intake and taking at least three medications per day were the same MNA parameters that cause the most loss of points, but the rates were different.
Conclusions
A nutritional intervention should be done as soon as possible in patients who are at risk of malnutrition.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Aging is associated with progressive changes in biological, physiological, environmental and social conditions. Nutritional status is one of the conditions affected by aging. Nutritional status in the older people can be affected by many social situations such as being widowed, living alone, reduced budget, and difficulties with eating and supplies. And also, medicines used for chronic diseases may also cause a decrease in food intake. The physiological changes and social situations cause a metabolic stress on many organ systems, and may also affect nutritional needs. If the nutritional requirements are not met appropriately and adequately, malnutrition may occur [1].
Malnutrition is a highly relevant pathologic condition in the older people. It is associated with functional impairment, reduced quality of life, higher frequency of hospital admissions, and increased morbidity and mortality [2, 3]. Therefore, nutritional disorders are of special importance for the older people. In spite of its negative impact on clinical outcomes, awareness of malnutrition is still limited worldwide [4]. Nutritional status should be screened regularly and nutritional therapy should be administered as soon as possible in older adults [5].
The clinical evaluation of the nutritional status requires the investigation of the patient's medical history, anthropometric measurements, laboratory tests and dietary interviews. Therefore, it is a complex and time-consuming procedure [6]. And also, biochemical markers are time consuming and expensive, and the criteria for their interpretation in the older age are uncertain [7]. Some screening methods can only be performed by trained clinicians [7]. In the last two decades, significant progress has been made in diagnosing of malnutrition, mainly due to many studies investigating the use of Mini-Nutritional Assessment (MNA) [8,9,10,11]. MNA is a comprehensive tool, rapid and easy to perform by a healthcare professional, to facilitate the early detection of malnourished older people and those being at risk [12, 13]. Despite the simple and easy applicability of the MNA, patients with malnutrition are still poorly recognized by physicians [14].
For this reason, the present study sets out to obtain information which MNA parameters cause the most loss of points and to define the risk factors that may cause malnutrition and risk of malnutrition in detail.
Methods
Participants
A total of 1000 outpatients, who applied to a geriatric center between 2017 and 2018 and who had no exclusion criteria, were included in this prospective study. The criteria for inclusion were age 65 years or over, who applied to geriatric center for any reason, but not the entire community, and the ability to understand and answer questions. MNA was performed on all patients. The investigation conformed to the Declaration of Helsinki and approved by the local ethics committee, and verbal and written informed consent was obtained from all participants.
Exclusion criteria as follows:
-
Patients under 65 years of age.
-
Patients who refused to participate.
-
Patients who are hospitalized, live in nursing homes, or are in home-care programs.
-
Patients with moderate and severe cognitive impairment.
-
Patients requiring parenteral and/or enteral nutrition.
-
Patients who were not measured body weight or height.
-
Patients who have a history of severe illness that may lead to acute impairment of general health status, such as acute cerebrovascular event, gastrointestinal bleeding, sepsis, acute renal failure, acute coronary syndrome, acute liver failure, acute respiratory failure.
Mini-Nutritional Assessment
The MNA test is composed of simple measurements and 18 brief questions that can be completed in 15 min. The MNA consists of four parts: anthropometric measurements (four questions related to BMI, weight loss, MAC, and CC), global assessment (six questions related to lifestyle, medication, and mobility), dietary assessment (six questions related to number of meals, food and fluid intake, and autonomy of feeding), and subjective assessment (two questions related to self-perception of health and nutrition status). Each question/item is assigned certain points according to the answer. The total score is the sum of screening and assessment scores and ranges from 0 to 30 points. If the total score was > 23.5, 17–23.5, < 17, it was accepted that there was no malnutrition, risk of malnutrition, or malnutrition, respectively [5]. To calculate body mass index, height was measured to the nearest centimeter (cm) and weight was measured to the nearest half kilogram (kg) with the same stadiometer. MNA was performed in all participants even if their MNA-Short Form (SF) scores were 12. All data were collected by only one geriatrician to increase the reliability of the estimates. MNA was validated to screen malnutrition for Turkish geriatric patients in 2015 [15].
Statistical analyses
Data analyses were carried out using the Statistical Package for the Social Sciences 17. Descriptive statistics are reported as mean ± standard deviation for variables with a normal distribution, and the number of cases and percentage (%) for nominal variables. Demographic characteristics of participants were analyzed using descriptive statistics. When groups were present, the significance of differences between the groups in terms of averages was investigated by t test and in terms of median values was investigated by Mann–Whitney U test. When the number of groups was more than two, the significance of differences between the groups in terms of averages was investigated by the ANOVA test, post hoc ANOVA test and the significance of medians was determined by the Kruskal–Wallis test. Nominal variables were assessed by Pearson Chi-square. Identifying the risk factors for malnutrition, univariate and multiple logistic regressions were performed. Odds ratio (OR) was calculated with 95% confidence intervals. Significant variables at p < 0.05 were entered into multiple models and backward elimination was performed using Wald statistic to identify the independent risk factors. In all analyses, p < 0.05 was considered to indicate statistical significance.
Results
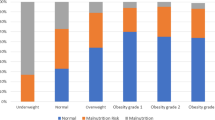
The overall characteristics of the 1000 patients included in the study are summarized in Table 1. The mean age was 74.3 ± 8.28 years, and there were 729 women (72.9%) and 271 men (27.1%). 618 participants (61.8%) had normal nutritional status, 316 patients were diagnosed with malnutrition risk (31.6%) and 66 patients were diagnosed with malnutrition (6.6%).
There was no difference in the patients with malnutrition, the risk of malnutrition, or normal nutrition in terms of the presence of marital status, living arrangement and serum albumin level (for each p > 0.05). There was a significant difference between the three groups in terms of age, sex, educational level, BMI and number of drugs used (for each p < 0.05). In malnutrition group, age (81.46 ± 9.27 years), female gender (71.2%) and low educational level (≤ 5 years) (97.9%) were higher than the other MNA subgroups, and also it is the group with the lowest BMI level (25.38 ± 6.59) (for each p < 0.05) (Table 1).
All participants’ responses to MNA questions were analyzed (Table 2). The frequencies of ‘0 points’ in the MNA questions revealed that 62.4% took at least 3 drugs per day, 37.8% did not consume protein products, 31.6% did not eat fruit/vegetables daily, 26.8% had neuropsychological problems, and 21.7% perception of health status was not as good. In all, 18% did not have more than 3 cups of fluid intake per day, and 15.5% suffered psychological stress/acute disease in the past 3 months. 14.2% reported a loss of weight of more than 3 kg during the preceding 3 months.
The answers given to the questions except the full score resulted in the loss of points, which resulted in low scores. In all three subgroups, the common question that causes the most points loss was of protein intake (p > 0.05). In patients with malnutrition subgroup, the parameters that cause the most loss of points were self-perception of health status (87.9%), protein intake (86.4%), taking at least 3 drugs per day (77.3%), fluid intake (63.6%) and weight loss (56.1%). At the risk of malnutrition subgroup; protein intake (86.7%), self-perception of health (74.7%), taking at least 3 medications per day (65.2%), number of full meals (53.2%) and fluid intake (49.7%) were the parameters that cause the most loss of points. Furthermore, the patients who lost points from the MNA parameters which were self-perception of nutrition status, MAC, taking at least 3 drugs per day, CC and mobility had a risk of malnutrition of 3.09, 2.89, 2.60, 2.53 and 1.86 times, respectively, compared to those who did not lose points (full score points) (Tables 3, 4).
There was no difference between MNA subgroups in the following questions: decrease in neuropsychological problems, pressure/skin ulcers, number of full meals, protein intake, fruit/vegetables intake (for each p > 0.05).
Discussion
In the present study, perception of health status, protein intake and taking at least three medications per day parameters caused the most loss of points in both at risk of malnutrition and malnourished subgroups. However, between these two subgroups, the rate of losing points from these three parameters was different. Among the all three subgroups, number of full meals, protein intake, fruit/vegetables intake, neuropsychological problems and pressure/skin ulcers were not significant. Furthermore, low MNA scores were significantly correlated with older age, lower BMI, female gender and low level of education.
Malnutrition, which may cause negative clinical of outcomes, is an important medical problem in Turkish geriatric population as well as in the worldwide [16]. Previous studies in Turkey have shown a high prevalence of malnutrition among the older population. In Saka et al. study which included 413 outpatients, malnutrition and at risk of malnutrition were found to be 13% and 31%, respectively [17]. In a multicenter study, which was conducted with 1030 outpatients, 19% were regarded as malnourished and 29.1% were at risk of malnutrition [18]. When other studies in our country were taken into consideration, the rate of malnutrition in our sample group was lower, while the risk of malnutrition was similar [18, 17, 19]. Additionally, in comparison to studies among community-dwelling, outpatients or home-care older people in developed countries, our study showed a lower prevalence of risk of malnutrition but higher rates of malnutrition [20,21,22,23]. The reason for the low rate of malnutrition in our study can be the sample that represents the healthier outpatients living in this area. Although the prevalence of malnutrition is less than in similar studies, the risk of malnutrition is very important, because in recent years, the risk of malnutrition is as important as malnutrition and has been shown to cause a large number of adverse clinical outcomes [24, 25].
Lower MNA scores were related to older age in our study. This result is consistent with some studies [26, 27]. Chewing/swallowing, oral health problems and reduced appetite together with the inability can lead to a reduced nutritional intake and thus to a poor nutritional status [28]. We observed some bad nutritional habits in older participants: higher carbohydrate intake (bread, rice, and vegetables), lower meat consumption, generally eating two meals a day. About half of the participants (47%) were eating two meals daily, in our study. In Kabir et al. study, malnutrition was observed in older people who ate two meals daily [29]. In another study, which was conducted in Turkey, the following data were obtained on daily energy consumption: 53.3% of the carbohydrates, 13.7% of the protein and 33% of the fat are provided [30]. In the same study, the consumption of milk and dairy products was 13%, fruits were 10%, vegetables were 6% and meat or poultry products was 6% [30]. When we analyze the question of ‘protein intake’ in more detail, the percentage of loss of points among the well-nourished, risk of malnutrition and malnutrition subgroups were 88.2%, 86.7% and 86.4%, respectively. Although there was a decrease in protein consumption in patients with risk of malnutrition and malnutrition, but it is noteworthy that there was not enough protein intake in patients with well-nourished. These findings may depend on the nutritional habits of the participants and the low socioeconomic level of our country. Furthermore, in a study conducted in our country, the frailty rate in older adults was found to be 31% [31]. This high prevalence may be the result of insufficient protein consumption in our country.
In our study, it was determined that BMI decreased gradually from the normal nutritional status group to the malnutrition group. This finding was observed in older people in other studies [21, 27]. Patients with malnutrition had lower BMI values, while in 17% of them BMI was ≥ 30 kg/m2. In other words, some of the patients with malnutrition were obese. It is not correct to assess the nutritional status according to the BMI alone. On the other hand, a patient could be thin with a low BMI but without malnutrition [5]. And also, it should be kept in mind that, as with a low BMI, the MNA is predictive of mortality [32, 33]. As determining the BMI in older people is often difficult, in this instance, CC can be replaced with BMI, and CC rescored from one point to three points.
In our study, there was no significant relationship between MNA subgroups and albumin levels. Albumin levels are nonspecific and could be low because of an underlying inflammatory process [34]. Mowe et al.’s study suggests that the decrease in nutritional intake occur before weight loss and a fall in serum albumin levels [28]. These changes currently used in clinical practice to assess nutritional status often appear too late to be useful nutritional markers [5]. Before severe changes in weight and albumin levels occur, MNA should be performed to evaluate nutritional status in older people. Such patients, especially with MNA score between 17 and 23.5, respond well to nutritional intervention.
The differences in our results may be due to differences arising from demographic characteristics. In rural areas, some of older individuals often do not know their own age. The family bonds are stronger in individuals with lower educational and income levels. Besides that, older people in Turkey usually live with their close relatives by tradition. Older people may consider their health status not as good, because of most of their daily living activities are done by young relatives.
Overall, the present study has some strong points. First, all data were collected by only one geriatrician to increase the reliability of the estimates. Second, the sample size was large. Finally, MNA long form was performed on all participants and the answers to all MNA questions were analyzed individually, and it was determined that participants had lost points from the questions at which rate. This study has some limitations. Only MNA was used to evaluate nutritional status of the patients and no other tests were performed. The cross-sectional nature of the study does not allow us to determine causality. The participants were recruited from only one city, the results in this study may not reflect data of the whole population.
Conclusion
We analyzed all MNA questions individually. Low MNA scores had a significant association with older age, lower BMI, female gender, low educational level, ‘not as good’ perception of health status, not consuming protein products and taking at least three medications per day. Besides, for the at-risk and malnourished groups, MNA parameters that cause the most loss of points were the same, but the rates were different. For this reason, a nutritional intervention should be done as soon as possible to patients who are at risk of malnutrition.
References
Ahmed T, Haboubi N (2010) Assessment and management of nutrition in older people and its importance to health. Clin Interv Aging 5:207–216
Donini LM, Felice MR, De Savina C et al (2011) Predicting the outcome of long-term care by clinical and functional indices: the role of nutritional status. J Nutr Health Aging 15:586–592
Pirlich M, Lochs H (2001) Nutrition in the elderly. Best Pract Res Clin Gastroenterol 15:869–884. https://doi.org/10.1053/bega.2001.0246
Muscaritoli M, Molfino A (2013) Malnutrition: the hidden killer in healthcare systems. BMJ (Clin Res ed) 346:f1547. https://doi.org/10.1136/bmj.f1547
Vellas B, Guigoz Y, Garry PJ et al (1999) The Mini Nutritional Assessment (MNA) and its use in grading the nutritional state of elderly patients. Nutrition (Burbank, Los Angeles County, Calif) 15:116–122
Omran ML, Salem P (2002) Diagnosing undernutrition. Clin Geriatr Med 18:719–736
Reuben DB, Greendale GA, Harrison GG (1995) Nutrition screening in older persons. J Am Geriatr Soc 43:415–425
Salva A (2010) Health and nutritional promotion program for patients with dementia (Nutrialz Study): design and baseline data. J Nutr Health Aging 14:78
Salva A, Coll-Planas L, Bruce S et al (2009) Nutritional assessment of residents in long-term care facilities (LTCFs): recommendations of the task force on nutrition and ageing of the IAGG European region and the IANA. J Nutr Health Aging 13:475–483
Vellas B, Guigoz Y, Baumgartner M et al (2000) Relationships between nutritional markers and the mini-nutritional assessment in 155 older persons. J Am Geriatr Soc 48:1300–1309
Vellas B, Villars H, Abellan G et al (2006) Overview of the MNA—its history and challenges. J Nutr Health Aging 10:456–463 (discussion 463–455)
Guigoz Y, Vellas B, Garry PJ (1996) Assessing the nutritional status of the elderly: the Mini Nutritional Assessment as part of the geriatric evaluation. Nutr Rev 54:S59–65
Bauer JM, Kaiser MJ, Anthony P et al (2008) The Mini Nutritional Assessment—its history, today's practice, and future perspectives. Nutr Clin Pract 23:388–396. https://doi.org/10.1177/0884533608321132
Volkert D, Saeglitz C, Gueldenzoph H et al (2010) Undiagnosed malnutrition and nutrition-related problems in geriatric patients. J Nutr Health Aging 14:387–392
Sarikaya D, Halil M, Kuyumcu ME et al (2015) Mini nutritional assessment test long and short form are valid screening tools in Turkish older adults. Arch Gerontol Geriatr 61:56–60. https://doi.org/10.1016/j.archger.2015.04.006
Granic A, Mendonca N, Hill TR et al (2018) Nutrition in the very old. Nutrients. https://doi.org/10.3390/nu10030269
Saka B, Kaya O, Ozturk GB et al (2010) Malnutrition in the elderly and its relationship with other geriatric syndromes. Clin Nutr (Edinb, Scotl) 29:745–748. https://doi.org/10.1016/j.clnu.2010.04.006
Gunduz E, Eskin F, Gunduz M et al (2015) Malnutrition in community-dwelling elderly in turkey: a multicenter, cross-sectional study. Med Sci Monit Int Med J Exp Clin Res 21:2750–2756. https://doi.org/10.12659/msm.893894
Ulger Z, Halil M, Kalan I et al (2010) Comprehensive assessment of malnutrition risk and related factors in a large group of community-dwelling older adults. Clin Nutr (Edinb, Scotl) 29:507–511. https://doi.org/10.1016/j.clnu.2010.01.006
de Groot L, Beck AM, Schroll M et al (1998) Evaluating the DETERMINE Your Nutritional Health Checklist and the Mini Nutritional Assessment as tools to identify nutritional problems in elderly Europeans. Eur J Clin Nutr 52:877. https://doi.org/10.1038/sj.ejcn.1600658
Soini H, Routasalo P, Lagstrom H (2004) Characteristics of the Mini-Nutritional Assessment in elderly home-care patients. Eur J Clin Nutr 58:64–70. https://doi.org/10.1038/sj.ejcn.1601748
Buffa R, Floris G, Lodde M et al (2010) Nutritional status in the healthy longeval population from Sardinia (Italy). J Nutr Health Aging 14:97–102
Salva A, Andrieu S, Fernandez E et al (2009) Health and nutritional promotion program for patients with dementia (NutriAlz Study): design and baseline data. J Nutr Health Aging 13:529–537
Kocyigit SE, Soysal P, Ates Bulut E et al (2018) Malnutrition and malnutrition risk can be associated with systolic orthostatic hypotension in older adults. J Nutr Health Aging 22:928–933. https://doi.org/10.1007/s12603-018-1032-6
Slee A, Birch D, Stokoe D (2016) The relationship between malnutrition risk and clinical outcomes in a cohort of frail older hospital patients. Clin Nutr ESPEN 15:57–62. https://doi.org/10.1016/j.clnesp.2016.06.002
Vedantam A, Subramanian V, Rao NV et al (2010) Malnutrition in free-living elderly in rural south India: prevalence and risk factors. Public Health Nutr 13:1328–1332. https://doi.org/10.1017/s1368980009991674
Donini LM, Poggiogalle E, Molfino A et al (2016) Mini-nutritional assessment, malnutrition universal screening tool, and nutrition risk screening tool for the nutritional evaluation of older nursing home residents. J Am Med Dir Assoc 17:959.e911–958. https://doi.org/10.1016/j.jamda.2016.06.028
Mowe M, Bohmer T, Kindt E (1994) Reduced nutritional status in an elderly population (%3e 70 y) is probable before disease and possibly contributes to the development of disease. Am J Clin Nutr 59:317–324. https://doi.org/10.1093/ajcn/59.2.317
Kabir ZN, Ferdous T, Cederholm T et al (2006) Mini Nutritional Assessment of rural elderly people in Bangladesh: the impact of demographic, socio-economic and health factors. Public Health Nutr 9:968–974
Arslan P, Mercanligil S, Ozel H (2006) Nutritional habits and nutritional patterns of participants of the Turkish Adult Risk Factor Survey 2003–2004. Arch Turk Soc Cardiol 34:331–339
Soysal P, Isik AT, Arik F et al (2018) Validity of the Mini-Nutritional Assessment Scale for evaluating frailty status in older adults. J Am Med Dir Assoc. https://doi.org/10.1016/j.jamda.2018.07.016
Luchsinger JA, Patel B, Tang MX et al (2008) Body mass index, dementia, and mortality in the elderly. J Nutr Health Aging 12:127–131
Chan M, Lim YP, Ernest A et al (2010) Nutritional assessment in an Asian nursing home and its association with mortality. J Nutr Health Aging 14:23–28
Reuben DB, Moore AA, Damesyn M et al (1997) Correlates of hypoalbuminemia in community-dwelling older persons. Am J Clin Nutr 66:38–45. https://doi.org/10.1093/ajcn/66.1.38
Funding
None of the authors received any funding for this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study design and all procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (Ethics Committee of Erciyes University Health Application and Research Center Hospital - 2017/405) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Human and animal rights disclosure
This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kalan, U., Arik, F., Isik, A.T. et al. Nutritional profiles of older adults according the Mini-Nutritional Assessment. Aging Clin Exp Res 32, 673–680 (2020). https://doi.org/10.1007/s40520-019-01235-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-019-01235-1