Abstract
Objectives
The aim of this study was to investigate the association between the videofluoroscopic (VFS) signs of impaired efficacy (pharyngeal residue) and safety (aspiration) swallowing and the clinical/nutritional status of patients with suspect of dysphagia.
Design
A cross-sectional study was conducted with patients submitted to videofluoroscopy.
Setting and Participants
Data of 76 patients were analyzed between March 2011 and December 2014.
Measurements
The clinical history and VFS exams of patients ≥ 38 years were retrospectively analyzed.
Results
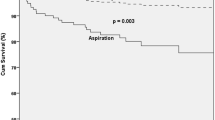
88% patients presented Oropharyngeal Dysphagia (OD), 44.7% presented laryngeal penetration and 32% presented aspiration. 78% patients presented pharyngeal residue. Aspiration was associated with Head Neck Cancer (HNC) [Prevalence Ratio (PR): 2.27, p = 0.028] and cardiovascular disease (PR 1.96, p = 0.027). Underweight [Body Mass Index < 18.5 kg/m2] was not associated with the presence of aspiration. Underweight patients with OD had a higher prevalence rate of pharyngeal residue than those normally nourished (100% vs. 78%) (PR 1.34, p = 0.011). Pharyngeal residue was associated with male sex (PR 1.32, p = 0.040), neurodegenerative disease (PR 1.57, p = 0.021), stroke (PR 1.62, p = 0.009), cerebral palsy (PR 1.76, p = 0.006) and HNC (PR 1.73, p = 0.002).
Conclusion
In the present study, neurologic diseases, HNC, male sex and underweight were associated to impaired swallowing efficacy. Underweight, independently of the other variables, was not associated with impaired swallowing safety.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Oropharyngeal dysphagia (OD) is a symptom that involves changes in the oral, pharyngeal or esophageal phases of swallowing and is associated with different adverse health conditions (1). The International Classification of Diseases (ICD), published by the World Health Organization (WHO), recognizes OD as a symptom of the digestive system (#782.2 and R13.10) (1).
Prevalence rates of OD are 37% and 78% of stroke survivors in the acute and chronic phases, respectively (2). Regarding neurodegenerative diseases (NDD), 82% of patients with Parkinson’s Disease (PD) are symptomatic for OD (3) and 25% of patients with amyotrophic lateral sclerosis have dysphagia (4). After chemotherapy/radiotherapy for head and neck cancer (HNC), 40 to 85% of patients experience OD (5). Moreover, altered swallowing function is found in 37.5% of patients with chronic obstructive pulmonary disease (COPD) (6).
In addition to disease-related dysphagia, swallowing function can be altered due to the physiological changes stemming from aging (7). Older adults have slower swallowing mechanisms, lower extension of the hyoid-larynx complex during swallowing and shorter closure laryngeal time, which implies impaired protection of the airways (8). Systematic review with eight studies, five theirs was conducted in the first seven days following stroke and three studies were managed during the rehabilitation phase. This study showed that stroke survivors with dysphagia have a 2.4-fold greater chance of suffering from underweight compared with those without dysphagia (9). Thus, it is important to investigate whether the efficacy and/or swallowing safety are associated with nutritional status and whether it is possible to develop appropriate strategies by adjusting the diet and hydration of patients with dysphagia (10).
OD can impair both the efficacy and swallowing safety. Efficacy is the ability to ingest all food (calories and nutrients) and water necessary for adequate nourishment and hydration (3, 11). Signs of impaired efficacy can be the presence of oral and/or pharyngeal residue (12). Swallowing safety is the ability to ingest all needed food (calories and nutrients) and water with no respiratory complications, such as respiratory infections and aspirate pneumonia (3, 11). Signs of impaired safety are laryngeal penetration, when the bolus enters into the larynx that does not pass below the vocal folds and/or tracheobronquial aspiration, when the bolus passes below the level to vocal folds (12).
Aim
The aim of this study was to investigate the association between the videofluoroscopic (VFS) signs of impaired efficacy (pharyngeal residue) and safety (aspiration) swallowing and the clinical/nutritional status of patients with suspect of dysphagia.
Methods
Study Design and Participants
A cross-sectional study with patients of the radiology sector of the Federal University of Santa Catarina hospital (Brazil) between March 2011 and December 2014. The study was approved by the Human Research Ethics Committee of the UFSC (#24862813.8.0000.0121) and it is registered with the Brazilian Registry of Clinical Trials (RBR-2FBQP5 and UTN: U1111-1161-5468). The informed consente was obtained from patients.
The initial sample was made up of 173 patients. Thirtysix patients were excluded for being under 19 years of age and 61 were excluded due to incomplete information on their medical charts regarding clinical or nutritional data. Thus, the final sample comprised 76 patients. Median age of the sample was 63 years (63 years [interquartil range (IQR) = 55.0 to 73.3 percentile]), 58% were male and 46% were hospitalized. The following were the diagnoses with indication for videofluoroscopy: degenerative disease (n = 17, 22%): Parkinson’s disease (n = 8), amyotrophic lateral sclerosis (n = 6), myasthenia gravis (n = 2) and Machado-Joseph disease (n = 1), COPD (n = 16, 21%), stroke (n = 15, 20%), HNC (n = 10, 13%), gastroesophageal disorder (n = 8, 11%): hiatus hernia (n = 2), erosive gastritis (n = 2), esophageal cancer (n = 1) and esophagitis (n = 3), neurological trauma (n = 6, 8%): head trauma (n = 4), firearm wound (n = 1 ) and spine/ spinal cord injury (n = 1), sepsis/septic shock (n = 3, 4%) and cerebral palsy (n = 1, 1%). The most common comorbidities were systemic arterial hypertension (n = 28, 37%), a history of previous pneumonia (n = 22, 29%), diabetes mellitus (n = 22, 29%), cardiovascular disease (n = 21, 27%) and dyslipidemia (n = 15, 20%).
Videofluoroscopy
The exams were performed with the Precision RX (General Electrics, São Paulo, SP, Brazil) following the standard protocol of the university hospital (13). Opti-Bar® 67% barium contrast (Alko, Taquara, RJ, Brazil) was diluted up to 30% with water to obtain liquid consistencies of nectar, honey and pudding, following the guidelines of the National Dysphagia Diet (2002) (14). The thickener utilized was the Thick & Easy® (Fresenius Kabi, Barueri, SP, Brazil), with the following volumes: free drink, 5 mL, 10 mL and 20 mL. Solid food intake was tested with crackers. The presence of contrasted material in the valleculae or pyriforms sinus after the first swallow was considered indicative of pharyngeal residues (15). Laryngeal penetration and aspiration were investigated (11) and classified by Rosenbeck Scale (16). Oral intake was classified based on the Functional Oral Intake Scale (FOIS) (17).
Nutritional diagnosis
Body mass index (BMI) was obtained from weight and height measurements (18), and classified by WHO (2006) (19), as underweight (mild thinness, moderate thinness and severe thinness) (BMI < 18.5 kg/m2), normal weight (≥ 18.5 kg/m2 BMI ≤ 24.99 kg/m2), overweight and obesity (BMI > 25 kg/m2) (19).
Statistical analysis
The Shapiro-wilk test was used to determine the normality and homogeneity of the data. The data were expressed as median and (IQR) (25 to 75 percentile) when the distribution was asymmetric as well as frequency (%). Poisson regression analysis was used to determine associations among the variables swallowing disorders and the clinical and nutritional status. It was considering dependent variables the residue pharyngeal and the aspiration. Independent variables were age: ≥ 70 years old, < 70 years of age, sex, stroke, cerebral palsy, NDD, sepsis/septic shock, COPD, neurological trauma, gastroesophageal disorder, diabetes mellitus, cardiovascular disease, dyslipidemia, systemic arterial hypertension, history of pneumonia and nutritional status: underweight, overweight/obesity and normal weight range. The backward stepwise method was used for variable selection. Variables that presented statistical significance p-value < 0.20 according to Wald’s test were maintained in the model. In the final model, variables with a two-tailed p < 0.05 were considered to be associated with the outcome. The SPSS program, version 16.0 (College Station, TX Stata Corporation) was used for the statistical analysis.
Results
Swallowing and Nutritional Characteristics
The prevalence of OD was 88%, laryngeal penetration was 45% and aspiration was diagnosed in 32% of patients. The Rosenbeck scale (16) was the median score of laryngeal penetration and aspiration was 1.5 (1.0 to 6.0). Pharyngeal residue was diagnosed in 78% of patients: in valleculae (11%), pyriformis sinus (4%) and both (63%). It was classified as mild (33%), moderate (17%) or severe (28%). The median score on the FOIS was 6.0 (3.0 to 7.0).
Median BMI was 22.9 kg/m2 (IQR = 19.9 - 27.7 percentile). Thirty-six patients (47%) were classified in the normal weight range, 30 (40%) were classified as overweight/obesity and ten (13%) were classified as underweight: severe thinness (n = 3), moderate thinness (n = 4) and mild thinness (n = 3).
Association between pharyngeal residues and clinical/nutritional status
In the adjusted model, after controlling for other variables, it was observed that 100% of patients with underweight had pharyngeal residue versus 78% of normal weight [Prevalence Ratio (PR) adjusted 1.34, p = 0.011]. Only one of patients with underweight was fully released orally (FOIS = 7), the others found themselves with restricted food intake by mouth. In addition, underweight patients 30% showed pharyngeal residue in mild, 20% in moderate and 50% in severe degree. Moreover, pharyngeal residue was associated with male sex (PR adjusted 1.32, p = 0.040), NDD (PR adjusted 1.57, p = 0.021), stroke (PR adjusted 1.62, p = 0.009), cerebral palsy (PR adjusted 1.76, p = 0.006) and HNC (PR adjusted 1.73, p = 0.002). In the adjusted analysis, no significant associations were found between neurological trauma, diabetes mellitus and pharyngeal residue (Table 1).
Association between aspiration and clinical/nutritional status
In the adjusted analysis, after controlling for the other variables, aspiration was associated with HNC (PR) adjusted 2.27, p = 0.028) and patients with cardiovascular disease (PR adjusted 1.96, p = 0.027), but not with underweight. Patients with overweight/obesity had, on average, 0.34 less pharyngeal residue (p = 0.021). Age, COPD, Systemic Arterial Hypertension were not association to aspiration (Table 2).
Discussion
The main findings of the present study were the association between underweight and impaired swallowing efficacy as well as the absence of an association between underweight and swallowing safety. A previous study suggests that malnutrition is likely associated with a reduction in food intake due to difficulty swallowing (20). Two other recent studies report evidence of the relationship between malnutrition and dysphagia (21, 22). In a multi-center cross-sectional study conducted in Spain (PREDyCES®) involving 1597 cases, dysphagia was found 20.5% of patients and was identified as a factor for the development of malnutrition (Nutrition Risk Scale – NRS-2002® screening test ≥ 3, BMI < 18.5 kg/m2) [adjusted odds ratio (OR) = 1.85 (95% CI: 1.38-2.50), p = 0.002] (23). In a study conducted by Kim and Byeon (2014) involving 261 acute stroke survivors (67.2 ± 13.4 years), those with severe dysphagia had significantly low protein levels (p = 0.031) seven days after admission to the stroke unit (24). Similarly, other authors found a strong correlation between OD and malnutrition; moreover, the clinical severity score of dysphagia was 325.6 ± 12.3 points among patients with normal nutritional status and 529 ± 34.5 points in patients classified using the Subject’s Global Assessment as “B” (mildly malnourished or suspected of malnutrition) or “C” (severely malnourished ) (p < 0.05) (11).
The association between malnutrition and dysphagia was described in a study with 1662 hospitalized older patients (62% female; mean age: 85.1 ± 6.2 years). The Mini-Nutritional Assessment (MNA®) demonstrated that 45.3% of patients with OD were malnourished compared 18% of those without OD (p < 0.001) and that dysphagia was a strong factor for malnutrition (MNA® scores lower than 17 were considered indicative of malnutrition) (MNA® < 17, OR: 12.6, 95% CI: 7.49-21.2); moreover, patients with OD had lower BMI scores (25.5 ± 5.3 vs. 26.8 ± 5.1, p < 0.001) (25).
Likewise, impaired swallowing efficacy may be related to underweight/malnutrition, as malnutrition or poor nutritional status is a marker of a population highly susceptible to acquiring infection due to the fact that malnutrition depresses the immune system. Malnutrition negatively affects muscle function, such as respiratory muscles, and delays or prevents adequate recovery (26). In cases of impaired swallowing efficacy, residue in spaces between the tongue base and epiglottis (valleculae) may be present due to the reduction in the tongue propulsion force (15). Other factors, such as residue in the pyriform sinus, can impair pharyngeal clearance (15). Changes in the opening of the upper esophageal sphincter may also be associated with pharyngeal residue (27).
One of the few studies to investigate the relationship between specific swallowing disorders (pharyngeal residue) and nutritional status followed 224 older adults and found a high prevalence rate of individuals either ‘malnourished or at risk of malnutrition’, which was associated with basal signs of impaired swallowing efficacy (OR = 2.73, p = 0.015) (28). In a multicenter study involving 63 patients diagnosed with post-stroke OD, vallecular residue (OR = 3.56, p = 0.001) and pharyngeal recesses (OR = 9.08, p = 0.001) upon admission increased the chance of aspiration six months after a stroke (29).
Regarding clinical conditions, the male sex was associated with the presence of pharyngeal residue in the present study. While signs of efficacy have not been associated with sex, a greater occurrence of OD has been reported among males (4, 30). An association between signs of impaired efficacy and neurological problems, such as neurodegenerative diseases, stroke and cerebral palsy, was found in this study. These findings are in agreement with data from a similar study, in which the authors found pharyngeal residue in 53% of the patients, which was associated with unsafe swallowing (p < 0.001) (31). Likewise, increased oropharyngeal residue is a common radiological finding in patients with Parkinson’s disease (32). In a previous study involving 29 children with cerebral palsy, vallecular residue was found in 82.7% of patients and residue in the pyriformis sinus was found in 37.9% of patients (33).
In the present study, impaired swallowing efficacy and safety were associated with head and neck cancer. A previous study reports the presence of pharyngeal residue in 20% of patients (54 ± 9 years) with oral and oropharyngeal cancer treated with chemotherapy and surgery, assessed using videofluoroscopy (34). As changes in the safety of swallowing in cases of head and neck cancer lead patients to a tendency toward initiating swallowing by interrupting the inspiratory phase of the breathing cycle, such patients have more severe airway invasion and swallowing impairment in comparison to those with a more stable pattern (35).
No association was found between pharyngeal residue and neurological trauma in the present investigation. However, a prospective study with a 12-month follow-up involving patients with severe traumatic brain injury assessed the acute phase of the process (time of admission and one month after the injury) and found impaired efficacy (presence of pharyngeal residue) (36). Regarding comorbidities, no association was found between pharyngeal residue and diabetes mellitus, as observed in previous studies involving hospitalized patients with dysphagia (21, 37). Nonetheless, diabetes mellitus is associated with vascular complications and neuropathies (38), which are risk factors for OD (2).
In relation to swallowing safety, aspiration was not associated with underweight (BMI < 18.5 kg/m2) in the present study, which is in agreement with data reported in an investigation involving older adults with impaired swallowing safety (MNA® < 17, OR = 2.04, 95% CI 0.84-4.95, p = 0.110) (39). However, other authors have pointed out that patients with aspiration exhibit poor nutritional status based on the MNA® (p = 0.004) as well as poor outcomes regarding swallowing safety (p = 0.010) (30). In the same study, malnutrition was associated with mortality within one year in older adults with pneumonia and was closely associated with oropharyngeal dysphagia (30).
Patients aged 70 years or older had not a higher prevalence rate of aspiration in the present study. This result is not in agreement with data reported in a prospective cohort study involving older adults, which found an older mean age among patients with OD (p < 0.001) discharged from the acute geriatric unit (40). We not found association between age and aspiration. Indeed, older individuals have a higher prevalence rate of OD (p < 0.001) (39). It has recently been shown that older adults hospitalized with acute disease have a 47.4% prevalence rate of OD and the chance of OD is higher among those aged > 85 years (OR = 1.6) (21). In other study, the risk of dysphagia was related to an increased likelihood of malnutrition at an older age, even after adjusting for covariables (MNA® ≤ 7, PR = 1.30, 95% CI: 1.01-1.67) (41). Moreover, OD and aspiration are prevalent in older adults with pneumonia (55%), leading a worse prognosis and a greater risk of mortality when associated with comorbidities, impaired clinical status and malnutrition (8). Swallowing disorders can lead to the prescription of alternative feeding methods (gastrostomy and nasogastric feeding tube), which can be contribute to the risk of aspiration pneumonia. In a study recent involving patients aged ≥ 60 years with dysphagia and advanced dementia (classified as at least 7A according to the Functional Assessment Staging Test), the six-month follow up revealed that significantly more patients in the alternative feeding group (n = 18, 58.1%) had a diagnosis of aspiration pneumonia in comparison to the oral feeding group (n = 9, 25.0%) (p = 0.006) (42). Moreover, it is not yet clear in the literature, which one (gastrostomy and nasogastric feeding tube) would offer best the better benefit (43).
In the present study, the COPD was not associated with aspiration. The literature reports that changes in the breathing pattern may influence the coordination of swallowing and respiration synchrony, thereby affecting the protection of the lower airways (44). Cardiovascular diseases were associated with aspiration, which is agreement with data reported by Cabré et al. (2013) (40), who found prevalent ischemic heart disease among patients with OD (61%; p < 0.001) (40). These associations may be explained by the pathological mechanism directly related to respiratory impairment, contributing to respiratory difficulty and altering the coordination of swallowing mechanisms (45).
No association was found between systemic arterial hypertension and aspiration, which is agreement with the findings of a previous study involving comorbidities in 32 patients hospitalized with dysphagia (p = 0.724) (37).
The limitations of the present study should be taken into account. First, the use of a non-probabilistic sample does not allow the extrapolation of the findings to other populations. Moreover, it is possible that the statistical analysis did not have sufficient power to find significant differences among the variables due to the small number of participants. Another limitation regards the cross-sectional design, which does not allow the establishment of causal relationships. Nonetheless, this preliminary investigation can contribute to future studies on impaired swallowing efficacy (presence of pharyngeal residue) and impaired swallowing safety (changes due to the occurrence of aspiration). Moreover, clinical/nutritional status should be conducted with probabilistic samples and further future studies are needed to confirm the association between specific markers of swallowing disorders and nutritional status assessed using other means rather than only the BMI.
In the present study, neurologic diseases, head and neck cancer, the male sex and underweight were associated to impaired swallowing efficacy. In contrast, underweight was not associated with impaired swallowing safety independently of the other variables.
Aknowledgments: We thank the financial support in the form of scholarships to: Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) to OLIVEIRA and GONÇALVES, the Fundo de Apoio a Manutenção e ao Desenvolvimento da Educação Superior (FUMDES) de Santa Catarina to de FREITAS and the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) to MOREIRA.
Financial Disclosure: None declared
Conflict of Interest: None
Declaration: This study received approval from the local institutional review board of Federal University of Santa Catarina (#24862813.8.0000.0121) and it is registered with the Brazilian Registry of Clinical Trials (RBR-2FBQP5 and UTN: U1111-1161-5468). The informed consent was obtained.
References
World Health Organization. International Classification of Disease (ICD). http:// www.who.int/classifications/icd/en/. Accessed July 20 2014.
Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke 2009;36(12):2756–2763.
Kalf G, de Swart BJM, Bloem B R, Munneke M. Prevalence of oropharyngeal dysphagia in Parkinson’s disease: A meta-analysis. Parkinsonism Relat Disord 2012;18(4):311–315. doi: 10.1016/j.parkreldis.2011.11.006.
Trail M, Nelson N, van JN, Appel SH, Lai EC. Major stressors facing patients with amyotrophic lateral sclerosis (ALS): a survey to identify their concerns and to compare with those of their caregivers. Amyotroph Lateral Scler Other Motor Neuron Disord 2004;5(1):40–45.
Francis DO, Weymuller EA Jr., Parvathaneni U, Merati AL, Yueh B. Dysphagia, stricture, and pneumonia in head and neck cancer patients: does treatment modality matter? Ann Otol Rhinol Laryngol 2010;119(6):391–397.
Cvejic L, Harding R, Churchward T et al. Laryngeal penetration and aspiration in individuals with stable COPD. Respirology 2011;16(2):269–275. doi: 10.1111/j.1440-1843.2010.01875.x
Ney DM, Weiss JM, Kind AJ, Robbins J. Senescent swallowing: impact, strategies, and interventions. Nutr Clin Pract 2009;24(3):395–413. doi: 10.1177/0884533609332005.
Rofes L, Arreola V, Romea M et al. Pathophysiology of oropharyngeal dysphagia in the frail elderly. Neurogastroenterol Motil 2010;22(8):851–858. doi: 10.1111/j.1365-2982.2010.01521.x.
Foley NC, Martin RE, Salter KL, Teasell RL. A review of the relationship between dysphagia and malnutrition following stroke. J Rehab Medic 2009;41(9):707–713.
Jensen GL, Mirtallo J, Compher JC et al. Adult starvation and disease-related malnutrition: a proposal for etiology based diagnosis in the clinical practice setting from the International Consensus Guideline Committee. Clin Nutr 2010;29(2):151–153. doi: 10.1016/j.clnu.2009.11.010.
Clavé P, de Kraa M, Arreola V et al. The effect of bolus viscosity on swallowing function in neurogenic dysphagia. Aliment Pharmacol Ther 2006;24(9):1385–1894.
Logemann JA. Dysphagia-evaluation and treatment. Folia Phoniatr Logop 1995;47(3):140–164.
Furkim AM, Duarte ST, Soria FS et al. Avaliação de segurança da deglutição. In: Susanibar F, Parra D, Dioses A. Tratado de evaluación de motricidad orofacial y áreas afines. 1th edn. Madrid, Spain, 2014;pp 225–231.
National Dysphagia Diet Task Force. National Dysphagia Diet: Standardization for Optimal. Care American Dietetic Association, Chicago, Illinois, 2002.
Eisenhuber E, Schima W, Schober E et al. Videofluoroscopic assessment of patients with dysphagia: pharyngeal retention is a predictive factor for aspiration. Am J Roentgenol 2002;178(2):393–398.
Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia 1996;11(2):93–98.
Crary MA, Man E, Groher ME. Initial psychometric assessment of a functional oral intake scale for dysphagia in stroke patients. Arch Phys Med Rehabil 2005;86(8):1516–1520.
World Health Organization 1995. Expert committee on physical status: the use and interpretation of anthropometry. Physical status: the use and interpretation of anthropometry. Technical Report Series nº854.
World Health Organization 2006. Body mass index classification. http://who.int/bmi/index.jsp?introPage=3.html. Accessed 20 October 2014.
Lorefält B, Granérus A-K, Unosson M. Avoidance of solid food in weight losing older patients with Parkinson’s disease. J Clin Nurs 2006;15(11):1404–1412.
Carrión S, Cabre M, Monteis R, Roca M, Palomera E, Clavé P Association between oropharyngeal dysphagia and malnutrition in elderly patients with acute diseases admitted to a general hospital. Clin Nutr 2015;34(3):436–442. doi: 10.1016/j.clnu.2014.04.014.
Alvarez-Hernandez J, Leon-Sanz M, Planas Vila M, Araujo K, Garcia de Lorenzo A, Celaya-Pérez S, On behalf of the PREDyCESR researchers. Prevalence and costs of malnutrition in hospitalized dysphagic patients: a subanalysis of the PREDyCES® study. Nutr Hosp. 2015;32(4):1830–1836. doi:10.3305/nh.2012.27.4.5986.
Alvarez-Hernandez J, Planas Vila M, Leon-Sanz M et al. PREDyCES researchers. Prevalence and costs of malnutrition in hospitalized patients; the PREDyCES Study. Nutr Hosp 2012;27(4):1049–1059. doi: 10.3305/nh.2012.27.4.5986.
Kim S, Byeon S. Comparison of nutritional status indicators according to feeding methods in patients with acute stroke. Nutr Neurosc 2014;17(3):138–144.
Carrión S, Cabre M, Monteis R et al. Oropharyngeal dysphagiais a prevalent risk factor for malnutrition in a cohort of older patients admitted with an acute disease to a general hospital. Clin Nutr. pii: 2014;S0261-5614(14):00122-00128. doi: http://dx.doi.org/10.1016/j.clnu.2014.04.014
Rofes L, Arreola V, Almirall J. Diagnosis and management of oropharyngeal dysphagia and its nutritional and respiratory complications in the elderly. Gastroenterol. Res. Pract. 2011; doi:10.1155/2011/818979 818979.
Shaker R, Easterling C, Kern M et al. Rehabilitation of swallowing by exercise in tube fed patients with pharyngeal dysphagia secondary to abnormal UES opening. Gastroenterology 2002;122(5):1314–1321.
Serra-Prat M, Palomera M, Gomez C et al. Oropharyngeal dysphagia as a risk factor for malnutrition and lower respiratory tract infection in independently living older persons: a population-based prospective study. Age Ageing 2012;41(3):376–381.
Han TR, Paik NJ, Park JW, Kwon BS. The prediction of persistent dysphagia beyond six months after stroke. Dysphagia 2008;23(1):59–64.
Cabré M, Serra-Prat M, Palomera E, Almirall J, Pallares R, Clavé P. Prevalence and prognostic implications of dysphagia in elderly patients with pneumonia. Age Ageing 2010;39(1):39–45. doi: 10.1093/ageing/afp100.
Molfenter MS, Steele CM. The relationship between residue and aspiration on the subsequent swallow: an application of the normalized residue ratio scale. Dysphagia 2013;28(4):494–500. doi: 10.1007/s00455-013-9459-8.
Leopold NA, Kagel MC. Prepharyngeal dysphagia in Parkinson’s disease. Dysphagia 1996;11(1):14–22.
Kim JS, Han ZA, Song DH, Oh HM, Chung ME. Characteristics of dysphagia in children with cerebral palsy, related to gross motor function. Am J Phys Med Rehabil 2013;92(10):912–919. doi: 10.1097/PHM.0b013e318296dd99.
de Bruijn MJ, Rinkel RN, Cnossen IC et al. Associations between voice quality and swallowing function in patients treated for oral or oropharyngeal cancer. Support Care Cancer 2013;21(7):2025–2032. doi: 10.1007/s00520-013-1761-3.
Brodsky MB, McFarland DH, Dozier TS et al. Respiratory-swallow phase patterns and their relationship to swallowing impairment in treated oropharyngeal cancer. Head Neck 2010;32(4):481–489. doi: 10.1002/hed.21209.
Terré R, Mearin F. Evolution of tracheal aspiration in severe traumatic brain injury-related oropharyngeal dysphagia: 1-year longitudinal followup study. Neurogastroenterol Motil 2009;21(4):361–369. doi: 10.1111/j.1365-2982.2008.01208.x.
Bassi D, Furkim AM, Silva CA et al. Identification of risk groups for oropharyngeal dysphagia in hospitalized patients in a university hospital. CoDAS 2014;26(1):17–27.
Weckbach S, Findeisen HM, Schoenberg SO et al. Systemic cardiovascular complications in patients with long-standing diabetes mellitus: comprehensive assessment with whole-body magnetic resonance imaging/magnetic resonance angiography. Invest Radiol 2009;44(4):242–250. doi: 10.1097/RLI.0b013e31819a60d3.
Serra-Prat M, Hinojosa G, Lopez D et al. Prevalence of oropharyngeal dysphagia and impaired safety and ef?cacy of swallow in independently living older persons. J Am Geriatr Soc 2011;59(1):186–187. doi: 10.1111/j.1532-5415.2010.03227.x.
Cabré M, Serra-Prat M, Force LL, Almirall J, Palomera E, Clavé P. Oropharyngeal dysphagia is a risk factor for readmission for pneumonia in the very elderly: observational prospective study. J Gerontol A Biol Sci Med Sci 2013;69(3):330–337. doi:10.1093/gerona/glt099.
Takeuchi K, Aida J, Ito K, Furuta M, Yamashita Y, Osaka T. Nutritional status and dysphagia risk among community-dwelling frail older adults. J Nutr Health Aging 2014;1;8(4):352–357. doi: 10.1007/s12603-014-0025-3.
Cintra MT, de Rezende NA, de Moraes EN, Cunha LC, da Gama Torres HO. A comparison of survival, pneumonia, and hospitalization in patients with advanced dementia and dysphagia receiving either oral or enteral nutrition. J Nutr Health Aging 2014;18(10):894–899. doi: 10.1007/s12603-014-0487-3.
Jaafar MH, Mahadeva S, Morgan K, Tan MP. Percutaneous endoscopic gastrostomy versus nasogastric feeding in older individuals with non-stroke dysphagia: a systematic review. J Nutr Health Aging 2015;19(2):190–197. doi: 10.1007/s12603-014-0527-z.
Kijima M, Isono S, Nishino T. Coordination of swallow phases of respiratory during added respiratory loads in awake subjects. Am J Respir Crit Care Med 1999;159(6):1898–1902.
Chaves RD, Carvalho CRF, Cukier A, Stelmach R, Andrade CRF. Symptoms of dysphagia in patients with COPD. J Bras Pneumol 2011;37(2):176–183.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Oliveira, D.L., Moreira, E.A.M., de Freitas, M.B. et al. Pharyngeal residue and aspiration and the relationship with clinical/nutritional status of patients with oropharyngeal dysphagia submitted to videofluoroscopy. J Nutr Health Aging 21, 336–341 (2017). https://doi.org/10.1007/s12603-016-0754-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-016-0754-6