Abstract
In this study, Lactobacillus plantarum F-10, a promising probiotic strain isolated from fecal microbiota of healthy breastfed infant, was assessed as a bio-control strategy for wound infections. Pseudomonas aeruginosa PAO1/ATCC 27853, methicillin-resistant Staphylococcus aureus ATCC 43300, and their hospital-derived strains isolated from skin chronic wound samples were used as important skin pathogens. The cell-free extract (CFE) of the strain F-10 was shown to inhibit the growth of all pathogens tested, while no inhibition was observed when CFE was neutralized. The strain displayed no hemolysis and exhibited a strong auto-aggregating phenotype (51.48 ± 1.45%, 5 h) as well as co-aggregation. Antibiotic resistance profile was found to be safe according to the European Food Safety Authority. Biofilm formation was measured by crystal violet assay and visualized with scanning electron microscopy and confocal laser scanning microscopy. One hundred percent reduction in biofilm formation of all pathogens tested was obtained by sub-MIC value (12.5 mg/ml) of CFE following 24-h co-incubation. Inhibition of quorum sensing–controlled virulence factors (motility, protease and elastase activity, production of pyocyanin and rhamnolipid) of P. aeruginosa strains was also observed. DPPH radical scavenging activity of the CFE was determined as 88.57 ± 0.49%. In conclusion, our results suggest that L. plantarum F-10 may represent an alternative bio-control strategy against skin infections with its antimicrobial, anti-biofilm, anti-quorum sensing, and antioxidant activity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The process of wound healing is ever more dangerous, complex, and requires a range of clinical skills and knowledge [1]. In recent years, the growing prevalence and incidence of non-healing wounds with infection as well as inflammation stages are a worrying global concern with its enormous social and economic implications worldwide. The incidence of wounds in the EU-27 is approximately 4 million and further 2 million patients acquire nosocomial infections each year [2]. While the cost of a problematic wound care is between €6650 and €10,000 per patient, the total cost constitutes the 2–4% of European healthcare budgets [3]. Besides these economic costs, delayed healing process in wound cases affects the quality of patients’ life as well as leads to their psychological isolation in the society [4]. Therefore, it is regarded as important to treat the wound cases as soon as possible. However, one of the biggest challenges for wound care is the risk of infection which causes a delayed wound healing that urgently needs to be controlled to facilitate the management [5].
Infections, developed in any type of wound and resulted in local and systemic host responses, can be defined as multiplication of bacteria that impair the wound healing process through the mechanisms such as the formation of biofilm, production of metabolic products and toxins, downregulation of immune response, and releasing of free radicals [6]. Many species of bacteria are implicated in wound infection. The most common ones are multiresistant Staphylococcus aureus and Pseudomonas aeruginosa [7]. These important pathogens are located in the first order of hospital-borne infections all over the world and have become increasingly widespread and global threats in developing countries since the day they first emerged [8]. Many different antibiotic-based approaches have been developed against these pathogens. However, it is a well-known fact that most antibiotics are broadly acting, killing, or preventing the growth of both good and bad bacteria and opening the door for drug-resistant microbes to cause infection. Therefore, the spread of multiple drug-resistant bacteria indicates a growing need for new products especially including natural materials, as an alternative to diagnose and treat resistant infections as well as reduce the use of antibiotic-based medicines in human health. Recently, some studies focus on alternative therapies such as honey, essential oils, and anti-microbial dressings [9]. In addition, one of the emerging trends in wound care research is the use of probiotics as a suitable, safe, and natural medication alternative for the patients.
Probiotics, defined as live microorganisms that confer health benefits when taken in adequate amounts, are receiving renewed attention in the medical fields [10]. Although numerous studies have demonstrated the importance of probiotics and their potential therapeutic effects within the gut [11], very few studies have been undertaken in the skin health, to date. Recent studies have been shown that probiotics have therapeutic potential in terms of prevention of skin infections with fighting against drug-resistant bacteria by producing potent antimicrobial substances (bacteriocins, bacteriocin-like metabolites, organic acids, and H2O2), inhibiting the biofilm formation of the pathogens as well as their quorum-sensing activity in long-term periods [12].
Our current study was undertaken to determine the potential effects of Lactobacillus plantarum F-10, a promising probiotic strain isolated from fecal microbiota of healthy breastfed infant, against bacterial human skin pathogens. To clarify the potential value of the strain, its antimicrobial, anti-biofilm, and anti-quorum sensing and antioxidant activities were analyzed.
Materials and Methods
Bacterial Strains and Growth Conditions
In this study, Lactobacillus plantarum F-10 isolated from fecal microbiota of healthy breastfed infant and identified by molecular methods based on 16S rRNA gene sequence analysis in our previous studies was used as a promising probiotic strain. The strain was activated using 10% (v/v) inoculum in Man, Rogosa, and Sharpe (MRS) medium for 24 h at 37 °C under static conditions and was sub-cultured twice prior to use. P. aeruginosa PAO1/ATCC 27853, methicillin-resistant S. aureus (MRSA) ATCC 43300, and their hospital-derived clinical isolates (CI) from skin chronic wound samples were used as important skin pathogens and were grown in TSB (Tryptic Soy Broth) medium for 24 h at 37 °C. All bacterial strains were preserved in 50% glycerol at − 80 °C. Unless otherwise stated, all laboratory materials, mediums, chemicals, and reagents were purchased from Fisher Scientific Ltd. (Loughborough, UK) or Oxoid (Basingstoke, UK).
Determination of Hemolytic Activity
Hemolytic activity and the antibiotic resistance of L. plantarum F-10 have been determined within the safety criteria of probiotic strains. An overnight culture of the strain F-10 was streak plated on Columbia agar (BioMerieux, France) containing 5% (w/v) sheep blood and incubated for 24 h at 37 °C. Pathogen bacteria were used as controls. Following the incubation, clear zones around the colonies were considered as β-hemolytic while the bright green zones as α-hemolytic and the absence of the zone as γ-hemolytic [13].
Determination of Antibiotic Resistance
The antibiotic susceptibility of the strain F-10 was investigated for nine different antibiotics (kanamycin, ampicillin, vancomycin, streptomycin, gentamicin, erythromycin, tetracycline, chloramphenicol, and clindamycin) as determined by EFSA (European Food Safety Authority) by disk diffusion (Kirby-Bauer Disc Susceptibility Test) and minimum inhibitory concentration (MIC) assays. For the disc diffusion method, the cell density of the overnight culture was adjusted to McFarland 0.5 and then spread plated on MRS agar plates. Different antibiotic discs were placed on agar surface at appropriate intervals and the inhibition zones formed around the antibiotic discs were measured following the incubation of 24 h at 37 °C [14]. The MIC values were determined according to the Clinical and Laboratory Standards Institute by the “microtitre plate assay” method [15]. Each well in the microtiter plate contained 200 μl MRS broth with twofold dilutions of antibiotics (1024–0.25 mg/l) and the overnight culture of the strain, adjusted to McFarland 0.5. Wells containing only bacteria but not antibiotics were used as positive control, while only MRS were used as negative control. The microtiter plates were incubated 24 h at 37 °C. Following the incubation, bacterial growth was measured spectrophotometrically at 620nm using a Dynatech microplate reader. Antibiotic susceptibility was defined on the microbiological breakpoints data categorizing bacteria as resistance, determined by EFSA [16].
Assessment of Antimicrobial Activity
In order to determine the antimicrobial activity of L. plantarum F-10 against the most common pathogens in wound infections, the efficacy of viable cells, culture supernatants recovered following the centrifugation and filtration through 0.22-μm filters (cell-free extract; CFE preparation), and its neutralized form with 8 M NaOH to pH 7 (neutralized filtrate; CFEn preparation) was used. The activity was assessed by the method of agar well diffusion [17]. Pathogen bacteria, grown in TSB for 24 h at 37 °C, were adjusted to McFarland 0.5, inoculated in soft agar, and then pour plated on agar surfaces. Viable cells, CFE, and CFEn samples were transferred as 50 μl into the 6-mm-diameter wells opened on agar surfaces and incubated 24 h at 37 °C. MRS medium was used as negative control. Following the incubation, the diameter of the inhibition zones around the wells was measured as millimeter. In addition, the retention of activity in the CFE following the exposure of heat (100 °C for 15 min) and enzymes (proteinase K, amylase, and catalase 1 mg/ml) was evaluated as described by Bhunia et al. [18].
MIC values of the lyophilized CFE (100–1.56 mg/l) against all pathogens tested were determined by using microtiter plate assay as described before [15].
Determination of Lactic Acid Production
Lactic acid production of L. plantarum F-10 was determined using a commercial kit according to the manufacturer’s instruction (Megazyme, International Ireland Ltd.).
Determination of Exopolysaccharide Production
Exopolysaccharide (EPS) of L. plantarum F-10 was investigated with the two forms of EPS as release (EPSr) and cell-bound (EPSb). An overnight culture of the strain F-10 was heated for 15 min at 100 °C then centrifuged at 15.000 rpm for 15 min. Trichloroacetic acid (20%) was added to the supernatant and incubated for 2 h at 4 °C under the shaking conditions. Following the centrifugation in 4 °C at 25.000 rpm for 20 min, 95% ethanol was added to the supernatant in 2× volume and incubated for overnight under the 4 °C conditions. After the incubation period, samples were centrifugated in 4 °C at 6.000 rpm for 30 min, and the pellet containing the EPSr was suspended with ddH2O and was stored in 4 °C for further analysis [19].
For the extraction of EPSb, an overnight culture of the strain F-10 was centrifugated in 4 °C at 15.000 rpm for 15 min. Pellet was washed with phosphate-buffered saline (PBS) twice and re-suspended in 1 M NaCl solution. Cells were sonicated at 40 W for 3 min in 4 °C and then centrifugated in 4 °C at 6.000 rpm for 30 min. Absolute ice-cold ethanol was added to the obtained supernatant in 2× volume and incubated overnight under the 4 °C conditions. After the incubation period, samples were centrifugated in 4 °C at 6.000 rpm for 30 min, and the pellet containing the EPSb was suspended with ddH2O and was stored in 4 °C for further analysis [19]. Quantitative determination was evaluated by the phenol-sulfuric acid method of Dubois et al. [20], using glucose as a standard.
Auto-aggregation and Co-aggregation Assay
Auto-aggregation and co-aggregation assays were achieved according to Del Re et al. [21], and Kos et al. [22]. An overnight culture of the strain F-10 was centrifugated in 4 °C at 6.000 rpm for 30 min, and the pellet was washed with PBS three times then re-suspended in the same buffer to give an OD of 0.5 (620nm). The cell suspension was mixed for 10 s and incubated for 5 h at room temperature. The auto-aggregation was determined by taking 1 ml sample of the upper suspension into a cuvette and measuring the absorbance at 620nm. The equation used to calculate the percentage of auto-aggregation was [1 − (At/A0) × 100] (A, absorbance; t, hours). The protocol was also carried out for each pathogen. For the co-aggregation assay, equal volumes of F-10 cells and pathogens were mixed and incubated for 5 h at room temperature without agitation. Following the incubation, the absorbance of the suspension’s upper phase was measured at 620nm, and the percentage of co-aggregation was calculated with the formula of [(Ax + Ay)/2] − A(x + y)]/Ax + Ay/2 (A, absorbance; x, F-10; y, pathogen). Auto-aggregation and co-aggregation were also visualized using light microscopy (Olympus) and scanning electron microscopy (SEM, Zeiss, EVO 40) according to Kiran et al. [23].
Assessment of Anti-biofilm Forming Activity
Biofilm formation was measured by crystal violet assay. For this purpose, polystyrene-based 96 well microplates (LP Italiana) were used. An overnight culture of the strain F-10 and pathogens were adjusted to McFarland 0.5 and added to the microplate wells. Following the 24-h incubation at 37 °C, biofilm biomass by adherent bacteria was quantified upon removal of medium, washing with PBS, and staining with crystal violet (0.1%). Biofilm-bound dye was recovered with acetone:ethanol (30:70, Meck) solution, and each biomass was quantified by measuring the absorbance at 595nm. Mediums without bacteria were used as negative controls. The biofilm production capabilities of the strains were evaluated by calculating the “cut off” values [24, 25].
Before the inhibition assays, the ideal conditions for the biofilm formation of each pathogenic strain was determined on the basis of crystal violet binding. Modified TSB medium with different concentrations of glucose (0.5–3%) was used for P. aeruginosa strains while TSB medium containing 3% NaCl prepared with different concentrations of glucose (0.5–3%) was used for MRSA strains. Following the 24-h incubation, the biofilm formations of the strains were assessed as described before. The conditions resulted in the highest biofilm formation were selected for each strain and used for further analysis.
For the anti-biofilm-forming activity of the strain F-10, three different approaches including co-incubation, eradication, and pre-treatment were carried out. Viable cells of the strain F-10, sub-MIC value of its lyophilized CFE, as well as EPSs were used as active ingredients. In the co-incubation approach, pathogen strains adjusted to McFarland 0.5 were co-incubated with each active ingredient (1:1), separately. For eradication assay, pathogenic bacteria were grown in microplate wells for 24 h at 37 °C. Then, wells were aspirated and planktonic cells were removed. The active ingredients were added to each well. For the pre-treatment assay, active ingredients were added to the microplate wells and incubated 3, 6, 9, and 12 h under room temperature. Following each incubation period, active ingredients were removed and each well washed with PBS, then pathogen bacteria adjusted to McFarland 0.5 were added to each well, separately. In all assays, medium without bacteria was used as a negative control while medium containing only the pathogens as positive controls. For all assays, biofilm formation was checked as described before, after 24-h incubation at 37 °C. Inhibition of biofilm formation was calculated as percentage inhibition with the formula of [(C − B) − (T − B)]/[(C − B)] × 100 (C, well including the pathogen; B, well including the medium; T, well including the pathogen and active ingredient together). The best results obtained from three assays were repeated on glass made coverslips and visualized with SEM [23] and confocal laser scanning microscopy. LIVE/DEAD BacLight Bacterial Viability Kit (Thermo Fisher) was used to determine the cell viability for the confocal laser scanning microscopy according to the user manual. Imaging was performed with a Leica TCS SP5 II confocal microscope, using a × 20 oil-immersion lens with 477 nm excitation and 560–600 nm emission range.
Co-incubation and pre-treatment assays were also carried out on the coupons made from stainless steel surfaces to determine the cell viability within the biofilms. Following the treatments, coupons were washed twice with PBS and then air-dried. Homogenization was obtained by speed vortexing of the coupons with the glass beads (r 3 mm) for 1 min. Samples were serially diluted and spread plated on TSA plates. After 48-h incubations at 37 °C, cell viability in the biofilms was calculated as logarithmic reduction [26].
Assessment of Anti-quorum Sensing Activity
For the assessment of anti-quorum sensing activity of the sub-MIC value of CFE, P. aeruginosa strains were used with their well-known QS activity. LB agar plates containing 1%, 0.5%, and 0.3% agar, supplemented with or without CFE, were used for determining the effect on twitching, swarming, and swimming mobility of strains spotted on the surface, respectively. Plates were analyzed after incubation of 24 h at 37 °C [27].
Pyocyanin was extracted by the method of Ramos et al. [28]. Following the 24-h incubation of the strains in LB medium supplemented with or without the sub-MIC value of CFE, the organic phase was obtained by adding 3 ml chloroform into the 5 ml culture. The solution was mixed with 1 ml 0.2 M HCl and then centrifugated at 8.000 rpm for 10 min. Pyocyanin-rich organic layer was removed and its absorbance was measured spectrophotometrically at 520nm. The amount of pyocyanine (μg/ml) was calculated as the multiplication of obtained wavelength with 17.072 (molar extinction coefficient, ε). For rhamnolipid production, strains were spotted on an M9 glutamate minimal agar supplemented with or without CFE. Following the incubation for 24 h at 37 °C, the clear zone around the growing bacteria was accepted as a sign of rhamnolipid activity and its diameter was measured as millimeter [29].
To determine the proteolytic activity, strains were spotted on the middle of the LB agar surfaces containing 2% skim milk supplemented with or without CFE. Following the incubation for 24 h at 37 °C, proteolytic activity was measured by the diameter of the clear zone surrounding the bacterial growth [30]. Elastase activity was measured by elastin congo red (ECR) assay according to Yin et al. [31]. The strains were inoculated into the LB medium supplemented with or without CFE and incubated for 24 h at 37 °C. The culture broth was centrifugated at 4500 rpm for 5 min. One hundred microliters of supernatant was mixed with 900 μl ECR solution (100 mM Tris,1 mM CaCl2, 20 mg elastin congo red, pH 7.5), and then incubated 3 h at 37 °C. Insoluble ECR was obtained after the centrifugation at 1500 rpm for 10 min and its absorbance was measured at 495nm for elastase activity.
Assessment of Antioxidant Activity
The total phenolic content in the CFE of the strain F-10 was determined using the spectrophotometric method of Singleton and Rossi [32]. The reaction was prepared by mixing 100 μl of CFE in different concentrations, and 100 μl of 50% Folin-Ciocalteu’s reagent dissolved in water. Following the incubation in darkness at room temperature for 3 min, 2 ml NaHCO3 (2%) was added to the reaction. Different gallic acid concentrations (0.05, 0.1, 0.15, 0.2, 0.3 mg/ml) were used as phenolic standard and MRS was used as blank. The color change after 30-min incubation in similar conditions was analyzed by spectrophotometric measurements at 750nm wavelength. Based on the measured absorbance, the concentration of phenolics was read (mg/ml) from the calibration line; then, the content of phenolics in the extract was expressed in terms of gallic acid equivalent (mg of GA/g of CFE).
The total amount of flavonoid substances in the CFE of the strain F-10 was determined using the ammonium chloride colorimetric method of Zhishen et al. [33]. The reaction was prepared by mixing 100 μl of CFE in different concentrations, 300 μl ethanol, 20 μl AlCl2 (10%), 20 μl 1 M sodium acetate, and 560 μl ddH2O. Different quercetin concentrations (0.025, 0.05, 0.1, 0.15, 0.2 mg/ml) were used as flavonoid standard and MRS was used as blank. Following the incubation in darkness at room temperature for 30 min, the absorbance was determined using spectrophotometer at 425nm and the concentration of flavonoids was read (mg/ml) on the calibration line.
The ability of the CFE of the strain F-10 to scavenge 2,2-diphenyl-1-picrylhydrazyl (DPPH) free radicals was assessed by the method of Blois [34]. The reaction was prepared by mixing 200 μl of CFE in different concentrations, 500 μl 120 μM DPPH in ethanol, and 500 μl ethanol. Different gallic acid concentrations (0.05, 0.1, 0.15, 0.2, 0.3 mg/ml) were used as standard and MRS was used as blank. Following the incubation in darkness at room temperature for 30 min, the absorbance was determined using spectrophotometer at 517nm. Percentage inhibition was calculated using the equation of [(Acontrol − Asample)/Acontrol] × 100 (A, absorbance), while IC50 value was estimated from the percentage inhibition versus concentration plot, using a non-linear regression algorithm.
Statistical Analysis
All assays were carried out with three independent experiments performed in triplicate and data were analyzed using SPSS version 19.0 (IBM, New York, NY, USA), by one-way analysis of variance (ANOVA) followed by Tukey’s post hoc test and unpaired t test (GraphPad Prism v.3.0, GraphPad Software, San Diego, CA, USA). All results were presented as a mean ± standard deviation. A p value of less than 0.05 was used to indicate a significant difference.
Results
Hemolytic Activity and Antibiotic Susceptibility
L. plantarum F-10 had no clear transparent or greenish zone on the blood agar plates, surrounding the colonies, and thus was found γ-hemolytic or non-hemolytic. The antibiotic susceptibility test results for the strain of F-10 were shown in Table 1. The strain was found resistant to gentamicin and kanamycin antibiotics, while susceptible to the rest of the antibiotics tested.
Antimicrobial Activity
Screening for the potential antagonistic activity of L. plantarum F-10 against the important skin pathogens was performed using the agar well diffusion assay. Overall, the results with CFE of the strain F-10 demonstrated powerful antimicrobial activity on all selected microorganisms tested in this work, with the greatest inhibition as follows: 18 ± 2.1 mm for MRSA ATCC 43300, 16 ± 2.1 mm for MRSA CI, 19 ± 0.7 mm for P. aeruginosa PAO1/ATCC 27853, and 18 ± 2.8 mm for P. aeruginosa CI, respectively (Fig. 1). Overall, results were summarized in Table 2 which was shown that there was no significant difference (p > 0.05) in the size of inhibition zones from the point of each pathogen and also between the viable cells and CFE of the strain.
The minimum inhibitory concentration (MIC) for CFE was determined as 25 mg/l for all pathogens tested and sub-minimum inhibitory concentration (sub-MIC) of CFE (12.5 mg/l) was used for further analysis.
To test whether the inhibition was due to the production of organic acids, the CFE was neutralized and no inhibition zones were observed. In addition, CFE was treated with heat and different enzymes and no significant differences (p > 0.05) were detected between the CFE and its treated samples from the point of inhibition zone diameter.
Lactic Acid and EPS Production
The pH in the MRS growth medium of the strain F-10 was reduced significantly (p < 0.05) to approximately 3.8 upon incubation for 24 h at 37 °C. The d-/l-lactic acid (d-/l-lactate) test kit is used for the rapid and specific concurrent measurement and analysis of l-lactic acid (l-lactate) and d-lactic acid (d-lactate) in CFE of the strain F-10. The amount of total lactic acid in the CFE, following the 24-h incubation at 37 °C in MRS medium, was detected as 15.1 ± 1.18 g/l.
L. plantarum F-10 was also evaluated for the production of EPS by a phenol-sulfuric acid method using glucose as standard. EPS content was calculated according to the regression equation based on the standard curve and then converted with a dilution ratio. With glucose as a carbon source, the total quantity of EPSb and EPSr was found as 750 ± 12 mg/l and 1.157 ± 72 mg/l, respectively.
Auto-aggregation and Co-aggregation
The results showed that the strain displayed a stronger auto-aggregation (51.48 ± 1.45%, Fig. 2a) after 5 h. From the point of each pathogen strain, clinical isolates demonstrated significantly higher auto-aggregation (P. aeruginosa 19.6 ± 1.21% and MRSA 17.2 ± 2.21%) compared with ATCC strains of P. aeruginosa (13.6 ± 1.05%) and MRSA (13.07 ± 1.02%), respectively. For the co-aggregation assay, results were defined as the percentage reduction after 5-h co-incubation in the absorbance of the mixed suspension compared with the individual strains. In the current experiment, the strain F-10 demonstrated greatest co-aggregation with all pathogens shown in Table 2. Co-aggregation with P. aeruginosa PAO1/ATCC 27853 was found greatest overall which also visualized in a light microscope (Fig. 2b, c) as well as SEM (Fig. 3a–f).
Anti-biofilm Forming Activity
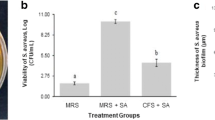
To determine the optimal conditions for biofilm production of the pathogens, experiments were conducted using modified TSB medium with different concentrations of glucose and NaCl. With the crystal violet assay, P. aeruginosa strains showed strong biofilm production in TSB medium supplemented with 0.5% glucose, while MRSA strains with 3% glucose and 3% NaCl (Fig. 4a), visualized by SEM (Fig. 5a, b). The effect of the various applications on the biofilm formation of skin pathogens was summarized in Table 3. All pathogens lost their ability to form biofilm and became no biofilm producer (0) when co-incubated with the sub-MIC value of L. plantarum F-10 CFE (Fig. 4b). EPS (10 mg/ml) derived from strain F-10 also exhibited an anti-biofilm activity between the range of 23–60%. Remarkably, EPSb is found significantly most effective than EPSr (p < 0.05). Upon treatment with EPSr, classification of all pathogens changed from strong to moderate biofilm producers, while strong to weak with EPSb. Among active ingredients derived from the F-10 strain, CFE was also used for eradication and pre-treatment assays. No valuable reduction was observed in eradication assays, although × 5 MIC value of CFE concentration has been used. From the point of pre-treatment assay, no significant differences between the reduction of biofilm formations of ATTC strains were observed in all time intervals (p > 0.05). However, > 50% reduction was observed for all clinical isolates following the 6-h pre-treatment. In all biofilm experiments, MRS was used as a control which had no significant inhibitory effect (p < 0.001) on biofilm production of all pathogens tested.
The scanning electron microscopy was used to illustrate the effect of pre-treatment approach on the topology of the biofilm developed by P. aeruginosa ATCC 24853. The micrographs (Fig. 6a–f) displayed a well-grown biofilm along with adhering bacterial cells in controls while dispersed bacterial cells in treated samples. It is also well observed that the treatment cause cells to shrink, and cell number and biofilm formation have also been affected time dependently. Less attachment of bacterial cells to the surface was observed even up to 12 h in the treated samples compared to control. To confirm the results on biofilm inhibition, we visualized its structural organization by confocal laser microscopy using stainless steel slides for reproducing abiotic surfaces used in healthcare units and industries’ environment. The dead P. aeruginosa cells were labeled with propidium iodide, whereas live cells stained with SYTO 9, which produced red and green fluorescence, respectively. A significant number of dead cells were detected in the biofilms following the treatments (Fig. 7a–f). Similarly to SEM, the micrographs clearly show not only a reduction of viable cells but also the biofilm formation by the treated samples compared to control. The reduced intensity due to the reduction in the live cells on treatment CFE was easily visible, which signified the shrinking of biofilm formation.
Confocal laser microscopy images illustrating the effect of the sub-MIC value of CFE on the cell viability of pathogens and their biofilm formations. MRSA ATCC 43300: untreated (a), co-incubation (b), pre-treatment for 3 h (c). P. aeruginosa ATCC 27853: untreated (d), co-incubation (e), pre-treatment for 3 h (f)
Anti-quorum Sensing Activity
Our results exhibited the potential of sub-MIC value (12.5 mg/l) of CFE to attenuate the quorum sensing ability of P. aeruginosa ATCC 27853 and its clinical isolate from the point of motility and their virulence factors (Table 4). The concentration of pyocyanin produced by the strain P. aeruginosa ATCC 27853 and the clinical isolate was calculated to be 1.26 ± 0.0012 and 0.93 ± 0.0008 μg/ml. Following the treatment, concentrations were reduced to 0.13 ± 0.0002 and 0.05 ± 0.0001 μg/ml, respectively. Similarly, the concentration of the elastase produced by the strain P. aeruginosa ATCC 27853 and the clinical isolate was calculated to be 0.43 ± 0.004 and 0.40 ± 0.007 μg/ml, respectively. Following the treatment, concentrations were reduced to 0.06 ± 0.005 and 00.06 ± 0.003, respectively.
Antioxidant Activity
Level of phenolic content of CFE was expressed in terms of gallic acid equivalent (GAE). The equation of the right-hand side of the proportioning of total phenolic content by the method of Folin-Ciocalteu gave Y = 5.455 × + 0.013 with R2 = 0.999, and the total content of phenols was calculated as 5.8 mg GAE/g of CFE. Total flavonoid concentration of CFE was also expressed in terms of quercetin equivalent (QE) and determined as 0.9 mg QE/g. In the DPPH analysis, sub-MIC value of CFE exhibited strong radical-scavenging activity with an inhibition rate of 88.57 ± 0.49% (Fig. 8). The results were expressed as IC50 which was calculated as 4.16 mg/ml.
Discussion
Wound healing process affected from infection as well as inflammation is ever a more dangerous case for the patients. Medicinal products including antibiotics are in use for prevention from the infection during this period. However, antibiotic resistance is an irreversible problem all over the world [35]. In addition, skin pathogens are an emerging therapeutic problem due to their biofilms which offer them considerable advantages in terms of self-protection from the effects of antibiotics [36]. Therefore, developments of antimicrobial and anti-biofilm, as well as anti-quorum sensing strategies against important skin pathogens, are of major concerns of wound healing and new therapies including innovative materials are urgently required for wound therapy.
The studies investigating the role of probiotics in skin diseases are very often when compared to the other studies dealing with the importance of probiotics [11]. Convincing evidence is demonstrated in a few studies that live probiotics or their spent culture fluid could impact significantly on enhancing the wound healing process by reducing the infection [37,38,39,40,41,42,43]. However, limited data suggest their possible effect in the wound management, and in general, the mechanisms underlying their positive effects have not been well understood [40]. Current researches are focused on understanding the concept of probiotics use to reduce skin infections [41]. In this study, we first investigated whether the potential probiotic strain L. plantarum F-10 might interfere with the pathogenic properties of P. aeruginosa and MRSA. Based on susceptibility tests, the CFE from L. plantarum F-10 exhibited high ability to inhibit the infection-causing capacity of P. aeruginosa and MRSA. The potential of Lactobacillus species to inhibit pathogens of clinical importance had been evaluated in many studies. Similarly to our results, L. fermentum CMUL054 and L. plantarum CMUL140 had shown antimicrobial potential against S. aureus [44]. A study conducted by Tejero-Sarinena et al. [45] showed that most of the selected strains of probiotics were able to produce active compounds against skin pathogens. The primary antimicrobial effect exerted by different Lactobacillus species of lactic acid bacteria may be explained via production of a range of antimicrobial agents such as organic acids which reduces the pH of the immediate environment, bacteriocins, hydrogen peroxide, and other surfactants [46]. According to our results, neutralization of the CFE resulted in the loss of the inhibitory effect, suggesting that the lowered pH of CFE, related with the production of organic acids, is responsible for the inhibition [47].
Pathogenic bacterial cells communicate with each other via signal molecules, and when they reach a sufficient majority, they regulate critical gene expression, such as the synthesis of virulence factors which is the basis for the successful infection process. Therefore, the prevention of communication by means of quorum sensing molecules has become one of the current goals of antimicrobial treatment approaches. Targeted use of natural components instead of antibiotics has been a promising approach in recent years. The presence of some substances (plant extracts, mushroom extracts) that block the quorum sensing system in P. aeruginosa has been determined in the literature [48]. However, the obtained results have not found the application under in vivo systems due to their toxic effects on the host and the requirements of their high concentrations. Using in vitro studies, we have demonstrated that CFE of L. plantarum F-10 inhibited the expression of soluble virulence factors of opportunistic dermal pathogens mainly involved in biofilm-based wound infections. The effect of probiotics on MRSA and P. aeruginosa was first carried out by Valdez and colleagues who evaluated the ability of the probiotic strain L. plantarum to inhibit the P. aeruginosa through blocking the production of quorum sensing molecules and elastase with the whole culture cells as well as culture filtrates [43]. Similar inhibitory effects were also obtained by Sadowska and coworkers with the CFE of L. acidophilus H-1 via competitive interactions between S. aureus strains and the probiotic strain [49]. Since quorum sensing signals are also necessary for the biofilm formation, our results showed that CFE might have reduced quorum sensing signals needed for biofilm formation. Accordingly to the recent studies evaluated the ability of commonly used probiotic strains (L. acidophilus DSM 20079, L. paracasei DSMZ 16671, L. rhamnosus GG, etc.) to hamper pathogen growth and biofilm formation were all suggested that the antimicrobial activity of Lactobacilli seems to be strain-specific and especially pH-dependent, similar to our results [50, 51]. In another previous report, the supernatant of L. bulgaricus FTDC8611 inhibited significantly S. aureus biofilm production via the effect attributed to organic acids [52]. In addition, Zmantar and colleagues stated that the decrease in pH caused a decrease in MRSA biofilm formation [53]. The observed information of reduced biofilm ability of postbiotics produced by L. fermentum is also determined Kanmani et al. [54] and Bulgasem et al. [55]. In contrast to our study, Walencka et al. [56] defined that L. acidophilus–derived surfactants reduced the MRSA biofilm development by the mechanism of influencing the cell surface hydrophobicity, without affecting the cell growth. In our study, the cell viability of MRSA and P. aeruginosa in their biofilms was also reduced by co-incubation with CFE, similarly to the results of Varma et al. [57]. However, eradication results were not found sufficient compared to the initial addition or pre-treatment of the CFE in the microtiter wells. Therefore, a possible conclusion of the biofilm assays is that CFE might modify the target surface in a way that there might be a reduction or inhibition of irreversible attachment of the biofilm-forming bacteria that prevents biofilm formation for the organisms studied in this work.
Although many probiotics have been described as generally recognized as safe (GRAS) by the American Food and Drug Administration (FDA), careful assessments must be taken within their use. It is a necessary requirement to select safe strain-specific probiotics with their appropriate properties for host consumptions. To confirm the safety of the strain, in vitro and in vivo studies are required. In our study, we only evaluated its safety aspects from the point of hemolytic activity and antibiotic susceptibility, under in vitro conditions. L. plantarum F-10 was found non-hemolytic and sensitive to all antibiotics considered as important by the European Food Safety Authority (EFSA), except gentamicin and kanamycin. These antibiotics are regarded in intrinsic antibiotic resistance property within lactic acid bacteria which helps its applications for human health [58, 59]. In addition to the safety issues, other valuable and important features of the strain were also evaluated such as antioxidant capacity. Antioxidant activities of lactic acid bacteria are associated with many diseases in the field of health. Synthetic antioxidants exhibit disadvantages because of their low oxidation capacity, reliability, and toxic effects. Therefore, the extracellular extracts of lactic acid bacteria have recently gained attention as natural sources of antioxidants. Our results from the point of antioxidant capacity of L. plantarum F-10 strain were found similar to the literature data [60,61,62]. Nevertheless, among antioxidant properties, DPPH inhibition activity was found very high than other studies as evaluated by Uugantsetseg and Batjargal [63], which determined the antioxidant activity of the CFE between the range of 26.1 and 38.4%. Detection of the 88.57% DPPH inhibition activity and high total phenolic and flavonoid content of the CFE proved the antioxidative potential of L. plantarum F-10 strain and offer a practical advantage in reduction of oxidative stress in wound healing stages [64, 65]. Considering the importance of different stages in wound healing process, it is thought that L. plantarum F-10 strain can provide additional contributions to the healing management from the point of not only protection from the infections but also with its antioxidant effect.
Conclusion
Our main concept is to combine the probiotics or their postbiotic mediators originated from human microbiota and nanofiber materials for the development of a novel bio-therapeutic wound dressing product to be used in skin and surgical practice. For this purpose, our current study aimed to investigate the role of selective probiotics on some bacterial human skin pathogens as an adjunct therapy against infection in wound management. In conclusion, an ideal probiotic which is able to compete and interfere with biofilm-growing pathogens has been identified, especially in the context of specific wound infections. Despite being regarded as GRAS, there is no current evidence for the topical use of probiotic bacteria as viable cells due to the possibility of accessing the blood circulation. Therefore, we decided to use CFE of L. plantarum F-10 with its antimicrobial, anti-biofilm, and anti-quorum sensing and antioxidant activities, for the further development of wound management strategies. But clearly, more work is needed in this area to fully demonstrate the proof of principle.
References
Greatrex-White S, Moxey H (2015) Wound assessment tools and nurses’ needs: an evaluation study. Int Wound J 12:293–301
Moore Z (2012) The war on wounds. Public Sect Rev Eur 24:1–2
Posnett J, Gottrup F, Lundgren H et al (2009) The resource impact of wounds on health-care providers in Europe. J Wound Care 18(4):154–161
Sen CK, Gordillo GM, Roy S et al (2009) Human skin wounds: a major and snowballing threat to public health and the economy. Wound Repair Regen 17(6):763–771
Cogen AL, Nizet V, Gallo RL (2008) Skin microbiota: a source of disease or defence? Br J Dermatol 158:442–455
Moore Z, Butcher G, Corbett LQ et al (2014) AAWC, AWMA, EWMA position paper: managing wounds as a team. J Wound Care 23(5):1–38
Serra R, Grande R, Butrico L et al (2015) Chronic wound infections: the role of Pseudomonas aeruginosa and Staphylococcus aureus. Expert Rev Anti-Infect Ther 13(5):605–613
Plata K, Rosato AE, Wegrzyn G (2009) Staphylococcus aureus as an infectious agent: overview of biochemistry and molecular genetics of its pathogenicity. Acta Biochim Pol 56:597–612
Okhiria OA, Henriques AFM, Burton NF et al (2009) Honey modulates biofilms of Pseudomonas aeruginosa in a time and dose dependent manner. J Api Prod ApiMed Sci 1(1):6–10
Howard JC, Reid G, Gan BS (2004) Probiotics in surgical wound infections: current status. Clin Invest Med 27(5):274–281
Markowiak P, Slizewska K (2017) Effects of probiotics, prebiotics, and synbiotics on human health. Nutrients. https://doi.org/10.3390/nu9091021
Cinque B et al (2011) Use of probiotics for dermal applications. In: Liong MT (ed) Probiotics, Microbiology monographs. Springer-Verlag, Berlin, pp 221–241
Maragkoudakis PA, Zoumpopoulou G, Miaris C, Kalantzopoulos G, Pot B, Tsakalidou E (2006) Probiotic potential of Lactobacillus strains isolated from dairy products. Int Dairy J 16(3):189–199
Wilkins TD, Holdeman LV, Abramson IJ, Moore WEC (1972) Standardized single-disc method for antibiotic susceptibility testing of anaerobic bacteria. Antimicrob Agents Chemother 1:451–459
Clinical Laboratory Standards Institute (2012) Performance standards for antimicrobial susceptibility testing; 22nd informational supplement. Document M100-S22. Clinical Laboratory Standards Institute Wayne, PA
Anonymous (2008) European food safety authority. Update of the criteria used in the assessment of bacterial resistance to antibiotics of human or veterinary importance. EFSA J 732:715
Savadogo A, Ouattara CAT, Bassole HNI, Traore AS (2004) Antimicrobial activities of lactic acid bacteria strains isolated from Burkina faso fermented milk. Pak J Nutr 3:174–179
Bhunia AK, Johnson MC, Ray B (1988) Purification, characterization and antimicrobial spectrum of a bacteriocin produced by Pediococcus acidilactici. J Appl Bacteriol 65(4):261–268
Tallon R, Bressollier P, Urdaci MC (2003) Isolation and characterization of two exopolysaccharides produced by Lactobacillus plantarum EP56. Res Microbiol 154:705–712
Dubois M, Gilles KA, Hamilton JK, Rebers PA, Smith F (1956) Colorimetric method for determination of sugars and related substances. Anal Chem 28(3):350–356
Del Re B, Sgorbati B, Miglioli M, Palenzona D (2000) Adhesion, autoaggregation and hydrophobicity of 13 strains of Bifidobacterium longum. Lett Appl Microbiol 31:438–442
Kos B, Suskovic J, Vukovic S, Simpraga M, Frece J, Matosic S (2003) Adhesion and aggregation ability of probiotic strain Lactobacillus acidophilus M92. J Appl Microbiol 94:981–987
Kiran F, Mokrani M, Osmanagaoglu O (2015) Effect of encapsulation on viability of Pediococcus pentosaceus OZF during its passage through the gastrointestinal tract model. Curr Microbiol 71(1):95–105
Stepanovic S, Vukovic D, Dakic I, Savic B, Svabic-Vlahovic M (2000) A modified microtiter-plate test for quantification of staphylococcal biofilm formation. J Microbiol Methods 40(2):175–179
Vestby LK, Moretro T, Langsrud S, Heir E, Nesse LL (2009) Biofilm forming abilities of Salmonella are correlated with persistence in fish meal and feed factories. BMC Vet Res 5(20):1–6
Giaouris E, Chorianopoulos N, Nychas GJE (2005) Effect of temperature, pH, and water activity on biofilm formation by Salmonella enterica Enteritidis PT4 on stainless steel surfaces as indicated by the bead vortexing method and conductance measurements. J Food Prot 68(10):2149–2154
Rashid MH, Kornberg A (2000) Inorganic polyphosphate is needed for swimming, swarming, and twitching motilities of Pseudomonas aeruginosa. Proc Natl Acad Sci U S A 97:4885–4890
Ramos AN, Sesto Cabral M, Noseda D, Bosch A, Yantorno OM, Valdez JC (2012) Antipathogenic properties of Lactobacillus plantarum on Pseudomonas aeruginosa: the potential use of its supernatants in the treatment of infected chronic wounds. Wound Repair Regen 20:552–562
Siegmund I, Wagner F (1991) New method for detecting rhamnolipids excreted by Pseudomonas species during growth on mineral agar. Biotechnol Tech 5:265–268
Dong YH, Zhang LH (2005) Quorum sensing and quorum-quenching enzymes. J Microbiol 43:101–109
Yin H, Deng Y, Wang H, Liu W, Zhuang X, Chu W (2015) Tea polyphenols as an antivirulence compound disrupt quorum-sensing regulated pathogenicity of Pseudomonas aeruginosa. Nat Sci Rep 5:16158–16170
Singleton VL, Rossi JA (1965) Colorimetry of total phenolics with phosphomolybdic-phosphotungstic acid reagent. J Enol Vitic 16(3):144–158
Zhishen J, Mengcheng T, Jianming W (1999) The determination of flavonoid contents in mulberry and their scavenging effects on superoxide radicals. Food Chem 64(4):555–559
Blois MS (1958) Antioxidant determinations by the use of a stable free radical. Nature 181:1199–1200
World Health Organization (2015) Global action plan on antimicrobial resistance. WHO:1–28
Freedman M, Stassen LF (2013) Commonly used topical oral wound dressing materials in dental and surgical practice–a literature review. J Ir Dent Assoc 59(4):190–195
Gan BS, Kim J, Reid G, Cadieux P, Howard JC (2002) Lactobacillus fermentum RC-14 inhibits Staphylococcus aureus infection of surgical implants in rats. J Infect Dis 185:1369–1372
Hasslöf P, Hedberg M, Twetman S, Stecksen-Blicks C (2010) Growth inhibition of oral mutans streptococci and candida by commercial probiotic lactobacilli - an in vitro study. BMC Oral Health 10:355–362
Karska-Wysocki B, Bazo M, Smoragiewicz W (2010) Antibacterial activity of Lactobacillus acidophilus and Lactobacillus casei against methicillin-resistant Staphylococcus aureus (MRSA). Microbiol Res 165:674–686
Peral MC, Huaman Martinez MA, Valdez JC (2009) Bacteriotherapy with Lactobacillus plantarum in burns. Int Wound J 6:73–81
Prince T, Mcbain AJ, O’Neill CA (2012) Lactobacillus reuteri protects epidermal keratinocytes from Staphylococcus aureus-induced cell death by competitive exclusion. Appl Environ Microbiol 78:5119–5126
Sullivan M, Schnittger SF, Mammone T, Goyarts EC (2009) Skin treatment method with Lactobacillus extract. US Patent 2005/0196480 A1. 11/070:810
Valdez JC, Peral MC, Rachid M, Santana M, Perdigon G (2005) Interference of Lactobacillus plantarum with Pseudomonas aeruginosa in vitro and in infected burns: the potential use of probiotics in wound treatment. Clin Microbiol Infect 11:472–479
Al Kassaa I, Hamze M, Hober D, Chihib NE, Drider D (2014) Identification of vaginal lactobacilli with potential probiotic properties isolated from women in north Lebanon. Microb Ecol 67:722–734
Tejero-Sarinena S, Barlow J, Costabile A, Gibson GR, Rowland I (2012) In vitro evaluation of the antimicrobial activity of a range of probiotics against pathogens: evidence for the effects of organic acids. Anaerobe 18:530–538
Melo TA, dos Santos TF, de Almeida ME et al (2016) Inhibition of Staphylococcus aureus biofilm by Lactobacillus isolated from fine cocoa. BMC Microbiol 16:250–259
Simark-Mattsson C, Jonsson R, Emilson CG, Roos K (2009) Final pH affects the interference capacity of naturally occurring oral Lactobacillus strains against mutans streptococci. Arch Oral Biol 54:602–607
Rasmussen TB, Givskov M (2006) Quorum-sensing inhibitors as anti-pathogenic drugs. Int J Med Microbiol 296:149–161
Sadowska B, Walencka E, Wieckowska-Szakiel M et al (2010) Bacteria competing with the adhesion and biofilm formation by Staphylococcus aureus. Folia Microbiol (Praha) 55(5):497–501
Söderling EM, Marttinen AM, Haukioja AL (2011) Probiotic lactobacilli interfere with Streptococcus mutans biofilm formation in vitro. Curr Microbiol 62(2):618–622
Keller MK, Hasslöf P, Stecksen-Blicks C (2011) Co-aggregation and growth inhibition of probiotic lactobacilli and clinical isolates of mutans streptococci: an in vitro study. Acta Odontol Scand 69(5):263–268
Hor YY, Liong MT (2014) Use of extracellular extracts of lactic acid bacteria and bifidobacteria for the inhibition of dermatological pathogen Staphylococcus aureus. Dermatol Sin 32:141–147
Zmantar T, Kouidhi B, Miladi H, Mahdouani K, Bakhrouf A (2010) A microtiter plate assay for Staphylococcus aureus biofilm quantification at various pH levels and hydrogen peroxide supplementation. New Microbiol 33:137–145
Kanmani P, Kumar SR, Yuvaraj N, Paari KA et al (2011) Production and purification of a novel exopolysaccharide from lactic acid bacterium Streptococcus phocae PI80 and its functional characteristics activity in vitro. Bioresour Technol 102(7):4827–4833
Bulgasem Y, Hassan Z, Abdalsadiq NKA, Yusoff et al (2015) Antiadhesion activity of lactic acid bacteria supernatant against human pathogenic Candida species biofilm. Health Sci J 9:1–9
Walencka E, Rozalska S, Sadowska B et al (2008) The influence of Lactobacillus acidophilus-derived surfactants on staphylococcal adhesion and biofilm formation. Folia Microbiol (Praha) 53(1):61–66
Varma P, Nisha N, Dinesh KR et al (2011) Anti-infective properties of Lactobacillus fermentum against Staphylococcus aureus and Pseudomonas aeruginosa. J Mol Microbiol Biotechnol 20(3):137–143
Ashraf R, Shah NP (2011) Antibiotic resistance of probiotic organisms and safety of probiotic dairy products. Int Food Res J 18(3):837–853
Mathur S, Singh R (2005) Antibiotic resistance in food lactic acid bacteria-a review. Int J Food Microbiol 105:281–295
Liu C, Pan T (2010) in vitro effects of lactic acid bacteria on cancer cell viability and antioxidant activity. J Food Drug Anal 18:77–86
Zhang S, Liu L, Su Y, Li H, Sun Q, Liang X (2011) Antioxidative activity of lactic acid bacteria in yogurt. Afr J Microbiol Res 5:5194–5201
Xing J, Wang G, Zhang Q et al (2015) Determining antioxidant activities of lactobacilli cell-free supernatants by cellular antioxidant assay: a comparison with traditional methods. PLOS ONE. https://doi.org/10.1371/journal.pone.0119058
Uugantsetseg E, Batjargal B (2014) Antioxidant activity of probiotic lactic acid bacteria isolated from Mongolian airag. Mongolian J Chem 15:73–78
Pieniz S, Andreazza R, Okeke BC, Camargo FAO, Brandelli A (2015) Antimicrobial and antioxidant activities of Enterococcus species isolated from meat and dairy products. Braz J Biol. https://doi.org/10.1590/1519-6984.02814
Wang Y, Wu Y, Wang Y et al (2017) Antioxidant properties of probiotic bacteria. Nutrients 9:521–236
Acknowledgments
The authors wish to sincerely thank Dr. Basar KARACA (Ankara University) for his excellent technical assistance on biofilm analysis.
Funding
This work was supported by grants of the Scientific Research Project Coordination Unit of Ankara University, Turkey (Project No: 17B0430001).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Onbas, T., Osmanagaoglu, O. & Kiran, F. Potential Properties of Lactobacillus plantarum F-10 as a Bio-control Strategy for Wound Infections. Probiotics & Antimicro. Prot. 11, 1110–1123 (2019). https://doi.org/10.1007/s12602-018-9486-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12602-018-9486-8