Abstract
Background
In end-stage renal disease patients with preserved LV ejection fraction undergoing chronic hemodialysis, we investigated the relationship of left atrial deformational parameters evaluated by two-dimensional speckle tracking imaging (2D-STI) with conventional echocardiographic diastolic dysfunction parameters and brain natriuretic peptide level.
Methods
The study group enrolled 30 patients treated with chronic hemodialysis three times weekly. Two-dimensional transthoracic echocardiography and Doppler studies were performed 44.93 (13.46) immediately before and after HD. All patients had preserved left ventricular ejection fraction.
Results
The mean age of patients was 44.93 ± 13.46 years. The mean brain natriuretic peptide (BNP) value after HD was 221.56 ± 197.79 pg/ml. BNP values were significantly higher before HD (p = 0.004), the anteroposterior diameter, area, and the volumes of the LA decreased significantly after HD. On the other hand, the left atrial ejection fraction (LAEF) and the peak LA strain during LV systole (LAGS) were found to be higher. Before HD, there were significant inverse correlations between LAGS and BNP levels (r = −0.482, p = 0.007), E/E′ (r = −0.33, p = 0.049), LAVmax (r = −0.366, p = 0.047), and LAVmin (r = –0.579, p = 0.001). LAGS had a significant correlation with E′ velocity (r = 0.557, p = 0.001) (Table 5) and LAEF (r = 0.58, p = 0.001). After HD, there were also significant correlations between LAGS and echocardiographic parameters of systolic and diastolic LV function.
Conclusions
We observed that left atrium global peak systolic strain values decreased consistently with deteriorating systolic and diastolic function. Our results suggest that LAGS measurements may be helpful as a complimentary method to evaluate diastolic function.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Chronic renal disease results in structural and functional abnormalities in the heart, known as uremic cardiomyopathy. These changes are associated with greater risk of cardiovascular (CV) morbidity and mortality [1]. In fact, end-stage renal disease (ESRD) is associated with left ventricular (LV) hypertrophy, LV systolic and diastolic dysfunction, and an increased left atrial volume (LAV). The size of the LA reflects the severity and duration of increased LA pressure consequent to increased LV end-diastolic pressure. Therefore, the LAV is a good echocardiographic marker of the LV diastolic dysfunction [2]. Echocardiographic studies conducted on different patient groups have demonstrated that the phasic functions of LA decrease in parallel to the increase in the LAV. Especially in heart failure patients with preserved LV ejection fraction (LVEF), the reduction in the LA function may lead to a decrease in the functional capacity and to CV complications [3]. Two-dimensional speckle tracking imaging (2D-STI) is a new echocardiographic tool that may directly assess myocardial LA functions [4]. This analysis can allow a more direct assessment of LA endocardial contractility and passive deformation. Previous studies have shown that decreased LA peak strain during LV systole (LAGS) was related to systolic and diastolic dysfunction and then to CV events and mortality [5, 6].
Moreover, because of the high prevalence of heart failure in ESRD patients, there is a great need for a good clinical biomarker enabling early identification of hemodialysis (HD) patients at risk of cardiovascular events and mortality, as well as earlier aggressive intervention.
Brain natriuretic peptide (BNP) is a cardiac hormone produced and secreted mainly by the ventricles, which is elevated in patients with cardiac hypertrophy or heart failure [7].
BNP levels are also elevated in patients with chronic kidney disease, especially those undergoing dialysis [8]. This is likely related to left ventricular dysfunction as well as to reduced clearance and increased plasma volume. It is widely recognized that cardiac function is a major confounder influencing levels of this peptide in dialysis patients. Thus, even in dialysis patients with ESRD, BNP is used for diagnosis and evaluation of the severity of heart failure and it is predictive of patient prognosis [9].
In ESRD patients with preserved LVEF undergoing chronic hemodialysis, we investigated the relationship of left atrial deformational parameters evaluated by 2D-STI with conventional echocardiographic diastolic dysfunction parameters and brain natriuretic peptide level.
Methods
Study population
The study group enrolled 30 patients treated with chronic hemodialysis three times weekly. All these patients were referred to the Echocardiography Laboratory between May 1, 2014 and June 28, 2014 for echocardiographic evaluation. We excluded patients with known coronary artery disease, cardiac arrhythmias, cardiomyopathy, or moderate-to-severe valvular disease diagnosed by echocardiography. All patients had preserved left ventricular ejection fraction (LVEF) of 50 % or greater. Blood pressure, heart rate, and anthropometric measurements of all patients were recorded before the echocardiography. Body surface area (BSA) was calculated from the anthropometric measurements by the Mosteller formula [10]. Blood analysis for serum electrolytes and brain natriuretic peptide (BNP) was performed for all patients.
Echocardiography
Two-dimensional transthoracic echocardiography (TTE) and Doppler studies were performed immediately before and after HD using a GE Vivid E9 ultrasound machine with a 3.5-MHz transducer. Heart rate was continually monitored during the transthoracic evaluation. All data were transferred to a workstation for offline analyses (EchoPac PC).
Conventional echocardiographic evaluation
All patients underwent an echocardiographic evaluation in the left lateral position using a GE Vivid 9 system. Heart rate was continually monitored during the transthoracic evaluation. Parasternal long-axis view was used for the M-mode measurements of the left atrial diameter, interventricular septal, LV posterior wall thickness (IVST and LVPWT), LV end-diastolic and end-systolic dimensions (LVEDd and LVESd). LVEF was calculated from LV volumes by the modified biplane Simpson rule using apical four-chamber and two-chamber images and expressed as a percentage. The left atrial area and volume were also determined. LA maximum volume (LAVmax) was measured when the mitral valve was completely opened and LA minimum volume (LAVmin) was measured when the mitral valve was completely closed. The LA volumes were indexed to the BSA. The LAEF was calculated as (LAVmax–LAVmin)/LAVmax and expressed as percentage. Peak transmitral flow velocity in early diastole (E) and peak transmitral flow velocity in late diastole (A) were attained by pulsed-wave Doppler echocardiography in the apical four-chamber image. The mitral A wave duration (dAm), the pulmonary A wave duration (dAp), E/A ratio, and the E deceleration time (DT) were evaluated. Doppler tissue imaging (TDI) was performed in the four-chamber view. The myocardial systolic (S′), early diastolic (E′), and late diastolic (A′) wave velocities were attained at the lateral mitral annulus. The E/E′ for lateral annulus was calculated. The color M-mode Doppler flow propagation velocity (Vp) was obtained by combined color-flow Doppler and MM-mode interrogation of the mitral inflow during diastole. Diastolic dysfunction was defined by left ventricle elevated filling pressures.
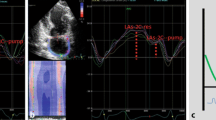
Two-dimensional speckle tracking analysis of the left atrium
Two-dimensional echocardiography views for the LA were attained from the apical four- and two-chamber images. All views were obtained with patients holding their breath at end-expiration and with an electrocardiographic reading taken at the same time. The frame rate for views was set at 60–80 frames/s. The views were stored in a cineloop format and three consecutive heart cycles were recorded for offline analysis using EchoPac software. The atrial endocardium was first determined manually. The epicardial surface is calculated automatically and the software system automatically divides the atrial wall to six segments. If speckle tracking is not adequate, the region of interest is manually adjusted to include only the atrial wall. Segments in which adequate tracking quality could not be obtained despite manual adjustments were excluded from the analysis. If the tracking segments were sufficient for analysis, the software system was allowed to read the data. The typical LA strain graph was obtained for each patient. Mean peak LA strain valuations during LV systole (LAGS) for six segments were evaluated.
BNP measurement
Blood samples were obtained from all patients before and after HD. The blood samples were immediately centrifuged and plasma was stored at −80 °C until the time of evaluation. The quantitative definition of BNP in plasma was performed using the immune fluorescence method.
Statistical analysis
Statistical analysis was performed using Statistical Package for Social Sciences version 20.0 software (SPSS, Chicago, IL, USA). Continuous variables with normal distribution were presented as the mean (standard deviation, SD). Qualitative variables were given as percentage. Correlations between continuous variables were assessed using Pearson’s or Spearman’s correlation analysis after the normality of the distribution of the data was verified. A p value under 0.05 was considered as statistically significant.
Results
The mean duration of chronic hemodialysis in ESRD patients was 7.14 ± 5.91 years. The demographic and clinical data of the study population are summarized in Table 1. After HD session, the systolic and diastolic blood pressures, body weight, and BSA decreased significantly (p = 0.000). The mean BNP value after HD was 221.56 ± 197.79 pg/ml. BNP values were significantly higher before HD (p = 0.004). The results of laboratory analyses before and after HD are shown in Table 2.
Table 3 summarizes the results of echocardiographic evaluation before and after HD. After HD, the LV end-diastolic and end-systolic dimensions and volumes decreased significantly. However, no significant difference was observed in the LVEF. When the Doppler and TDI LV echocardiographic data before and after HD were compared, mitral early diastolic flow velocity (E), mitral E/A ratio, E/E′, and LV filling pressure were observed to be significantly lower after HD.
When the atrial parameters of the study population were assessed, the anteroposterior diameter, area, and the volumes of the LA decreased significantly after HD. On the other hand, the LAEF and the peak LA strain during LV systole (LAGS) were found to be higher. An assessment of the LA structure and function is presented in Table 4.
Before HD, there were significant inverse correlations between LAGS and BNP levels (Table 5, Fig. 1) (r = −0.482, p = 0.007), E/E′ (r = −0.33, p = 0.049), LAVmax (r = −0.366, p = 0.047) and LAVmin (r = −0.579, p = 0.001). LAGS had significant correlation with E′ velocity (r = 0.557, p = 0.001) (Table 5; Fig. 2a) and LAEF (r = 0.58, p = 0.001) (Table 5; Fig. 2b). LAGS value of 29.39 % predicted diastolic dysfunction with a sensibility of 83 % and a specificity of 76 %. After HD, there were also significant correlations between LAGS and echocardiographic parameters of systolic and diastolic LV function, as shown in Table 5. LAGS value of 32.59 % predicted diastolic dysfunction with a sensibility of 93 % and a specificity of 82 %.
Discussion
In the present study, the comparison before and after hemodialysis in ESRD patients revealed that as the LAV decreased, the LA function and deformation parameters estimated by the global systolic strain increased after hemodialysis. We also demonstrated that LAGS was closely related to BNP levels and LV function.
LA size and function are important determinants of cardiovascular morbidity and mortality in ESRD patients [11]. In general, the LA performs multiple functions, acting as a reservoir during LV systole, a conduit for blood passing from the pulmonary veins to the LV during early diastole, an active contractile chamber that augments LV filling in late diastole, and a suction pump that refills itself in early systole [12]. LA functions play a central role in maintaining the optimal cardiac output despite impaired LV relaxation and reduced LV compliance in ESRD patients with preserved LVEF. LV diastolic dysfunction, LV hypertrophy, and volume overload may lead to elevated LV filling pressure and LA afterload in patients with ESRD [13]. Consequently, these alterations produce a compensatory mechanism in the LA characterized by LA dilatation and the stretching of the atrial myocardium. This remodeling leads to a slow and incomplete relaxation with LA systolic and diastolic dysfunction [14,15].
Two-dimensional speckle tracking imaging (STI) is a new echocardiographic tool that tracks the speckle pattern frame by frame in standard B-mode images to calculate left ventricular strain [16]. This analysis may allow a more direct assessment of LA endocardial contractility, and regional and global deformation and has been recently proposed [17–19]. LA myocardial deformation curves attained with two-dimensional STI are similar to LA volume graphs. LA volume and function graphs contain three phases, known as reservoir, conduit, and booster pump [4]. LAGS is closely related to the LA reservoir function (LARF), and the LA strain during atrial systole is associated with booster pump function [20]. The LARF is evaluated in two sequential phases: early and late. Although the early LARF depends on LA relaxation, the late LARF depends on LV contraction through the descent of the base during systole. Thus, both LA relaxation and LV systolic function might influence the LARF and, subsequently, LAGS [21, 22]. When the LA is well stretched longitudinally, and consequently a high LAGS is present, the LV relaxes rapidly, generating high E wave and E′, as blood rushes into the LV, generating a high LA ejection fraction. Therefore, LAGS correlated with parameters of LV diastolic function, the maximum LA volume, and LA volumetric indexes of conduit and reservoir function [4]. Recent works have shown that the Doppler indices of diastolic filling are very load-dependent, fluctuating widely with changes in the intravascular status during dialysis. LA size, which has previously been shown to correlate with LV dysfunction, may be a more stable measurement option that is preload-independent. A recent study showed that fluctuations in the LAV are less pronounced than the changes in the intravascular status during dialysis. However, the evaluation of LAV by 2D echocardiography is limited by the use of geometric models that determine the volume of a non-symmetric chamber, and by errors that occur due to foreshortening [23]. This finding may support previous evidence showing that a large proportion of the variability in the standard indices of LAV and function is likely to be explained by the changes in the LA size, whereas abnormalities in the LA strain are relatively independent from LA dilatation and volume overload [24].
In our study, we found significant correlations between LV systolic parameters and LAGS. Similarly, Wakami et al. [6] found a significant relation between peak LA wall strain during LV systole and LV hemodynamic measurements. They also demonstrated that peak LA wall strain during LV systole was determined not only by LV systolic function but also by LV end-diastolic pressure (LVEDP) [6]. Other previous studies investigated the impact of LV filling pressure (LVEDP)—which is the hemodynamic marker of LV dysfunction—and pulmonary capillary wedge pressure (PCWP) on LAGS during LV systole, reporting that enhanced LVEDP is related to a decrease of LAGS [5].
Cameli et al. [5] demonstrated that in a group of patients with advanced systolic heart failure, E/E′ ratio was poorly correlated with invasively obtained LV filling pressures. Nevertheless, LAGS analysis by speckle tracking imaging correlates well with pulmonary capillary wedge pressure, providing a better estimation of LV filling pressure in this particular clinical setting. E/E′ ratio, LA volumes, and BNP were also significantly increased in ESRD patients, reflecting increased diastolic filling pressures and diastolic dysfunction.
Therefore, in our study, we evaluated LAGS to assess diastolic dysfunction in ESRD patients before and after HD. Altekin et al. [23] demonstrated that in ESRD patients with preserved systolic function who are undergoing hemodialysis, the LA myocardial function assessed through the 2D-STI method was an independent correlative of increased ePCWP, which is an echocardiographically calculated hemodynamic marker of LV dysfunction. Our results agreed; in our ESRD patients undergoing HD, average LAGS was substantially lower before HD and was inversely correlated to echocardiographic parameters of diastolic function such as LA volumes and E/E′ ratio.
In the present study, we also evaluated BNP levels before and after HD in ESRD patients. Plasma BNP levels are elevated in patients with heart failure [24, 25], and correlate strongly with LV filling pressure [26, 27]. This biomarker increases with increasing severity of heart failure evaluated based on New York Heart Association Class, functional capacity [28], or systolic and diastolic dysfunction [29, 30]. Even in patients with chronic kidney disease and ESRD, left ventricular end-diastolic wall stress remains a strong determinant of circulating BNP levels [31]. Furthermore, in ESRD patients receiving long-term dialysis, BNP and NT-proBNP levels are strongly associated with the severity of LV hypertrophy and systolic dysfunction, and their elevation also reflects the presence of myocardial ischemia and is indicative of the severity of coronary artery disease [32]. Finally, BNP and NTproBNP are highly predictive of subsequent cardiac events and mortality in hemodialysis patients [33]. In our study, we observed that BNP levels decreased significantly after HD and that LAGS was inversely correlated with BNP levels, as well as echocardiographic LV diastolic parameters.
Study limitations
Our study had several limitations. Although the efficiency of the 2D-STI method was validated on our study population, the limited number of patients may present a limitation for the validation of the efficiency of the method. Another limitation of the study was the lack of invasive hemodynamic data. Cardiac catheterization provides more accurate information about the LV filling pressures than echocardiographic measurements. Nonetheless, several studies have demonstrated the high sensitivity, specificity, and accuracy of the mitral E/E′ ratio in the assessment of LV filling pressures. The evaluation of the LA through 2D-STI is more difficult and time-consuming than the assessment of the segmental LV function. We used current software for the LV analysis to study the LA pattern strain. Since our study was an observational study and did not include the clinical follow-up of the patients, the relationship between the results and the cardiovascular prognosis of the patients was not evaluated.
Conclusions
The present study demonstrated that in ESRD patients with preserved systolic left ventricular function who are undergoing chronic hemodialysis, 2D-STI is a non-invasive, reproducible, and relatively simple technique for evaluating LA function. We observed that left atrium global peak systolic strain values decreased consistently with deteriorating systolic and diastolic LV function. Our results suggest that LAGS measurements may be helpful as a complementary method to evaluate diastolic function.
References
McIntyre CW, Odudu A, Eldehni MT, et al. Cardiac assessment in chronic kidney disease. Curr Opin Nephrol Hypertens. 2009;18(6):501–6.
Omae K, Ogawa T, Yoshikawa M, et al. Left atrial dilatation and ST-T changes predict cardiovascular outcome in chronic hemodialysis patients. Heart Vessels. 2012;27(6):610–7.
Morris DA, Gailani M, Vaz Pérez A, et al. Left atrial systolic and diastolic dysfunction in heart failure with normal left ventricular ejection fraction. J Am Soc Echocardiogr Off Publ Am Soc Echocardiogr. 2011;24(6):651–62.
Saraiva RM, Demirkol S, Buakhamsri A, et al. Left atrial strain measured by two-dimensional speckle tracking represents a new tool to evaluate left atrial function. J Am Soc Echocardiogr Off Publ Am Soc Echocardiogr. 2010;23(2):172–80.
Cameli M, Lisi M, Mondillo S, et al. Left atrial longitudinal strain by speckle tracking echocardiography correlates well with left ventricular filling pressures in patients with heart failure. Cardiovasc Ultrasound. 2010;8:14.
Wakami K, Ohte N, Asada K, et al. Correlation between left ventricular end-diastolic pressure and peak left atrial wall strain during left ventricular systole. J Am Soc Echocardiogr Off Publ Am Soc Echocardiogr. 2009;22(7):847–51.
Nishikimi T, Yoshihara F, Morimoto A, et al. Relationship between left ventricular geometry and natriuretic peptide levels in essential hypertension. Hypertension. 1996;28(1):22–30.
Nishikimi T, Futoo Y, Tamano K, et al. Plasma brain natriuretic peptide levels in chronic hemodialysis patients: influence of coronary artery disease. Am J Kidney Dis Off J Natl Kidney Found. 2001;37(6):1201–8.
Daniels LB, Maisel AS, et al. Natriuretic peptides. J Am CollCardiol. 2007;50(25):2357–68.
Mosteller RD, et al. Simplified calculation of body-surface area. N Engl J Med. 1987;317(17):1098.
Shizuku J, Yamashita T, Ohba T, et al. Left atrial volume is an independent predictor of all-cause mortality in chronic hemodialysis patients. Intern Med Tokyo Jpn. 2012;51(12):1479–85.
Leung DY, Boyd A, Ng AA, Chi C, et al. Echocardiographic evaluation of left atrial size and function: current understanding, pathophysiologic correlates, and prognostic implications. Am Heart J. 2008;156(6):1056–64.
Kim SJ, Han SH, Park JT, et al. Left atrial volume is an independent predictor of mortality in CAPD patients. Nephrol Dial Transplant Off PublEur Dial TransplAssoc—EurRen Assoc. 2011;26(11):3732–9.
Losi MA, Memoli B, Contaldi C, et al. Myocardial fibrosis and diastolic dysfunction in patients on chronic haemodialysis. Nephrol Dial Transplant Off PublEur Dial TransplAssoc—EurRen Assoc. 2010;25(6):1950–4.
Boyd AC, Richards DAB, Marwick T, et al. Atrial strain rate is a sensitive measure of alterations in atrial phasic function in healthy ageing. Heart. 2011;97(18):1513–9.
Cho G-Y, Chan J, Leano R, et al. Comparison of two-dimensional speckle and tissue velocity based strain and validation with harmonic phase magnetic resonance imaging. Am J Cardiol. 2006;97(11):1661–6.
Vianna-Pinton R, Moreno CA, Baxter CM, et al. Two-dimensional speckle-tracking echocardiography of the left atrium: feasibility and regional contraction and relaxation differences in normal subjects. J Am Soc Echocardiogr Off Publ Am Soc Echocardiogr. 2009;22(3):299–305.
Ogawa K, Hozumi T, Sugioka K, et al. Automated assessment of left atrial function from time-left atrial volume curves using a novel speckle tracking imaging method. J Am Soc Echocardiogr Off Publ Am Soc Echocardiogr. 2009;22(1):63–9.
Değirmenci H, Bakırcı EM, Demirtaş L, et al. Relationship of left atrial global peak systolic strain with left ventricular diastolic dysfunction and brain natriuretic peptide level in patients presenting with non-ST elevation myocardial infarction. Med SciMonitInt Med J ExpClin Res. 2014;20:2013–9.
Lang RM, Bierig M, Devereux RB, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr Off Publ Am Soc Echocardiogr. 2005;18(12):1440–63.
Barbier P, Solomon SB, Schiller NB, et al. Left atrial relaxation and left ventricular systolic function determine left atrial reservoir function. Circulation. 1999;100(4):427–36.
Appleton CP, Kovács SJ, et al. The role of left atrial function in diastolic heart failure. Circ Cardiovasc Imaging. 2009;2(1):6–9.
Altekin RE, Yanikoglu A, Karakas MS, et al. Evaluation of left atrial function using two-dimensional speckle tracking echocardiography in end-stage renal disease patients with preserved left ventricular ejection fraction. Kardiol Pol. 2013;71(4):341–51.
Cowie MR, Struthers AD, Wood DA, et al. Value of natriuretic peptides in assessment of patients with possible new heart failure in primary care. Lancet. 1997;350(9088):1349–53.
Davis M, Espiner E, Richards G, et al. Plasma brain natriuretic peptide in assessment of acute dyspnoea. Lancet. 1994;343(8895):440–4.
De Lemos JA, McGuire DK, Drazner MH, et al. B-type natriuretic peptide in cardiovascular disease. Lancet. 2003;362(9380):316–22.
Haug C, Metzele A, Kochs M, et al. Plasma brain natriuretic peptide and atrial natriuretic peptide concentrations correlate with left ventricular end-diastolic pressure. Clin Cardiol. 1993;16(7):553–7.
Jourdain P, Funck F, Bellorini M, et al. Bedside B-type natriuretic peptide and functional capacity in chronic heart failure. Eur J Heart Fail. 2003;5(2):155–60.
Yamamoto K, Burnett JC, Jougasaki M, et al. Superiority of brain natriuretic peptide as a hormonal marker of ventricular systolic and diastolic dysfunction and ventricular hypertrophy. Hypertension. 1996;28(6):988–94.
Troughton RW, Prior DL, Pereira JJ, et al. Plasma B-type natriuretic peptide levels in systolic heart failure: importance of left ventricular diastolic function and right ventricular systolic function. J Am Coll Cardiol. 2004;43(3):416–22.
Niizuma S, Iwanaga Y, Yahata T, et al. Impact of left ventricular end-diastolic wall stress on plasma B-type natriuretic peptide in heart failure with chronic kidney disease and end-stage renal disease. Clin Chem. 2009;55(7):1347–53.
Niizuma S, Iwanaga Y, Yahata T, et al. Plasma B-type natriuretic peptide levels reflect the presence and severity of stable coronary artery disease in chronic haemodialysis patients. Nephrol Dial Transplant Off Publ Eur Dial Transpl Assoc—EurRen Assoc. 2009;24(2):597–603.
Sivalingam M, Suresh M, Farrington K, et al. Comparison of B-type natriuretic peptide and NT proBNP as predictors of survival in patients on high-flux hemodialysis and hemodiafiltration. Hemodial Int Int Symp Home Hemodial. 2011;15(3):359–65.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Abid L, S Charfeddine, and S Kammoun declare that they have no conflicts of interest.
Human rights statements and informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and later revisions. Informed consent was obtained from all patients for being included in the study.
Rights and permissions
About this article
Cite this article
Abid, L., Charfeddine, S. & Kammoun, S. Relationship of left atrial global peak systolic strain with left ventricular diastolic dysfunction and brain natriuretic peptide level in end-stage renal disease patients with preserved left ventricular ejection fraction. J Echocardiogr 14, 71–78 (2016). https://doi.org/10.1007/s12574-016-0276-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12574-016-0276-6