Abstract
Background
Heart failure with preserved ejection fraction (HFpEF) is a syndrome in which patients have symptoms and signs of heart failure but preserved ejection fraction. Left atrial (LA) volume and function are known to be impaired in these patients. Two-dimensional speckle-tracking echocardiography (2D-STE) has recently enabled the quantification of LA deformation dynamics. In this study, we evaluated the use of 2D-STE for the diagnosis of HFpEF.
Patients and methods
The study included 83 patients with suspected HFpEF. Patients were divided into two groups after HFpEF had been diagnosed according to current guidelines. Parameters of diastolic dysfunction were evaluated, including left ventricular mass index (LVMI), LA volume index (LAVI), E/A ratio, deceleration time (DT), E/E’, and STE parameters such as global longitudinal LA strain during ventricular systole (GLAs-res) and strain during late diastole (GLAs-pump).
Results
The values of BNP, LVMI, DT, LAVI, and GLAs-res were significantly different between the two groups. In univariate analysis, a strong negative correlation was seen between GLAs-res and BNP (r = −0.567, p < 0.001) as well as between GLAs-res and DT (r = −0.665, p < 0.001), while a moderate negative correlation was found between GLAs-res and LVMI (r = −0.458, p < 0.001) and GLAs-res and LAVI (r = −0.316, p = 0.004). In logistic regression analysis, GLAs-res (p = 0.049, OR = 0.71, 95 % CI = 0.451–0.99), BNP (p = 0.025, OR = 1.08, 95 % CI = 1.01–1.14), and LAVI (p = 0.042, OR = 1.59, 95 % CI = 1.02–2.48) were found to be independent predictors of HFpEF.
Conclusion
LA function as assessed by 2D-STE is impaired in patients with HFpEF. A GLAs-res value of < 17.5 % can be useful for the diagnosis of HFpEF.
Zusammenfassung
Hintergrund
Die Herzinsuffizienz mit erhaltener Ejektionsfraktion (HFpEF) stellt ein Syndrom dar, bei dem die Patienten Symptome einer Herzinsuffizienz aufweisen, aber die Ejektionsfraktion erhalten ist. Volumen und Funktion des linken Vorhofs (LA) sind bekanntermaßen bei diesen Patienten eingeschränkt. Mit der zweidimensionalen Speckle-Tracking-Echokardiographie (2D-STE) wurde vor Kurzem die Quantifizierung der LA-Deformationsdynamik ermöglicht. In der vorliegenden Studie wurde der Einsatz der 2D-STE für die Diagnosestellung einer HFpEF untersucht.
Patienten und Methoden
An der Studie nahmen 83 Patienten mit Verdacht auf HFpEF teil. Dabei wurden die Patienten in 2 Gruppen eingeteilt, nachdem die Diagnose HFpEF gemäß aktuellen Leitlinien gestellt worden war. Es wurden Parameter einer diastolischen Funktionsstörung bestimmt, dazu gehörten linksventrikulärer Massenindex (LVMI), LA-Massenindex (LAVI), E/A-Ratio (Verhältnis der frühen zur späten Mitralklappenflussgeschwindikgeit), Dezelerationszeit (DT), E/E’, und STE-Parameter, wie die globale longitudinale LA-Deformation während der Ventrikelsystole (GLAs-res) und die Deformation während der Spätdiastole (GLAs-pump).
Ergebnisse
Die Werte für BNP („brain natriuretic peptide“), LVMI, DT, LAVI und GLAs-res unterschieden sich signifikant zwischen den beiden Gruppen. In der univariaten Analyse zeigte sich eine starke negative Korrelation zwischen GLAs-res und BNP (r = −0,567; p < 0,001) sowie zwischen GLAs-res und DT (r = −0,665; p < 0,001), während eine nur mäßig ausgeprägte negative Korrelation zwischen GLAs-res und LAVI (r = −0,458; p < 0,001) sowie GLAs-res und LVMI festgestellt wurde (r = −0,316; p = 0,004). In der logistischen Regressionsanalyse stellten sich GLAs-res (p = 0,049; Odds Ratio, OR = 0,71; 95 %-Konfidenzintervall, 95 %-KI = 0,451–0,99), BNP (p = 0,025; OR = 1,08; 95 %-KI = 1,01–1,14) und LAVI (p = 0,042; OR = 1,59; 95 %-KI = 1,02–2,48) als unabhängige Prädiktoren einer HFpEF heraus.
Schlussfolgerung
Die mit der 2D-STE bestimmte LA-Funktion bei Patienten mit HFpEF erwies sich als eingeschränkt. Ein GLAs-res-Wert von < 17,5 % kann für die Diagnose einer HFpEF hilfreich sein.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Heart failure with preserved ejection fraction (HFpEF) is a clinical syndrome in which patients have symptoms and signs of heart failure (HF) but normal or near-normal left ventricular ejection fraction (LVEF). Patients with reduced ejection fraction (HFrEF) have similar signs and symptoms of heart failure [1–3]. HFpEF accounts for more than 50 % of heart failure patients [4, 5]. The primary pathology in HFpEF is diastolic dysfunction [1]. Three conditions need to be met for the diagnosis of HFpEF, namely, (a) the presence of signs or symptoms of congestive heart failure, (b) normal or mildly abnormal systolic left ventricular function, and (c) evidence of abnormal left ventricular relaxation, filling, diastolic distensibility, and diastolic stiffness [6]. According to the consensus report by the European Society of Cardiology, evidence of abnormal left ventricular relaxation, filling, diastolic distensibility, and diastolic stiffness can be shown invasively, noninvasively by tissue Doppler as E/E’ > 15, or by the rise in biomarkers such as N-terminal pro B-type natriuretic peptide (NT-proBNP) or BNP. When the E/E’ values are between <15 and >8, confirmation by BNP levels or other echocardiographic parameters such as deceleration time (DT), ratio of early (E) to late (A) mitral valve flow velocity (E/A), left ventricular mass index (LVMI), or left atrial volume index (LAVI) are required [6]. LA strain parameters are now increasingly used in daily practice, and are known to be impaired in patients with diastolic dysfunctions. In this study, we used two-dimensional speckle-tracking echocardiography (2D-STE) to evaluate the LA function in patients suspected of having HFpEF but whose E/E’ values are in the gray zone of >8 and <15. We aimed to investigate the probable use of LA strain in diagnosing HFpEF in patients who are in this gray zone.
Patients and methods
Study population
The study comprised 83 patients who underwent echocardiography examination between January 2010 and April 2012 at the Kartal Kosuyolu Cardiovascular Education and Research Hospital and Fatih University Hospital for heart failure symptoms but who had a LVEF of more than 50 % and an E/E’ more than 8 and but less than 15, and were suspected of having HFpEF . The mean age of the patients was 64.7 ± 6.2 years, and 48.2 % were female. The diagnosis of HFpEF was made according to the consensus report by the European Society of Cardiology [6]. HFpEF was diagnosed in the following cases: when BNP was more than 200 pg/ml, LAVI was greater than 40 ml/m2, LVMI was greater than 149 g/m2 (male) or greater than 122 g/m2 (female), E/A>50 yr was less than 0.5, and DT>50 yr was more than 280 ms. Patients were divided into two groups according to the presence of HFpEF. Patients with an LVEF of < 50 %, atrial fibrillation, severe obesity, and significant valvular, pulmonary, or renal diseases were excluded. All work was done in compliance with the Declaration of Helsinki and was performed with the approval of the local ethics committee.
Two-dimensional and Doppler echocardiography
All patients underwent an echocardiographic examination in the left lateral position using the GE Vivid 7 system (GE Vingmed Ultrasound AS, Horten, Norway) with a 3.5-MHz transducer. Blood pressure and heart rate were monitored during the echocardiographic examination. The data were analyzed offline using EchoPAC (GE Vingmed Ultrasound AS). Cardiac dimensions and volumes were measured according to the American Society of Echocardiography’s Guidelines, and LVEF was calculated using the biplane Simpson method [7]. Peak velocities of early and late diastolic filling, mitral E deceleration time, and mitral E/A ratio were derived from Doppler recordings of mitral inflow. Tissue Doppler imaging was used to measure mitral annular velocities. Early diastolic velocity (E’) was measured at both the mitral septal and lateral annulus, and the mean was taken. The ratio of E/E’ was calculated by using the average E’ value. LA volume was calculated using the bi-plane area–length method as described previously; LA volume = 0.85 × ((LA area in four-chamber view) × (LA area in two-chamber view))/LA length [8]. LA maximum volume (before mitral valve opening) was indexed to body surface area.
Speckle-tracking echocardiography
For speckle tracking analysis, images from apical four- and two-chamber views were obtained using conventional 2D gray-scale echocardiography. Three consecutive cardiac cycles were recorded while the patients held their breath, and averaged. The frame rate was adjusted between 60 and 80 frames/s. The data were analyzed offline using EchoPAC (GE Vingmed Ultrasound AS). The endocardial border was defined manually, and tracing was done by the software automatically for each view. Inadequately tracked segments were either corrected manually or excluded from the analysis. Overall, 976 segments were analyzed. A total of 20 (1.85 %) segments were excluded from the study because no analysis could be done manually and/or automatically. From apical four- and two-chamber views, longitudinal LA strain during ventricular systole (or reservoir phase; LAs-4C-res and LAs-2C-res) was obtained just before mitral valve opening; strain during late diastole (or pump phase; LAs-4C-pump and LAs-2C-pump) was obtained at the onset of the P wave on electrocardiography (Fig. 1). Global longitudinal LA strain during ventricular systole (GLAs-res) and late diastole (GLAs-pump) were calculated by averaging values obtained from all LA segments.
Reproducibility
Intra- and interobserver reproducibilities were assessed for both the GLAs-res and the GLAs-pump values. For intraobserver assessment, the measurements were re-analyzed after 4 weeks. Bland–Altman analysis was performed to calculate interobserver reproducibility (mean difference, 95 % confidence interval [CI]) and intraobserver reproducibility (intraclass correlation coefficient, 95 % CI); the intraclass correlation coefficient showed good inter- and intraobserver agreement: interobserver and intraobserver agreement were assessed for GLAs-res, 1.2 (−4.0–(6.4)) and 0.89 (0.81–0.93), respectively; and for GLAs-pump, −2.0 (−5.7–(1.7)) and 0.92 (0.87–0.95), respectively.
BNP measurement
Blood samples for BNP were obtained from all patients before the echocardiographic examination. BNP was measured with the use of the immunoassay method on an ADVIA Centaur-XP device (Siemens Medical Solutions, Germany) using the kits of ADVIA Centaur BNP assay (Bayer Diagnostics, Tarrytown, N.Y.).The measurable range of the BNP assay was 2.0–5,000 pg/ml. The ADVIA Centaur BNP assay had a within-run coefficient of variation of 1.8–4.3 % and a total coefficient of variation of 2.3–4.7 % at concentrations of 29.4–1,736.0 pg/ml.
Statistical analysis
Continuous variables are expressed as mean (±SD) or median as appropriate. A p value of < 0.05 was taken as significant. The independent Student t test or the Mann–Whitney U test was used to compare parametric continuous variables. For categorical variables, the chi-squared test was used. Correlations between variables were tested by using the Pearson or Spearman correlation tests as appropriate. Stepwise multivariate logistic regression analysis was applied to identify the independent predictors of HFpEF evaluated by echocardiography or blood test. Variables with a significant p value on univariate analysis (BNP, LAVI, LVMI, DT, and GLAs-res) were included in the multivariate model. Receiver-operating characteristic (ROC) curves were plotted to determine the optimal cut-off values for GLAs-res in order to predict HFpEF and to establish the optimal cut-off points for use in clinical decision making. Statistical analyses were performed using SPSS (version 15.0 for Windows).
Results
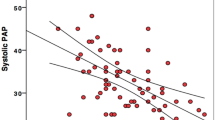
A total of 83 patients with suspected HFpEF were included in the study. The mean age was 64.7 ± 6.2 years, and 52.2 % were female. The patients were divided into two groups two according to the diagnosis of HFpEF as described in the previous section. The clinical, echocardiographic, and demographic characteristics of the patients are shown in Table 1. Baseline demographic and hemodynamic parameters, New York Heart Association (NYHA) class, body mass index (BMI), diabetes mellitus (DM), and hypertension (HT) were similar between the two groups. Of the patients, 36 had NYHA class II and 47 had NYHA class III symptoms. The average E/E’ was 11.22 ± 1.71. In all, 37 patients had high BNP, 26 patients had LAVI > 40 ml/m2, and 15 had increased LVMI. Patients with HFpEF had higher BNP (248.7 ± 48.7 vs. 165.6 ± 26.7 pg/ml, p < 0.001), higher LVMI (132 ± 33.4 vs. 107.1 ± 17.4 g/m2, p < 0.001), higher DT (259.9 ± 44.1 vs. 231 ± 31.5 ms, p = 0.001), and increased LAVI (43.7 ± 9.4 vs. 34.1 ± 3.7 ml/m2, p < 0.001). The GLAs-res value was significantly different between the two groups (17 ± 4.1 vs. 31.9 ± 10.5 %, p < 0.001; Table 2). In univariate analysis, a good negative correlation was seen between GLAs-res and BNP (r = −0.567, p < 0.001) as well as GLAs-res and DT (r = −0.665, p < 0.001), while a moderate negative correlation was found between GLAs-res and LAVI (r = −0.458, p < 0.001) and GLAs-res and LVMI (r = −0.316, p = 0.004). Parameters found to be statistically significant predictors of HFpEF in univariate analysis – i.e., LAVI, BNP, GLAs-res, DT, and LVMI – were studied by logistic regression analysis. GLAs-res, BNP, and LAVI were found to be independent predictors of HFpEF (Table 3). In ROC analysis, the area under the curve (AUC) to predict HFpEF was 0.899 (95 % CI, 0.836–0.962, p < 0.001). A GLAs-res value of < 17.5 % predicted HFpEF with 89 % sensitivity and 55.3 % specificity (Fig. 2). The correlations between GLAs-res and BNP, DT, LAVI, and LVMI are shown in Table 4.
Discussion
In this study, we explored LA functions by 2D-STE in patients with HFpEF. The diagnosis of HFpEF usually demands the use of a set of echocardiographic criteria and can sometimes be challenging. In our study, we found that the LA strain value can give us some idea of HFpEF before the results of BNP testing are attained. Heart failure with preserved LVEF is a clinical syndrome in which patients have symptoms and signs of heart failure, normal or near-normal LVEF, normal or near-normal LV volume, and evidence of diastolic dysfunction [1, 9, 10]. It has been reported to account for more than 50 % of all heart failure patients [4, 5]. The prevalence of HFpEF increases with age [1, 11, 12] and is reported to be more common in women than in men [13–16]. In HFpEF, dyspnea due to pulmonary congestion is frequently the earliest symptom, whereas muscle fatigue is more prominent in heart failure with reduced EF owing to the reduced cardiac output, impairment of vasodilator capacity, and abnormalities of skeletal muscle metabolism [17]. The assessment of LV diastolic function should be part of a routine examination in patients presenting with signs or symptoms of heart failure. The assessment of diastolic function and filling pressures is of great clinical importance for distinguishing this syndrome from other diseases such as pulmonary disease resulting in dyspnea, for assessing the prognosis, and for identifying underlying cardiac disease and planning the best treatment. Evidence of impaired LV relaxation, filling, diastolic distensibility, and diastolic stiffness can be acquired invasively, and is considered as providing definite evidence of HFpEF [6]. Noninvasively, blood flow Doppler and tissue Doppler assessments can be used. The ratio of E, early mitral valve flow velocity, to E’, early tissue Doppler lengthening velocity (E/E’), has been suggested as the best parameter for determining LV filling pressure [6]. When E/E’ is greater than 15, elevated LV filling pressure is established, and HFpEF can be diagnosed, whereas an E/E’ of less than 8 excludes an elevated LV filling pressure. When the E/E’ is in the borderline zone of >8 to <15, more parameters are needed to confirm the diagnosis, such as the difference between the duration of reversed pulmonary vein atrial systole flow (Ard) and the duration of mitral A wave flow (Ad; Ard-Ad > 30 ms), E/A>50 yr < 0.5 and DT>50 yr > 280 ms, LAVI > 40 ml/m2, LVMI > 122 g/m2 (female) and >149 g/m2 (male), or atrial fibrillation. We aimed to evaluate the LA strain values in patients who were in the gray zone of E/E’ >8 and <15.
Recently, LA functions have been widely studied using speckle-tracking echocardiography. Previous studies have shown that LA strain was impaired in patients with both HFpEF and HFrEF [18–22]. It has been reported that LA strain is impaired in patients with diabetes and hypertension even if the size of the left atrium is normal (LA volume indexes < 28 ml/m2) [23]. Guler et al. reported in their study that GLAs-res and GLAs-pump were closely related to LV filling pressure and their values were negatively correlated with NT-proBNP and LA volumetric parameters in patients with nonischemic cardiomyopathy [24]. In the current study, we aimed to find the LA strain values for correctly diagnosing HFpEF. We measured GLAs-res (global longitudinal LA strain during ventricular systole) and GLAs-pump (global longitudinal LA strain during late diastole) in HFpEF patients who are in the gray zone of 8 > E/E’ < 15. We found that the GLAs-res value was significantly different between the two groups (17 ± 4.1 vs. 31.9 ± 10.5 %, p < 0.001). In ROC analysis, the AUC to predict HFpEF was 0.899 (95 % CI, 0.836–0.962, p < 0.001). GLAs-res < 17.5 % predicted HFpEF with 89 % sensitivity and 55.3 % specificity (Fig. 2). This parameter may be useful for the bedside diagnosis of HFpEF when BNP is not yet available or as an additional parameter to the current criteria.
Limitations
For the evaluation of LA strain, we used the software for LV analysis, which might have influenced the echocardiographic results. Obtaining optimal images for the 2D-STE study of the left atrium was sometimes challenging. Furthermore, the study was performed with a relatively small number of patients. Studies with a larger sample size are needed to give a definitive cut-off point for the diagnosis of heart failure with preserved ejection fraction.
Conclusion
LA function as assessed by 2D-STE is impaired in patients with HFpEF. GLAs-res might be useful as an additional tool for the diagnosis of HFpEF.
References
Zile MR, Brutsaert DL (2002) New concepts in diastolic dysfunction and HFpEF: Part I: diagnosis, prognosis, and measurements of diastolic function. Circulation 105:1387
Aurigemma GP, Gaasch WH (2004) Clinical practice. Diastolic heart failure. N Engl J Med 351:1097
Paulus WJ, Tschöpe C, Sanderson JE et al (2007) How to diagnose diastolic heart failure: a consensus statement on the diagnosis of heart failure with normal left ventricular ejection fraction by the heart failure and echocardiography associations of the european society of cardiology. Eur Heart J 28:2539
Owan TE, Hodge DO, Herges RM et al (2006) Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med 355:251–259
Abhayaratna WP, Marwick TH, Smith WT et al (2006) Characteristics of left ventricular diastolic dysfunction in the community: an echocardiographic survey. Heart 92:1259–1264
Paulus WJ, Tschöpe C, Sanderson JE et al (2007) How to diagnose diastolic heart failure: a consensus statement on the diagnosis of heart failure with normal left ventricular ejection fraction by the heart failure and echocardiography associations of the european society of cardiology. Eur Heart J 28(20):2539–2550
Lang RM, Bierig M, Devereux RB et al (2006) American society of echocardiography’s nomenclature and standards committee; task force on chamber quantification; american college of cardiology echocardiography committee; american heart association; european association of echocardiography, european society of cardiology. recommendations for chamber quantification. Eur J Echocardiogr 7(2):79–108
Kircher B, Abbott JA, Pau S et al (1991) Left atrial volume determination by biplane two-dimensional echocardiography: validation by cine computed tomography. Am Heart J 121(3 Pt 1):864–871
Aurigemma GP, Gaasch WH (2004) Clinical practice. Diastolic heart failure. N Engl J Med 351(11):1097–1105
Paulus WJ, Tschöpe C, Sanderson JE et al (2007) How to diagnose diastolic heart failure: a consensus statement on the diagnosis of heart failure with normal left ventricular ejection fraction by the heart failure and echocardiography associations of the european society of cardiology. Eur Heart J 28:2539
Topol EJ, Traill TA, Fortuin NJ (1985) Hypertensive hypertrophic cardiomyopathy of the elderly. N Engl J Med 312(5):277–283
Gottdiener JS, McClelland RL, Marshall R et al (2002) Outcome of congestive heart failure in elderly persons: influence of left ventricular systolic function. The cardiovascular health study. Ann Intern Med 137(8):631
Masoudi FA, Havranek EP, Smith G et al (2003) Gender, age, and heart failure with preserved left ventricular systolic function. J Am Coll Cardiol 41:217
Kitzman DW, Gardin JM, Gottdiener JS et al (2001) Importance of heart failure with preserved systolic function in patients > or = 65 years of age. CHS research group. Cardiovascular health study. Am J Cardiol 87:413
Devereux RB, Roman MJ, Liu JE et al (2000) Congestive heart failure despite normal left ventricular systolic function in a population-based sample: the strong heart study. Am J Cardiol 86:1090
Smith GL, Masoudi FA, Vaccarino V et al (2003) Outcomes in heart failure patients with preserved ejection fraction: mortality, readmission, and functional decline. J Am Coll Cardiol 41:1510
Packer M (1990) Abnormalities of diastolic function as potential cause of exercise intolerance in chronic heart failure. Circulation 81(86):III–78
Morris DA, Gailani M, Vaz PA et al (2011) Left atrial systolic and diastolic dysfunction in heart failure with normal left ventricular ejection fraction. J Am Soc Echocardiogr 24(6):651–662
Kurt M, Wang J, Torre-Amione G et al (2009) Left atrial function in diastolic heart failure. Circ Cardiovasc Imaging 2(1):10–15
Santos AB, Kraigher-Krainer E, Gupta DK et al (2014) Impaired left atrial function in heart failure with preserved ejection fraction. Eur J Heart Fail 16(10):1096–1103
Nascimento CA, Gomes VA, Silva SK et al (2013) Left atrial and left ventricular diastolic function in chagas disease. J Am Soc Echocardiogr 26(12):1424–1433
Sahebjam M, Zoroufian A, Sadeghian H et al (2013) Relationship between left atrial function and size and level of left ventricular dyssynchrony in heart failure patients. Echocardiography 30(7):772–777
Mondillo S, Cameli M, Caputo ML et al (2011) Early detection of left atrial strain abnormalities by speckle tracking inhypertensive and diabetes patients with normal left atrial size. J Am Soc Echocardiogr 24(8):898–908
Guler A, Tigen KM, Dundar C et al (2014) Left atrial deformation and nonischemic dilated cardiomyopathy. A 2D speckle-tracking imaging study. Herz 39(2):251–257
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
S.M. Aung, A. Güler, Y. Güler, A. Huraibat, C.Y. Karabay, and I. Akdemir state that there are no conflicts of interest.
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964, as revised in 2013. Informed consent was obtained from all patients for being included in the study.
Rights and permissions
About this article
Cite this article
Aung, S.M., Güler, A., Güler, Y. et al. Left atrial strain in heart failure with preserved ejection fraction. Herz 42, 194–199 (2017). https://doi.org/10.1007/s00059-016-4456-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-016-4456-y