Abstract
Phage therapy is revolving to address the issues mainly dealing with antibiotic resistance in the pathogenic bacteria. Among the drug-resistant microbial populations, the bacterial species have been categorized as high-priority or critical-priority bacteria. This review summarizes the efficiency and development in phage therapy used against these drug-resistant bacteria in the past few years mainly belonging to the critical- and high-priority list. Phage therapy is more than just an alternative to antibiotics as it not only kills the target microbial population directly but also leads to the chemical and physical modifications in bacterial cell structures. These phage-mediated modifications in the bacterial cell may make them antibiotic sensitive. Application of phage therapy in antibiotic-resistant foodborne bacteria and possible modulation in gut microbes has also been explored. Further, the phage cocktail antibiotic formulation, containing more than one type of phage with antibiotics, has also been discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It has been more than a century when the bacteriophages were first reported in the waters of the rivers Ganges and Yamuna in India for their distinguished antibacterial action against Vibrio cholerae (Hankin, 1896). First bacteriophage therapy or phage therapy was used to treat bacterial infection during 1910–1917 and commercially produced during the 1940s. However, since the discovery of antibiotics, most of the countries stopped the usage of bacteriophage for treatment (Sulakvelidze et al., 2001). Antibiotic therapy has been very successful in the treatment of a wide range of bacterial infections. The emergence and transfer of antimicrobial resistance among pathogenic microbial community alerted the scientific community and health care practitioners to look for alternate therapies.
Higher antibiotic resistance is prominent in bacterial biofilms as compared to an individual cell. Biofilms are made up of self-produced extracellular polymeric substances (EPS) to provide surface attachment and increased resistance to antibiotics. This resistance mechanism involves a combination of mechanisms within biofilm cells. Antibiotic resistance genes may be present on the bacterial genome, plasmid, or can be taken up by Horizontal gene transfer (HGT), which seems to be the most common mode for transferring the resistance. Understanding of genotypes at a depth might allow the further understanding of phenotypic changes that imparts the resistance (Banin et al., 2017).
Antibiotic resistance ultimately results in an antibiotic failure during the treatment. Bacteriophage or phages therapy is regaining the importance to deal with antibiotic failure. Bacteriophages are infectious viral particles, which may invade and kill the bacterial cell through the lytic cycle. These Bacteriophages are highly specific toward their target and bind to cell surface receptors. The lytic cycle releases new infectious virions, which may further infect the nearby bacterial cells, thus reducing the target bacterial population (Nobrega et al., 2018). There are a number of advantages associated with phage therapy as it may work with single-dose potential. As the virulent phages have the ability to increase their number till the availability of host bacterial cells thus further follow auto-dosing. The numbers of bacteriophages are regulated through auto-dosing without affecting the other microbial cells. However, in many cases, including animals a single dose may not work well and several doses may be required. Bacteriophage attack on host bacterial cell sometimes results in phage resistance by modifying the cell surface targets. These phage-resistant bacterial strains do not allow a particular bacteriophage to infect the cell; thus, the phage is unable to replicate in bacterial cell. Phage cocktail development has the potential to deal with such issues (Yen et al., 2017). A phage cocktail contains more than one type of bacteriophages with different strategy or receptor sites to attack the bacterial cells. It is worth mentioning here that the phages may attack on specific bacterial species, whether they are resistant to an antibiotic or not. So, the idea behind using phage cocktail is to increase the host range (the ability of bacteriophage to infect diverse bacterial strains or species). This host range includes (i) antibiotic-resistant pathogenic strains, (ii) non-resistant pathogenic strains, and (iii) particular phage-resistant pathogenic strains. Restoration or enhanced sensitivity toward antibiotics has also been observed in infectious microbes during phage treatment (Chan et al., 2018). Bacteriophages are abundantly present in the human body. However, their direct relationship with the human is still being explored. Some studies point toward a complex association related to direct cure from infectious bacteria or supporting the human immune system. Bacteriophages may also influence the mammalian host cell to kill the infection-causing bacteria through a number of mechanisms (Bodner et al., 2020).
Overall the platform is open to discuss the potential role of bacteriophages in clinical treatments. Thus, this review summarizes the antibiotic resistance in bacteria mainly included in priority lists, different phages used against critical and high-priority antibiotic-resistant bacteria, and advantages of phage cocktail on the basis of in vitro and in vivo experiments. Further, the mechanisms involved in the restoration of antibiotic sensitivity in drug-resistant bacteria were emphasized. Bacteriophage therapy in combination of antimicrobial or antibiotic compounds has also been discussed, which seems to be a future direction of this research.
Antibiotic-Resistant Bacteria in Priority List
The spread of antibiotic-resistant bacteria poses a substantial threat to morbidity and mortality worldwide. A lot of literature is available on different mechanisms and the emergence of antibiotic resistance in pathogenic bacteria (Wilson et al., 2020; Yelin & Kishony, 2018). WHO categorized antibiotic-resistant "priority pathogens" in it’s first-ever list. These antibiotic-resistant bacteria were stratified in the priority list as critical, high, and medium priority. On the basis of this categorization, carbapenem-resistant Acinetobacter baumannii, Pseudomonas aeruginosa, carbapenem-resistant, and third-generation cephalosporin-resistant Enterobacteriaceae were included in the critical-priority bacteria list. The high-priority bacteria list consists of vancomycin-resistant Enterococcus faecium, methicillin-resistant Staphylococcus aureus, clarithromycin-resistant Helicobacter pylori, fluoroquinolone-resistant Campylobacter spp., Neisseria gonorrhoeae, and Salmonella typhi (Tacconelli et al., 2018). Antibiotic failure is commonly observed in the case of infection with these antibiotic-resistant bacteria. Thus, there is an urgent need to take care of these drug-resistant bacteria along with some multidrug-resistant bacteria, which could be life-threatening. There are a number of phages that have been used against infectious bacteria and we have selected a few recent studies dealing with antibiotic-resistant bacterial strains.
The ESKAPE pathogens (Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter species) are the opportunistic pathogens involved in nosocomial infections. These bacterial species are continuously developing antibiotic resistance (Ma et al., 2020). High pathogenicity and emergence of antibiotic resistance in these pathogens have allowed them to be in the priority list.
Phage Therapy for Critical-Priority Antibiotic-Resistant Bacteria
The most critical group of multidrug-resistant bacteria includes Acinetobacter, Pseudomonas, and various Enterobacteriaceae. These bacteria are particularly associated with hospitals-acquired infections. Table 1 enlists few recent studies related to the application of bacteriophages against antibiotic-resistant high-priority bacteria. Acinetobacter baumannii is a Gram-negative nosocomial pathogen species. Phage therapies have been used against antibiotic-resistant strains of A. baumannii. A lytic phage Bϕ-R2096 ameliorated histologic damage to lungs infected by carbapenem-resistant A. baumannii in Galleria mellonella larvae and a mouse model during acute pneumonia. There was no mortality or any significant side effects that were observed in phage-treated groups during the 15 days of treatment. Thus, the study strongly suggested the use of lytic phage Βϕ-R2096 as an alternative antibacterial agent to treat A. baumannii infections (Jeon et al., 2019). Similarly, two lytic bacteriophages WCHABP1 and WCHABP12 belonging to the Myoviridae family were able to infect about 50% of the carbapenem-resistant strains of A. baumannii isolated from clinical samples. A. baumannii infection in Galleria mellonella larva could efficiently be treated with these bacteriophages, which increased the survival rate of these larvae up to 75% (Zhou et al., 2018). Phage SH-Ab15519 belonging to the Podoviridae family was considered to be safe for phage therapy on the basis of its complete genome analysis. In vivo study on a mice suffering from lethal A. baumannii lung infections successfully demonstrated that phage SH-Ab15519 could effectively rescue the mice without any side effects (Hua et al., 2018).
It is important for the lytic phages to efficiently destroy the bacterial biofilms along with free planktonic cells. Two phages ISTD and NOVI have shown their activity against carbapenem-resistant A. baumannii strain 6077/12. Phage ISTD could reduce 3.5 log in planktonic cells, while 2 log biofilm-associated viable bacterial cells and also demonstrated a broader host range, when tested against different clinically isolated A. baumannii strains in terms of better adsorption rate and larger burst size (Vukotic et al., 2020). Supplementation of antibiotics also augmented the antibacterial property of bacteriophage. KARL-1, a lytic phage belonging to the Myoviridae family, was effective against 40% of multidrug-resistant clinical isolates of A. baumannii. This bactericidal activity was significantly enhanced by supplementation of meropenem and colistin antibiotics. The therapeutic outcome of the study confirmed a positive influence on the antibacterial activity of KARL-1 by the supplementation of traditional antibiotics (Jansen et al., 2018). Multidrug-resistant Acinetobacter baumannii may cause severe urinary tract infections (UTI). A randomized, placebo-controlled, double-blind trial investigating bacteriophages in UTI treatment revealed that the bacteriophages seem to be potentially revolutionizing treatment option (Leitner et al., 2017).
P. aeruginosa is a widespread Gram-negative opportunistic pathogen in natural and domestic environments. It may cause severe infections and the treatment becomes difficult in the case of multidrug resistance strain. Three lytic phages SL1, SL2, and SL4 isolated from hospital sewage demonstrated their activity against different clinical isolates of multidrug-resistant P. aeruginosa. SL2 demonstrated its activity against planktonic cells, while SL4 showed significant anti-biofilm activity. Phage SL1 rescued bacteria-infected Galleria melonella larvae (Latz et al., 2017). Similarly, lytic phages MAG1 and MAG4 were active against different antibiotic-resistant strains of P. aeruginosa including carbapenem-resistant P. aeruginosa (Kwiatek et al., 2017). In both the studies, the application of phages cocktail was suggested against antibiotic-resistant strains. However, few more detailed studies are required before human trials of these phages.
There are a number of ongoing human clinical trials to investigate the safety and efficiency of the phage cocktail therapy. In a randomized phase 1 and 2 trials, patients with a confirmed burn wound clinically infected with P aeruginosa were given a cocktail of 12 natural lytic anti-P aeruginosa bacteriophages or standard care (1% sulfadiazine silver emulsion cream). The study revealed that low concentrations of phage cocktail decreased bacterial burden in burn wounds at a slower pace than standard of care. However, further studies using increased phage concentrations in a larger sample size are warranted (Jault et al., 2019). Clinical trial involving phage cocktail-SPK as an adjunct to standard therapy for the prevention and treatment of burns susceptible to infection/or infected by S. aureus, P. aeruginosa, or K. pneumoniae species is underway. Phase I of this trail involves the application of phage- cocktail-SPK spray for second degree burn wounds (less than 10 percent of total body surface area) in adult patients. This phage cocktail-SPK spray may be used with Xeroform primary dressing and Kenacomb topical antibiotic cream (for wounds with signs of localized infection). This trial is estimated to be completed by August 2021 (ClinicalTrials.gov NCT Number: NCT04323475). Few recent human clinical trials of phage cocktail have been enlisted in (Table 2).
Family Enterobacteriaceae includes different Gram-negative facultative anaerobic opportunistic pathogenic bacteria, which can cause a variety of chronic and acute diseases. Escherichia coli, Klebsiella spp., and Enterobacter spp. are well-known disease-causing members of Enterobacteriaceae. Multidrug resistance in these bacteria is becoming more challenging day by day. The emergence of antibiotic resistance in E. coli biofilms has become challenging and is associated with higher antibiotic treatment failure rates. A lytic bacteriophage ɸWL-3 in combination with fosfomycin has been successfully tested against the biofilm of ciprofloxacin/ceftriaxone-resistant E. coli strain. The in vivo study using a Galleria mellonella infection model enhanced the survival rates of infected larvae when ɸWL-3/fosfomycin was used against E. coli infected larvae (Wang et al., 2020). Similarly, a combination of a lytic phage ΦEcSw and antibiotic ampicillin significantly inhibited the growth of an antibiotic-resistant E. coli Sw1. Phage ΦEcSw also showed clinical relevance through its effectiveness in treating the bacterial infected zebrafish and mice. This provides a solution to overcome the challenges of antibiotic resistance and phage resistance (Easwaran et al., 2020). Among different parameters of phage selection during phage therapy, the strict lytic nature of the bacteriophages along with a large burst size is also important. Lytic phage phiLLS significantly reduced the growth of multidrug-resistant E. coli. This phage belongs to the Siphoviridae family and exhibited a large burst size. The genome analysis of phage phiLLS confirmed it's strict lytic and absence of virulence genes, which further endorsed its potential application in phage therapy (Amarillas et al., 2017).
Phage-antibiotic synergistic effects refer to the increase in phage production in the presence of certain antibiotics (Kim et al., 2018). This synergistic effect may efficiently destroy the bacterial cells in different states i.e., planktonic, sessile, or in biofilms. It also reduces the chances of the pathogen to escape as either phage or antibiotic will destroy the bacterial cell. Personalized phage therapy also seems to be a promising approach as a case report confirmed the eradication of multidrug-resistant, carbapenemase-producing Klebsiella pneumoniae infection. Custom-made, lytic bacteriophage preparation was administered to the patient, which subsequently eradicated the Klebsiella infection without any adverse effect (Corbellino et al., 2020). Another case study reported successful eradication of recurrent urinary tract infection caused by extensively drug-resistant K. pneumonia. The application of a phage cocktail consists of six lytic phages (Kp152, Kp154, Kp155, Kp164, Kp6377, and HD001) and antibiotics trimethoprim-sulfamethoxazole demonstrated a strong synergistic effect against the bacterial infection. This phage-antibiotic combination also inhibited the emergence of phage resistance in bacterial cells (Bao et al., 2020a, 2020b). A phage cocktail consisted of the multidrug-resistant A. baumannii infecting bacteriophages, in combination with antibiotics could destroy the bacterial biofilm in human urine model. It was further observed that some of the antibiotics commonly used in the treatment of urinary tract infection acted synergistically with phage cocktails (Grygorcewicz et al., 2021).
In the genus Enterobacter, E. cloacae and E. aerogenes are often considered pathogens. Multidrug-resistant strains are also quite common in both of these species. A circularly permuted linear double-stranded DNA containing E. aerogenes infecting bacteriophage ATCEA85 has been isolated and characterized recently (Oh et al., 2020). Bacteriophage MJ2 belongs to the Podoviridae family could reduce the biofilm of chronic infection-causing multidrug-resistant E. cloacae. The phage was also active against the planktonic bacterial cells (Jamal et al., 2019). Carbapenem-resistant E. aerogenes has been successfully lyzed by a lytic phage vB_EaeM_φEap-3. Phage vB_EaeM_φEap-3 belongs to the family Myoviridae and does not contain any undesirable genes (e.g., the genes encoding for antibiotic resistance, toxin production, or integrase). Based on the host range and different physiological parameters it was suggested that phage vB_EaeM_φEap-3 may be a suitable candidate for phage therapy against antibiotic-resistant E. aerogenes (Zhao et al., 2019).
Broad host range activity of the bacteriophage cocktail against all the three drug-resistant bacteria (Escherichia coli, Klebsiella spp., and Enterobacter spp.) has been prepared, which consists of three bacteriophages myPSH2311, myPSH1235 (Podoviridae family) and myPSH1140 (Myoviridae family). This phage cocktail was successfully used against multiple bacterial mixtures, resistant to meropenem and colistin that reduced the bacterial load within 2 h (Manohar et al., 2019).
Phage Therapy for High-Priority Antibiotic-Resistant Bacteria
High and medium priority categories include the drug-resistant bacteria, which cause some common diseases e.g., gonorrhea and foodborne pathogens like Salmonella. Few recently used bacteriophages against high-priority antibiotic-resistant bacteria are listed in Table 3. Gram-positive opportunistic pathogen Enterococcus faecalis causes nosocomial infections and commonly associated with recalcitrant endodontic infections. E. faecalis is resistant to several routinely used antibiotics and some strains are resistant to vancomycin. The antibiotic resistance and biofilm-forming ability of E. faecalis may lead to serious therapeutic problems. Several phages belonging to Siphoviridae have been isolated from the oral cavity of patients suffering from root canal infections that target E. faecalis. One of the lytic phages SHEF2 could eradicate E. faecalis biofilm in vitro along with a lethal infection in zebrafish (Al-Zubidi et al., 2019). Bacteriophage therapy has also been proposed as a potential alternative therapy to treat nosocomial infections caused by vancomycin-resistant Enterococcus. Lytic bacteriophage SRG1 belongs to the family Myoviridae has been successfully used against the Vancomycin-Resistant E. faecalis (Rahmat Ullah et al., 2017). E. faecalis specificity lytic phage EF-P29 belongs to the Siphoviridae family showed a broad host range against different E. faecalis strains, including vancomycin-resistant E. faecalis. Genome analysis of EF-P29 confirmed that it does not contain any putative virulence factors, antibiotic resistance genes, or integration-related proteins. A study on the mouse model reported that the vancomycin-resistant E. faecalis was rapidly eliminated from the blood of infected mice using phage EF-P29. This phage also alleviated the gut microbiota imbalance caused by E. faecalis (Cheng et al., 2017a). A Lytic bacteriophage EFA1 has disrupted E. faecalis biofilms. This bacteriophage also modulated the growth stimulatory effects of E. faecalis in a HCT116 colon cancer cell co-culture system, which further reduces its associated potential to develop colorectal cancers (Kabwe et al., 2021).
Methicillin-resistant Staphylococcus aureus (MRSA) is a multidrug-resistant pathogenic bacterium. Staphylococcus induces cellular apoptosis, while its fibronectin-binding proteins allow other bacteria to initiate secondary infections. MRSA has also shown resistance toward common antibiotics, which made its treatment more challenging. Thus, bacteriophage therapy has been proposed as an effective alternative against this life-threatening MRSA (Nasser et al., 2019). Phage ɸMR003 showed a wide host range by infecting clinical and community-associated MRSA strains. Wall teichoic acid of S. aureus has been recognized as a receptor site for phage ɸMR003. No virulence genes (tRNA and antibiotic resistance genes) were detected in its genome, which endorsed its safety for phage therapy (Peng et al., 2019).
S. aureus is one of the major causative agents of bovine mastitis (an inflammation of the mammary gland) in cattle. Proliferation of different S. aureus strains including MRSA has been reduced by phage therapy using ΦSA012 and ΦSA039 bacteriophages in mouse mastitis model. It was suggested that phage therapy may reduce the treatment cost by reducing antimicrobial doses and also effective against MRSA (Iwano et al., 2018). To eradicate the MRSA biofilm there are a few commercial phage formulations also available. Two commercially available phage formulations including monophage Sb-1 and a polyphage PYO have been evaluated for preventing and eradicating an in vitro biofilm of MRSA as well as in vivo efficacy on a Galleria mellonella model of MRSA systemic infection. These phage formulations were promising for preventing the colonization and killing bacteria in biofilms (Tkhilaishvili et al., 2020). Staphylococcus aureus bacteriophage Sb-1 has shown its potential activity against two MRSA strains when used alone or with antibiotic combinations i.e., daptomycin-phage and vancomycin-phage combinations (Kebriaei et al., 2020).
Gonorrhea is a frequently reported disease around the globe. Drug-resistant Neisseria gonorrhoeae have acquired several resistance mechanisms to all antimicrobials used for the treatment. Besides this, no successful phage therapy has been reported against antibiotic-resistant N. gonorrhoeae to date. This has triggered the scientists to find an effective alternative against multidrug-resistant N. gonorrhoeae strains (Suay-García & Pérez-Gracia, 2017). Thus, it seems to be an urgent need to look for new lytic bacteriophages, specific to multidrug-resistant N. gonorrhoeae, and validate their clinical application. As reported by several studies mentioned in this article, a phage cocktail or a combination of phage with antibiotics may be explored to establish a successful alternative treatment strategy.
Recently, different bacteriophages against antibiotic-resistant ESKAPE pathogens have been isolated from river Ganga’s water, which suggested this river’s water to be a huge source of diverse bacteriophages (Mishra & Nath, 2020). Clinical studies involving bacteriophage therapy against ESKAPE pathogens have been reviewed recently and suggested appropriate phage selection criteria, as well as recommendations for clinicians and scientists for a successful therapy (El Haddad et al., 2019). It has been suggested that extensive bacteriophage cocktails, and bacteriophage in combination with antibiotics are needed to develop as an effective therapeutics against ESKAPE infections (Patil et al., 2021). There are a number of animal models have been used to evaluate the efficiency of phage therapy. But, the results obtained from the phage therapy on different animal models cannot be applied directly in human body. However, the knowledge gained from these animal model based experiments seems to be valuable and helpful to evaluate the effectiveness of phage therapy in the case of ESKAPE pathogens (Cieślik et al., 2021).
Phage Therapy for Foodborne Illnesses
The frequency of antibiotic resistance in foodborne bacterial pathogens is a growing concern; these bacteria are primarily included in the high-priority list. Among different foodborne bacterial infections, Salmonella infection is quite common, and different strains of this bacterium have already acquired antibiotic resistance. In the present scenario, phage therapy may be advantageous. Salmonella spp. with more than 2500 serovars require broad-host-range bacteriophages for clinical therapy. To effectively control the Salmonella food contamination, lytic phage LPSE1 with a broad Salmonella host range, extensive pH tolerance, and prolonged thermal stability has been explored. Phage LPSE1 could efficiently control the growth of Salmonella (Salmonella enterica subsp. enterica serovar Enteritidis) in milk, sausage, and lettuce. These results seem to be promising to develop a lytic phage-based effective formulations against pathogenic Salmonella species present in various ready to eat foods (Huang et al., 2018).
For the bacteriophages used during food processing, it is also important to ensure the safety related to oral toxicity and foodborne allergens. Further, it is worth mentioning here that phages may work well when their host bacteria are available at high concentration. But when the numbers of bacterial cells are low (which is expectable in a food processing plant) phages might not encounter with these cells, and then the use of phages in this application may be limited. A lytic phage STP4-a demonstrated a broad host range by infecting about 96% (88 out of 91) of the tested Salmonella strains. In silico analyses further confirmed the absence of any known lysogeny factors and pathogenic or toxicity related genes. In the poultry industry, the chicken's pretreatment with phage STP4-a was suggested to be an effective food additive approach to control Salmonella infection (Li et al., 2020a, 2020b). An extended-spectrum β-lactamase producing Salmonella (Salmonella enterica subsp. enterica serovar Typhi) with decreased ciprofloxacin susceptibility has been successfully infected by different bacteriophages. There were some lysogenic bacteriophages, which did not show any adverse effect on the growth of Salmonella. All the lytic phages belong to the Siphoviridae family (Kakabadze et al., 2018). This study further indicates that the lytic and lysogenic nature of phages must be confirmed before their application. Lytic phages may rapidly kill the bacterial cells by multiplying its genetic material and forming new virions. On the other hand, lysogenic phages may integrate their genetic material into host’s chromosome and may live there for generations as prophage. These phages may also transfer some antibiotic resistance genes to bacterial cell through transduction. However, it is also possible to convert lysogenic phages into lytic ones by removing the genes involved in lysogeny e.g., vir genes (McCallin et al., 2013).
Shigellosis is another acute enteric infection caused by Shigella spp. Among Shigella spp., Shigella flexneri causes severe dysentery with high frequency in the emergence of multidrug-resistant strains. Phage therapy has been suggested for the management of S. flexneri contamination in foodstuffs. A lytic phage B_SflS-ISF001 reduced S. flexneri growth in vitro, indicated its high potential for developing a phage formulation against multidrug-resistant S. flexneri (Shahin & Bouzari, 2018).
Antibiotic-resistant Campylobacter jejuni is another high-priority bacterium, which causes foodborne illness. Different bacteriophage formulations have been developed against such foodborne pathogens. A thermally stable dry powder containing bacteriophage CP 30A was formulated against C. jejuni (Carrigy et al., 2019). The application of Campylobacter specific bacteriophages has been explored in the poultry meat production chain, which appears as a promising food safety tool for the biocontrol of this pathogen (Nafarrate et al., 2020). Overall, bacteriophages are extensively explored for their application against different multidrug-resistant foodborne pathogens. The strategies dealing with, preparation of bacteriophage containing food additive preparations, direct coating of the packaging material, and release of phages from food packaging material to control the microbial contaminations needs to be investigated.
Phage Resistance in Bacteria
There are a number of phage resistance mechanisms in bacteria including outer membrane vehicles (OMVs), inhibition of phage adsorption, and blocking phage DNA injection (Azam & Tanji, 2019). OMVs act as the first line of bacterial defense against phage attack. Bacteria provide OMVs as phage receptor site and phages may inject their genetic material into these vesicles, which do not allow the phage genetic material to further replicate in the bacterial cell cytoplasm using host cell machinery (Azam & Tanji, 2019). Cleavage of injected phage genetic material is another well-employed defense mechanisms by the host bacterial cell. Bacteria may alter the phage receptors by blocking them through the overproduction of exopolysaccharides or binding proteins. Super infection exclusions can block the entry of phage DNA by overproduction of proteins. Another important method includes clustered regularly interspaced short palindromic repeats (CRISPRs) and CRISPR-associated (cas) genes. This CRISPR–Cas system may destroy the foreign phage DNA to protect the cell. All these mechanisms have already been described in detail earlier (Labrie et al., 2010).
Similar to antibiotics, there is also a possibility to develop phage resistance in bacteria, which may restrict the execution of clinical phage therapy. The emergence of phage resistance in bacteria may lead to some mutations, which alter their cell surface receptors. Some phage-induced modifications include reduced virulence and biofilm formation ability and resensitization to antibiotics (Mangalea & Duerkop, 2020). Recent study on the emergence of phage resistance in E. faecium demonstrated that the development of resistance was conferred through an array of cell wall-associated molecules, which include secreted antigen A, enterococcal polysaccharide antigen, wall teichoic acids, capsule, and an arginine-aspartate-aspartate protein. Phage resistance leads to the mutation in secreted antigen A and enterococcal polysaccharide antigen may resensitize the bacteria against the some antibiotics. It was observed that the phages may synergize with cell wall-acting antibiotics (ceftriaxone and ampicillin) and membrane-acting antibiotic (daptomycin) to reduce or inhibit the growth of E. faecium (Canfield et al., 2021).
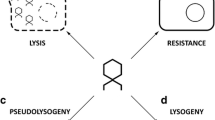
Phage resistance in bacterial strains has been observed during animal as well as in human clinical trials. However, bacterial mutations that confer phage resistance could be beneficial to the host as these strains may lose their pathogenicity or again resensitize to antibiotics (Oechslin, 2018). Bacteriophages-mediated transduction may lead to the dissemination of antibiotic resistance genes through their lysogenic cycle. However, some studies reported that this lysogenic cycle may incorporate the sensitivity toward some antibiotics, while few studies suggested a phage-transferable CRISPR-Cas system to killing the pathogens (Colavecchio et al., 2017). Bacteriophage infection may either lead to a lytic or lysogenic cycle. These infections may trigger the release of signaling molecules to communicate among the bacterial population, which induces various mechanisms to resensitize the bacterial cell against antibiotics (Fig. 1). Based on the literature available (Chan et al., 2016; Colom et al., 2019) phage-mediated modifications in bacterial cell surface structures are illustrated in Fig. 2. Thus, it is evident from the growing literature that the bacterial defense mechanism is well developed and phage infection may further induce these mechanisms. The mutations and modifications in the bacterial cells may often result in a reduction in virulence and reduced growth rate resensitization toward the antibiotics.
Phage-mediated antibiotic sensitivity; (1) phage attack on bacterial cell, (2) phage-mediated lytic phase and release of signing molecules, (3) PROPHAGE-containing lysogenic phage, which may result in sensitivity toward antibiotics, (4) Modification in bacterial cell membrane/cell wall structures does not allow the antibiotics its degradation, (5) modification in pili structures does not allow the transfer of plasmid, (6) modification in membrane porins hinders the outside transfer of antibiotic through efflux pump, and (7) loss of antibiotic-resistant gene coding plasmid results in the sensitivity against antibiotics
Phage-mediated modifications in bacterial cell surface structures providing phage resistance and sensitivity toward antibiotics: (1) mutation resulting in changes in phage receptor glycoprotein, (2) changes in flagella proteins to modify the phage receptor site (NA: no attachment), (3) conformational changes in receptor protein, (4) modification in glycolipids resulting in phage resistance and sensitivity toward cell membrane degrading antibiotics (ABS), (5) modification in pili structure to block the phage attachment site, which further may prevent the spreading antibiotic resistance through horizontal gene transfer (HGT), and (6) conformational changes in outer membrane proteins (OMP) like porins block the phage attachment, which further hinders the antibiotic efflux
In conjunction with different microbes like bacteria, protozoa, and fungi, bacteriophages are naturally found inside the human stomach, oral and nasal cavity, genital tract, and eye. Most of the bacteriophages that are naturally present in the human body are temperate phages, while many are prophages. Under different conditions, the induction of this prophage may lead to disruption of the equilibrium among the microbiome balance and dysbiosis (imbalance between the species present in our natural microflora) that induce temperate intestinal phage. Recent study has suggested a strategy involving the recombinant polyvalent phages, which may target a wide host range including genetically distinct bacterial species. However, their effect and influence on human gut microflora is yet to be investigated (Gabashvili et al., 2021).
Phage Cocktail and Antibiotic Supplementation
Bacteriophage host co-evolution dynamics have been well proposed to understand the co-existence of phage and bacteria. Phages are extremely specific to their host bacteria, which may specifically target a particular group of bacteria without disturbing other microbes. Although the development of resistance against bacteriophage is quite common, that can be minimized by the use of a phage cocktail. A cocktail containing phage EFDG1 and EFLK1 was highly effective against both planktonic and biofilm cultures of vancomycin-resistant Enterococcus. This study demonstrated the emergence of phage EFDG1-resistant Enterococcus faecalis, which was quickly and successfully handled by isolating a new phage EFLK1 and further formulating a cocktail containing both the phages (Khalifa et al., 2018). Some recent studies have endorsed the application of phage cocktail as already discussed at the relevant places. For the production of phage cocktail, the strains of bacteria may be isolated from patients suffering from septic or intestinal infections, or from the bacteriological diagnostic laboratories. Only virulent phages are isolated, cultured, and produced in bioreactors. The purified bacteriophages are mixed in appropriate combinations to formulate a phage cocktail (Merabishvili et al., 2009).
Besides, research articles, there are some patents and commercial phage formulations available. A patent SalmoFREE® consists of a mixture of six Salmonella lytic bacteriophages that have been successfully used as a potential therapy to control Salmonella infection in poultry products. The study suggested that SalmoFREE® may be an efficient prevention measure to avoid Salmonella--associated food poisoning (Clavijo et al., 2019).
To overcome the issues that arise during phage therapy including lower stability, narrow host spectrum, and deprived pharmacokinetic profiles (restricted movement of phage into the body, the time course of its absorption, and action), different delivery systems for their efficient delivery are being explored. Among different methods, microencapsulation of phages or phage cocktail may efficiently protect phages against adverse gastrointestinal environmental conditions and control their targeted release at the site of infection. Microencapsulation involves the entrapment of phage particles in thin polymer coats. An encapsulated lytic phage cocktail containing MRSA-infecting phages has been developed using nanostructured lipid-based carriers. This encapsulation strategy involved a transfersome-entrapped phage cocktail, which showed good persistence and stability that helped in the recovery from MRSA in vivo in rat models (Chhibber et al., 2017). Several studies have demonstrated formulation of phage-delivering hydrogels in order to deliver a phage to the site of infection. These hydrogels mainly including alginate hydrogels have been used in catheter-associated urinary tract infection, orthopedic implant-associated bone infection, and trauma-associated wound infection (Kim et al., 2021). For various food applications and to control drug-resistant Salmonella contaminations, a formulation containing microencapsulation of phage as a dry powder using whey protein isolate and trehalose was prepared. This microencapsulated phage powder protected the phage particles from the harsh temperature and pH conditions and showed high effectiveness in controlling the S. Enteritidis and S. Typhimurium (Petsong et al., 2020).
Human body is a reservoir of bacteria and bacteriophages (Barr, 2017). During the bacterial infections, an antibiotic dose may be supplemented by bacteriophages to form an axis. In this scenario, bacteriophages may directly kill the bacteria, make them susceptible toward the antibiotics, as well as indirectly support the human body to fight against infections. Hence, there is a three-way pressure on the bacterial cells, this pressure can be balanced by a perfect bacteriophage-antibiotic axis. Thus, phage therapy using a phage cocktail and in combination with antibiotics holds the potential for future clinical applications (Segall et al., 2019). Phage cocktail containing Pseudomonas phages, ϕPA01 and ϕPA02, and antibiotic ciprofloxacin and meropenem successfully suppressed the growth of P. aeruginosa (Ong et al., 2020). A recent case study reported that a patient suffering from a trauma-related left tibial infection caused by multidrug-resistant A. baumannii and Klebsiella pneumoniae was successfully treated with a phage cocktail and antibiotics. The phage cocktail contained a combination of phage ɸAbKT21phi3 and ɸKpKT21phi1 along with meropenem and colistin (Nir-Paz et al., 2019). Another clinical case report of a 10‐year-old cystic fibrosis patient infected with an antibiotic-resistant Achromobacter spp. revealed that a co-administration of cefiderocol, meropenem/vaborbactam, and bacteriophage Ax2CJ45ϕ2 cleared her infection and further restored baseline pulmonary function (Gainey et al., 2020). Thus, the recent studies and clinical trials are more clearly portraying the pictures related to the synergistic use of phage cocktail and antibiotics on planktonic as well as biofilm-associated sessile antibiotic-resistant bacteria (Fig. 3).
Conclusion
Lytic phages are a potential alternative in the treatment of bacterial infections. Similar to antibiotic resistance, phage resistance has also been observed in several bacteria. To address this issue, phage cocktails have been suggested, which consist of two or more types of phages having different target cell-receptors. It was also observed that phage therapy can make resistant bacteria again sensitive toward antibiotics through a number of mechanisms. Thus, besides phage cocktail, a combination of phage along with antibiotic may be a successful strategy. It is important to note that some bacteria have developed resistance toward most of the available antibiotics and there is no clinically certified phage therapy available for these antibiotic-resistant bacteria. Future research may be focused on exploring the phage therapy for such bacterial pathogens.
Data Availability
All data are obtained from publicly available information.
References
Abdel-Haliem, M. E., & Askora, A. (2013). Isolation and characterization of bacteriophages of Helicobacter pylori isolated from Egypt. Future Virology, 8(8), 821–826. https://doi.org/10.2217/fvl.13.58
Al-Zubidi, M., Widziolek, M., Court, E. K., Gains, A. F., Smith, R. E., Ansbro, K., et al. (2019). Identification of novel bacteriophages with therapeutic potential that target Enterococcus faecalis. Infection and Immunity. https://doi.org/10.1128/IAI.00512-19
Amarillas, L., Rubí-Rangel, L., Chaidez, C., González-Robles, A., Lightbourn-Rojas, L., & León-Félix, J. (2017). Isolation and characterization of phiLLS, a novel phage with potential biocontrol agent against multidrug-resistant Escherichia coli. Frontiers in Microbiology. https://doi.org/10.3389/fmicb.2017.01355
Aslam, S., Courtwright, A. M., Koval, C., Lehman, S. M., Morales, S., Furr, C. L. L., et al. (2019). Early clinical experience of bacteriophage therapy in 3 lung transplant recipients. American Journal of Transplantation, 19(9), 2631–2639.
Azam, A. H., & Tanji, Y. (2019). Bacteriophage-host arm race: An update on the mechanism of phage resistance in bacteria and revenge of the phage with the perspective for phage therapy. Applied Microbiology and Biotechnology, 103(5), 2121–2131. https://doi.org/10.1007/s00253-019-09629-x
Banin, E., Hughes, D., & Kuipers, O. P. (2017). Editorial: Bacterial pathogens, antibiotics and antibiotic resistance. FEMS Microbiology Reviews, 41(3), 450–452. https://doi.org/10.1093/femsre/fux016
Bao, H., Zhou, Y., Shahin, K., Zhang, H., Cao, F., Pang, M., et al. (2020a). The complete genome of lytic Salmonella phage vB_SenM-PA13076 and therapeutic potency in the treatment of lethal Salmonella Enteritidis infections in mice. Microbiological Research. https://doi.org/10.1016/j.micres.2020.126471
Bao, J., Wu, N., Zeng, Y., Chen, L., Li, L., Yang, L., et al. (2020b). Non-active antibiotic and bacteriophage synergism to successfully treat recurrent urinary tract infection caused by extensively drug-resistant Klebsiella pneumoniae. Emerging Microbes & Infections, 9(1), 771–774. https://doi.org/10.1080/22221751.2020.1747950
Barr, J. J. (2017). A bacteriophages journey through the human body. Immunological Reviews, 279(1), 106–122. https://doi.org/10.1111/imr.12565
Bodner, K., Melkonian, A. L., & Covert, M. W. (2020). The enemy of my enemy: New insights regarding bacteriophage-mammalian cell interactions. Trends in Microbiology. https://doi.org/10.1016/j.tim.2020.10.014
Canfield, G. S., Chatterjee, A., Espinosa, J., Mangalea, M. R., Sheriff, E. K., Keidan, M., et al. (2021). Lytic bacteriophages facilitate antibiotic sensitization of Enterococcus faecium. Antimicrobial Agents and Chemotherapy. https://doi.org/10.1128/AAC.00143-21
Carrigy, N. B., Liang, L., Wang, H., Kariuki, S., Nagel, T. E., Connerton, I. F., & Vehring, R. (2019). Spray-dried anti-Campylobacter bacteriophage CP30A powder suitable for global distribution without cold chain infrastructure. International Journal of Pharmaceutics, 569, 118601. https://doi.org/10.1016/j.ijpharm.2019.118601
Chan, B. K., Sistrom, M., Wertz, J. E., Kortright, K. E., Narayan, D., & Turner, P. E. (2016). Phage selection restores antibiotic sensitivity in MDR Pseudomonas aeruginosa. Scientific Reports, 6(1), 26717. https://doi.org/10.1038/srep26717
Chan, B. K., Turner, P. E., Kim, S., Mojibian, H. R., Elefteriades, J. A., & Narayan, D. (2018). Phage treatment of an aortic graft infected with Pseudomonas aeruginosa. Evolution, Medicine, and Public Health, 2018(1), 60–66. https://doi.org/10.1093/emph/eoy005
Cheng, M., Liang, J., Zhang, Y., Hu, L., Gong, P., Cai, R., et al. (2017a). The bacteriophage EF-P29 efficiently protects against lethal vancomycin-resistant Enterococcus faecalis and alleviates gut microbiota imbalance in a murine bacteremia model. Frontiers in Microbiology. https://doi.org/10.3389/fmicb.2017.00837
Cheng, M., Zhang, Y., Li, X., Liang, J., Hu, L., Gong, P., et al. (2017b). Endolysin LysEF-P10 shows potential as an alternative treatment strategy for multidrug-resistant Enterococcus faecalis infections. Scientific Reports, 7(1), 10164. https://doi.org/10.1038/s41598-017-10755-7
Chhibber, S., Shukla, A., & Kaur, S. (2017). Transfersomal phage cocktail is an effective treatment against methicillin-resistant Staphylococcus aureus-mediated skin and soft tissue infections. Antimicrobial Agents and Chemotherapy. https://doi.org/10.1128/AAC.02146-16
Cieślik, M., Bagińska, N., Górski, A., & Jończyk-Matysiak, E. (2021). Animal models in the evaluation of the effectiveness of phage therapy for infections caused by Gram-negative bacteria from the ESKAPE group and the reliability of its use in humans. Microorganisms, 9(2), 206. https://doi.org/10.3390/microorganisms9020206
Clavijo, V., Baquero, D., Hernandez, S., Farfan, J. C., Arias, J., Arévalo, A., et al. (2019). Phage cocktail SalmoFREE® reduces Salmonella on a commercial broiler farm. Poultry Science, 98(10), 5054–5063. https://doi.org/10.3382/ps/pez251
Colavecchio, A., Cadieux, B., Lo, A., & Goodridge, L. D. (2017). Bacteriophages contribute to the spread of antibiotic resistance genes among foodborne pathogens of the enterobacteriaceae family—A review. Frontiers in Microbiology. https://doi.org/10.3389/fmicb.2017.01108
Colom, J., Batista, D., Baig, A., Tang, Y., Liu, S., Yuan, F., et al. (2019). Sex pilus specific bacteriophage to drive bacterial population towards antibiotic sensitivity. Scientific Reports, 9(1), 12616. https://doi.org/10.1038/s41598-019-48483-9
Corbellino, M., Kieffer, N., Kutateladze, M., Balarjishvili, N., Leshkasheli, L., Askilashvili, L., et al. (2020). Eradication of a multidrug-resistant, carbapenemase-producing klebsiella pneumoniae isolate following oral and intra-rectal therapy with a custom made lytic bacteriophage preparation. Clinical Infectious Diseases, 70(9), 1998–2001. https://doi.org/10.1093/cid/ciz782
Easwaran, M., De Zoysa, M., & Shin, H. (2020). Application of phage therapy: Synergistic effect of phage EcSw (ΦEcSw) and antibiotic combination towards antibiotic-resistant Escherichia coli. Transboundary and Emerging Diseases, 67(6), 2809–2817. https://doi.org/10.1111/tbed.13646
El-Shibiny, A., Scott, A., Timms, A., Metawea, Y., Connerton, P., & Connerton, I. (2009). Application of a group II campylobacter bacteriophage to reduce strains of Campylobacter jejuni and Campylobacter coli colonizing broiler chickens. Journal of Food Protection, 72(4), 733–740. https://doi.org/10.4315/0362-028X-72.4.733
El Haddad, L., Harb, C. P., Gebara, M. A., Stibich, M. A., & Chemaly, R. F. (2019). A Systematic and critical review of bacteriophage therapy against multidrug-resistant ESKAPE organisms in humans. Clinical Infectious Diseases, 69(1), 167–178. https://doi.org/10.1093/cid/ciy947
Fish, R., Kutter, E., Wheat, G., Blasdel, B., Kutateladze, M., & Kuhl, S. (2018). Compassionate use of bacteriophage therapy for foot ulcer treatment as an effective step for moving toward clinical trials. Methods in Molecular Biology, 1693, 159–170. https://doi.org/10.1007/978-1-4939-7395-8_14
Gabashvili, E., Kobakhidze, S., Koulouris, S., Robinson, T., & Kotetishvili, M. (2021). Bi- and multi-directional gene transfer in the natural populations of polyvalent bacteriophages, and their host species spectrum representing foodborne versus other human and/or animal pathogens. Food and Environmental Virology. https://doi.org/10.1007/s12560-021-09460-6
Gainey, A. B., Burch, A., Brownstein, M. J., Brown, D. E., Fackler, J., Horne, B., et al. (2020). Combining bacteriophages with cefiderocol and meropenem/vaborbactam to treat a pan-drug resistant Achromobacter species infection in a pediatric cystic fibrosis patient. Pediatric Pulmonology, 55(11), 2990–2994. https://doi.org/10.1002/ppul.24945
Grygorcewicz, B., Wojciuk, B., Roszak, M., Łubowska, N., Blstrokaejczak, P., Jursa-Kulesza, J., et al. (2021). Environmental phage-based cocktail and antibiotic combination effects on Acinetobacter baumannii biofilm in a human urine model. Microbial Drug Resistance, 27(1), 25–35. https://doi.org/10.1089/mdr.2020.0083
Hankin, E. H. (1896). L’action bactericide des eaux de la Jumna et du Gange sur le vibrion du cholera. In Annales de l’Institut Pasteur (Vol. t. 10, p. 790). http://www.biodiversitylibrary.org/item/22126
Hua, Y., Luo, T., Yang, Y., Dong, D., Wang, R., Wang, Y., et al. (2018). Phage therapy as a promising new treatment for lung infection caused by carbapenem-resistant Acinetobacter baumannii in mice. Frontiers in Microbiology. https://doi.org/10.3389/fmicb.2017.02659
Huang, C., Virk, S. M., Shi, J., Zhou, Y., Willias, S. P., Morsy, M. K., et al. (2018). Isolation, characterization, and application of bacteriophage LPSE1 against Salmonella enterica in ready to eat (RTE) Foods. Frontiers in Microbiology. https://doi.org/10.3389/fmicb.2018.01046
Iwano, H., Inoue, Y., Takasago, T., Kobayashi, H., Furusawa, T., Taniguchi, K., et al. (2018). Bacteriophage ΦSA012 has a broad host range against Staphylococcus aureus and effective lytic capacity in a mouse mastitis model. Biology, 7(1), 8. https://doi.org/10.3390/biology7010008
Jamal, M., Andleeb, S., Jalil, F., Imran, M., Nawaz, M. A., Hussain, T., et al. (2019). Isolation, characterization and efficacy of phage MJ2 against biofilm forming multi-drug resistant Enterobacter cloacae. Folia Microbiologica, 64(1), 101–111. https://doi.org/10.1007/s12223-018-0636-x
Jansen, M., Wahida, A., Latz, S., Krüttgen, A., Häfner, H., Buhl, E. M., et al. (2018). Enhanced antibacterial effect of the novel T4-like bacteriophage KARL-1 in combination with antibiotics against multi-drug resistant Acinetobacter baumannii. Scientific Reports, 8(1), 14140. https://doi.org/10.1038/s41598-018-32344-y
Jault, P., Leclerc, T., Jennes, S., Pirnay, J. P., Que, Y. A., Resch, G., et al. (2019). Efficacy and tolerability of a cocktail of bacteriophages to treat burn wounds infected by Pseudomonas aeruginosa (PhagoBurn): A randomised, controlled, double-blind phase 1/2 trial. The Lancet Infectious Diseases, 19(1), 35–45. https://doi.org/10.1016/S1473-3099(18)30482-1
Jeon, J., Park, J.-H., & Yong, D. (2019). Efficacy of bacteriophage treatment against carbapenem-resistant Acinetobacter baumannii in Galleria mellonella larvae and a mouse model of acute pneumonia. BMC Microbiology, 19(1), 70. https://doi.org/10.1186/s12866-019-1443-5
Kabwe, M., Meehan-Andrews, T., Ku, H., Petrovski, S., Batinovic, S., Chan, H. T., & Tucci, J. (2021). Lytic bacteriophage EFA1 Modulates HCT116 colon cancer cell growth and upregulates ROS production in an Enterococcus faecalis co-culture system. Frontiers in Microbiology. https://doi.org/10.3389/fmicb.2021.650849
Kakabadze, E., Makalatia, K., Grdzelishvili, N., Bakuradze, N., Goderdzishvili, M., Kusradze, I., et al. (2018). Selection of potential therapeutic bacteriophages that lyse a CTX-M-15 extended spectrum β-lactamase producing Salmonella enterica Serovar Typhi Strain from the Democratic Republic of the Congo. Viruses, 10(4), 172. https://doi.org/10.3390/v10040172
Kebriaei, R., Lev, K., Morrisette, T., Stamper, K. C., Abdul-Mutakabbir, J. C., Lehman, S. M., et al. (2020). Bacteriophage-antibiotic combination strategy: An alternative against methicillin-resistant phenotypes of Staphylococcus aureus. Antimicrobial Agents and Chemotherapy. https://doi.org/10.1128/AAC.00461-20
Khalifa, L., Gelman, D., Shlezinger, M., Dessal, A. L., Coppenhagen-Glazer, S., Beyth, N., & Hazan, R. (2018). Defeating antibiotic- and phage-resistant Enterococcus faecalis using a phage cocktail in vitro and in a clot model. Frontiers in Microbiology. https://doi.org/10.3389/fmicb.2018.00326
Kim, H. Y., Chang, R. Y. K., Morales, S., & Chan, H.-K. (2021). Bacteriophage-delivering hydrogels: Current progress in combating antibiotic resistant bacterial infection. Antibiotics, 10(2), 130. https://doi.org/10.3390/antibiotics10020130
Kim, M., Jo, Y., Hwang, Y. J., Hong, H. W., Hong, S. S., Park, K., & Myung, H. (2018). Phage-antibiotic synergy via delayed lysis. Applied and Environmental Microbiology. https://doi.org/10.1128/AEM.02085-18
Kwiatek, M., Parasion, S., Rutyna, P., Mizak, L., Gryko, R., Niemcewicz, M., et al. (2017). Isolation of bacteriophages and their application to control Pseudomonas aeruginosa in planktonic and biofilm models. Research in Microbiology, 168(3), 194–207. https://doi.org/10.1016/j.resmic.2016.10.009
Labrie, S. J., Samson, J. E., & Moineau, S. (2010). Bacteriophage resistance mechanisms. Nature Reviews Microbiology, 8(5), 317–327. https://doi.org/10.1038/nrmicro2315
Latz, S., Krüttgen, A., Häfner, H., Buhl, E., Ritter, K., & Horz, H.-P. (2017). Differential effect of newly isolated phages belonging to PB1-like, phiKZ-like and LUZ24-like viruses against multi-drug resistant Pseudomonas aeruginosa under varying growth conditions. Viruses, 9(11), 315. https://doi.org/10.3390/v9110315
Leitner, L., Sybesma, W., Chanishvili, N., Goderdzishvili, M., Chkhotua, A., Ujmajuridze, A., et al. (2017). Bacteriophages for treating urinary tract infections in patients undergoing transurethral resection of the prostate: A randomized, placebo-controlled, double-blind clinical trial. BMC Urology. https://doi.org/10.1186/s12894-017-0283-6
Leitner, L., Ujmajuridze, A., Chanishvili, N., Goderdzishvili, M., Chkonia, I., Rigvava, S., et al. (2021). Intravesical bacteriophages for treating urinary tract infections in patients undergoing transurethral resection of the prostate: A randomised, placebo-controlled, double-blind clinical trial. The Lancet Infectious Diseases, 21(3), 427–436. https://doi.org/10.1016/S1473-3099(20)30330-3
Li, M., Lin, H., Jing, Y., & Wang, J. (2020a). Broad-host-range Salmonella bacteriophage STP4-a and its potential application evaluation in poultry industry. Poultry Science, 99(7), 3643–3654. https://doi.org/10.1016/j.psj.2020.03.051
Li, M., Guo, M., Chen, L., Zhu, C., Xiao, Y., Li, P., et al. (2020b). Isolation and characterization of novel lytic bacteriophages infecting epidemic carbapenem-resistant Klebsiella pneumoniae strains. Frontiers in Microbiology. https://doi.org/10.3389/fmicb.2020.01554
Ma, Y., Wang, C., Li, Y., Li, J., Wan, Q., Chen, J., et al. (2020). Considerations and caveats in combating ESKAPE pathogens against nosocomial infections. Advanced Science, 7(1), 1901872. https://doi.org/10.1002/advs.201901872
Mangalea, M. R., & Duerkop, B. A. (2020). Fitness trade-offs resulting from bacteriophage resistance potentiate synergistic antibacterial strategies. Infection and Immunity. https://doi.org/10.1128/IAI.00926-19
Manohar, P., Tamhankar, A. J., Lundborg, C. S., & Nachimuthu, R. (2019). Therapeutic characterization and efficacy of bacteriophage cocktails infecting Escherichia coli, Klebsiella pneumoniae, and Enterobacter species. Frontiers in Microbiology. https://doi.org/10.3389/fmicb.2019.00574
McCallin, S., Alam Sarker, S., Barretto, C., Sultana, S., Berger, B., Huq, S., et al. (2013). Safety analysis of a Russian phage cocktail: From MetaGenomic analysis to oral application in healthy human subjects. Virology, 443(2), 187–196. https://doi.org/10.1016/j.virol.2013.05.022
Merabishvili, M., Pirnay, J.-P., Verbeken, G., Chanishvili, N., Tediashvili, M., Lashkhi, N., et al. (2009). Quality-controlled small-scale production of a well-defined bacteriophage cocktail for use in human clinical trials. PLoS ONE, 4(3), e4944. https://doi.org/10.1371/journal.pone.0004944
Mishra, R. R., & Nath, G. (2020). Detection Of bacteriophages against Eskape group of nosocomial pathogens from Ganga River water during community bath at various rituals: Since 2013–2019. Journal of Applied Pharmaceutical Sciences and Research., 5, 7.
Nafarrate, I., Mateo, E., Amárita, F., de Marañón, I. M., & Lasagabaster, A. (2020). Efficient isolation of Campylobacter bacteriophages from chicken skin, analysis of several isolation protocols. Food Microbiology, 90, 103486. https://doi.org/10.1016/j.fm.2020.103486
Nasser, A., Azizian, R., Tabasi, M., Khezerloo, J. K., Heravi, F. S., Kalani, M. T., et al. (2019). Specification of bacteriophage isolated against clinical methicillin-resistant Staphylococcus Aureus. Osong Public Health and Research Perspectives, 10(1), 20–24. https://doi.org/10.24171/j.phrp.2019.10.1.05
Nir-Paz, R., Gelman, D., Khouri, A., Sisson, B. M., Fackler, J., Alkalay-Oren, S., et al. (2019). Successful treatment of antibiotic-resistant, poly-microbial bone infection with bacteriophages and antibiotics combination. Clinical Infectious Diseases, 69(11), 2015–2018. https://doi.org/10.1093/cid/ciz222
Nobrega, F. L., Vlot, M., de Jonge, P. A., Dreesens, L. L., Beaumont, H. J. E., Lavigne, R., et al. (2018). Targeting mechanisms of tailed bacteriophages. Nature Reviews Microbiology, 16(12), 760–773. https://doi.org/10.1038/s41579-018-0070-8
Oechslin, F. (2018). Resistance development to bacteriophages occurring during bacteriophage therapy. Viruses, 10(7), 351. https://doi.org/10.3390/v10070351
Oh, H. K., Jo, J. H., Hwang, Y. J., & Myung, H. (2020). Complete genome sequence of a novel bacteriophage, ATCEA85, infecting Enterobacter aerogenes. Archives of Virology, 165(10), 2397–2400. https://doi.org/10.1007/s00705-020-04751-y
Ong, S. P., Azam, A. H., Sasahara, T., Miyanaga, K., & Tanji, Y. (2020). Characterization of Pseudomonas lytic phages and their application as a cocktail with antibiotics in controlling Pseudomonas aeruginosa. Journal of Bioscience and Bioengineering, 129(6), 693–699. https://doi.org/10.1016/j.jbiosc.2020.02.001
Onsea, J., Soentjens, P., Djebara, S., Merabishvili, M., Depypere, M., Spriet, I., et al. (2019). Bacteriophage application for difficult-to-treat musculoskeletal infections: Development of a standardized multidisciplinary treatment protocol. Viruses. https://doi.org/10.3390/v11100891
Patil, A., Banerji, R., Kanojiya, P., Koratkar, S., & Saroj, S. (2021). Bacteriophages for ESKAPE: Role in pathogenicity and measures of control. Expert Review of Anti-Infective Therapy. https://doi.org/10.1080/14787210.2021.1858800
Peng, C., Hanawa, T., Azam, A. H., LeBlanc, C., Ung, P., Matsuda, T., et al. (2019). Silviavirus phage ɸMR003 displays a broad host range against methicillin-resistant Staphylococcus aureus of human origin. Applied Microbiology and Biotechnology, 103(18), 7751–7765. https://doi.org/10.1007/s00253-019-10039-2
Petrovic Fabijan, A., Lin, R. C. Y., Ho, J., Maddocks, S., Ben Zakour, N. L., Iredell, J. R., et al. (2020). Safety of bacteriophage therapy in severe Staphylococcus aureus infection. Nature Microbiology, 5(3), 465–472. https://doi.org/10.1038/s41564-019-0634-z
Petsong, K., Benjakul, S., & Vongkamjan, K. (2020). Optimization of wall material for phage encapsulation via freeze-drying and antimicrobial efficacy of microencapsulated phage against Salmonella. Journal of Food Science and Technology. https://doi.org/10.1007/s13197-020-04705-x
Rahmat Ullah, S., Andleeb, S., Raza, T., Jamal, M., & Mehmood, K. (2017). Effectiveness of a lytic phage SRG1 against vancomycin-resistant Enterococcus faecalis in compost and soil. BioMed Research International, 2017, 1–8. https://doi.org/10.1155/2017/9351017
Segall, A. M., Roach, D. R., & Strathdee, S. A. (2019). Stronger together? Perspectives on phage-antibiotic synergy in clinical applications of phage therapy. Current Opinion in Microbiology, 51, 46–50. https://doi.org/10.1016/j.mib.2019.03.005
Shahin, K., & Bouzari, M. (2018). Bacteriophage application for biocontrolling Shigella flexneri in contaminated foods. Journal of Food Science and Technology, 55(2), 550–559. https://doi.org/10.1007/s13197-017-2964-2
Suay-García, B., & Pérez-Gracia, M. T. (2017). Drug-resistant Neisseria gonorrhoeae: Latest developments. European Journal of Clinical Microbiology & Infectious Diseases, 36(7), 1065–1071. https://doi.org/10.1007/s10096-017-2931-x
Sulakvelidze, A., Alavidze, Z., & Morris, J. G. (2001). Bacteriophage therapy. Antimicrobial Agents and Chemotherapy, 45(3), 649–659. https://doi.org/10.1128/AAC.45.3.649-659.2001
Tabassum, R., Shafique, M., Khawaja, K. A., Alvi, I. A., Rehman, Y., Sheik, C. S., et al. (2018). Complete genome analysis of a Siphoviridae phage TSK1 showing biofilm removal potential against Klebsiella pneumoniae. Scientific Reports, 8(1), 17904. https://doi.org/10.1038/s41598-018-36229-y
Tacconelli, E., Carrara, E., Savoldi, A., Harbarth, S., Mendelson, M., Monnet, D. L., et al. (2018). Discovery, research, and development of new antibiotics: The WHO priority list of antibiotic-resistant bacteria and tuberculosis. The Lancet Infectious Diseases, 18(3), 318–327. https://doi.org/10.1016/S1473-3099(17)30753-3
Taha, O. A., Connerton, P. L., Connerton, I. F., & El-Shibiny, A. (2018). Bacteriophage ZCKP1: A potential treatment for Klebsiella pneumoniae isolated from diabetic foot patients. Frontiers in Microbiology. https://doi.org/10.3389/fmicb.2018.02127
Tkhilaishvili, T., Wang, L., Tavanti, A., Trampuz, A., & Di Luca, M. (2020). Antibacterial efficacy of two commercially available bacteriophage formulations, staphylococcal bacteriophage and PYO bacteriophage, against methicillin-resistant Staphylococcus aureus: Prevention and eradication of biofilm formation and control of a syst. Frontiers in Microbiology. https://doi.org/10.3389/fmicb.2020.00110
Vasilyev, A. O., Sazonova, N. A., Melnikov, V. D., Gabdullin, A. F., Zaitsev, A. V., Shiryaev, A. A., et al. (2020). The experience of using a bacteriophages-based complex antibacterial and analgesic drug in gel formulation in women who underwent various instrumental and diagnostic and treatment interventions. Gynecology, 22(3), 42–48. https://doi.org/10.26442/20795696.2020.3.200199
Vukotic, G., Obradovic, M., Novovic, K., Di Luca, M., Jovcic, B., Fira, D., et al. (2020). Characterization, antibiofilm, and depolymerizing activity of two phages active on carbapenem-resistant Acinetobacter baumannii. Frontiers in Medicine. https://doi.org/10.3389/fmed.2020.00426
Wang, L., Tkhilaishvili, T., Bernal Andres, B., Trampuz, A., & Gonzalez Moreno, M. (2020). Bacteriophage–antibiotic combinations against ciprofloxacin/ceftriaxone-resistant Escherichia coli in vitro and in an experimental Galleria mellonella model. International Journal of Antimicrobial Agents, 56(6), 106200. https://doi.org/10.1016/j.ijantimicag.2020.106200
Wang, Z., Zheng, P., Ji, W., Fu, Q., Wang, H., Yan, Y., & Sun, J. (2016). SLPW: A virulent bacteriophage targeting methicillin-resistant Staphylococcus aureus in vitro and in vivo. Frontiers in Microbiology. https://doi.org/10.3389/fmicb.2016.00934
Wilson, D. N., Hauryliuk, V., Atkinson, G. C., & O’Neill, A. J. (2020). Target protection as a key antibiotic resistance mechanism. Nature Reviews Microbiology, 18(11), 637–648. https://doi.org/10.1038/s41579-020-0386-z
Yelin, I., & Kishony, R. (2018). Antibiotic resistance. Cell, 172(5), 1136-1136.e1. https://doi.org/10.1016/j.cell.2018.02.018
Yen, M., Cairns, L. S., & Camilli, A. (2017). A cocktail of three virulent bacteriophages prevents Vibrio cholerae infection in animal models. Nature Communications, 8(1), 14187. https://doi.org/10.1038/ncomms14187
Zhao, J., Zhang, Z., Tian, C., Chen, X., Hu, L., Wei, X., et al. (2019). Characterizing the biology of lytic bacteriophage vB_EaeM_φEap-3 infecting multidrug-resistant Enterobacter aerogenes. Frontiers in Microbiology. https://doi.org/10.3389/fmicb.2019.00420
Zhou, W., Feng, Y., & Zong, Z. (2018). Two new lytic bacteriophages of the myoviridae family against carbapenem-resistant Acinetobacter baumannii. Frontiers in Microbiology. https://doi.org/10.3389/fmicb.2018.00850
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kaur, G., Agarwal, R. & Sharma, R.K. Bacteriophage Therapy for Critical and High-Priority Antibiotic-Resistant Bacteria and Phage Cocktail-Antibiotic Formulation Perspective. Food Environ Virol 13, 433–446 (2021). https://doi.org/10.1007/s12560-021-09483-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12560-021-09483-z