Abstract
To our knowledge, no published research has developed an individual difference measure of health-related stereotype threat (HRST). We adapted existing measures of academic stereotype threat to the health domain on a sample of black college students (N = 280). The resulting health-related stereotype threat scale-24 (HRST-24) was assessed for internal consistency, construct and incremental validity, and whether it explains variance in self-reported delays among four preventive health behaviors—blood pressure and cholesterol assays, physical exams, and routine checkups. After adjusting for several control variables, the HRST-24’s (full scale α = 0.96) perceived black health inferiority (18 items; α = 0.96) and perceived physician racial bias (6 items; α = 0.85) subscales explained unique variance in delays among two of the four behaviors including a blood cholesterol check (p < .01) and routine checkup—albeit at marginal levels (p = .063) in the case of the latter. Overall, these data provide preliminary evidence of construct and incremental validity for the HRST-24 among blacks. Recommendations for administering the scale are provided and future directions for HRST research are discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
I think it was very disrespectful. As a matter of fact, I think [the doctor] was looking down on me… She just decided that, this guy was a minority [and] we’re going to do whatever we feel like doing without consulting you…. She just felt like minorities are all the same—they don’t know anything, they’re not intelligent, they’re not educated.
—Reactions from John Reid, a black diabetic who presented to the Emergency Department with a toe infection and was advised to undergo an amputation when less invasive alternatives existed (as cited in Cohen, 2009; first brackets added).
Introduction
Anecdotes like this one reflect persistent stereotypes associated with blacks and offer insight into the perceptions of blacks toward those in medicine. Indeed, the beliefs and attitudes of blacks toward the US healthcare system are well documented. For instance, when compared to whites, blacks are less satisfied with the quality of medical care they receive (Johnson et al. 2004; LaVeist et al. 2000; Lillie-Blanton et al. 2000), more distrustful of the healthcare system and its elements (e.g., physicians; Boulware et al. 2003; LaVeist et al. 2000), and more concerned about the integrity of their personal information (Boulware et al. 2003). In addition, when compared to other minorities, blacks generally indicate more exposure to racism, which has been linked to poorer mental health among this demographic (Pieterse et al. 2012).
These perceptual differences may be rooted in a host of mechanisms including socioeconomic status, educational disparities, a history of medical maltreatment, and cultural mistrust (Corbie-Smith et al. 1999; Gamble 1993; Smedley 2011; Terrell and Terrell 1981). Moreover, these negative perceptions can have a profound impact on the development of cultural stereotypes as they pertain to and are held by blacks. Such experiences may affect the willingness of blacks to interact with components of the healthcare system (e.g., hospitals) and, consequently, have implications for racial health disparities.
Racial Health Disparities
Racial health disparities have been examined for more than a century (DuBois 1906; Gamble 2011), and mortality and morbidity differences between blacks and whites are well established (Arias 2006; Aronson 2011; Calman 2007; Macinko and Elo 2009; Sawyer et al. 2012; Shavers et al. 2012; Smith et al. 2007). For instance, the life expectancy gap between blacks and whites remains sizeable (Harper et al. 2007). Mortality and morbidity rate discrepancies between blacks and whites are often attributed to blacks’ reluctance, compared to whites, to participate in early detection and treatment efforts. For example, some medical practitioners believe that men, particularly black males, may not want to visit their doctors or partake in preventive screenings because they simply, “… don’t want to think that there’s anything wrong with them” (McGairk 2008, p. 14). It is likely, however, that the motives behind these behaviors are more complex.
Identifying the mechanisms that contribute to such behaviors among blacks has long been a goal of empirical studies conducted by those in public health and healthcare. Considerable research has focused on factors within and outside of the healthcare system (Smedley 2012; Smedley et al. 2003, 2007). The impact of psychosocial factors, however, has been relatively underappreciated as a determinant of black-white health inequities. Moreover, although some researchers suggest that racial disparities can be minimized through public policy (Macinko and Elo 2009), the present study posits that stereotype threat, which is a psychosocial phenomenon whereby stigmatized individuals (e.g., blacks) face added pressure when they are at risk of confirming negative, group-based stereotypes (Steele 1997, 2010; Steele and Davies 2003; Nguyen and Ryan 2008), could play an important role in this process. Stereotype threat may contribute to and help explain the health outcomes of blacks. In addition, stereotype threat theory (Steele 2001, 2010; Steele and Davies 2003) can be used as a conceptual framework in understanding racial mortality and morbidity gaps (Aronson 2011).
A Primer on Stereotype Threat
In short, stereotype threat is a disruptive “situational predicament” (Steele and Aronson 1998) that can be triggered when an individual is susceptible to validating a demeaning stereotype linked to his or her social group (e.g., race; Aronson et al. 2013; Steele and Aronson 1995, 1998). Everyone is vulnerable to threat if they are associated with a group connected to a negative stereotype, and neither belief in nor endorsement of the stereotype is necessary for this phenomenon to occur (Steele and Aronson 1995, 1998). Stereotype threat theory (Steele 2001, 2010) also posits that the likelihood of threat effects (e.g., poor performance) is greatest among those with considerable investment in the domain linked to the stereotype (e.g., academics; Steele and Aronson 1998). Although studies have shown that stereotype threat generalizes across activities (e.g., verbal, sports; Steele and Aronson 1995; Stone et al. 1999) and social groups (e.g., women, elderly; Davis and Simmons 2009; Levy 1996; Nguyen and Ryan 2008), Steele and Aronson’s (1995) seminal studies have received considerable media and scholarly attention (e.g., Chandler et al. 1999; Sackett et al. 2004; Steele and Aronson 1998, 2004).
In their classic experiment, Steele and Aronson (1995, Study 1) examined whether black and white Stanford undergraduates would perform differently on a demanding verbal exam described in one of three ways: (1) diagnostic of verbal ability (high threat), (2) nondiagnostic of ability (low threat), or (3) nondiagnostic, but mentally challenging (low threat + challenge). After controlling for prior SAT scores, these researchers found that, compared to whites, blacks’ performance was significantly impaired when the test was described as diagnostic. These differences disappeared when blacks and whites were told that the test was nondiagnostic. Blacks in the diagnostic condition also underperformed relative to their black counterparts in the nondiagnostic conditions.Footnote 1
Subsequent experiments have replicated this basic effect with different manipulations (e.g., asking participants to indicate their race before an exam; Steele and Aronson 1995, Study 4) and measures (e.g., assessing preference for stereotypical activities, such as listening to rap music; Steele and Aronson 1995, Study 3). The striking feature of these studies was that simple experimental manipulations of threat could affect the performance and self-reports of black students. But is stereotype threat merely a contextually based phenomenon?
Blacks and Dispositional Stereotype Threat
Anecdotal and empirical evidence from the academic domain has indicated that threat has situational (Steele and Aronson 1995; McKay 1999; McKay et al. 2002, 2003) and dispositional components (Steele 1997, 2010; Ziegert et al. 2002) among blacks. Steele and Aronson (1995), for example, found that situational threat produced higher scores on a self-report measure of perceived threat among blacks versus whites. Steele (2010) also used terms such as balloon, cloud, and stereotype in the air (pp. 5 and 7) to describe blacks’ recurring experience of this phenomenon.
Social scientists have also examined, with varying levels of success, the extent to which individual differences in this phenomenon exist more generally (Chatman 1999; Pseekos et al. 2008; Steele et al. 2002; Ziegert et al. 2002). For instance, using a reliable variant of Spencer’s (1993) stereotype vulnerability scale, Steele et al. (2002) found that women in male-dominated disciplines reported higher levels of threat when compared to women in female-dominated disciplines and men across disciplines.Footnote 2 Other researchers, however, have had difficulty in obtaining sufficient internal consistency (i.e., α > 0.7; George and Mallery 1999) when using such instruments (e.g., Chatman 1999; Spencer 1993, as cited in Barnard et al. 2008; Steele et al. 2002). Despite the limited number of studies probing dispositional threat, it seems that this form of vulnerability exists in academic contexts.
Stereotype Threat and Health
An emerging line of research is investigating ways in which stereotype threat may affect the health outcomes of stigmatized groups (Inzlicht and Kang 2010; Kit et al. 2008; Seacat and Mickelson 2009), contribute to racial health disparities (Aronson 2011; Aronson et al. 2013; Burgess et al. 2010), and influence the training and medical achievement of minorities (Aronson 2011; Burgess et al. 2010; Woolf et al. 2008). For instance, regarding physical and mental health, Seacat and Mickelson (2009) found that clinically overweight women presented with material designed to activate obesity-related threat reported reduced exercise and dietary intentions relative to their nonthreatened, overweight counterparts. Further, Henry et al. (2010) observed that schizophrenic patients who were told that two confederates were aware of their clinical diagnosis before conversing with them (threat condition) received less favorable social skill evaluations from the dyad (e.g., poorer ratings of their ability to change topics) than did patients told that these confederates had no knowledge of their disorder (control condition). Relative to public health, Yeung and von Hippel (2008) found that, in a driving simulator, women under threat of confirming the stereotype that women are bad drivers ran over jaywalkers at a higher rate than nonthreatened women. Comparable effects (i.e., increased driving errors) have also been found in a simulation exercise among older drivers contending with the social consensus that their age group poses a danger to motorists, when compared to their age-related counterparts for whom this stereotype was not activated (Joanisse et al. 2013).
Limitations of Existing Health-Related Stereotype Threat Research
There are currently more questions than answers regarding the implications of stereotype threat for racial disparities. The few published studies devoted to understanding the health-related parameters of threat are largely narrative (Burgess et al. 2010; Kit et al. 2008) or qualitative (Woolf et al. 2008), or they examine the behaviors of individuals classified with specific health conditions (e.g., schizophrenics; Henry et al. 2010) after receiving a threat manipulation. Even threat research that incorporates health-related variables into its methods often assesses academic performance as the dependent variable of interest as opposed to a clear health criterion (Blascovich et al. 2001). Furthermore, the scant studies on health-related stereotype threat (HRST), instead of being race focused, are concentrated on other forms of stigma (e.g., obesity; Seacat and Mickelson 2009). Therefore, the effect of racial stereotypes on the health behavior of blacks remains unclear.
Finally, few studies have provided confirmatory data to support the hypothesis that blacks are both chronically and contextually aware of the black health inferiority stereotype (i.e., the belief that blacks are less healthy than whites). Similar to other prominent social stereotypes (e.g., “women are bad at math”), the black health inferiority stereotype is likely anchored in blacks’ efforts to comprehend and adjust to their environment (Mackie et al. 1996; Oskamp and Schultz 2005). Moreover, this belief may be formed and reinforced by communications within- and between groups (e.g., parental instruction), incidental learning, and personal experiences, among other factors (Mackie et al. 1996; Oskamp and Schultz 2005). Coping with the content of this stereotype, however, may adversely affect the health outcomes (Blascovich et al. 2001) and psychological well-being of blacks (Steele 2010).
Demonstration of black health inferiority stereotype awareness is important for theoretical and methodological reasons. Relative to theory, establishing such awareness is one of the minimal conditions necessary to evoke threat (Pseekos et al. 2008; Steele 2010). Methodologically, its confirmation lends credence to the causal chain whereby awareness, followed by placement in a context where stereotype confirmation is possible, can produce threat effects (Pseekos et al. 2008; Steele 2010; Steele and Aronson 1995).
Goals of the Present Research
Our objective was to add to the small but growing body of research on HRST (Aronson 2011; Burgess et al. 2010). We examined the role HRST plays in discouraging blacks from seeking preventive health services (i.e., screenings and exams) in a timely manner. For instance, blacks may be reluctant to schedule and receive preventive tests, or confront the results from such exams, because they do not want to be stereotyped (i.e., black health inferiority stereotype; Steele and Aronson 1995, 1998).
Examination of the predictors of preventive health services delays among blacks has also received attention in medical and public health journals (Hammond et al. 2010a, b; Musa et al. 2009). For example, Hammond et al. (2010a) found that, compared to older, married, medically insured, and more norm-exposed black males, black men who are younger, unmarried, uninsured, and have decreased exposure to male subjective norms are less likely to receive routine preventive health services. Given the reported health gaps between blacks and whites (Aronson 2011; Calman 2007; Smedley 2011), trends in the early onset of disease among the former subgroup (Hammond et al. 2010b), and prevention emphasis in the public health and medical literatures (Cohen et al. 2003; U.S. Preventive Services Task Force 2007), understanding the antecedents of preventive service seeking among blacks should be of great importance to those in medicine, psychology, public health, and policy.
The goals of our study were threefold. First, we determined whether blacks were aware of the black health inferiority stereotype; such awareness is essential to stereotype threat effects when applied to health. Second, we adapted extant scales and inventories that assess education-based perceived threat to the health domain to establish a psychometrically stable measure of dispositional HRST. Third, we investigated the construct and incremental validity of this scale (Sackett and Lievens 2008) by correlating it with variables linked to threat effects in the psychological literature (e.g., anxiety; Pseekos et al. 2008; Spencer et al. 1999) and examining its ability to predict delays in preventive health screening and examination behaviors among blacks. Specifically, after accounting for a subset of associated factors identified in the literature (e.g., insurance status; Hammond et al. 2010a), we looked at delays in the receipt of a routine checkup, physical exam, blood pressure (BP) check, and cholesterol assay. Several of these preventive services (e.g., BP screening) are recommended for young adults (Agency for Healthcare Research and Quality Agency for Healthcare Research and Quality (AHRQ) 2010a, b; Ozer et al. 2012).
Hypotheses
We addressed these goals by examining the beliefs of blacks and the psychometrics and correlates of our HRST scale. We hypothesized that blacks would score significantly higher than the midpoint on our black-white health-related stereotype awareness item which was used as a proxy of participants’ knowledge of the black health inferiority stereotype. The latter benchmark indicated the belief that there is no difference between the health status of blacks and whites.
Consistent with theory and research (Spencer et al. 1999; Steele 1997; Steele and Aronson 1995), we posited that our HRST scale would correlate with other conceptually similar measures (e.g., black-white health-related stereotype awareness) and proxies of anxiety. Generally, we anticipated that the linear combination of several control variables—age, physical and mental health importance, health insurance and marital status, and annual income—would collectively predict delays in the receipt of preventive screenings and exams among blacks. Specifically, we expected significant, independent linear relationships to emerge between these variables and self-reported delays in preventive exams and screenings. Finally, we believed that, after accounting for the impact of the control variables, statistically reliable and independent positive linear relationships would emerge between the HRST scale and self-reported delays. To minimize article length, we only report on key findings associated with blacks apart from descriptive results.
Method
Participants
We recruited 292 students from Delaware State University (DSU; n = 242), Campbell University (CU; n = 30), and Wake Technical Community College (WTCC; n = 20). These students completed a survey containing items measuring dispositional HRST and potential correlates (e.g., anxiety), attitudes (e.g., mental health importance), enabling factors (i.e., income and insurance status), and demographics during the fall and spring semesters of 2010 and 2012. Volunteers from DSU were recruited from nursing and communications courses (and paid $5 during the fall 2010 administration), and those from CU and WTCC were recruited from psychology, education, and business courses.
Given that only the data of blacks were of interest in our study, we excluded 12 participants (4 %) who did not self-identify solely as a member of this group (e.g., biracial). The final sample consisted of 280 collegiate men (n = 65) and women (n = 209), identified as Black or African-American.Footnote 3 Although a single participant (<1 %) failed to indicate their disease history on our survey, most participants (93 %; n = 259) reported no history of hypertension, diabetes, cancer, or heart disease (dichotomous scales; 0 = No, 1 = Yes). The remaining respondents (7 %; n = 20) indicated having been diagnosed with one (n = 17), two (n = 2), or three of these conditions (n = 1).
Item Selection and Adaptation
We adapted and combined pre-existing academic threat measures to develop a scale measuring dispositional HRST among blacks. In addition, we defined this trait as the extent to which members of this group exhibit a recurring, subjective sense of fear or apprehension toward the prospect of confirming a group-based stereotype (e.g., the black health inferiority stereotype) in the health domain. Relevant proxies included Pseekos et al.’s (2008) academic stereotype threat inventory (e.g., men are better at math than women), one item from McKay’s (1999) Posttest Attitude Survey (a negative opinion exists about how people from my race perform on that type of test),Footnote 4 a single item from Chatman (1999) assessing stereotype vulnerability (I never worry that people will draw conclusions about my intelligence based on my race [reverse-coded]),Footnote 5 five items taken from the threat measure employed by Steele and Aronson (1995; for example, my race does not affect people’s perception of my verbal ability [reverse-coded]), and an item modified from Steele and Aronson by Ziegert et al. (2002; in college classes, people of my race often face biased evaluations).
Although the academic stereotype threat inventory consists of 56 items (5-point scale; 1 = never, 5 = almost always), we were interested only in the 24-item stereotype subscale. The items employed by Chatman, Steele and Aronson, and Ziegert et al. used a 7-point scale (1 = strongly disagree, 7 = strongly agree), and McKay’s item was scored on a 5-point scale (1 = strongly disagree, 5 = strongly agree).
To adapt items to the health domain, we replaced all mention of women/girls, men/boys, and math with the words blacks, whites, and health. All items referring to teachers were modified to focus on doctors. Items referring to English/math or English/math courses were altered to reflect health or doctor’s visits/routine checkups, and references to English/math tests were converted to reflect health exams or screenings.
In keeping with the academic stereotype threat inventory, our 24-item stereotype subscale was scored on a 5-point scale. The remaining eight items were assessed on a 7-point scale (1 = strongly disagree, 7 = strongly agree) with four items reverse-coded. For consistency, the latter items were converted to the former metric prior to the analysis. To minimize the activation of academic threat (e.g., triggering the black academic inferiority stereotype), we limited our use of the terms exams and tests to five items (Table 3).
To ensure that our HRST scale contained accessible vocabulary, we enlisted a master-certified health educator to conduct a readability analysis on these items. The Flesch reading easiness (range: 0–100) and Flesch-Kincaid grade level tests (Flesch 1948) in Microsoft Word (ver. 14) were used to assess the scale’s reading comprehension (Microsoft Corporation 2012) with both outcomes accounting for word and sentence difficulty in their scoring algorithms (Flesch 1948). Additionally, one’s Flesch reading score can be converted to a Flesch-Kincaid score and interpreted as an American grade level (e.g., 2nd grade; Flesch 1948; Microsoft Corporation 2012). Results confirmed that the HRST measure was understandable to an average seventh grader (Flesch score = 66.1; Flesch-Kincaid = 7.4) and, therefore, below the reading capability of most adults (Viswanath and Kreuter 2007).
Supplemental Measures
Demographics and Enabling Factors
Our survey assessed age, gender, race, annual income, marital status, and primary source of medical insurance coverage. Several of these items served as control variables in our primary analyses (e.g., age). We treated all participants who reported that they had some form of insurance as being “insured,” and the remaining participants (e.g., I don’t have health insurance) were classified as “uninsured.” Because asking participants to indicate their race has been used as a threat manipulation (Steele and Aronson 1995), we assessed this variable at the end of our survey.
Black-White Health-Related Stereotype Awareness
We included an item modified from Johns and colleagues (2008) to assess black-white health-related stereotype awareness (7-point scale [reverse-coded]; 1 = whites are stereotyped as healthier than blacks; 4 = there is no stereotype that whites and blacks differ in health status; 7 = blacks are stereotyped as healthier than whites). Higher scores reflect the belief that whites are healthier than blacks.
Routine Preventive Health Screenings and Exams
Following Hammond et al. (2010a, b), we explored delays in receiving routine preventive screenings and exams—including a checkup, physical exam, BP check, and cholesterol assay—as our primary dependent measures. Each item was scored on a 6-point scale (1 = within the past year; 2 = within the past 2 years; 3 = within the past 3 years; 4 = within the past 5 years; 5 = more than 5 years; 6 = never) with higher values indicating longer delays.Footnote 6
Subjective Physical and Mental Health Identification
According to stereotype threat theory’s domain identification tenet, threat is assumed to impact those who strongly identify with a domain (Steele 2001; Steele and Aronson 1998). As a proxy of health identification, participants indicated whether “…having the best possible physical/mental health” was important to them on two 7-point scales (1 = not at all important, 7 = extremely important).
Trait Anxiety and Fear of Physician
We included the state-trait anxiety inventory (trait version; Spielberger 1972) and fear of physician scale (Richmond et al. 1998) in our survey. The former 20-item inventory (α = 0.90; for example, I feel nervous and restless) and 5-item measure (α = 0.84; for example, when communicating with a physician, I feel nervous) used a 4-point scale (1 = not at all, 4 = very much so), with higher mean scores indicating greater trait anxiety and physician-directed apprehension, respectively. Both measures have been reliable in the past (e.g., fear of physician scale α = 0.89; Richmond et al. 1998).
Procedure
After obtaining informed consent, each participant completed the anonymous survey during self-administered group sessions.Footnote 7 Although self-paced, participants took approximately 30 min to finish our instrument. Upon completion, all participants were debriefed.
Statistical Analysis
Our data analysis was fivefold. First, we used Chi-square (χ 2) tests to explore associations between recruitment site and key categorical variables (e.g., marital status). Second, we conducted one-way analysis of variance (ANOVA) tests to assess differences in sample demographics by recruitment site. Third, we used a one-sample t-test to determine whether blacks in our sample exhibited black-white health-related stereotype awareness. Fourth, we conducted an exploratory factor analysis to examine the latent structure and stability of our HRST scale. Fifth, we provided initial validation for the resulting scale via a series of regression analyses aimed at understanding the extent to which individual differences in HRST predict preventative service use among blacks.
Results
Descriptives
Sample characteristics appear in Table 1 by recruitment site. These data revealed a significant association between marital status and institutional affiliation, χ 2(2, N = 274) = 8.65, p < .05 (Table 1). In addition, several variables produced significant institutional differences, including age, F(2, 271) = 9.44, p < .001, and trait anxiety, F(2, 260) = 7.35, p < .01.
No other significant institution-based discrepancies emerged, all ps > .26. We considered these differences as largely superficial and, therefore, collapsed these data across institutions. Table 2 presents correlations among selected study variables.
Black-White Health-Related Stereotype Awareness
As hypothesized, irrespective of institution, blacks scored significantly higher (M = 5.4; SD = 1.31; Table 1) than the midpoint (4.0) on the black-white health-related stereotype awareness item, t(251) = 16.34, p < .001. The median value for this item (Mdn = 5.0) was also above the item’s midpoint. These results indicate that participants were aware of the black health inferiority stereotype across institutions.
Factor Analysis
Given the novelty of examining dispositional HRST and the precedent of assessing individual differences in perceived academic threat among women (Pseekos et al. 2008), we analyzed participants’ scores on the initial 32 HRST items using an exploratory factor analysis with varimax orthogonal rotation. This method allowed us to tap into the most rudimentary, underlying structure exhibited by these data (George and Mallery 1999). Two extraction methods were used to determine the appropriate number of factors to retain: scree test (Cattell 1966) and parallel analysis (Franklin et al. 1995). Additionally, our sample exceeded the minimum 5-to-1 observations to variables criterion suggested by Hair and colleagues (Hair et al. 1995).
We used a three-factor solution that accounted for 55.8 % of the total model variance based on converging evidence from our extraction approaches. Specifically, these data indicated that Factors 1 (eigenvalue = 13.5), 2 (eigenvalue = 2.6), and 3 (eigenvalue = 1.8) should be retained, which explained 42.0, 8.2, and 5.6 % of the overall pre-rotated variance, respectively. For subsequent data reduction and ease of interpretation, after rotation, we used a conservative factor loading cutoff of ≥ ± 0.55 for item retention purposes. This value is just above the threshold considered high by George and Mallery (1999). Item loadings ≤ ± 0.40 on all factors were excluded, as were items with moderate loadings (i.e., ≥ ± 0.45) on two or more factors. These latter criteria removed 6 items from the scale.
We presumed that the 18-item perceived black health inferiority (PBHI) (Factor 1; α = 0.96; M = 2.8, SD = 0.83) and 6-item perceived physician racial bias (PPRB) (Factor 2; α = 0.85; M = 2.5, SD = 0.87) subscales would index the beliefs that blacks are less healthy than whites (e.g., whites have an easier time achieving good health than blacks) and physicians are biased toward blacks (e.g., doctors expect that black patients will do worse on their routine checkups than white patients). The remaining items (Factor 3) appeared to capture respondents’ beliefs regarding how race affects others’ perception of their personal health; however, this subscale was not reliable (α = 0.55). Consequently, the resulting HRST scale consisted of 24 items (heretofore referred to as the HRST-24 [full scale α = 0.96; M = 2.8, SD = 0.77]) and included the PBHI and PPRB subscales. Scale items and factor loadings from the rotated component matrix appear in Table 3.
Though correlated, r PBHI–PPRB (239) = 0.59, p < .001, these subscales were not completely redundant. In addition, mean scores on the PBHI subscale were positively correlated with the black-white health-related stereotype awareness item, r(226) = 0.23, p < .001, age, r(243) = 0.20, p < .01, and fear of physician scale scores—at marginal levels in the case of the latter, r(245) = 0.11, p = .075. Mean PPRB subscale scores were also associated with these variables, r(234) = 0.20, p < .01, r(252) = 0.25, p < .001, and r(253) = 0.16, p < .05, respectively. The latter subscale maintained a significant relationship with self-reported physical health importance, r(252) = 0.13, p < .05. Attitudes toward physical and mental health were also correlated, r(275) = 0.41, p < .001, with nearly all (>96 %) of the sample scoring at or above the midpoint on these items (Ms = 6.1 and 6.7, SDs = 1.05 and 0.78, respectively). As expected, mean scores on the state-trait anxiety inventory and fear of physician scales were significantly correlated, r(260) = 0.38, p < .001, though the former measure was not associated with either HRST subscale (all ps > .09).
Evidence of Construct and Incremental Validity
In keeping with prior studies (Pseekos et al. 2008), initial evidence of convergent validity can be gleaned from the significant intercorrelations between the HRST subscales and black-white health-related stereotype awareness item scores. Regarding incremental validity (Jaccard and Turrisi 2003; Pseekos et al. 2008; Sackett and Lievens 2008), our hierarchical multiple regression analysis consisted of two steps for all four of our preventive health delay measures. In Step 1, each dependent measure (Y) was independently regressed on the control variables (Xs; simultaneously). In Step 2, mean HRST-24 subscale scores were concurrently entered into the regression equation. However, because of our prevention focus and the greater likelihood that those already suffering from a medical condition (e.g., heart disease) would seek professional healthcare services, we excluded participants (n = 20) from these analyses that reported any pre-existing condition.
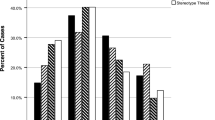
In most of our models (Table 4), adding the HRST-24 subscales to the regression equation produced models that significantly predicted postponement in routine checkup, blood cholesterol check, and physical exam behaviors even after accounting for background characteristics, enabling factors, health-related attitudes, and fear of physician scale scores. Adding subscale scores to the regression model for each of these criteria produced small effect sizes, 0.02 ≤ Cohen’s f 2 ≤ 0.07. There was no evidence, however, that the HRST-24’s subscales were associated with delays in BP check behaviors (ps for Steps 1 and 2 = 0.09 and 0.17, respectively).
The proportion of variance explained (R 2) in the models containing HRST-24 subscale scores increased anywhere from 3 % (for a routine checkup; p = .063) to 6 % (for a blood cholesterol check; p < .01), albeit at marginal levels in the case of the former when compared to the models that merely combined the control variables. The change in R 2 associated with a physical exam was negligible, p > .13.
Overall, these data indicate that incremental validity has been achieved for the HRST-24 with respect to routine checkup and blood cholesterol assay behaviors. Noteworthy, however, is that much of the incremental validity shown by the HRST-24 stems from scores on the PBHI subscale, which was (in Step 2) independently and collectively associated with three-quarters of our primary outcomes. Beta coefficients (β) obtained for this subscale were significant on the routine checkup, physical exam, and blood cholesterol check measures, ranging from 0.18 to 0.24. Furthermore, models including both subscales in their regression equations, explained between 10 and 14 % of the variance in delays in receiving a routine physical exam, checkup, and blood cholesterol assay (ps < .05), respectively.
Discussion
A limited number of published studies address the health implications of stereotype threat. In addition, much of the current HRST research can be viewed as a de facto call to action (Aronson 2011; Burgess et al. 2010), rather than a comprehensive understanding of this phenomenon in the health domain. However, if a psychometrically sound dispositional measure of HRST was to be adapted and validated, it would be a novel contribution to the literature. Such a measure would speak to the robustness and portability of extant threat scales (e.g., academic stereotype threat inventory; Pseekos et al. 2008), build on the strengths (Pseekos et al. 2008; Steele and Aronson 1995; Ziegert et al. 2002) and weaknesses (i.e., poor reliability; Chatman 1999) of these instruments, and represent one of the few assessments of this construct in the context of health.
We found that the HRST-24 was relatively short and internally consistent. Evidence of construct validity was gleaned from the scale exhibiting adequate convergent validity based on its association with our black-white health-related stereotype awareness item. Additionally, the HRST-24’s ability to predict postponement in routine preventive screening and exam behaviors, even after accounting for our control variables, served as preliminary evidence of incremental validity.
Specifically, our results showed that adding HRST-24 subscale scores to the regression equations containing our control variables significantly increased predictive ability in two of the four preventive behaviors we studied (i.e., routine checkups and blood cholesterol checks). Even so, the effect sizes associated with our findings were small. Nonetheless, inclusion of our scale in these models constituted a significant, though modest, increase in incremental explained variance (Jaccard and Turrisi 2003) and points to its potential utility in other models designed to assess health behavior among blacks.
Finally, our results support the hypothesis that blacks are cognizant of the negative stereotype surrounding the health of their racial group. Moreover, among blacks, dispositional HRST appears to be rooted in generalized beliefs about racial health differences and physician bias that are consistently “in the air” (Steele 1997, 2010).
Limitations
Despite its virtues, there are several limitations to this study. First, the lack of relationship between scores on the HRST-24 and several of our predictors and outcomes is notable. For example, though domain identification is an expected prerequisite for threat effects (Steele 2001, 2010; Steele and Aronson 1998), our data only produced significant covariation between the HRST-24’s PPRB subscale scores and physical health importance. In addition, both health importance variables failed to independently predict delays on any of the preventive health behaviors. We believe at least two reasons account for the emergence of such results: one statistical and one practical.
Statistically, the high degree of health identification expressed by participants across institutions likely produced range restriction on these items. Additionally, our sample may have been too small to detect such effects, particularly if the effect size of the relationships between health importance, the HRST-24 subscales, and health service delay scores are minimal. Indeed, survey research (Hammond et al. 2010a) has used samples in excess of 380 participants when detecting such effects—a cohort at least 36 % larger than our sample.
From a practical standpoint, extant studies (Hammond et al. 2010a, b) have focused on black males in their samples, using universities, events, and barbershops as recruitment sites. In our study, however, we relied on the former as recruitment centers and expanded our sampling frame to include black males and females. Given that black males comprised only 23 % of the final sample, our failure to replicate prior research possibly stems more from the size and gender composition of our sample than from the lack of association between the phenomena of interest.
Second, our use of a collegiate sample limits the applicability of these results. Third, our study was limited by the significant negative correlation (β) observed between PPRB and blood cholesterol check delay scores. After holding all others predictors constant, we found that higher PPRB scores were associated with shorter delays. We attribute this result to a sizeable cohort of participants (n = 49; 22 %) who reported having never received a blood cholesterol check and, on average, scored below the midpoint of the 5-point PPRB subscale (M = 2.24, SD = 0.90). These data suggest that heightened PPRB may result from real interactions with healthcare providers. Specifically, this subcomponent of HRST may be contingent upon direct communication(s) with one’s physician that affect subsequent preventive behaviors.
Recommendations for Administering the HSRT-24
The HRST-24 can be used as a research tool for investigators in the lab or field, in both academic and health contexts. For example, psychologists can use this instrument in lab studies for pre-selection purposes. Health educators can use this tool to assess individual differences in HRST among recipients of their educational interventions so that they can structure their materials in a manner least likely to trigger threat, particularly among blacks. Practitioners can use the HRST-24 as a resource in clinical contexts (e.g., waiting rooms) to identify black patients who may be highly sensitive to this phenomenon and, therefore, less likely to attend to their written or verbal health communications. We strongly discourage its inappropriate use, however, as a clinical assessment tool to identify pathology among patients.
We offer two practical recommendations for physicians, educators, and researchers regarding the HRST-24’s administration. Users of this instrument should consider: (1) interspersing distractor items among these questions and (2) reverse coding one-half of these items to control for response biases (e.g., acquiescent responding). One might accomplish the latter recommendation by altering the racial order in a given item—for example, whites are healthier than blacks (item 17) can be modified to blacks are healthier than whites.
Future Directions for HRST Research
Intuitively, one may question whether it is wise to examine HRST effects on college students at all, given that the incidence of negative health outcomes are often less of a concern among an otherwise young, healthy sample. College students may also be insufficiently representative of the population as a whole that experiences health disparities. We believe neglecting this group is unwise for at least two reasons. First, we maintain that preventive screenings are often among the first line of defense in preventing the onset of disease in young adulthood. For instance, evidence-based recommendations indicate that there is efficacy associated with BP assays among this population (Ozer et al. 2012; U.S. Preventive Services Task Force 2007). This is particularly important in the case of blacks who often experience the premature onset of adverse health events (Hammond et al. 2010b) and a reduced life expectancy (Arias 2006; Aronson 2011; Calman 2007; Hammond et al. 2010b; Harper et al. 2007) when compared with whites.
Second, though the change in R 2 and effect sizes associated with the models predicting delays in the receipt of a blood cholesterol check and routine checkup were minor, our findings show that even among a sample of predominantly young and healthy black college students, participants high in the HRST-24’s PBHI subcomponent were more likely to delay using these preventive services than their low-HRST-24 PBHI subcomponent counterparts. Future research should explore other health outcomes that are affected by HRST among this cohort.
Third, published findings suggest that: (1) the base rates associated with the receipt of preventive services (e.g., cholesterol screenings) among young adults are fairly low (Lau et al. 2013) and (2) ambulatory and preventive health care services are underused in young adulthood, particularly among black men and the uninsured, when compared to other age groups (Fortuna et al. 2009). When taken together, the implications of these findings and practical significance of our small, though significant, results suggest that HRST, with other important factors (e.g., lack of health insurance), may help to explain blacks’ infrequent use of preventive services. Early adulthood may also offer a practical intervention point in the developmental trajectory of blacks to offset lags in the receipt of preventive care among this population (Lau et al. 2013; Ozer et al. 2012). Given a limited evidence base investigating the use of preventive care among young adults (Lau et al. 2013) and the paucity of HRST research, such claims are only speculative.
Finally, our finding that age is positively correlated with HRST-24 subdimension scores suggests that the magnitude of the relationships detected herein may be different among older blacks. When compared to their younger counterparts, older blacks may be more aware of their: (1) greater odds of suffering from an aversive health condition and (2) personal experiences with physician bias, in addition to the (3) negative health outcomes experienced by members of their race (Gamble 1993). Future studies may also yield larger effects if the HRST-24 is administered to a specific age group to predict selected preventive services recommended for such cohorts. Consequently, further research is warranted.
Conclusion
Researchers have only begun to explore whether stereotype threat is associated with health outcomes (Aronson 2011; Aronson et al. 2013; Burgess et al. 2010). Our research is intended, in part, to determine whether dispositional HRST exists among blacks, and examine its association with negative health behaviors. Our results show that stereotype threat extends beyond the realm of education. For instance, our findings suggest that, if blacks are unable to insulate themselves from trait HRST, this phenomenon may lead them to postpone preventive actions that could improve their health.
Our enthusiasm regarding these results must be tempered by the limited number of empirical tests of HRST. In addition, we do not wish to discount the role of racism and discrimination in producing adverse health outcomes in minority populations (Brondolo 2011; Brondolo et al. 2009; Sawyer et al. 2012; Shavers et al. 2012) and contributing to racial disparities (Smedley 2012; Williams et al. 2012). Rather, we wish to illuminate the role of a novel trait (i.e., dispositional HRST) that may explain meaningful variance in health phenomena among blacks. Though the present research advances our understanding of HRST in a meaningful way, the questions of how and when this phenomenon operates in the health domain remain largely unanswered.
Notes
These results must be interpreted with caution given the nonsignificant race-by-condition interaction reported in this study (p < .19; Steele and Aronson 1995, 1998). Moreover, this interaction only approached significance (p < .08) when data from the nondiagnostic challenge conditions were removed from the analysis (Steele and Aronson 1995, 1998).
This planned contrast involved comparing scores on the stereotype vulnerability scale for women in male-dominated disciplines to the combined scores of women in female-dominated professions and males in male- and female-dominated areas.
Six participants (2%) did not indicate their gender on our survey.
Two items from McKay’s (1999) original three-item measure were removed from consideration given our belief that they were situationally driven (i.e., tests, like the one that I just took, have been used to discriminate against people from my race and during the test, I wanted to show that people of my race could perform well on it).
This item was a part of Spencer’s (1993) stereotype vulnerability scale used by Chatman (1999). Dr. Chatman-Nelson indicated to the first author (Paul Jones), however, that the instrument demonstrated poor internal consistency when implemented in her dissertation research (C. Chatman-Nelson, personal e-mail communication, May 4, 2010). It was included in our battery, nonetheless, to maximize our potential to achieve a stable measure of dispositional HRST.
Our treatment of the routine health screenings and exams variables was such that responses ranged from short-term (1 = within the past year) to long-term delays (6 = never). Participants indicating having never received a given preventive health service were, therefore, scored as having experienced the longest possible delay.
All procedures described herein were approved by the Institutional Review Boards at PIRE, CU, and DSU. Departmental approval was granted at WTCC.
References
Agency for Healthcare Research and Quality (AHRQ). (2010a). Men: Stay healthy at any age. Rockville, MD: Department of Health and Human Services, Agency for Healthcare Research and Quality, from http://www.ahrq.gov/ppip/healthymen.htm.
Agency for Healthcare Research and Quality (AHRQ). (2010b). Women: Stay healthy at any age. Rockville, MD: Department of Health and Human Services, Agency for Healthcare Research and Quality, from http://www.ahrq.gov/ppip/healthywom.htm.
Arias, E. (2006). United States Life Tables, 2003 National Vital Statistics Reports (Vol. 54, No. 14). Hyattsville, MD: National Center for Health Statistics. Retrieved from http://www.cdc.gov/nchs/data/nvsr/nvsr54/nvsr54_14.pdf.
Aronson, J. (2011). Stereotype threat: Implications for health disparities. Bethesda: Paper presented at the Meeting of The Science of Research on Discrimination and Health.
Aronson, J., Burgess, D., Phelan, S. M., & Juarez, L. (2013). Unhealthy interactions: The role of stereotype threat in health disparities. American Journal of Public Health, 103(1), 50–56.
Barnard, L., Burley, H., Olivarez, A., & Crooks, S. (2008). Measuring vulnerability to stereotype threat. Electronic Journal of Research in Educational Psychology, 6(1), 51–64.
Blascovich, J., Spencer, S. J., Quinn, D., & Steele, C. (2001). African Americans and high blood pressure: The role of stereotype threat. Psychological Science, 12, 225–229.
Boulware, L. E., Cooper, L. A., Ratner, L. E., LaVeist, T. A., & Powe, N. R. (2003). Race and trust in the health care system. Public Health Reports, 118(4), 358–365.
Brondolo, E. (2011, February). Discrimination, stress, and physical health. Paper presented at the Meeting of The Science of Research on Discrimination and Health, Bethesda, MD. http://128.231.124.72/download/conference/nci020411_512.f4v.
Brondolo, E., Brady ver Halen, N., Pencille, M., Beatty, D. L., & Contrada, R. J. (2009). Coping with racism: A selective review of the literature and a theoretical and methodological critique. Journal of Behavioral Medicine, 32(1), 64–88.
Burgess, D., Warren, J., Phelan, S., Dovidio, J., & van Ryn, M. (2010). Stereotype threat and health disparities: What medical educators and future physicians need to know. Journal of General Internal Medicine, 25(Suppl. 2), 169–177.
Calman, N. (2007). Disparities in diabetes control within our Community Health Center Network. Paper presented at the Annual Meeting of the Office of Health Information Technology (OHIT) Grantees, Crystal City, VA.
Cattell, R. B. (1966). The scree test for the number of factors. Multivariate Behavioral Research, 1(2), 245–276.
Chandler, M. (Writer) & M. Chandler (Director). (1999). Secrets of the SAT [Televison series episode]. In M. Chandler (Producer), Frontline. Virginia: Public Broadcasting Service (PBS).
Chatman, C. M. (1999). The identity paradox model: Explaining school performance among African-American college students. Dissertation Abstracts International, 60(2–B), 0872.
Cohen, E. (2009, July 26). Does your doctor judge you based on your color? CNN health.com. Retrieved from CNN health.com website: http://www.cnn.com/2009/HEALTH/07/23/doctors.attitude.race.weight/.
Cohen, L., Miller, T. R., Sheppard, M. A., Gordon, E., Gantz, T., & Atnafou, R. (2003). Bridging the gap: Bringing together intentional and unintentional injury prevention efforts to improve health and well being. Journal of Safety Research, 34(5), 473–483.
Corbie-Smith, G., Thomas, S. B., Williams, M. V., & Moody-Ayers, S. (1999). Attitudes and beliefs of African Americans toward participation in medical research. Journal of General Internal Medicine, 14(9), 537–546.
Davis, C, I. I. I., & Simmons, C. (2009). Stereotype threat: A review, critique, and implications. In H. A. Neville, B. M. Tynes, & S. O. Utsey (Eds.), Handbook of African American Psychology (pp. 211–222). Thousand Oaks: Sage Publications.
DuBois, W. E. B. (1906). The health and physique of the Negro American. Atlanta: Atlanta University Press.
Flesch, R. (1948). A new readability yardstick. Journal of Applied Psychology, 32(3), 221–233.
Fortuna, R. J., Robbins, B. W., & Halterman, J. S. (2009). Ambulatory care among young adults in the United States. Annals of Internal Medicine, 151(6), 379–385.
Franklin, S. B., Gibson, D. J., Robertson, P. A., Pohlmann, J. T., & Fralish, J. S. (1995). Parallel analysis: A method for determining significant principal components. Journal of Vegetation Science, 6, 99–106.
Gamble, V. N. (1993). A legacy of distrust: African Americans and medical research. American Journal of Preventive Medicine, 9(6, Suppl), 35–38.
Gamble, V. N. (2011). Background/history race/ethnicity-based discrimination and its association with health. Bethesda: Paper presented at the Meeting of The Science of Research on Discrimination and Health.
George, D., & Mallery, P. (1999). SPSS for windows step by step: A simple guide and reference. Needham Heights: Allyn & Bacon.
Hair, J. F., Jr, Anderson, R. E., Tatham, R. L., & Black, W. C. (1995). Multivariate Data Analysis (3rd ed.). New York: Macmillan.
Hammond, W. P., Matthews, D., & Corbie-Smith, G. (2010a). Psychosocial factors associated with routine health examination scheduling and receipt among African American men. Journal of the National Medical Association, 102, 276–289.
Hammond, W. P., Matthews, D., Mohottige, D., Agyemang, A., & Corbie-Smith, G. (2010b). Masculinity, medical mistrust, and preventive health services delays among community-dwelling African American men. Journal of General Internal Medicine, 25, 1300–1308.
Harper, S., Lynch, J., Burris, S., & Davey Smith, G. (2007). Trends in the Black-White life expectancy gap in the United States, 1983–2003. Journal of the American Medical Association, 297, 1224–1232.
Henry, J. D., von Hippel, C., & Shapiro, L. (2010). Stereotype threat contributes to social difficulties in people with schizophrenia. British Journal of Clinical Psychology, 49, 31–41.
Inzlicht, M., & Kang, S. K. (2010). Stereotype threat spillover: How coping with threats to social identity affects aggression, eating, decision making, and attention. Journal of Personality and Social Psychology, 99(3), 467–481.
Jaccard, J., & Turrisi, R. (2003). Interaction effects in multiple regression (2nd ed.). Thousand Oaks: Sage.
Joanisse, M. M., Gagnon, S. S., & Voloaca, M. M. (2013). The impact of stereotype threat on the simulated driving performance of older drivers. Accident Analysis and Prevention, 50, 530–538.
Johns, M., Inzlicht, M., & Schmader, T. (2008). Stereotype threat and executive resource depletion: The influence of emotion regulation. Journal of Experimental Psychology, 137, 691–705.
Johnson, R. L., Saha, S., Arbelaez, J. J., Beach, M. C., & Cooper, L. A. (2004). Racial and ethnic differences in patient perceptions of bias and cultural competence in health care. Journal of General Internal Medicine, 19(2), 101–110.
Kit, K. A., Tuokko, H. A., & Mateer, C. A. (2008). A review of the stereotype threat literature and its application in a neurological population. Neuropsychology Review, 18(2), 132–148.
Lau, J. S., Adams, S. H., Irwin, C. E., Jr, & Ozer, E. M. (2013). Receipt of preventive health services in young adults. Journal of Adolescent Health, 52(1), 42–49.
LaVeist, T. A., Nickerson, K. J., & Bowie, J. V. (2000). Attitudes about racism, medical mistrust, and satisfaction with care among African American and White cardiac patients. Medical Care Research and Review, 57(suppl 1), 146–161.
Levy, B. (1996). Improving memory in old age through implicit self-stereotyping. Journal of Personality and Social Psychology, 71, 1092–1107.
Lillie-Blanton, M., Brodie, M., Rowland, D., Altman, D., & McIntosh, M. (2000). Race, ethnicity, and the health care system: Public perceptions and experiences. Medical Care Research and Review, 57(suppl 1), 218–235.
Macinko, J., & Elo, I. T. (2009). Black-White differences in avoidable mortality in the United States, 1980–2005. Journal of Epidemiology and Community Health, 63(9), 715–721.
Mackie, D. M., Hamilton, D. L., Susskind, J., & Rosseli, F. (1996). Social psychological foundations of stereotype formation. In C. N. Macrae, C. Stangor, & M. Hewstone (Eds.), Stereotypes and stereotyping (pp. 41–78). New York: Guilford Press.
McGairk, C. (2008). High blood pressure: Black men least aware of its symptoms, study reveals. Jet, 114, 12–14.
McKay, P.F. (1999). Stereotype threat and its effect on the cognitive ability test performance of African-Americans: The development of a theoretical model. Unpublished doctoral dissertation, University of Akron, Akron, OH.
McKay, P. F., Doverspike, D., Bowen-Hilton, D., & Martin, Q. D. (2002). Stereotype threat effects on the Raven Advanced Progressive Matrices scores of African Americans. Journal of Applied Social Psychology, 32, 767–787.
McKay, P. F., Doverspike, D., Bowen-Hilton, D., & McKay, Q. D. (2003). The effects of demographic variables and stereotype threat on black/white differences in cognitive ability test performance. Journal of Business and Psychology, 18, 1–14.
Microsoft Corporation. (2012). Test your document’s readability. Microsoft Corporation: Redmond, WA. Retrieved July, 2012, from http://office.microsoft.com/en-us/word-help/test-your-document-s-readability-HP010148506.aspx#BM1.
Musa, D., Schulz, R., Harris, R., Silverman, M., & Thomas, S. B. (2009). Trust in the health care system and the use of preventive health services by older Black and White adults. American Journal of Public Health, 99(7), 1293–1299.
Nguyen, H. D., & Ryan, A. M. (2008). Does stereotype threat affect test performance of minorities and women? A meta-analysis of experimental evidence. Journal of Applied Psychology, 93(6), 1314–1334.
Oskamp, S., & Schultz, P. W. (2005). Attitudes and Opinions. Mahwah: Lawrence Erlbaum Associates.
Ozer, E. M., Urquhart, J. T., Brindis, C. D., Park, M. J., & Irwin, C. E, Jr. (2012). Young adult preventive health care guidelines: There but can’t be found. Archives of Pediatrics and Adolescent Medicine, 166(3), 240–247.
Pieterse, A. L., Todd, N. R., Neville, H. A., & Carter, R. T. (2012). Perceived racism and mental health among Black American adults: A meta-analytic review. Journal of Counseling Psychology, 59(1), 1–9.
Pseekos, A. C., Dahlen, E. R., & Levy, J. J. (2008). Development of the academic stereotype threat inventory. Measurement and Evaluation in Counseling and Development, 41, 2–12.
Richmond, V. P., Smith, R. S., Heisel, A. M., & McCroskey, J. C. (1998). The impact of communication apprehension and fear of talking with a physician and perceived medical outcomes. Communication Research Reports, 15, 344–353.
Sackett, P. R., Hardison, C. M., & Cullen, M. J. (2004). On interpreting stereotype threat as accounting for African American-White differences on cognitive tests. American Psychologist, 59, 7–13.
Sackett, P. R., & Lievens, F. (2008). Personnel selection. Annual Review of Psychology, 59, 419–445.
Sawyer, P. J., Major, B., Casad, B. J., Townsend, S. S. M., & Mendes, W. B. (2012). Discrimination and the stress response: Psychological and physiological consequences of anticipating prejudice in interethnic interactions. American Journal of Public Health, 102(5), 1020–1026.
Seacat, J. D., & Mickelson, K. D. (2009). Stereotype threat and the exercise/dietary health intentions of overweight women. Journal of Health Psychology, 14, 556–567.
Shavers, V. L., Fagan, P., Jones, D., Klein, W. M. P., Boyington, J., Moten, C., et al. (2012). The state of research on racial/ethnic discrimination in the receipt of health care. American Journal of Public Health, 102(5), 953–966.
Smedley, B. (2011). Why study discrimination?. Bethesda: Paper presented at the Meeting of The Science of Research on Discrimination and Health.
Smedley, B. (2012). The lived experience of race and its health consequences. American Journal of Public Health, 102(5), 933–935.
Smedley, B., Stith, A., & Nelson, A. (2003). Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academies Press.
Smith, W. R., Betancourt, J. R., Wynia, M. K., Bussey-Jones, J., Stone, V. E., Phillips, C. O., et al. (2007). Recommendations for teaching about racial and ethnic disparities in health and health care. Annals of Internal Medicine, 147, 654–665.
Spencer, S.J. (1993). The effect of stereotype vulnerability on women’s math performance. Unpublished doctoral dissertation. University of Michigan.
Spencer, S. J., Steele, C. M., & Quinn, D. M. (1999). Stereotype threat and women’s math performance. Journal of Experimental Social Psychology, 35(1), 4–28.
Spielberger, C.D. (1972). Anxiety: Current trends in theory and research. In C.D. Spielberger (Ed.) (Vol. 1). New York: Academic Press.
Steele, C. M. (1997). A threat in the air: How stereotypes shape intellectual ability and performance. American Psychologist, 52(6), 613–629.
Steele, C.M. (2001). Reading 6: Contemporary. Thin ice: “Stereotype threat” and Black college students. In E.J. Coats & R.S. Feldman (Eds.), Classic and Contemporary Readings in Social Psychology (pp. 71–80). Upper Saddle River, NJ: Prentice-Hall Inc.
Steele, C. M. (2010). Whistling Vivaldi and other clues to how stereotypes affect us. New York: W.W. Norton and Company.
Steele, C. M., & Aronson, J. (1995). Stereotype threat and the intellectual test performance of African Americans. Journal of Personality and Social Psychology, 69(5), 797–811.
Steele, C. M., & Aronson, J. (1998). Stereotype threat and the test performance of academically successful African Americans. In C. Jencks & M. Phillips (Eds.), The Black-White Test Score Gap (pp. 401–427). Washington, DC: Brookings Institution Press.
Steele, C. M., & Aronson, J. (2004). Stereotype threat does not live by Steele and Aronson (1995) alone. American Psychologist, 59(1), 47–48.
Steele, C. M., & Davies, P. G. (2003). Stereotype threat and employment testing. Human Performance, 16, 311–326.
Steele, J., James, J. B., & Barnett, R. C. (2002). Learning in a man’s world: Examining the perceptions of undergraduate women in male-dominated academic areas. Psychology of Women Quarterly, 26(5), 46–50.
Stone, J., Lynch, C. I., Sjomeling, M., & Darley, J. M. (1999). Stereotype threat effects on Black and White athletic performance. Journal of Personality and Social Psychology, 77(6), 1213–1227.
Terrell, F., & Terrell, S. (1981). An inventory to measure cultural mistrust among blacks. Western Journal of Black Studies, 5, 180–185.
U.S. Preventive Services Task Force. (2007). Screening for high blood pressure: U.S. Preventive Services Task Force reaffirmation recommendation statement. Annals of Internal Medicine, 147(11), 783–786.
Viswanath, V., & Kreuter, M. W. (2007). Health disparities, communication inequalities and E-health: A commentary. American Journal of Preventative Medicine, 32(Suppl. 5), 131–133.
Williams, D. R., John, D. A., Oyserman, D., Sonnega, J., Mohammed, S. A., & Jackson, J. S. (2012). Research on discrimination and health: An exploratory study of unresolved conceptual and measurement issues. American Journal of Public Health, 102(5), 975–978.
Woolf, K., Cave, J., Greenhalgh, T., & Dacre, J. (2008). Ethnic stereotypes and the underachievement of UK medical students from ethnic minorities: Qualitative study. British Medical Journal, 337(Clinical Research Edition), 1–7.
Yeung, N. C. J., & von Hippel, C. (2008). Stereotype threat increases the likelihood that female drivers in a simulator run over jaywalkers. Accident Analysis and Prevention, 40, 667–674.
Ziegert, J.C., Ployhart, R.E., & McFarland, L.A. (2002, April). Perceived stereotype threat: Development of a self-report scale. Paper presented at the 17th Annual Conference of the Society for Industrial and Organizational Psychology, Toronto, Canada.
Acknowledgments
This research was funded by NCI Grant #1R21CA154258 to the primary author and supported by the Office of Behavioral and Social Sciences Research. The views expressed herein are those of the authors and do not necessarily reflect those of the funding agency. We give special acknowledgement to Ted Miller, Elizabeth Klonoff, and the anonymous reviewers for their helpful comments. We also acknowledge Maria Nguyen, Samuel Faulkner, and Brooke Strouth for their help in survey preparation and data collection. Special thanks go to Mary Beth Mason and Alma Lopez for their editorial assistance, and Raymond Mullings for his help in data entry.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jones, P.R., Taylor, D.M., Dampeer-Moore, J. et al. Health-Related Stereotype Threat Predicts Health Services Delays Among Blacks. Race Soc Probl 5, 121–136 (2013). https://doi.org/10.1007/s12552-013-9088-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12552-013-9088-8