Abstract
Purpose
This cross-sectional study examined the relationship between headache-specific locus of control (HSLC) and migraine-related quality of life, and anxiety as a mediator of this relationship.
Method
Two hundred and thirty-two people with migraine participated in the treatment of severe migraine trial. At baseline, participants completed self-report questionnaires of headache-specific locus of control (HSLC; subscales = internal, chance, and medical professionals), anxiety, and migraine-related quality of life. Correlations examined relationships between HSLC, anxiety, and migraine-related quality of life; ordinary least squares regression evaluated anxiety as a mediator of the relationship between HSLC and migraine-related quality of life.
Results
Higher internal HSLC was related to higher overall migraine-related quality of life (ps < .05) and emotion function impairments (p = .012). Anxiety mediated the relationship between internal HSLC and all measures of migraine-specific quality of life (ps < .05). Higher external (medical professionals and chance) HSLC was related to higher migraine-related quality of life impairments (all ps < .001).
Conclusion
All HSLC beliefs are associated with higher migraine-related quality of life impairments. Anxiety mediates the relationship between internal HSLC and migraine-related quality of life.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Migraine is a headache disorder in which individuals experience moderate to severe unilateral pulsating head pain, which lasts from 4 to 72 h [1]. Associated symptoms include nausea, vomiting, photophobia, and phonophobia [1]. Migraine prevalence rates, in adults in the USA, range from 11.7 to 22.7 % [2]. The Global Burden of Disease Survey, 2010 ranked migraine as the seventh highest specific cause of disability worldwide [3]. Migraine has been linked to significant burden, including impaired social and occupational functioning and decreased quality of life [4, 5]. Psychosocial difficulties associated with migraine include emotional difficulties, functioning limitations and restrictions, and poor quality of life [6]. Further understanding what factors are associated with poor quality of life will aid treatment planning to ameliorate the negative impact of migraine.
In the cognitive behavioral therapy model [7] of migraine, beliefs influence affective (emotional) and behavioral responses to migraine [7, 8], which in turn influence quality of life. Headache-specific locus of control (HSLC) refers to an individual’s belief that the development and progression of headache symptoms are a consequence of their own behavior (internal HSLC) or something external to themselves, including chance (chance HSLC) or their medical professional’s actions (medical professionals HSLC) [9]. External (chance and medical professionals) HSLC has demonstrated associations with impaired headache-related quality of life in a handful of older studies examining college students or outpatients with migraine and/or tension-type headache [9–11]. Higher internal HSLC has also demonstrated associations with higher disability [9]. None of these aforementioned studies evaluated the differential impact of HSLC beliefs on the role functioning and emotional functioning aspects of headache-related quality of life. Further, these three studies included participants with heterogeneous headache diagnoses; no study has examined the impact of HSLC on headache-related quality of life in a homogenous sample of people with migraine.
Anxiety disorders are comorbid with migraine [12, 13] and are associated with poorer migraine-related quality of life within people with migraine [12, 14]. Anxiety is a potent affective response characterized as “a state of helplessness, because of a perceived inability to predict, control, or obtain desired results or outcomes [15]” (p 1249). Thus, anxiety is intrinsically related to beliefs regarding control [16] and may be implicated in the relationship between HSLC and migraine-related quality of life. Interestingly, one study has demonstrated that higher anxiety is associated with both higher internal and chance HSLC, even though internal and chance HSLC are negatively related to each other [11]. Thus, it is possible that the mechanism of anxiety operates differently for internal and chance HSLC. To date, no studies have examined anxiety as a mediator of the relationship between HSLC and migraine-related quality of life. This knowledge will allow us to enhance cognitive behavioral treatment targets to improve migraine-related quality of life.
The present cross-sectional study aims to (1) examine the relationship between HSLC and migraine-related quality of life, including both role and emotional impairment, and (2) evaluate anxiety as a mediator of the relationships between HSLC and migraine-related quality of life in patients with migraine recruited from outpatient settings.
Method
Treatment of Severe Migraine Trial
The current cross-sectional study is a secondary analysis of baseline data from a larger 16-month randomized controlled treatment trial evaluating whether the addition of behavioral migraine management, preventive medication, or their combination to optimized acute therapy improved migraine symptoms and migraine-related quality of life among people with migraine (treatment of severe migraine trial) [17]. To date, six papers have been published from the treatment of severe migraine trial [17–22]. The primary analysis demonstrated that the combination of behavioral migraine management and preventive medication produced the largest decrease in migraine symptoms and migraine-related quality of life [17].
Participants
Two hundred and thirty-two participants were recruited for the treatment of severe migraine trial from July 2001 to November 2005, in two outpatient settings in Ohio. Inclusion and exclusion criteria were aligned with recommendations made by the American Headache Society regarding behavioral randomized clinical trials [23]. Inclusion criteria were (1) individuals aged 18 to 65 with an International Classification of Headache Disorders diagnosis of migraine (with or without aura) [24] by two evaluations in the clinic (2) at least three migraines with reported disability in a 30-day diary monitoring period and (3) less than 20 headache days over a 30-day period. Exclusion criteria were (1) International Classification of Headache Disorders [24] diagnosis of definite and probable medication overuse headache, (2) an additional primary pain disorder, (3) 20 or more headache days over a 30-day period, (4) contraindication to study medications (β blocker: Propranolol or Nadolol), or current use of preventive medications, (5) receiving current psychological treatment, (6) inability to read and understand study documents, and (7) female participants who are pregnant or breastfeeding or plan to become pregnant or breastfeed. Of note, inclusion/exclusion criteria for the present study were in accordance with the International Classification of Headache Disorder’s 1998 criteria [24]. The International Classification of Headache Disorder’s second edition in 2004 [25] and the current third edition (ICHD-3 beta) published in 2013 [1], include chronic migraine as a diagnosis, referring to individuals who experience 15 or more migraine days per month. The by default the current study therefore includes some participants with chronic migraine (up to 20 days) and excludes those with greater than 20 days.
Table 1 presents participants’ demographic data. Two hundred and thirty-two males (N = 48, 20.7 %), and females (N = 184, 79.3 %) participated in the study. Their ages ranged from 18 to 62 years (M = 38.6, SD = 10). The majority of the participants were married (N = 134, 59.3 %), not of Hispanic origin (N = 194, 83.6 %), and held a high school/GED degree (N = 83, 37.1 %) or a BA/BS degree (N = 62, 27.7 %). Participants recorded an average of 5.5 migraines (SD = 1.9) and 8.5 days (SD = 3.6) with migraine over a 30-day period.
Procedure
At baseline, participants were given a structured interview pertaining to their headache and psychosocial history, in addition to receiving a medical examination by a neurologist. Participants completed electronic self-report questionnaires pertaining to headache related cognitions (HSLC), migraine-related quality of life, and psychiatric symptoms (anxiety). The current study utilizes baseline data.
Materials
Demographics
Participants answered self-report demographic questions relating to their age, gender, ethnicity, the highest degree completed, household income, marital status, and employment status.
Headache-Specific Locus of Control (HSLC) [9]
A 33-item self-report measure pertaining to an individuals’ belief that the development and progression of headache symptoms are a consequence of their own behavior, their medical professional’s actions, or due to chance. Items are rated on a 5-point Likert scale (1 = strongly disagree to 5 = strongly agree). Three subscale scores were utilized: internal HSLC, chance HSLC, and health care professionals HSLC. Items include, “When I drive myself too hard I get headaches” (internal), “When I have a headache, there is nothing I can do to affect its course” (chance), and “Health professionals keep me from getting headache” (medical professionals). In the original validation study, the HSLC demonstrated good internal consistency (αs = 0.84–0.88), and adequate test-retest reliability over a 3-week period (rs = 0.72 to 0.78).
Headache Disability Inventory (HDI) [26]
A 25-item self-report measure pertaining to the impact of headaches in terms of emotion “I feel desperate because of my headaches” and on daily functioning “I restrict my recreational activities (e.g., sports, hobbies) because of my headaches.” Individuals respond to items indicating yes, sometimes or no. The HDI demonstrated good internal consistently (r = 0.94), and good 60-day test-retest reliability (r = 0.83) in the original validation study. Items on the HDI scale have a large emotional overlay. Within our sample, emotion and functioning subscales did not emerge as distinct factors; thus, only the total score is utilized in the current analysis.
Migraine-Specific Quality of Life Questionnaire (MSQL) [27]
A 16-item self-report measure pertaining to an individual’s migraine-related quality of life impairments over the past 4 weeks. Items are rated on a 6-point Likert scale (1 = none of the time to 6 = all of the time). This scale measures a wide range of aspects of migraine-related quality of life: role functioning and emotional functioning. There are three subscales: role function-restrictive, role function-preventive, and emotional function. Items include, “In the past 4 weeks, how often have migraines interrupted your leisure time activities, such as reading or exercising?” (role function-restrictive), “In the past 4 weeks, how often have you had to cancel work or daily activities because you had a migraine?” (role function-preventative), and “In the past 4 weeks how often have you felt like you were a burden on others because of your migraines?” (emotional function). Higher scores on the MSQL indicate higher levels of disability. The MSQL demonstrated good internal consistency for all three subscales (αs = 0.70–0.85) in the original validation study.
Beck Anxiety Inventory (BAI) [28]
A 21-item self report measure pertaining to an individual’s anxiety related symptoms. Items are rated on a 4-point Likert (0 = not at all to 4 = severely—it bothered me a lot). Items include “unable to relax,” “fear of losing control” and “numbness or tingling.” Higher scores on the BAI indicate higher levels of anxiety. In the original validation study, the BAI demonstrated high internal consistency (α = .92).
Data Analysis
Aim 1
Descriptive statistics characterized the data. Normality of the data was assessed by examining skewness and kurtosis statistics. Pearson’s product-moment correlation coefficient examined the zero-order relationships between HSLC and migraine-related quality of life. In order to correct for multiple comparisons, a Bonferroni-Holm correction was applied. The Bonferroni-Holm correction is calculated by firstly ordering the p vales in ascending order, and then dividing the alpha level (0.05) by the remaining family-wise comparisons in order to control the family-wise error rate [29]. The Bonferroni-Holm correction is a popular and more powerful method used to correct for multiple comparisons compared with the Bonferroni correction [30].
Aim 2
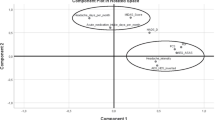
Mediation analysis provides a method to test theory-driven hypotheses about paths between related variables [31]. Conceptually, mediation occurs when a predictor variable (X) influences an outcome (Y) through a mediator (M) (Fig. 1). This pathway is called the “indirect effect,” (ab), as opposed to the “direct effect” (c′; the influence of X on Y with M in the model) and the “total effect” (c: the zero-order relationship between X and Y). For the current paper, we were interested in whether HSLC (X) influenced migraine quality of life (Y) through anxiety (M).
The current paper uses a series of Hayes PROCESS procedures to directly test the indirect effect (ab) using a series of regressions and a bootstrapping procedure [32]. As depicted in Fig. 1, in order to obtain the ab estimate, we first regressed X (HSLC) on M (BAI). The coefficient for X in this model corresponds with the a pathway. Second, we regressed X (HSLC) and M (BAI) on Y (quality of life). The coefficient for M in this model corresponds with the b pathway. A bootstrapping procedure was then utilized to obtain the ab estimate and a 95 % confidence interval surrounding the ab estimate. Bootstrapping creates the estimate and 95 % confidence interval using random sampling of the dataset with replacement, which does not assume normality of the data and is thus robust to non-normal distributions [21]. A significant indirect effect (e.g., one in which the 95 % confidence interval does not include zero) represents a significant mediation model [32, 33].
Each MSQL subscale and HDI served as an outcome in separate mediation models. Each HSLC subscale served as a predictor in separate mediation models. The BAI served as the mediator in all mediation models. Mediation can occur even when the total effect is not significant, [32], therefore mediation was tested for each outcome and predictor.
Alpha was set at .05. All analyses were two-tailed. All Analyses were completed in SPSS version 22.0.
Results
Relationships Between HSLC and Migraine-Related Quality of Life
Table 2 presents correlations among the variables. Pearson-product moment correlations using the Bonferroni-Holm procedure for multiple comparisons indicated that higher internal HSLC was related to higher overall migraine-related quality of life impairments (HDI total), and higher impairment on the emotion function subscale of the MSQL. Both higher chance HSLC and higher medical professionals HSLC were related to higher overall migraine-related quality of life impairments (MSQL total and HDI total) and to all three MSQL subscales (role restriction, role prevention, and emotion function MQoL impairments).
Anxiety as a Mediator Between HSLC and Migraine-Related Quality of Life
Anxiety mediated the relationship between internal HSLC and all measures of migraine-specific quality of life (see Table 3). There was a significant indirect effect of internal HSLC on MQoL (HDI total) through anxiety, ab = 0.20, 95 % CI [0.08, 0.37], R 2 = 27 % (see Fig. 2). The size of the effect was small (k 2 = .09). There was a significant indirect effect of internal HSLC on migraine-related quality of life (MSQL total) through anxiety, ab = 0.09, 95 % CI [0.03, 0.17], R 2 = 13 % (see Fig. 3). The size of the effect was small (k 2 = .06). This result was comparable for each MSQL subtest ps < .05.
There were no significant indirect effects of chance HSLC or medical professionals HSLC on any measures of migraine-related quality of life through anxiety, ps > .05.
Discussion
The present cross-sectional study found that higher internal HSLC was related to emotionally laden quality of life impairments, which was mediated by anxiety. Higher external HSLC (medical professional HSLC and chance HLC) was related to higher migraine-related quality of life impairments in terms of role restriction, role prevention, and emotion function. Results indicate that higher internal HSLC demonstrated a direct negative impact on the emotional aspects of migraine-related quality of life. Thus, internal HSLC beliefs may be maladaptive in certain circumstances, particularly when evaluating emotional quality of life. For example, the belief that the development and progression of headache symptoms is due to the patients’ own actions may be maladaptive in relation to phenomena which the individual may exert little influence, such as whether they will experience a migraine. The relationship between internal HSLC and anxiety appears to at least partly explain this relationship. In this study, as in previous studies, higher internal HSLC was related to higher anxiety symptoms [11, 16]. Further, this study demonstrated that anxiety mediated relationships between internal HSLC and all measures of migraine-related quality of life. This accounts for at least part of the maladaptive nature of internal HSLC among people with migraine. Current findings provided novel information regarding anxiety as a mediator between internal HSLC beliefs and migraine-related quality of life. To our knowledge, this is the first study to evaluate the interrelationships between HSLC, anxiety, and migraine-related quality of life in people with migraine.
It should be noted that previous studies have found that higher internal HSLC is associated with higher levels of adaptive headache-related beliefs (self-efficacy [11]). Further, behavioral treatments that increase internal HSLC have demonstrated efficacy for reducing migraine-related quality of life [19]. Thus, it appears that internal HSLC is multifaceted: on the one hand, it is related to anxiety, and is associated with poorer emotional migraine-related quality of life in cross-sectional studies; on the other hand, it is related to adaptive headache-related beliefs, and improves during effective treatment of migraine. It is possible that internal HSLC is multi-factorial; perhaps internal HSLC is adaptive in relation to headache-related phenomena that are indeed controllable by the individual (e.g., stress management, migraine medication-taking behaviors), whereas, internal HSLC is less adaptive in relation to phenomena which the individual may exert little influence (e.g., the presence of migraine), partly due to the relationship with anxiety and emotional migraine-related quality of life impairments. Future research should continue evaluate the multiple roles of internal HSLC in migraine-related quality of life, and in the behavioral treatment of migraine.
Higher beliefs that the development and progression of headache symptoms are predominantly due to chance, or a consequence of medical professional’s actions, were associated with poorer MQoL across all measures. These findings are consistent with previous research [9–11]. Certainly the belief that only chance or fate can influence the onset and course of migraines is fatalistic and maladaptive, and could lead to skepticism about treatment recommendations and discontinuing adaptive migraine management efforts. However, it is less immediately clear how higher medical professionals HSLC is necessarily maladaptive. Higher medical professionals HSLC may indicate an overreliance on the actions of one’s headache provider, to the exclusion of self-management behaviors necessary for successful treatment of a complex chronic disorder such as migraine. On the other hand, many lifestyle recommendations for migraine include dietary and lifestyle restriction to avoid migraine triggers; perhaps high medical professionals HSLC leads to excessive restriction of adaptive pleasurable activities for fear that they may induce migraine. People with migraine may thus benefit from clarity from their physicians regarding their ability to partake in a variety of activities.
Taken together with the prior literature, findings from this study suggest that higher external (medical professionals and chance) HSLC is consistently associated with poorer migraine-related quality of life. Higher internal HSLC is associated with poorer emotional migraine-related quality of life; further, internal HSLC is associated with higher anxiety, which mediates relationships between internal HSLC and migraine-related quality of life. Future research should use these findings to guide evaluation of different clinical techniques for different HSLC beliefs. For example, people with migraine and high internal HSLC may benefit specifically from techniques that focus on reducing anxiety and the emotional burden of migraine, such as third-wave cognitive behavioral therapies for migraine (e.g., acceptance and commitment therapy and mindfulness-based cognitive therapy), which are designed to reduce the burden of migraine and associated affective distress [34]. Further, this study suggests that although effective behavioral treatments increase internal HSLC, higher internal HSLC in the absence of migraine management tools taught during behavioral treatment may be maladaptive. Thus, within clinical practice, the use of a HSLC measure may help guide the types of treatments offered, with the ultimate goal of reducing migraine-related quality of life impairments.
Limitations/Future Directions
The current study evaluates baseline data from a randomized controlled trial. Consequently, all participants were seeking further treatment, and may therefore not be satisfied with their current health care. Future research would benefit from examining participants who are not enrolled in a trial, where participants might be more satisfied with their health care. Additional information pertaining to provider characteristics, such as patient’s satisfaction with their medical provider, and length of relationship with their medical provider would also be beneficial, as this may impact individuals’ HSLC beliefs. Further, addressing whether migraine-related quality of life differs between patients who are satisfied with their treatment in comparison with those who are not will be useful.
Due to the cross-sectional nature of the study, we were unable to examine temporal relationships between the variables. Further, all measures utilized in this study comprised of self-report data, which is reliant on participant recall and is subject to bias. All of the participants experienced migraines; thus, it is possible that their reported headache-related quality of life may differ from those who are diagnosed with other headache disorders. Future research should therefore examine whether differences in HSLC beliefs and headache-related quality of life impairments prevail in patients with other types of headaches.
Conclusion
This study found that people with migraine who believe that the development and progression of their headache symptoms are due to internal factors experience emotion-related migraine-related quality of life impairments. Moreover, the relationship between internal HSLC and migraine-related quality of life is mediated by anxiety. Individuals who believe that the development and progression of their headache symptoms are due to external factors experience migraine-related quality of life impairments in terms of both role and emotional impairments. Future studies should further examine the utility of HSLC beliefs in guiding treatments for people with migraine.
References
International Headache Society Classification Subcommittee. The international classification of headache disorders, 3rd edition (beta version). Cephalalgia. 2013;33(9):629–808. doi:10.1177/0333102413485658.
Smitherman TA, Burch R, Sheikh H, Loder E. The prevalence, impact, and treatment of migraine and severe headaches in the United States: a review of statistics from national surveillance studies. Headache. 2013;53(3):427–36.
Martelletti P, Birbeck GL, Katsarava Z, Jensen RH, Stovner LJ, Steiner TJ. The Global Burden of Disease survey 2010, Lifting The Burden and thinking outside-the-box on headache disorders. J Headache Pain. 2013;14(1):13. doi:10.1186/11292377-14-13.
Leonardi M, Steiner TJ, Scher AT, Lipton RB. The global burden of migraine: measuring disability in headache disorders with WHO’s Classification of Functioning, Disability and Health (ICF). J Headache Pain. 2005;6(6):429–40. doi:10.1007/s10194005-0252-4.
Leonardi M, Raggi A, Bussone G, D’Amico D. Health-related quality of life, disability and severity of disease in patients with migraine attending to a specialty headache center. Headache. 2010;50(10):1576–86. doi:10.1111/j.1526-4610.2010.01770.x.
Raggi A, Giovannetti AM, Quintas R, et al. A systematic review of the psychosocial difficulties relevant to patients with migraine. J Headache Pain. 2012;13(8):595–606. doi:10.1007/s10194-012-0482-1.
Beck AT. The current state of cognitive therapy: a 40-year retrospective. Arch gen psychiatry. 2005;62(9):953–9. doi:10.1001/archpsyc.62.9.953.
Holroyd KA, Andrasik F. A cognitive-behavioral approach to recurrent tension and migraine headache. Adv Cogn Behav Res Ther. 1982;1:275–320.
Martin NJ, Holroyd KA, Penzien DB. The headache-specific locus of control scale: adaptation to recurrent headaches. Headache. 1990;30(11):729–34.
Scharff L, Turk DC, Marcus DA. The relationship of locus of control and psychosocial behavioral response in chronic headache. Headache. 1995;35(9):527–33. doi:10.1111/j.1526-4610.1995.hed3509527.x.
French DJ, Holroyd KA, Pinell C, Malinoski PT, O’Donnell F, Hill KR. Perceived self efficacy and headache-related disability. Headache. 2000;40(8):647–56. doi:10.1046/j.1526-4610.2000.040008647.x.
Buse D, Silberstein S, Manack A, Papapetropoulos S, Lipton R. Psychiatric comorbidities of episodic and chronic migraine. J Neurol. 2013;260(8):1960–9. doi:10.1007/s00415-012-6725-x.
Sheftell FD, Atlas SJ. Migraine and psychiatric comorbidity: from theory and hypotheses to clinical application. Headache. 2002;42(9):934–44. doi:10.1046/j.15264610.2002.02217.x.
Ligthart L, Gerrits MM, Boomsma DI, Penninx BW. Anxiety and depression are associated with migraine and pain in general: an investigation of the interrelationships. J Pain. 2013;14(4):363–70. doi:10.1016/j.jpain.2012.12.006.
Barlow DH. Unraveling the mysteries of anxiety and its disorders from the perspective of emotion theory. Am Psychol. 2000;55(11):1247–63. doi:10.1037/0003066X.55.11.1247.
Rotter JB. Some problems and misconceptions related to the construct of internal versus external control of reinforcement. J Consult Clin Psychol. 1975;43(1):56–67. doi:10.1037/h0076301.
Holroyd KA, Cottrell CK, O’Donnell FJ, Cordingley GE, Drew JB, Carlson BW, et al. Effect of preventive (beta blocker) treatment, behavioural migraine management, or their combination on outcomes of optimised acute treatment in frequent migraine: randomised controlled trial. BMJ. 2010;341:c4871. doi:10.1136/bmj.c4871.
Holroyd KA, Drew JB, Cottrell CK, Romanek KM, Heh V. Impaired functioning and quality of life in severe migraine: the role of catastrophizing and associated symptoms. Cephalalgia. 2007;27(10):1156–65. doi:10.1111/j.1468-2982.2007.01420.x.
Seng EK, Holroyd KA. Dynamics of changes in self-efficacy and locus of control expectancies in the behavioral and drug treatment of severe migraine. Ann Behav Med. 2010;40(3):235–47. doi:10.1007/s12160-010-9223-3.
Seng EK, Holroyd KA. Psychiatric comorbidity and response to preventative therapy in the treatment of severe migraine trial. Cephalalgia. 2012;32(5):390–400.
Seng EK, Holroyd KA. Behavioral migraine management modifies behavioral and cognitive coping in people with migraine. Headache. 2014;54(9):1470–83.
Minen MT, Seng EK, Holroyd KA. Influence of family psychiatric and headache history on migraine-related health care utilization. Headache. 2014;54(3):485–92.
Penzien DB, Andrasik F, Freidenberg BM, Houle TT, Lake 3rd AE, Lipchik GL, et al. Guidelines for trials of behavioral treatments for recurrent headache. Headache. 2005;45 Suppl 2:S110–32. doi:10.1111/j.1526-4610.2005.4502004.x.
Headache Classification Committee of the International Headache Soceity. Classification and diagnostic criteria for headache disorders, cranial neuralgias and facial pain. Cephalalgia. 1988;8 Suppl 7:1–96.
International Headache Society Classification Subcommittee. The international classification of headache disorders: 2nd edition. Cephalalgia. 2004;24(Suppl 1):9–160.
Jacobson GP, Ramadan NM, Aggarwal SK, Newman CW. The Henry Ford headache disability inventory (HDI). Neurology. 1994;44(5):837–42.
Jhingran P, Osterhaus JT, Miller DW, Lee JT, Kirchdoetfer L. Development and validation of the migraine-specific quality of life questionnaire. Headache. 1998;38(4):295–302. doi:10.1046/j.15264610.1998.3804295.x.
Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988;56(6):893–7. doi:10.1037/0022-006X.56.6.893.
Holm S. A simple sequentially rejective multiple test procedure. Scand J Stat. 1979;6:65–70.
Abdi H. Holm’s sequential Bonferroni procedure. In: Salkind NJ, Dougherty DM, Frey B, editors. Encyclopedia of research design. Thousand Oaks (CA): Sage; 2010. pp. 573–577.
Nicholson RA, Hursey KG, Nash JM. Moderators and mediators of behavioral treatment for headache. Headache. 2005;45:513–9. doi:10.1111/j.1526-4610.2005.05103.x.
Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. Guilford Press; 2013
Hayes AF. Beyond Baron and Kenny: statistical mediation analysis in the new millennium. Commun Monogr. 2009;76(4):408–20. doi:10.1080/03637750903310360.
Smitherman TA, Wells RE, Ford SG. Emerging behavioral treatments for migraine. Curr Pain Headache Rep. 2015;19(4):13. doi:10.1007/s11916-015-0486-z.
Acknowledgments
We would like to acknowledge the contributions of the principal investigator of the TSM trial, Kenneth A. Holroyd, for his invaluable mentorship. We would also like to acknowledge the members of the TSM trial team; Constance Cottrell, Francis O’Donnell, Gary Cordingley, Carol Nogrady, Kimberly Hill, Victor Heh, Suzanne Smith, Bernadette Devantes Heckman, Brenda Pinkerman, Gregg Tkachuk, Sharon Waller, Donna Shiels, Kathleen Darchuk, Yi Chen, Timur Skeini, Manish Singla, Swati Dalmai, Lorie Arnott, and Lina Himawan.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The TSM trial was funded by the National Institute of Neurological Disorders and Stroke (NS-32375; PI Holroyd). Merck Pharmaceuticals, Inc. and GlaxoSmithKline Pharmaceuticals donated triptans for acute migraine therapy, which was their only involvement.
Conflict of Interest
Dr. Seng reports funding from the International Headache Academy. Ms. Grinberg has no conflicts to report.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Grinberg, A.S., Seng, E.K. Headache-Specific Locus of Control and Migraine-Related Quality of Life: Understanding the Role of Anxiety. Int.J. Behav. Med. 24, 136–143 (2017). https://doi.org/10.1007/s12529-016-9587-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12529-016-9587-2