Abstract
Background
Modification of expectancies (headache self-efficacy and headache locus of control) is thought to be central to the success of psychological treatments for migraine.
Purpose
The purpose of this study is to examine expectancy changes with various combinations of Behavioral Migraine Management and migraine drug therapies.
Methods
Frequent migraine sufferers who failed to respond to 5 weeks of optimized acute migraine drug therapy were randomized to a 2 (Behavioral Migraine Management+, Behavioral Migraine Management−) × 2 (β-blocker, placebo) treatment design.
Results
Mixed models for repeated measures analyses (N = 176) revealed large increases in headache self-efficacy and internal headache locus of control and large decreases in chance headache locus of control with Behavioral Migraine Management+ that were maintained over a 12-month evaluation period. Chance headache locus of control and socioeconomic status moderated changes in headache self-efficacy with Behavioral Migraine Management+.
Conclusions
The “deficiency” hypothesis best explained how patient characteristics influenced changes in of headache self-efficacy with Behavioral Migraine Management.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The efficacy of psychological treatments for migraine is reasonably well established [1–5]. However, less is known about changes in theoretically relevant migraine-related beliefs (expectancies) with psychological or non-psychological (e.g., drug) treatments for migraine. Social Cognitive and Learning Theories [6–8], and the broader literature on self-management of chronic disease [9–11], posit that changing disease-specific self-efficacy and locus of control expectancies is a central goal of self-management interventions for chronic diseases [11–15]. However, information is lacking about the impact of Behavioral Migraine Management on these expectancies, including the existence of treatment effects, the time course and maintenance of any observed treatment effects, and participant characteristics that influence treatment effects.
Effects of Behavioral Treatment on Expectancies
Headache self-efficacy refers to confidence in one’s ability to use behavioral skills to prevent and manage recurrent headaches [7, 16]. Increasing headache self-efficacy is one goal of social cognitive and learning-based treatments, and may be essential for the success of these treatments [7, 16], including behavioral treatments for headache [13, 17]. Positive experiences managing headaches using medication might also generalize to all headache management behaviors, thus increasing headache self-efficacy. However, studies with tension-type headache have indicated that electromyographic biofeedback [18, 19] and cognitive-behavioral stress management therapy [17, 20], but not preventative drug therapy, produce large (effect size ≥1) increases in headache self-efficacy.
Less is known about changes in headache self-efficacy occurring with psychological treatments for migraine. By definition, even frequent (episodic) migraine is less pervasive than chronic tension-type headache, but more acutely debilitating, and thus the pattern of treatment effects on psychological variables may differ in these two disorders. The three availableFootnote 1 studies that have examined changes in headache self-efficacy with psychological treatment of migraine have suggested that headache self-efficacy increases substantially with cognitive-behavioral therapy [21, 22] and (thermal) biofeedback for migraine [23]. However, these studies suffered from a number of limitations, including the lack of a control or comparison group that would allow changes in headache self-efficacy to be unequivocally attributed to treatment [21, 23], the failure to report findings separately for participants with migraine and participants with tension-type headache [21, 22], and data from only a small number (N < 25) of patients [21, 23].
While at least some participants in the studies examining psychological treatments for migraine were also receiving migraine drug therapy, the effect of adding psychological treatment to a specifiable drug therapy could not be evaluated in any of the studies mentioned above. The one available study that examined the effect of migraine drug therapy on headache self-efficacy reported moderate (effect size ≈ 0.5) increases in mean headache self-efficacy with preventive drug therapy, and smaller increases (effect size ≈ 0.3) with placebo, although neither the change in headache self-efficacy with treatment, nor the differences between active drug and placebo, were statistically significant [24]. Thus, questions about the impact of psychological or drug treatments for migraine on headache self-efficacy, and the time course and maintenance of any observed treatment effects, remain unanswered.
Headache locus of control refers to the expectation that the onset, course and severity of one’s migraines can be influenced by one’s own actions (internal), by fate/chance (chance), or by the actions of medical providers (medical professionals) [8, 25]. Social Cognitive Theory [6, 7] locates self-efficacy expectancies more proximally to the execution of specific self-management behaviors than outcome (locus of control) expectancies, and designates self-efficacy as a common path for change mechanisms operating across psychological treatments. An individual may believe their behavior is causally related to (or at least influences) their headaches (internal headache locus of control), but completely lack confidence they can either execute the behaviors they believe could ameliorate their headaches, or stop engaging in the behaviors they believe exacerbate their headaches (headache self-efficacy) [6, 7]. In fact, this combination of headache locus of control and headache self-efficacy expectancies is commonly encountered clinically.
Psychological interventions have been postulated to increase internal and reduce chance headache locus of control [26, 27]. To the best of our knowledge, no clear hypothesis has been offered about the effect of psychological treatments on medical professionals headache locus of control. On the other hand, drug therapy, at least when successful, might be expected to decrease chance headache locus of control and increase medical professionals headache locus of control. However, drug therapy also has been postulated to undermine internal headache locus of control [28]. Unfortunately, empirical data bearing on these hypotheses for migraine treatment is lacking. Nicholson and colleagues [21] reported no significant increase in internal headache locus of control with self-administered cognitive-behavioral therapy for headache. Although Mizener and colleagues [23] reported a significant increase in the internality of general health locus of control in 11 patients treated with thermal biofeedback for migraine, more than half the patients had dropped out of treatment, and thus were not included in the analysis. Finally, Cox and colleagues [29] reported a significant increase in the internality of general locus of control in patients receiving electromyographic biofeedback, progressive relaxation, and placebo for chronic tension-type headache. Unfortunately, these three studies also suffered from the methodological limitations already noted in the previous paragraph.
Patient Characteristics
Locus of control is postulated to moderate changes in other outcome variables observed with psychological treatment, particularly self-efficacy [26, 27]. However, the direction of this moderation is in dispute. The competency hypothesis frames advantageous locus of control beliefs (high internal/low chance) as competencies that “prime,” or enable, patients to participate in psychological treatment, allowing these individuals to experience greater gains in self-efficacy during treatment. Some support for this competency hypothesis has been found in the broader psychotherapy literature (e.g., the Treatment of Depression Collaborative Research Program [30]). Clinical wisdom similarly suggests that increasing confidence in one’s ability to use behavioral headache skills is most feasible in individuals who already perceive a relationship between their behavior and their migraines (high internal/low chance headache locus of control). On the other hand, what we have termed the deficiency hypothesis posits the opposite direction to this moderator effect: that is, individuals who begin treatment believing their headaches are influenced primarily by chance or fate, rather than their own behavior (high chance/low internal headache locus of control), will show the largest (rather than the smallest) changes in headache self-efficacy during psychological treatment. This is because these individuals have the most to learn from Behavioral Migraine Management, and thus, have at least the potential to show the greatest change in headache self-efficacy.
Headache severity and migraine-related disability might also be expected to influence headache self-efficacy change observed with psychological treatment [26]. With the experience of more severe and disabling headaches, one’s perceived inability to successfully use behavioral migraine management skills may become less malleable. To our knowledge, no study has examined headache locus of control expectancies or headache-related severity and disability as moderators of changes in headache self-efficacy observed with psychological or drug treatment of headache.
Present Study
The present study uses data from the Treatment of Severe Migraine trial [31, 32] to address the above questions. We examine the time course and maintenance of changes in expectancies associated with different combinations of drug and psychological treatments for migraine. We also examine the postulated moderation of changes in headache self-efficacy by headache locus of control, and the influence of migraine severity and migraine-related disability, as well as demographic characteristics, on any changes in headache self-efficacy observed with treatment. We regard these as exploratory (rather than confirmatory) analyses, both because they are secondary analyses of data from a trial that was designed to address other questions, and because there is either no existing literature, or only a very limited available literature that would allow the formulation of directional hypotheses.
Methods
Treatment of Severe Migraine Trial Overview
The current study is a secondary analysis of data from the Treatment of Severe Migraine trial (Fig. 1). At a pretreatment evaluation, participants received a structured headache interview and psychosocial history, neurological and medication evaluation, and completed measures of expectancies and migraine-related disability. Participants were required to meet International Classification of Headache Disorders diagnosis of migraine with or without aura [33]. All participants then received 5 weeks of Optimized Acute Therapy. Participants who continued to experience frequent migraine (≥3 migraines with disability per 30 days) while on Optimized Acute Therapy alone were stratified by sex and randomized into one of four treatments added onto Optimized Acute Therapy. These treatments are best conceptualized for these analyses as a 2 (Preventive Medication: β-blocker vs. placebo) × 2 (Behavioral Migraine Management: Behavioral Migraine Management+ vs. Behavioral Migraine Management−) factorial design. Project counselors administered Behavioral Migraine Management and project neurologists adjusted β-blocker (or placebo) dose during 4 monthly clinic visits (months 1–4; see Fig. 1). Three phone contacts between treatment visits identified and addressed problems with medication adherence or, in participants receiving Behavioral Migraine Management, problems in learning and applying Behavioral Migraine Management skills. During a 12-month evaluation period, participants returned for five follow-up visits, each of which included a neurologist evaluation and completion of computer-administered expectancy and disability questionnaires. Participants also recorded headache activity and medication use daily for the duration of the trial using an (Palm OS) electronic headache diary. All participants provided written informed consent following procedures approved by the Ohio University Human Subjects Committee.
Optimized Acute Therapy
All participants received Optimized Acute Therapy throughout the study. This was individually tailored drug therapy for the acute treatment of migraine, including a 5-HT1B/D-agonist or triptan, and nonsteroidal anti-inflammatory, anti-emetic, and/or rescue medications as needed. Optimized Acute Therapy also involved education in the effective use of acute migraine medications.
Preventative Medication
Participants randomized to the β-blocker condition received long acting propanolol HCL, or nadolol if propranolol was not well tolerated or ineffective. Participants randomized to the placebo condition received matched β-blocker placebos. This was a double blind protocol, and was continued throughout the study.
Behavioral Migraine Management
Participants randomized to the Behavioral Migraine Management+ condition received limited-contact Behavioral Migraine Management treatment. The Behavioral Migraine Management program [34] is a psychological treatment program based on Social Cognitive Theory. It includes 12 modules, each of which focuses on a different facet of migraine management (Table 1). Migraine management skills were demonstrated during 4 monthly clinic visits and applied between sessions through readings from the Behavioral Migraine Management workbook, audiotape lessons, and guided home practice of behavioral migraine management skills [34]. In the Behavioral Migraine Management+ condition, the three phone calls between sessions addressed problems with behavioral migraine management skills as well as medication management.
Primary Outcomes of the Treatment of Severe Migraine Trial
Primary outcome analyses of the Treatment of Severe Migraine trial revealed clinically significant decreases in migraines and migraine days with all treatment conditions [31, 32]. However, adding the combination of Behavioral Migraine Management and β-blocker to Optimized Acute Therapy yielded significantly larger improvements in migraines, migraine days, and migraine-related impairments in quality of life than was observed with the addition of any of the other three treatments (placebo, β-blocker, or the combination of Behavioral Migraine Management and placebo) to Optimized Acute Therapy.
Measures
Headache Management Self-Efficacy Scale
The Headache Management Self-Efficacy Scale [16] is a self-report, 25-item measure (7-points, ranging from 1 = strongly disagree to 7 = strongly agree), which assesses an individual’s self-efficacy to manage headache pain and prevent headache episodes. Questions include, “I can reduce the intensity of a headache by relaxing,” and “Nothing I do will keep a mild headache from turning into a bad headache (reverse).” It has demonstrated excellent internal consistency, (Cronbach’s α = 0.90) [16]. Support has been provided for the construct validity of the Headache Management Self-Efficacy Scale, including: (1) negative associations with measures of headache severity and disability; (2) a positive association with positive psychological coping; (3) a positive association with Internal headache locus of control; and (4) a negative association with Chance headache locus of control.
Headache Specific Locus of Control
The Headache Specific Locus of Control [25] is a 33-item measure designed to assess the extent to which individuals with recurrent headache expect the occurrence, worsening and improvement of their headaches are influenced primarily by their own behavior, by chance or fate, or by the actions of medical professionals. Items are coded on a 5-point Likert-type scale ranging from “strongly disagree” to “strongly agree.” Items include the following: “My actions influence whether or I have headaches,” (Internal); “My headaches are beyond all control,” (Chance); and “Following the doctor’s medication regimen is the best way for me not to be laid-up with a headache,” (Medical Professionals). Though the Internal subscale is scored so that low scores indicate high internality of control beliefs, it will be reversed for the analyses. Each subscale demonstrated good internal consistency (αs = 0.80–0.89) [25] and adequate 3-week test–retest reliability (rs = 0.72–0.78) [25]. Subscales demonstrated significant expected relationships with related measures. For example, the Chance subscale was related to catastrophizing in response to headaches (r = 0.44), while the Internal subscale was related to a preference for self-regulation treatments (r = 0.21) and the Medical Professionals subscale related to a preference for medical treatment (r = 0.45) [25].
Migraine Specific Quality of Life Questionnaire
The Migraine Specific Quality of Life Questionnaire [35] is a 16-item questionnaire designed to measure migraine-related impairment/quality of life in individuals with migraine. The Migraine Specific Quality of Life Questionnaire can be divided into three subscales: Role Function-Restrictive, Role Function-Preventative, and Emotional Function. Sample items include “In the past 4 weeks, how often have migraines interfered with how well you dealt with family, friends, and others who are close to you?” (Role Function-Restrictive), “In the past 4 weeks, how often have you had to cancel work or daily activities because you had a migraine?” (Role Function-Preventative), and “In the past 4 weeks how often have you felt fed up or frustrated because of your migraines?” (Emotional Function). The subtests demonstrated adequate reliability (αs = 0.79–0.85) and were highly correlated (rs = 0.84–0.89). Regarding validity, all three subscales were significantly related to frequency, severity, and duration of headaches [35].
Demographics
Demographic variables were assessed prior to treatment by questionnaire. Participants answered questions regarding age, gender, and ethnicity. Due to small numbers of participants from the other ethnic groups (n = 7), only self-identified Caucasian and African American participants were used in ethnicity analyses. To construct the socioeconomic status variable, a principal components analysis was conducted using the variables “Number of Years of Education Completed” and “Annual Income.” These two variables are commonly used when creating a composite measure of socioeconomic status [36, 37]. The principal components analysis identified one factor in the analysis (eigenvalue = 1.3) which accounted for 62.7% of the variance in the two measures. Number of Years of Education Completed and Annual Income had equal loadings on the socioeconomic status factor (factor loadings = 0.79). A standard socioeconomic status score (M = 0.0, SD = 1.0) was then calculated for each patient.
Statistical Analyses
Because this study examines the changes in expectancies induced by different treatments, only participants who received treatment, specifically participants who completed the 4 monthly clinic visits during which Behavioral Migraine Management was administered and Preventative Medication dosing was adjusted, and the month 5 assessment, are included in the analyses. ANOVA was used to examine pretreatment differences on continuous variables and Chi-Square for categorical variables.
2 (Behavioral Migraine Management+ vs. Behavioral Migraine Management−) × 2 (β-blocker vs. placebo) mixed models for repeated measures analyses were used to evaluate treatment-related changes in expectancies and moderation of change in the Headache Management Self-Efficacy Scale by selected participant characteristics. A first-order autoregressive covariance matrix best explained the variance in expectancies according to Akaike’s Information Criterion. Time was modeled using log10 because expectancy change was expected to be curvilinear. Predictor variables and all their interactions were entered in the first step and, for the final model, removed in consecutive steps until all entered variables were significant or used in a higher-order interaction. The Headache Management Self-Efficacy Scale and each of the Headache Specific Locus of Control subscales served as outcome variables in separate mixed models analyses. Behavioral Migraine Management, Preventative Medication, and Time served as fixed effects. A significant interaction between a treatment variable (Behavioral Migraine Management or Preventative Medication) and Time would indicate differential expectancy change between the treatment conditions. Significant interactions were followed-up by within-condition mixed models for repeated measures analyses to examine within-condition expectancy changes. Within-condition effect sizes (Cohen’s d) were computed from pretreatment to month 5. All significance tests were two-tailed.
Mixed model analysis is preferable to last observation carry forward for the estimation of missing values, because last observation carry forward yields unbiased parameter estimates only under the restrictive, missing completely at random assumption: missing observations are unrelated to both the observed (prior to dropout) and the unobserved (following dropout) outcome measure values. Moreover, the direction of bias when the missing completely at random assumption is violated is not easy to predict. In contrast, mixed model analysis, which uses all available data to estimate missing values, can yield unbiased parameter estimates when missing observations are related to observed (but not unobserved) outcome values (missing at random), and performs surprising well even on simulated clinical trial data that includes both missing at random observations and observations missing not at random [38–44].
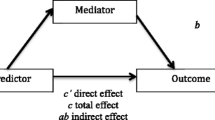
Moderator analyses examined whether patient characteristics (pretreatment Headache Specific Locus of Control subscales, pretreatment migraine severity and disability, and demographic characteristics) moderated the effects of treatment on the Headache Management Self-Efficacy Scale. The Headache Management Self-Efficacy Scale served as the outcome variable. Time, any significant treatment effect (Behavioral Migraine Management or Preventative Medication) identified in the previous analysis, and each participant characteristic (potential moderator variable), served as the fixed effects in separate analysis for each of the potential moderator variables. A significant three-way interaction between the potential Moderator variable, Treatment Condition, and Time would indicate that observed change in the Headache Management Self-Efficacy Scale over time varied with both the Treatment Condition and the Moderator variable.
Results
Participants
Two hundred thirty-two migraine sufferers were randomized into the treatment conditions [2 (Behavioral Migraine Management+ vs. Behavioral Migraine Management−) × 2 (β-blocker vs. placebo)]. Fifty-six participants dropped out by month 5 (leaving 176 participants) and an additional 58 dropped out of the study between months 5 and 16 (leaving 118 participants). Dropout rates did not differ across conditions at either months 5 or 16, and participants who dropped out did not differ on the Headache Specific Locus of Control subscales or Headache Management Self-Efficacy Scale from participants who did not dropout at either time point, all ps > 0.20. The 176 migraine sufferers that completed the month 5 evaluation (described in Table 2) were included in the analyses. Treatment conditions did not differ on any study variables prior to treatment.
Effects of Treatment
In general, Headache Management Self-Efficacy Scale scores and Internal Headache Specific Locus of Control scores increased, and Chance Headache Specific Locus of Control scores decreased during treatment (means and standard deviations presented in Table 3). Greater changes were observed in the Behavioral Migraine Management+ condition than in the Behavioral Migraine Management− condition, with changes with Behavioral Migraine Management occurring early in treatment and maintained through month 16 (see Figs. 2, 3, and 4). In contrast, no clinically meaningful differences between β-blocker and placebo were observed.
Expected changes in Chance Headache Specific Locus of Control by Behavioral Migraine Management and Preventative Medication treatment conditions. Month 0–1 Optimized Acute Therapy, months 1–5 Behavioral Migraine Management and dose adjustment, months 5–16 evaluation period, BMM Behavioral Migraine Management
For the Headache Management Self-Efficacy Scale, a significant Time effect, F(1, 1,074) = 287.5, p < 0.001, was qualified by a Behavioral Migraine Management × Time interaction, F(1, 1074) = 92.0, p < 0.001. Observed increases on the Headache Management Self-Efficacy Scale were more rapid and larger in the Behavioral Migraine Management+ condition than in the Behavioral Migraine Management− condition (Fig. 2). Within-condition analyses revealed large increases in Headache Management Self-Efficacy Scale scores in the Behavioral Migraine Management+ condition, t(550) = 16.8, p < 0.001, d = 1.50, and small to medium increases in Headache Management Self-Efficacy Scale scores in the Behavioral Migraine Management− condition, t(524) = 6.2, p < 0.001, d = 0.43.
Likewise for the Internal Headache Specific Locus of Control subscale, a significant main effect of Time, F(1, 1,075) = 84.9, p < 0.001, was qualified by a Behavioral Migraine Management × Time interaction, F(1, 1,075) = 37.0, p < 0.001. Observed increases in Internal Headache Specific Locus of Control scores were more rapid and larger in the Behavioral Migraine Management+ condition than in the Behavioral Migraine Management− condition (Fig. 3). Within-condition analyses revealed large increases in Internal Headache Specific Locus of Control scores in the Behavioral Migraine Management+ condition, t(551) = 10.2, p < 0.001, d = 0.88; in contrast, increases in Internal Headache Specific Locus of Control scores in the Behavioral Migraine Management− condition at month 5 were statistically significant, but too small to be clinically meaningful, t(524) = 2.5, p < 0.05, d = 0.09.
For the Chance Headache Specific Locus of Control subscale, both two-way interactions were significant, Behavioral Migraine Management × Time, F(1, 1,073) = 10.2, p < 0.01, Preventative Medication × Time, F(1, 1,073) = 6.0, p < 0.05, qualifying the main effects of Behavioral Migraine Management, F(1, 1,073) = 4.5, p < 0.05, and Time, F(1, 1,073) = 29.6, p < 0.001 (Fig. 4). For the Behavioral Migraine Management × Time interaction, within-condition analyses revealed large decreases in Chance Headache Specific Locus of Control scores in the Behavioral Migraine Management+ condition, t(551) = −8.5, p < 0.001, d = 1.13, but substantially smaller decreases in Chance Headache Specific Locus of Control subscale scores in the Behavioral Migraine Management− condition, t(524) = −3.1, p < 0.01, d = 0.38 (Fig. 4a). However, for the Preventative Medication × Time interaction, within-condition analyses revealed no clinically meaningful difference between β-blocker, t(547) = −7.2, p < 0.001, d = 0.75, and placebo, t(528) = −5.1, p < 0.001 d = 0.71, effects (Fig. 4b).
In contrast to the pattern of results reported above, increases in Medical Professionals Headache Specific Locus of Control scores were only observed in the Behavioral Migraine Management− condition (Fig. 5). A Behavioral Migraine Management × Time interaction, F(1, 1,075) = 8.2, p < 0.01 qualified a significant Time effect, F(1, 1,075) = 10.9, p < 0.01. Within-condition analyses demonstrated small to moderate increases in Medical Professionals Headache Specific Locus of Control scores at month 5 in the Behavioral Migraine Management− condition, t(524) = 4.2, p < 0.001, d = 0.30. In contrast, no change was observed in the Behavioral Migraine Management+ condition, t(551) = 0.3, p > 0.20.
Moderation of Treatment Effects on Headache Management Self-Efficacy
Prior to examination of the moderation hypotheses, correlations among pretreatment Headache Management Self-Efficacy Scale scores and potential moderator variables were examined (Table 4). As expected, higher pretreatment Chance Headache Specific Locus of Control scores were strongly associated with lower pretreatment Headache Management Self-Efficacy Scale scores. Although no other correlations exceeded 0.30, the positive correlation between pretreatment Internal Headache Specific Locus of Control and Headache Management Self-Efficacy Scale scores approached 0.30. Also, socioeconomic status was positively associated, and pretreatment migraine-related disability negatively associated, with pretreatment Headache Management Self-Efficacy Scale scores.
Pretreatment scores on the Chance Headache Specific Locus of Control subscale moderated the Behavioral Migraine Management treatment effect on the Headache Management Self-Efficacy Scale, indicating that the relationship between pretreatment chance headache locus of control and headache self-efficacy changes differed by Behavioral Migraine Management treatment condition, Pretreatment Chance Headache Specific Locus of Control × Behavioral Migraine Management × Time F(1, 1,067) = 6.0, p < 0.05. The pattern of results supported the deficiency (rather than the competency) hypothesis of moderation. Consistent with the correlation presented in Table 4, participants with highFootnote 2 Chance Headache Specific Locus of Control scores exhibited substantially lower Headache Management Self-Efficacy Scale scores than participants with low Chance Headache Specific Locus of Control scores at pretreatment, F(1, 173) = 119.2, p < 0.001. However, in the Behavioral Migraine Management+ condition, participants with high pretreatment Chance Headache Specific Locus of Control scores exhibited larger increases in Headache Management Self-Efficacy Scale scores than participants with low pretreatment Chance Headache Specific Locus of Control subscale scores (Fig. 6). In contrast, in the Behavioral Migraine Management− condition, change in Headache Management Self-Efficacy Scale scores was unrelated to pretreatment Chance Headache Specific Locus of Control. Thus, high pretreatment Chance Headache Specific Locus of Control scores did not handicap individuals receiving Behavioral Migraine Management. For participants in the Behavioral Migraine Management+ condition, the relationship between Headache Management Self-Efficacy Scale scores and pretreatment Change Headache Specific Locus of Control scores was eliminated by month 16, F(1, 59) = 2.7, p > 0.05. For participants in the Behavioral Migraine Management− condition, this relationship was still evident at month 16, F(1, 53) = 16.7, p < 0.001.
Chance Headache Specific Locus of Control moderates the Behavioral Migraine Management treatment effect on Headache Management Self-Efficacy Expected Headache Management Self-Efficacy values with pretreatment Chance Headache Specific Locus of Control set at 1 standard deviation above the mean (a) and 1 standard deviation below the mean (b). Month 0–1 Optimized Acute Therapy, months 1–5 Behavioral Migraine Management and dose adjustment, months 5–16 evaluation period, BMM Behavioral Migraine Management, HSLC Headache Specific Locus of Control
Internal Headache Specific Locus of Control did not moderate the Behavioral Migraine Management effect on the Headache Management Self-Efficacy Scale, F(1, 1,066) = 2.2, p > 0.05. Nonetheless, within-condition analyses revealed a significant Pretreatment Internal Headache Specific Locus of Control × Time interaction in the Behavioral Migraine Management+ condition, F(1, 544) = 7.0, p < 0.01, but not in the Behavioral Migraine Management− condition, F(1, 523) = 2.2, p > 0.05. Individuals with low Internal Headache Specific Locus of Control began treatment with lower Headache Management Self-Efficacy Scale scores than individuals with high Internal Headache Specific Locus of Control (Table 4); however, in the Behavioral Migraine Management+ condition, individuals with low pretreatment Internal Headache Specific Locus of Control exhibited larger increases in Headache Management Self-Efficacy Scale scores during treatment.
Similarly, although socioeconomic status did not moderate the Behavioral Migraine Management treatment effect on the Headache Management Self-Efficacy Scale, F(1, 1,000) = 2.72, p > 0.05, within-condition analyses revealed a significant Socioeconomic Status × Time interaction in the Behavioral Migraine Management+ condition, F(1, 508) = 8.3, p < 0.01, but not in the Behavioral Migraine Management− condition, F(1, 493) = 2.0, p > 0.05. Although individuals with low socioeconomic status began treatment with lower Headache Management Self-Efficacy Scale scores (Table 4), in the Behavioral Migraine Management+ condition, individuals with low socioeconomic status exhibited larger increases in Headache Management Self-Efficacy Scale scores during treatment than individuals with high socioeconomic status.
Pretreatment Medical Professionals Headache Specific Locus of Control did not moderate or influence changes in the Headache Management Self-Efficacy Scale, F(1, 1,066) = 0.1, p > 0.05. Pretreatment migraine severity (migraine days), quality of life, and demographic characteristics other than socioeconomic status (i.e., age, gender, and ethnicity), did not moderate or otherwise influence changes in Headache Management Self-Efficacy Scale scores, ps > 0.05.
Discussion
Treatment Effects
Our findings provide new information about patterns of changes in headache-related expectancies with psychological treatment for migraine, the impact of non-psychological migraine treatment (drug therapy) on headache self-efficacy and headache locus of control expectancies, and patient characteristics that influence changes in headache self-efficacy with treatment. First, the addition of Behavioral Migraine Management to migraine drug therapy dramatically increased participants’ confidence in their ability to effectively self-manage migraine (headache self-efficacy), compared to migraine drug therapy alone. Behavioral Migraine Management also increased the belief that migraines can be influenced by one’s own behavior (internal headache locus of control) and decreased the belief that migraines are primarily influenced by chance or fate (chance headache locus of control). Large expectancy changes with Behavioral Migraine Management were evident early in treatment and were maintained throughout the 12-month evaluation period (Behavioral Migraine Management+ effect sizes > 1). Moreover, Behavioral Migraine Management increased both headache self-efficacy and internal headache locus of control, and decreased chance headache locus of control, when compared to an active, but non-psychological treatment (migraine drug therapy), indicating that this effect is specific to psychological treatment, rather than to treatment in general. Finally, similar but notably smaller increases in headache self-efficacy and reductions in chance headache locus of control were observed with migraine drug therapy alone (Behavioral Migraine Management− effect sizes ≈ 0.40). The fact that no clinically meaningful differences in expectancies were observed between Preventative Medication conditions (β-blocker and placebo) suggests that the observed effects of migraine drug therapy were related to the psychological experience of taking medication, rather than the pharmacological effects of the drug. The impact of psychological and preventive drug treatments on headache self-efficacy observed in the current study corresponds with results reported in the few previous studies which also examined changes in headache self-efficacy with migraine treatment, each of which used different treatments and research designs [21, 22, 24]. In contrast to a previous study which found no effect of self-administered cognitive-behavioral therapy on internal headache locus of control [21], the current study found a large, significant increase in internal headache locus of control with Behavioral Migraine Management. Differences in treatments, particularly the use of a completely self-administered treatment format, or differences in patient populations might account for differences in findings in these two studies.
Our findings also provide some reassurance regarding the concern that drug therapy, by encouraging recipients to attribute improvement to the actions of a medication, undermines internal locus of control, confidence in one’s ability to use behavioral strategies to manage symptoms (i.e., self-efficacy), and involvement in psychological treatment [28]. We found no evidence that migraine drug therapy alone undermined perceptions of internal headache locus of control or headache self-efficacy, or that, when combined with Behavioral Migraine Management, migraine drug therapy undermined expectancy changes induced by Behavioral Migraine Management. For headache self-efficacy, our results are consistent with the single previous report of a moderate (d = −0.53) effect of migraine drug therapy on headache self-efficacy [24].
Results for medical professionals headache locus of control provide additional support for this conclusion. In contrast to the findings with other expectancies, migraine drug therapy alone, but not migraine drug therapy in combination with Behavioral Migraine Management, was associated with increases in medical professionals headache locus of control. However, the increase in medical professionals headache locus of control with migraine drug therapy alone was not accompanied by a corresponding reduction in internal headache locus of control that would suggest drug therapy fostered an unrealistic overdependence on medical professionals. Overall, the moderate elevations in medical professionals headache locus of control observed in all treatment conditions are consistent with a collaborative patient–physician relationship.
Participant Characteristics Influence the Behavioral Migraine Management Treatment Effect on Headache Self-Efficacy
We also examined two competing hypotheses regarding the moderation of changes observed in headache self-efficacy with treatment by headache locus of control. The competency hypothesis posits that individuals with headache locus of control beliefs that are compatible with Behavioral Migraine Management (high internal/low chance) will show the greatest gains in headache self-efficacy with Behavioral Migraine Management. The deficiency hypothesis posits just the opposite: that is, individuals who begin treatment with headache locus of control beliefs that are not compatible with Behavioral Migraine Management, believing that their headaches are primarily influenced by chance or fate, rather than their own behavior, will show the greatest (rather than the least) change in headache self-efficacy.
Our results provided no support for the competency hypothesis, but instead, were consistent with the deficiency hypothesis: higher pretreatment chance headache locus of control was associated with larger (rather than smaller) changes in headache self-efficacy with Behavioral Migraine Management. This effect was not observed with migraine drug therapy alone. Thus, Behavioral Migraine Management effectively increased headache self-efficacy, even for participants who began treatment believing their headaches were determined primarily by factors outside of their control (higher chance headache locus of control). In fact, participants who received Behavioral Migraine Management, on average, achieved the same high levels of headache self-efficacy following Behavioral Migraine Management, irrespective their pretreatment chance headache locus of control scores. This occurred because participants with higher chance headache locus of control scores (and lower headache self-efficacy scores) at pretreatment showed the largest changes in headache self-efficacy with Behavioral Migraine Management, and thus “caught up” with participants who began treatment with lower chance headache locus of control scores (and higher headache self-efficacy scores).
Examination of the influence of pretreatment internal headache locus of control on the Behavioral Migraine Management treatment effect provided additional support for the deficiency hypothesis. Although no formal moderator effect was detected, for participants who received Behavioral Migraine Management, low pretreatment internal headache locus of control scores were associated with the greatest changes in headache self-efficacy, indicating that participants who began treatment believing that their behavior had little effect on their migraines showed the largest changes in headache self-efficacy with Behavioral Migraine Management. This effect was not observed in participants who received migraine drug therapy alone.
Despite the consistent support for the deficiency hypothesis, the results above might be best characterized as supporting a modified deficiency hypothesis. This is because one of the initial clinical goals of Behavioral Migraine Management is modifying headache locus of control beliefs that are not compatible with Behavioral Migraine Management. This goal is achieved through education about the ways behavioral migraine management skills influence migraines [34, 45]. Therefore, it is not surprising that decreases in chance headache locus of control and increases in internal headache locus of control were observed early in the course of Behavioral Migraine Management (Figs. 3 and 4a). Consequently, the large increases in headache self-efficacy that were observed with Behavioral Migraine Management in individuals with high pretreatment chance and low pretreatment internal headache locus of control scores may have been dependent on modifying these maladaptive chance and internal headache locus of control expectancies (“deficiencies”) early in treatment. Studies that conduct a more fine-grained analysis of the relationship between changes in headache self-efficacy and headache locus of control expectancies, and the timing of these changes throughout treatment, would be necessary to shed further light on this possibility.
If low socioeconomic status is conceptualized as a barrier to effective treatment [46, 47] (or as a participant “deficiency”), our findings with socioeconomic status are consistent with results supporting the deficiency hypothesis evident in our other analyses. While participants with lower socioeconomic status began treatment with lower headache self-efficacy, they exhibited larger increases in headache self-efficacy with Behavioral Migraine Management than did participants with higher socioeconomic status. This effect was not observed with migraine drug therapy alone. Thus, socioeconomic status did not influence the large changes in headache self-efficacy that were observed with Behavioral Migraine Management.
Contrary to some predictions, individuals with more severe and disabling headache problems, and individuals with less severe and disabling headache problems, showed similar changes in their confidence in their ability to effectively self-manage migraines, with both migraine drug therapy alone, and with the combination of migraine drug therapy and Behavioral Migraine Management.
Study Limitations
In our additive treatment design, all participants received at least an active acute drug therapy for migraine. Ethical concerns regarding the potentially detrimental physical and psychological effects of untreated frequent, severe migraines prevented the inclusion of a condition that received no active acute or preventive therapy [48]. In the absence of an untreated control condition, we cannot unambiguously attribute changes in expectancies observed in the Behavioral Migraine Management− condition to migraine drug therapy alone. On the other hand, our additive design allowed us to examine the effects of two well-specified drug therapy regimens on expectancies, both alone and when combined with Behavioral Migraine Management. This complements existing work on the psychological treatment of migraine, which were unable to examine the possible effects of drug therapy regimens on expectancies [21, 22].
All participants experienced frequent disabling migraines so it is unclear to what extent these results generalize to individuals with less frequent and severe migraines. However, for patients with frequent migraines with disability, both clinical textbooks on headache [46, 49] and clinical guidelines [5, 50–52] recommend treatment include both acute and preventive medication. Thus, our results should be relevant to evidence-based practice with this important population of migraine sufferers. Our ability to detect a moderator effect for migraine severity or disability may also have been limited by the restricted range of pretreatment migraine severity and disability in trial participants. However, other pretreatment variables which were shown to influence headache self-efficacy change, namely the Headache Specific Locus of Control subscales, would also be expected to show a more restricted range than in this population of individuals with frequent disabling migraine, arguing against this interpretation. Of course, the results from the current study may not generalize to other headache disorders, for example, chronic tension-type headache, though this has yet to be examined.
Participant dropout is inherent in the conduct of clinical trials. On the other hand, dropout rates in this trial (16 months in length)Footnote 3 were notably lower than those observed in other recent preventative migraine medication trials (typically 6 months in length or less) [53–55]. Moreover, mixed models analyses provide unbiased estimates of missing values under relatively unrestrictive conditions.
It also should be noted that the Headache Management Self-Efficacy Scale was designed to assess confidence in the use of behavioral headache management skills [16]. If self-efficacy expectancies specifically for the effective use of migraine drug therapy were assessed, drug therapy alone may have had a larger impact on this narrower self-efficacy variable. However, we would predict that Behavioral Migraine Management would also increase this medication self-efficacy variable.
Conclusion
Our results provide new information about the ability of psychological treatment of migraine disorder to influence expectancies. Results offer an optimistic message: Behavioral Migraine Management effectively increased headache self-efficacy and internal headache locus of control, and decreased chance headache locus of control. Thus, effective psychological treatment of migraines appears to include changes in these theoretically relevant expectancies. Expectancy changes were not undermined by concurrent drug therapy, indicating that psychological and drug therapies can be used additively with no detrimental effects on critical psychological variables. Expectancy changes were maintained for at least 1 year, indicating the long-lasting effects of a brief (four session) psychological intervention for migraine management. This effect is particularly notable given that Behavioral Migraine Management ended prior to the evaluation phase while drug therapy was continued throughout the 12 months of the evaluation phase.
Large changes in headache self-efficacy were also observed in individuals who, because of beliefs that their disorder could not be influenced by their behavior, are sometimes thought to be relatively poor candidates for psychological treatment. Our findings suggest that many of these individuals can make effective use of psychological treatments for migraine, at least when modifiable barriers to treatment are systematically challenged, as is the case in the Behavioral Migraine Management protocol. In the first Behavioral Migraine Management session, prior to teaching behavioral migraine management skills, an orientation to treatment demonstrates how behavioral migraine management skills address both the biological and environmental factors that influence the occurrence and course of migraines (Table 1) [34, 45]. This orientation to treatment, which is further reinforced in the participant’s treatment manual, is designed to challenge problematic headache-related beliefs (e.g., chance headache locus of control) that can impact the perceived relevance of psychological treatment, and thus performance of behavioral migraine management skills. Many individuals who believe their behavior has little or no influence on the occurrence, severity, and course of migraines may thus be good candidates for psychological treatment, if these problematic beliefs are effectively challenged prior to teaching behavioral migraine management skills.
Notes
Studies that experimentally manipulate “perceived success” and/or other treatment elements (physiological learning) may provide information about change mechanisms, but have experimentally altered clinical treatment, and thus fail to provide information about changes in expectancies that occur when treatment is administered in the clinical setting [56–58].
All variables examined in the moderator analyses, other than ethnicity, are continuous variables. However, the terms “high” and “low” are used for readability.
The most recent clinical trials of preventative migraine medication tend to report dropout rates of 50% at 6 months. In contrast, the Treatment of Severe Migraine trial has a dropout rate of 35% at 10 months. Thus, crudely averaged over months, the dropout rate for the Treatment of Severe Migraine trial (≈3.5% per month) was less than half of the comparative dropout rate for other recent preventative medication trials (≈8% per month). Another way to compare dropouts across trials is to note that the dropout rate for the Treatment of Severe Migraine trial at 16 months is similar to the dropout rate for other recent trials at 6 months.
References
Nestoriuc Y, Martin A: Efficacy of biofeedback for migraine: A meta-analysis. Pain. 2007, 128:111–127.
Penzien D, Rains J, Andrasik F: Behavioral management of recurrent headache: Three decades of experience and empiricism. Appl Psychophysiol Biofeedback. 2002, 27:163–181.
Campbell J, Penzien D, Wall E: Evidence-based guidelines for migraine headache: Behavioral and physical treatments. American Academy of Neurology Guidelines 2000. Retrieved May 03, 2010, from www.aan.com/professionals/practice/pdfs/gl0089.pdf
Holroyd K, Penzien D: Pharmacological vs. nonpharmacological prophylaxis of recurrent migraine headache: A meta-analytic review of clinical trials. Pain. 1990, 42:1–13.
Silberstein S: Practice Parameter: Evidence-based guidelines for migraine headache (an evidence-based review). Neurology. 2000, 55:754–762.
Bandura A: Self-efficacy: Toward a unifying theory of behavioral change. Psychol Rev. 1977, 84:191–215.
Bandura A: Self-efficacy: The exercise of control. New York: W.H. Freeman, 1997.
Rotter JB: Generalized expectancies for internal versus external control of reinforcement. Psychol Monogr. 1966, 80:1–28.
Bodenheimer T, Lorig K, Holman H, Grumbach K: Patient self management of chronic disease in primary care. JAMA. 2002, 288:2469–2475.
Marks R, Allegrante J, Lorig K: A review and synthesis of research evidence for self-efficacy-enhancing interventions for reducing chronic disability: Implications for health education practice. Health Promote Pract. 2005, 6:37–43.
Tobin D, Reynolds R, Holroyd K, Creer T: Self-management and social learning theory. In K. Holroyd and T. Creer (eds), Self-management of chronic disease: Handbook of clinical interventions and research. New York: Academic Press, 1986.
Rains J, Penzien D, Lipchik G: Behavioral facilitation of medical treatment for headache part II: Theoretical models and behavioral strategies for improving adherence. Headache. 2006, 46:1395–1403.
Nicholson RA, Hursey RG, Nash JM: Moderators and mediators of behavioral treatment for headache. Headache. 2005, 45:513–519.
Holroyd K, Penzien D, Rains J, Lipchik G, Buse D: Behavioral management of headaches. In S. Silberstein, R. Lipton and D. Dodick (eds), Wolff's Headache and Other Head Pain. New York, NY: Oxford University Press, 2008, 721–746.
Holroyd K, Martin P: Psychological treatments for tension-type headache. In J. Olesen, P. Tfelt-Hansen and K. Welch (eds), The headaches. Philadelphia: Lippincott Williams & Wilkins, 2000, 643–649.
French DJ, Holroyd KA, Pinnell C, et al.: Perceived self-efficacy and headache-related disability. Headache. 2000, 40:647–656.
Holroyd KA, Labus J, Carlson BW: Moderation and mediation in the psychological and drug treatment of chronic tension-type headache: The role of disorder severity and psychiatric comorbidity. Pain. 2009, 143:213–222.
Rokicki LA, Holroyd KA, France CR, et al.: Change mechanisms associated with combined relaxation/EMG biofeedback training for chronic tension headache. Appl Psychophysiol Biofeedback. 1997, 22:21–41.
Nestoriuc Y, Rief W, Martin A: Meta-analysis of biofeedback for tension-type headache: Efficacy, specificity, and treatment moderators. J Consult Clin Psychol. 2008, 76:379–396.
Holroyd KA, Malinoski PT, Carlson BW: Patient characteristics and treatment adherence predict response to antidepressant medication and to cognitive-behavior therapy for chronic tension-type headache. Ann. Behav. Med. 2002, 24:S050.
Nicholson R, Nash J, Andrasik: A self-administered behavioral intervention using tailored messages for migraine. Headache. 2005, 45:1124–1139.
Thorn BE, Pence LB, Ward LC, et al.: A randomized clinical trial of targeted cognitive behavioral treatment to reduce catastrophizing in chronic headache sufferers. J Pain. 2007, 8:938–949.
Mizener D, Thomas M, Billings R: Cognitive changes of migraineurs receiving biofeedback training. Headache. 1988, 28:339–343.
Lee S, Park J, Kim M: Efficacy of the 5-HT1A agonist, buspirone hydrochloride, in migraineurs with anxiety: A randomized, prospective, parallel group, double-blind, placebo-controlled study. Headache. 2005, 45:7.
Martin NJ, Holroyd KA, Penzien DB: The headache-specific locus of control scale: Adaptation to recurrent headaches. Headache. 1990, 30:729–734.
Wallston KA: The Validity of the Multidimensional Health Locus of Control Scales. J Health Psychol. 2005, 10:623–631.
Nicholson RA, Houle TT, Rhudy JL, Norton PJ: Psychological Risk Factors in Headache. Headache. 2007, 47:413–426.
Hollon SD, DeRubeis J: Placebo-psychotherapy combinations: Inappropriate representations of psychotherapy in drug-psychotherapy comparative trials. Psychol Bull. 1981, 90:467–477.
Cox DJ, Freundlich, A., Meyer, R.G.: Differential effectiveness of electromyograph feedback, verbal relaxation instructions, and medication placebo with tension headaches. J Consult Clin Psychol. 1975, 43:892–898.
Sotsky SM, Glass DR, Shea MT, Pilkonis PA, et al.: Patient predictors of response to psychotherapy and pharmacotherapy: Findings in the NIMH Treatment of Depression Collaborative Research Program. Am J Psychiatry. 1991, 148:997–1008.
Holroyd K, Cottrell C, O'Donnell F, et al.: Does Preventive (Beta Blocker) Medication, Behavioral Migraine Management or Their Combination Improve Outcomes of Optimal Acute Therapy in Frequent Migraine: A Randomized Trial. Submitted.
Holroyd K, Cottrell C, O'Donnell F, et al.: Does preventive medication, behavioral migraine management or their combination add to optimal acute therapy in the management of frequent migraines: The TSM trial. Headache. 2006, 46:835.
Headache Classification Committee of the International Headache Society: Classification and diagnostic criteria for headache disorders, cranial neuralgias and facial pain. Cephalalgia. 1988, 8:1–96.
Holroyd K, Cottrell C, Echelberger-McCune R: Behavioral management for migraine headaches: A treatment program. Athens, OH: Ohio University Headache Treatment and Research Project, 2000.
Jhingran P, Osterhouse JT, Miller DW, Lee JT, Kirchdoerfer L: Development and validation of the migraine-specific quality of life questionnaire. Headache. 1998, 38:295–302.
Heckman BD, Holroyd KA, Tietjen G, et al.: Whites and African-Americans in headache specialty clinics respond equally well to treatment. Headache. 2009, 29:650–661.
Williams DR, Collins C: US socioeconomic and racial differences in health: Patterns and explanations Annu Rev Sociol. 1995, 21:349.
Leon AM, CH, Chuang-Stein C, Archibald D, Archer G, Chartier K: Attrition in randomized controlled clinical trials: Methodological issues in pyschopharmacology. Biol Psychiatry. 2006, 59:1001–1005.
Mallinckrodt C, Clark W, David S: Accounting for dropout bias using mixed-effects models. J Biopharm Stat. 2001, 11:9–21.
Mallinckrodt C, Clark W, David S: Type I error rates from mixed-effects model repeated measures versus fixed effects ANOVA with missing values imputed via last observation carried forward. Drug Inf J. 2001, 35:1215–1225.
Mallinckrodt C, Sanger T, Dube S, et al.: Assessing treatment effects in longitudinal data. Biol Psychiatry. 2003, 53:754–760.
Molenberghs G, Thijs H, Jansen I, Beunckens C: Analyzing incomplete longitudinal clinical trial data. Biostatistics. 2004, 5:445–464.
Barnes S, Mallinckrodt C, Lindborg S, Carter M: The impact of missing data and how it is handled on the rate of false-positive results in drug development. Pharm Statist. 2008, 7:215–225.
Gadbury G, Coffey C, Allison D: Modern statistical methods for handling missing data. Obes Rev. 2003, 4:175–184.
Lipchik G, Holroyd K, Nash J: Cognitive-behavioral management of recurrent headache disorders: A minimal-therapist contact approach. In D. Turk and R. Gatchel (eds), Psychological Approaches to Pain Management. New York, NY: Guilford Press, 2002, 356–389.
Lipton R, Bigal M, Diamond M, et al.: Migraine prevalence, disease burden, and the need for preventive therapy. Neurology. 2007, 68:343–349.
Link BG, Phelan J: Social conditions as fundamental causes of disease. J Health Soc Behav. 1995, Spec No:80–94.
Brandes J: The migraine cycle: Patient burden of migraine during and between migraine attacks. Headache. 2008, 48:430–441.
Silberstein S, Freitag F, Bigal M: Migraine treatment. In S. Silberstein, R. Lipton and D. Dodick (eds), Wolff's Headache and Other Head Pain. London: Oxford University Press, 2008, 177–292.
Ramadan N, Silberstein S, Freitag F, Gilbert T, Frishberg B: Evidence-based guidelines for migraine headache in the primary care setting: Pharmacological management for the prevention of migraine. American Academy of Neurology Guidelines 2002. Retrieved Accessed May 03 2010, from http://www.aan.com/professionals/practice/pdfs/gl0090.pdf
Steiner T, Paemeiere K, Jensen RV, D, et al.: European principles of management of common headache disorders in primary care. J Headache Pain. 2007, 8 S3–47.
pt?>Kaniecki RL, S: Treatment of primary headache: Preventive treatment of migraine. Standards of care for headache diagnosis and treatment. Chicago: National Headache Foundation, 2004, 40–52.
Brandes J, Saper J, Diamond M, et al.: Topiramate for migraine prevention. JAMA. 2004, 291:965–973.
Silberstein S, Neto W, Schmitt J, Jacobs D: Topiramate in migraine prevention: Results of a large controlled trial. Arch Neurol. 2004, 61:490–495.
Diener H-C, Tfelt-Hansen P, Dahlof C, et al.: Topiramate in migraine prophylaxis: Results from a placebo-controlled trial with propranolol as an active control. J Neurol. 2004, 251:943–950.
French DJ, Gauthier JG, Roberge C, Nouwen A: Self-efficacy in the thermal biofeedback treatment of migraine sufferers. Beh Ther. 1997, 28:109–125.
Holroyd KA, Penzien DB, Hursey K, et al.: Change mechanisms in EMG biofeedback training: Cognitive changes underlying improvements in tension headache. J Consult Clin Psychol. 1984, 52:1039–1053.
Blanchard EB, Kim M, Hermann C, et al.: The role of perception of success in the thermal biofeedback treatment of vascular headache. Headache Q. 1994, 5:231–236.
Acknowledgments
We would like to thank the following people for their assistance in carrying out the TSM trial: Constance Cottrell, Francis O’Donnell, Gary Cordingley, Carol Nogrady, Kimberly Hill, Victor Heh, Suzanne Smith, Bernadette Devantes Heckman, Brenda Pinkerman, Gregg Tkachuk, Sharon Waller, Donna Shiels, Kathleen Darchuk, Yi Chen, Timur Skeini, Manish Singla, Swati Dalmai, Lori Arnott, and Lina Himawan. Support for this trial was provided by grant NS-32374 (awarded to Dr. Holroyd) from the National Institutes of Health. Merck Pharmaceuticals, Inc and GlaxoSmithKline Pharmaceuticals donated triptans (5-HT1B/D-agonists) for acute migraine therapy, which was their only involvement.
Conflict of Interest Statement
Ms. Seng reports no conflicts of interest. Dr. Holroyd has received support from the National Institutes of Health (NINDS; NS32375), has consulted for ENDO Pharmaceuticals and Takeda Pharmaceuticals North America, and received an investigator initiated grant from ENDO Pharmaceuticals.
Author information
Authors and Affiliations
Corresponding author
Additional information
Dr. Holroyd has full control of all primary data from the TSM trial. All analyses were conducted by Ms Seng.
About this article
Cite this article
Seng, E.K., Holroyd, K.A. Dynamics of Changes in Self-Efficacy and Locus of Control Expectancies in the Behavioral and Drug Treatment of Severe Migraine. ann. behav. med. 40, 235–247 (2010). https://doi.org/10.1007/s12160-010-9223-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12160-010-9223-3