Abstract
Background
Substance use is a known predictor of poor adherence to antiretroviral therapies (ART) in people living with human immunodeficiency virus (HIV)/acquired immunodeficiency syndrome. Less studied is the association between substance use and treatment outcomes, namely, suppression of HIV replication.
Methods
Adults living with HIV (N = 183) who reported alcohol use in the previous week and receiving ART were observed over a 12-month period. Participants completed computer interviews, monthly unannounced pill counts to monitor ART adherence, and daily cell-phone delivered interactive-text assessments for alcohol use. HIV viral load was collected at baseline and 12-month follow-up from medical records. Analyses compared participants who had undetectable HIV viral loads at baseline and follow-up (sustained viral suppression) to those with unsustained viral suppression. Analyses also compared participants who were adherent to their medications (>85 % pills taken) over the year of observation to those who were nonadherent.
Results
Fifty-two percent of participants had unsustained viral suppression; 47 % were ART nonadherent. Overall results failed to demonstrate alcohol use as a correlate of sustained viral suppression or treatment adherence. However, alcohol use was associated with nonadherence among participants who did not have sustained viral suppression; nonadherence in unsustained viral suppression patients was related to drinking on fewer days of assessment, missing medications when drinking, and drinking socially.
Conclusions
Poor HIV treatment outcomes and nonadherence were prevalent among adults treated for HIV infection who drink alcohol. Drinking in relation to missed medications and drinking in social settings are targets for interventions among alcohol drinkers at greatest risk for poor treatment outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Antiretroviral therapies (ART) suppress human immunodeficiency virus (HIV) replication and improve the health of people living with HIV infection. In addition, ART has the potential to stem the tide of new HIV infections by reducing viral load and therefore infectiousness [1, 2]. Achieving the health and prevention benefits of ART depends closely on treatment adherence, with all ART regimens requiring at least 85 % adherence [3, 4]. Behavioral research on HIV treatment adherence has identified several factors that reliably predict suboptimal treatment outcomes from ART, including mood disturbances, poor social support, and impoverished living conditions [5–8]. Another common and robust impediment to medication adherence is alcohol use [9].
Individuals who are taking ART and drink alcohol experience more missed doses, medication lapses, and treatment failure [9, 10]. There are several mechanisms by which drinking can interrupt ART adherence. Intoxication impairs memory, planning, organizational skills, and other cognitive abilities that can result in missed medication doses. In addition, the effects of alcohol on nonadherence can occur the day after drinking as a result of hangover [11]. Studies show temporal and dose–response relationships between alcohol consumption and missed HIV medications, with nonbinge drinkers missing more doses than nondrinkers and binge drinkers missing more doses than nonbinge drinkers [11]. Periods of drinking can also delay calling-in refills and picking-up prescriptions from the pharmacy. Furthermore, treatment interruptions may occur when individuals believe they should stop taking their medications to avoid mixing them with alcohol [12, 13].
Antiretroviral adherence must be persistent to achieve the optimal health outcome of viral suppression. While several studies have examined alcohol use in relation to adherence, there is less attention to the impact of drinking on viral suppression. Importantly, adherence is necessary to achieve viral suppression, but viral activity and infectiousness cannot be inferred from adherence alone [14]. ART regimens differ in their levels of adherence required to suppress HIV and interact with the genetic characteristics of the virus such that individuals can be less than optimally adherent and yet viral suppressed. In contrast, development of HIV treatment resistant strains can mean that individuals who are adherent can still have unsuppressed virus [15–17]. Patterns of alcohol use such as drinking frequency, quantity, and context may therefore differ in their association to viral suppression compared to the relationship between drinking and adherence.
The current study examined alcohol use associated with sustained viral suppression as well as medication adherence among people living with HIV who drink alcohol and take ART. We first describe the demographics, health characteristics, and adherence of drinkers who have sustained HIV suppression and those who have not sustained HIV suppression. Next, we report two sets of analyses that examine drinking in relation to HIV viral suppression and ART adherence. First, we compare alcohol use among participants who have and have not sustained HIV suppression, and second, we compare medication adherent to nonadherent participants. We hypothesized that both individuals with unsustained viral suppression and those who were medication nonadherent would evidence greater alcohol use than their viral suppressed and adherent counterparts. Finally, we performed subanalyses to investigate the associations between drinking and adherence in persons with unsustained HIV suppression. This subanalysis was performed to focus on the group of individuals at most risk for viral treatment failure and therefore in greatest need of intervention.
Methods
Participants
People living with HIV who were currently receiving ART and drank alcohol (N = 183) were reached through community recruitment strategies. Interested persons contacted our research program to schedule an intake assessment appointment. The study entry criteria were (a) 18 years of age or older, (b) HIV positive and prescribed ART, and (c) drank alcohol in the past week.
Measures
Participants provided four sources of data. First, participants completed audio-computer assisted self-interviews (ACASI) at the start of the study [18, 19]. Second, we assessed medication adherence using monthly phone-based unannounced pill counts and self-reported day-level adherence. Third, participants responded to cell-phone-delivered interactive text message assessments of daily alcohol use. Finally, we collected HIV viral load and CD4 cell counts at the initial office assessment and again proximal to the final assessment using a participant-assisted medical chart abstraction procedure. The specific measures are described below.
Computerized Interviews
Demographic and Health Characteristics
Participants were asked their gender, age, years of education, income, ethnicity, and employment status.
Substance Use
To assess global alcohol use we administered the Alcohol Use Disorders Identification Test (AUDIT), a 10-item scale designed to measure alcohol consumption and identify risks for alcohol abuse and dependence [20]. Scores on the AUDIT range from 0 to 40, and the AUIDT has demonstrated acceptable reliability and validity. Scores of >8 indicate high risk for alcohol use disorders and problem drinking, with demonstrated specificities between .80 and .90 [21]. In the current sample, the AUDIT was internally consistent, alpha = .90. We also asked participants if they used other drugs in the previous 4-months, including marijuana, cocaine, amphetamines, and other drugs.
ART Adherence
Participants consented to monthly unannounced telephone-based pill counts for the duration of the study. Unannounced pill counts are reliable and valid in assessing medication adherence when conducted in homes [22] and on the telephone [23, 24]. In this study, we conducted unannounced cell-phone-based pill counts. Participants were provided with a free cell phone for use in the study assessments. Following office-based training in the pill counting procedure, participants were called at unscheduled times by a phone assessor. Pill counts occurred over 21–35-day intervals and were conducted for each of the antiretroviral medications participants were taking. Pharmacy information from pill bottles was also collected to verify the number of pills dispensed between calls and whether there was a lapse in obtaining medications from the pharmacy. Adherence was calculated as the ratio of pills counted relative to pills prescribed, taking into account the number of pills dispensed. These data were used to define participant adherence over the course of the study. Based on studies of optimal clinical outcomes, we used pill count adherence to define adherent participants as having taken >85 % of their medications [3, 4].
Because pill count data cannot provide adherence values at the day level, we also measured self-reported adherence at each monthly unannounced phone assessment using a standard measure of 3-day retrospective adherence recall [25, 26]. This format for assessing self-reported 3-day adherence has been found reliable [27]. The phone interviewer asked participants to think back about what they did yesterday and recall the times they had taken each of their medications. A discussion occurred for daily events that was meant to help participants cue their memory and structure their responses. The interviewer asked whether the participant missed a dose of each medication yesterday and recorded the number of doses reportedly missed and taken for each drug. This section of the interview was repeated for each antiretroviral medication over the previous three days, asking participants to report the same information using the same procedures for the day before yesterday and the day before that. The day-level adherence data collection was timed to coincide with the electronic drinking diary in order to link daily adherence with daily alcohol use.
Electronic Drinking Diary
We used an interactive text-diary assessment to collect daily alcohol use. Participants were instructed in the use of text message functions on their study-provided cell phone. Brief daily assessments were designed and delivered using interactive short message system response. Electronic diaries have provided reliable data collection of socially sensitive behavioral data [28, 29]. To reduce participant burden, daily-drinking assessments occurred every other month. Participants received a text prompt to initiate and answer questions about their alcohol use during the previous day. The questions specifically asked about whether participants drank alcohol yesterday and, if so, how much alcohol they drank that day. Daily drinking was recorded by entering numerical responses using the cell phone keypad. The data were stored on a central secured server. Drinking assessments were administered daily for 10 consecutive days, 6 times during the 12-month study, resulting in 60 days of drinking data. Daily assessments included whether participants were drinking the day before, the number of drinks consumed, whether they drank at home, and whether they drank with another person.
Chart Abstracted Viral Load and CD4 Cell Count
We used a participant assisted method for collecting chart abstracted viral load and CD4 cell counts from participants' medical records. Participants were given a form that requested their doctor's office to provide results and dates of their most recent viral load and CD4 cell counts. These data were therefore obtained directly by the participants from their primary HIV care providers. The form included a place for the provider's office stamp or signature to assure data authenticity. Participants collected their chart data at the baseline assessment and again at the end of the study.
Procedures
People living with HIV were recruited through targeted community sampling. We used both venue recruitment and snowball sampling techniques. Venue recruitment relied on responses to brochures placed in waiting rooms of HIV service providers and infectious disease clinics throughout Atlanta, GA, USA. We also implemented an explicit systematic approach to word-of-mouth chain recruitment. Specifically, participants were given brochures that described the study opportunity with a phone number to the research offices. Participants were encouraged to use the brochures to refer their HIV-positive friends to the study.
Figure 1 illustrates the timing and sequence of assessments. Following written informed consent, participants completed the ACASI baseline that required approximately 45 min. Participants were called monthly to conduct unannounced pill counts as well as self-reported 3-day recall adherence. We established a schedule for conducting the 3-day retrospective recall adherence assessments in synch with the interactive drinking diary assessments. Specifically, the unannounced phone interviews were timed to commence after the fourth day of interactive text message assessments to allow for three overlapping days of self-report adherence and interactive text response drinking data. Because the pill counts were unannounced, the call schedule was not disclosed to participants. Unannounced phone interviews that were not completed on the fourth day of text message assessments were attempted on subsequent days, up and through the tenth day of drinking diary assessments. Thus, we obtained time-linked drinking and adherence data for 18 days over the study period. Viral load and CD4 cell counts were collected at the start and end of the study.
Participants were provided with cash reimbursements for each study activity completed: ACASI assessment, $30; unannounced pill count, $20 each; completed interactive text assessment, $2 each; and participant chart abstraction, $25. Data were collected between November 30, 2009 and June 29, 2011. The university Institutional Review Board approved the study.
Data Analyses
For the current study, we defined viral suppression groups on the basis of HIV RNA values obtained from medical record chart abstraction. Participants whose viral load was below the level of detection (<75 copies/ml) at the baseline and at the 12-month follow-up (N = 88) were defined as having sustained viral suppression. Individuals who were either viral suppressed only at baseline or follow-up, or at neither time point (N = 95) were defined as unsustained viral suppression. We first examined demographic and health characteristics of the sample by comparing sustained HIV suppression to unsustained suppression participants. Comparisons for alcohol use were also made between viral suppression groups using binary logistic regression models.
We then tested alcohol use in relation to ART adherence. For these analyses, we defined adherent as having taken at least 85 % of prescribed ART assessed by pill count over the course of the study; 104 participants were adherent and 79 were nonadherent. Table 1 shows the distribution of participants across sustained viral suppression and medication adherence groups. We also conducted a subanalysis of adherent and nonadherent participants among the 95 participants who had unsustained viral suppression. Missing data were most likely missing at random, and not missing completely at random. Among the options available for managing missing values, we selected to analyze all available data because we assume the missingness is not systematic and does not have direct bearing on our statistical models [30]. We chose not to remove participants with incomplete data (i.e., complete case analysis), and we did not impute missing values. For all analyses, groups were compared using logistic regression models with odds ratios and significance defined as p < .05. For each analysis and subanalysis, we performed bivariate models and report unadjusted odds ratios followed by multivariate models with odds ratios adjusted for demographic variables found significantly different between groups. In addition, nonalcohol drug use was included as a covariate in adjusted models.
Results
Among the 449 persons screened for the study, 344 (76 %) were currently taking ART and 320 (71 %) were currently drinking. A total of 183 (40 %) participants were both taking ART and drinking alcohol. All current drinkers taking ART were offered the opportunity, and all agreed to participate in the12-month cohort study. The study sample consisted of 141 men and 42 women. Participants were primarily African American (N = 170, 93 %). A total of 88 (48 %) participants were viral suppressed at both baseline and follow-up and therefore defined as having sustained HIV suppression. Among those defined as having unsustained viral suppression, 12 were suppressed at baseline but not at follow-up, 38 were not suppressed at baseline but were suppressed at follow-up, 32 were not suppressed at either time-point, and 13 were lost to follow-up and therefore did not have a final chart abstraction.
Table 2 shows the demographic and health characteristics of participants who had sustained viral suppression and unsustained viral suppression. The unsustained suppression participants were significantly less likely to be married and were of younger age. In addition, unsustained viral suppression was associated with a less likelihood of being unemployed, and greater likelihood of having a CD4 count <200 cells/cc3. As expected participants who had unsustained HIV suppression were significantly more likely to have been nonadherent and significantly more likely to run out of their medications during the observation period.
Substance Use and Sustained HIV Suppression
The association between problem drinking on the AUDIT and viral suppression at baseline was not significant; 99 (73 %) participants who scored <8 on the AUDIT had undetectable viral loads, as did 27 (59 %) of those scoring above the cut-off for problem drinking, X 2 (1, N = 183) = 3.47, p < .10. Contrary to the study hypotheses, results of unadjusted bivariate and adjusted multivariable logistic regression models did not indicate any significant associations between sustained viral suppression and daily alcohol use (see Table 3). Both the sustained viral suppression and unsustained viral suppression participants reported drinking an average of 12 days during the electronic diary assessments. Both groups reported drinking an average of one drink per day and missed ART on about the same number of drinking days. Drinking for both groups occurred similarly in participants' homes and with another person. With respect to other drug use, unsustained viral suppression was related to cocaine use in the previous 4 months in bivariate analysis but not in the adjusted analysis. There were no other associations with drug use and sustained viral suppression.
Substance Use and ART Adherence
Overall, the association between problem drinking on the AUDIT and baseline ART adherence was not significant; 91 (66 %) participants who scored <8 on the AUDIT were more than 85 % adherent to ART, as were 23 (50 %) of those scoring above the cut-off for problem drinking, X 2 (1, N = 183) = 3.49, p < .10. Table 4 shows the demographic and health characteristics of the adherent and nonadherent groups. Results indicated that participants who were nonadherent were significantly less likely to be viral suppressed at the 12-month follow-up, were significantly more likely to report running out of medications at baseline, and had significantly fewer years of education. There were no other significant differences between groups.
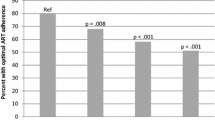
Results of bivariate logistic regressions comparing adherent and nonadherent participants indicated that participants who were nonadherent were significantly more likely to have missed their medications when they were drinking than participants who were adherent (see Table 5). This association remained significant in the model adjusted for education and drug use. In addition, opposite of what we expected, the multivariable model found adherent participants drank on more assessment days than nonadherent participants. There were no other differences between adherent and nonadherent groups on their alcohol or drug use.
Substance Use, Adherence, and Unsustained HIV Suppression
In the adjusted multivariable subanalysis of alcohol use in relation to adherence among participants who had unsustained viral suppression, we found that nonadherence was associated with missing medications on days when participants were drinking and greater proportion of days drinking socially (see Table 6). In addition, running out of medications was related to nonadherence in the bivariate and adjusted models. Results also showed that participants who were adherent drank on more assessment days.
Discussion
The current study found high rates of unsustained HIV suppression among drinkers taking ART. More than half of participants, all of whom were receiving ART and drinking alcohol, demonstrated unsustained HIV suppression. Although nonadherence was clearly a predominant factor in determining HIV nonsuppression, we found 55 % of participants with unsustained viral suppression were adherent and nearly one third of those who had sustained suppression were not adherent. These findings may indicate that for some participants viral nonsuppression may be the result of treatment resistant virus and that a significant number of suppressed participants are at risk for increased viral activity. Treatment resistant virus is often the result of a history of poor adherence to ART, and adherence demands differ across various ART regimens [31]. For example, drugs with a greater half-life as well as those drugs that metabolize more slowly will have a greater duration of antiretroviral activity and will be more forgiving to incomplete adherence [32].
Another factor that may have direct effects on viral replication even under conditions of medication adherence is cocaine use. Similar to recent reports [33], we observed an association between cocaine use and unsustained viral suppression in bivariate analysis. One likely mechanism accounting for cocaine's influence on HIV replication is a downregulation effect of cocaine on micro-RNA in CD4 cells, referred to as cocaine induced enhancement of HIV replication [34]. We also found that being married, older age, and having reliable access to ART were associated with sustained HIV suppression, suggesting potential resources that may bolster positive treatment outcomes.
Results showed different associations between drinking and sustained viral suppression compared to drinking and adherence. Across all of our measures of alcohol use, we failed to find any associations between alcohol use and sustained viral suppression. In addition, alcohol use was not robustly related to ART adherence in this study. Only having missed medications on drinking days was related to nonadherence and the association remained significant in the multivariable model. In addition, the multivariable model unmasked number of drinking days as a significant factor in better adherence. In contrast, characteristics of alcohol use were clearly related to adherence among those participants who did not have sustained viral suppression. Nonadherence in those who did not have sustained viral suppression was related to drinking on fewer days of assessment, missing medications when drinking, and drinking socially. These drinking characteristics were associated with nonadherence over and above running out of medications. These findings together indicate that drinking characteristics were not related to adherence or viral suppression in this sample of drinkers, whereas alcohol use was linked to nonadherence among those with poor treatment outcomes.
One potential explanation for our findings was the universal use of alcohol in the sample. Although the threshold of drinking required to meet the study entry criteria was low, having drank any alcohol in the previous week, sample-wide alcohol use may account for the lack of observed associations. The associations between problem drinking and nonadherence as well as viral suppression were also not significant. The influence of a range of drinking on adherence and viral suppression may therefore be slight among drinkers. Alternatively, our results showed an association between missing medication on drinking days and adherence, perhaps reflecting the impact of event-level alcohol use on adherence [35]. In summary, the high rates of HIV nonadherence and nonsuppression observed in this sample of alcohol drinkers is consistent with previous research showing that alcohol is associated with adherence and poor health outcomes.
These findings should be interpreted in light of the study limitations. First, we relied on a convenience sample that cannot be considered representative of people living with HIV infection. The sample also came from a wide-range of clinical services that likely varied in adherence assistance and substance use treatment. In addition, participants were taking a variety of ART combinations and for various lengths of time. The study also relied on self-report instruments to assess alcohol use. Although we collected alcohol data using a time-stamped daily electronic diary, these data may still be subject to reporting biases. Socially sensitive behaviors such as alcohol use assessed by self-report may be underreported, suggesting that rates of drinking in this study should be considered lower-bound estimates. Another limitation was our definition of nonadherence applied to all medication regimens, which differ in their demand for optimal adherence. We selected 85 % adherence as a cut-off because most combination ART regimens risk resistance at this level of adherence or lower [4, 36, 37]. With these limitations in mind, the current results have implications for improving HIV treatment adherence among people who are receiving ART and drink alcohol.
The high rates of nonadherence and poor treatment outcomes for people with HIV in this sample indicate an urgent need for medication adherence interventions for HIV-positive drinkers. However, we speculate that adherence interventions will have limited impact when alcohol use is not directly addressed. Alcohol cessation at best, or reducing alcohol consumption at minimum, should be central to comprehensive approaches to HIV medication management and treatment adherence. Brief alcohol treatment models that have been proven effective in clinical settings should be integrated into the clinical care of people living with HIV [38, 39]. The close association between missed medications when drinking and overall adherence and viral suppression suggests that interventions be targeted to drinking events proximal to medication doses. Finally, the role of social relationships in drinking should be addressed in alcohol treatment. We found that drinking socially was more common among individuals with poor treatment outcomes. Social relationships can be an asset in treatment adherence and may therefore be a resource for improving adherence among drinkers [5, 40]. Clinical standards are needed for guidance in addressing alcohol use in conjunction with ART.
References
Cohen MS, McCauley M, Gamble TR. HIV treatment as prevention and HPTN 052. Current opinion in HIV and AIDS. 2012;7(2):99–105. Epub 2012/01/10.
Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365(6):493–505. Epub 2011/07/20.
Parienti JJ, Das-Douglas M, Massari V, Guzman D, Deeks SG, Verdon R, et al. Not all missed doses are the same: sustained NNRTI treatment interruptions predict HIV rebound at low-to-moderate adherence levels. PLoS ONE. 2008;3(7):e2783. Epub 2008/07/31.
Kobin AB, Sheth NU. Levels of adherence required for virologic suppression among newer antiretroviral medications. The Annals of pharmacotherapy. 2011;45(3):372–9. Epub 2011/03/10.
Yard SS, Huh D, King KM, Simoni JM. Patient-level moderators of the efficacy of peer support and pager reminder interventions to promote antiretroviral adherence. AIDS Behav. 2011;15(8):1596–604. Epub 2011/07/09.
Franke MF, Murray MB, Munoz M, Hernandez-Diaz S, Sebastian JL, Atwood S, et al. Food insufficiency is a risk factor for suboptimal antiretroviral therapy adherence among HIV-infected adults in urban Peru. AIDS Behav. 2011;15(7):1483–9. Epub 2010/08/18.
Waldrop-Valverde D, Ownby RL, Wilkie FL, Mack A, Kumar M, Metsch L. Neurocognitive aspects of medication adherence in HIV-positive injecting drug users. AIDS Behav. 2006;10(3):287–97. Epub 2006/02/18.
Nilsson Schonnesson L, Williams ML, Ross MW, Bratt G, Keel B. Factors associated with suboptimal antiretroviral therapy adherence to dose, schedule, and dietary instructions. AIDS Behav. 2007;11(2):175–83. Epub 2006/08/24.
Hendershot CS, Stoner SA, Pantalone DW, Simoni JM. Alcohol use and antiretroviral adherence: review and meta-analysis. J Acquir Immune Defic Syndr. 2009;52(2):180–202. Epub 2009/08/12.
Braithwaite RS, Kozal MJ, Chang CC, Roberts MS, Fultz SL, Goetz MB, et al. Adherence, virological and immunological outcomes for HIV-infected veterans starting combination antiretroviral therapies. AIDS. 2007;21(12):1579–89. Epub 2007/07/17.
Braithwaite RS, McGinnis KA, Conigliaro J, Maisto SA, Crystal S, Day N, et al. A temporal and dose–response association between alcohol consumption and medication adherence among veterans in care. Alcoholism, clinical and experimental research. 2005;29(7):1190–7. Epub 2005/07/28.
Kalichman SC, Amaral CM, White D, Swetsze C, Pope H, Kalichman MO, et al. Prevalence and clinical implications of interactive toxicity beliefs regarding mixing alcohol and antiretroviral therapies among people living with HIV/AIDS. AIDS Patient Care STDs. 2009;23(6):449–54. Epub 2009/05/06.
Sankar A, Wunderlich T, Neufeld S, Luborsky M. Sero-positive African Americans' beliefs about alcohol and their impact on anti-retroviral adherence. AIDS Behav. 2007;11(2):195–203. Epub 2006/06/27.
Piacenti FJ. An update and review of antiretroviral therapy. Pharmacotherapy. 2006;26(8):1111–33. Epub 2006/07/26.
Bertagnolio S, De Luca A, Vitoria M, Essajee S, Penazzato M, Hong SY, et al. Determinants of HIV drug resistance and public health implications in low- and middle-income countries. Antivir Ther. 2012;17(6):941–53. Epub 2012/08/18.
Bangsberg DR, Charlebois ED, Grant RM, Holodniy M, Deeks SG, Perry S, et al. High levels of adherence do not prevent accumulation of HIV drug resistance mutations. AIDS. 2003;17(13):1925–32. Epub 2003/09/10.
Bangsberg DR, Moss AR, Deeks SG. Paradoxes of adherence and drug resistance to HIV antiretroviral therapy. J Antimicrob Chemother. 2004;53(5):696–9. Epub 2004/03/27.
Gribble JN, Miller HG, Cooley PC, Catania JA, Pollack L, Turner CF. The impact of T-ACASI interviewing on reported drug use among men who have sex with men. Subst Use Misuse. 2000;35(6–8):869–90. Epub 2000/06/10.
Morrison-Beedy D, Carey MP, Tu X. Accuracy of audio computer-assisted self-interviewing (ACASI) and self-administered questionnaires for the assessment of sexual behavior. AIDS Behav. 2006;10(5):541–52. Epub 2006/05/25.
Saunders JB, Aasland OG, Babor TF, DeLaFuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption II. Addictions. 1993;88(6):791–804.
Maisto SA, Conigliaro J, McNeil M, Kraemer K, Kelley ME. An empirical investigation of the factor structure of the AUDIT. Psychol Assess. 2000;12(3):346–53. Epub 2000/10/06.
Bangsberg DR, Hecht FM, Charlebois ED, Chesney M, Moss A. Comparing objective measures of adherence to HIV antiretroviral therapy: Electronic medication monitors and unannounced pill counts. AIDS and Behavior. 2001;5:275–81.
Kalichman SC, Amaral CM, Cherry C, Flanagan JA, Pope H, Eaton L, et al. Monitoring antiretroviral adherence by unannounced pill counts conducted by telephone: reliability and criterion-related validity. HIV Clinical Trials. 2008;9:298–308.
Kalichman SC, Amaral CM, Stearns HL, White D, Flanagan JA, Pope H, et al. Adherence to antiretroviral therapy assessed by unannounced pill counts conducted by telephone. Journal of General Internal Medicine. 2007;22:1003–6.
Chesney MA, Ickovics JR, Chambers DB, Gifford AL, Neidig J, Zwickl B, et al. Self-reported adherence to antiretroviral medications among participants in HIV clinical trials: the AACTG adherence instruments. Patient Care Committee & Adherence Working Group of the Outcomes Committee of the Adult AIDS Clinical Trials Group (AACTG). AIDS Care. 2000;12(3):255–66. Epub 2000/08/06.
Ickovics JR, Meisler AW. Adherence in AIDS clinical trials: a framework for clinical research and clinical care. J Clin Epidemiol. 1997;50(4):385–91. Epub 1997/04/01.
Simoni J, Kurth AE, Pearson C, Pantalone DW, Merrill J, Frick P. Self-report measures of antiretroviral therapy adherence: a review with recommendations for HIV research and clinical management. AIDS Behavior. 2006;10:227–331.
Bernhardt JM, Usdan S, Mays D, Martin R, Cremeens J, Arriola KJ. Alcohol assessment among college students using wireless mobile technology. J Stud Alcohol Drugs. 2009;70(5):771–5. Epub 2009/09/10.
McAuliffe TL, DiFranceisco W, Reed BR. Low numeracy predicts reduced accuracy of retrospective reports of frequency of sexual behavior. AIDS Behav. 2010;14(6):1320–9. Epub 2010/07/20.
Harel O, Pellowski J, Kalichman S. Are we missing the importance of missing values in HIV prevention randomized clinical trials? Review and recommendations. AIDS Behav. 2012;16:1382–93. Epub 2012/01/10
Bangsberg D, Kroetz DL, Deeks S. Adherence–resistance relationships to combination HIV antiretroviral therapy. Current HIV/AIDS Reports. 2007;4:65–72.
Bangsberg D, Deeks SG. Is average adherence to HIV antiretroviral therapy enough? J Gen Intern Med. 2002;17(10):812–3. Epub 2002/10/23.
Rasbach DA, Desruisseau AJ, Kipp AM, Stinnette S, Kheshti A, Shepherd BE, et al. Active cocaine use is associated with lack of HIV-1 virologic suppression independent of nonadherence to antiretroviral therapy: use of a rapid screening tool during routine clinic visits. AIDS Care. 2013;25(1):109–17. Epub 2012/06/08.
Mantri CK, Pandhare Dash J, Mantri JV, Dash CC. Cocaine enhances HIV-1 replication in CD4+ T cells by down-regulating MiR-125b. PLoS ONE. 2012;7(12):e51387. Epub 2012/12/20.
Weinhardt LS, Carey MP. Does alcohol lead to sexual risk behavior? Findings from event-level research. Annu Rev Sex Res. 2000;11:125–57. Epub 2001/05/16.
Bangsberg DR, Kroetz DL, Deeks SG. Adherence-resistance relationships to combination HIV antiretroviral therapy. Curr HIV/AIDS Rep. 2007;4(2):65–72. Epub 2007/06/06.
Bangsberg DR, Deeks SG. Is average adherence to HIV antiretroviral therapy enough? J Gen Intern Med. 2002;17(10):812–3. Epub 2002/10/23.
Miller WR. Are alcoholism treatments effective? The Project MATCH data: response. BMC Public Health. 2005;5:76. Epub 2005/07/20.
Anton RF, O'Malley SS, Ciraulo DA, Cisler RA, Couper D, Donovan DM, et al. Combined pharmacotherapies and behavioral interventions for alcohol dependence: the COMBINE study: a randomized controlled trial. JAMA. 2006;295(17):2003–17. Epub 2006/05/04.
Simoni JM, Frick PA, Lockhart D, Liebovitz D. Mediators of social support and antiretroviral adherence among an indigent population in New York City. AIDS Patient Care STDs. 2002;16(9):431–9. Epub 2002/10/25.
Author information
Authors and Affiliations
Corresponding author
Additional information
An America Reinvestment and Recovery Act (ARRA) Challenge Grant from the National Institute of Alcohol Abuse and Alcoholism (NIAAA) RC1AA018983 supported this research.
Rights and permissions
About this article
Cite this article
Kalichman, S.C., Grebler, T., Amaral, C.M. et al. Viral Suppression and Antiretroviral Medication Adherence Among Alcohol Using HIV-Positive Adults. Int.J. Behav. Med. 21, 811–820 (2014). https://doi.org/10.1007/s12529-013-9353-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12529-013-9353-7