Abstract
Objectives
The purpose of this study was to examine a qualitative scoring system and a semi-quantitative method of FDG-PET/CT imaging in the diagnosis of infective endocarditis (IE).
Methods
We retrospectively included 108 patients who underwent 18F-FDG-PET/CT for suspected IE. PET/CT scans were interpreted using a 4-point score (0 = no uptake; 1 = cardiac uptake < blood-pool activity; 2 = blood-pool < uptake < liver activity; 3 = uptake > liver) and semi-quantitatively using SUVmax and SUVmean of the suspected valve lesion, liver, spleen, and of the bone marrow (BM). BM and spleen SUVmean were normalized to the liver, and hypermetabolism (HSBM) was defined as a BM or spleen-to-liver ratio > 1.
Results
Comparing the score criteria results with the clinical final diagnosis, the sensitivity, specificity, positive predictive value, negative predictive value, and accuracy of qualitative criteria were 93%, 81%, 84%, 91%, and 87%, respectively. A definite IE was documented in 83% of patients showing HSBM and abnormal cardiac uptake, 44% with abnormal cardiac uptake, 28% with HSBM, and 10% with neither one.
Conclusion
The qualitative scoring system is helpful in the diagnosis of IE. The HSBM is an additional, reliable indirect sign of IE.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Infective endocarditis (IE) is defined as infection of a native or prosthetic heart valve (PVE) or an indwelling cardiac device (CIED).1 IE is associated with high-cost prolonged hospitalization and impaired quality of life.2
IE was described for the first time in 1885 by Osler, since then notable improvements in diagnosis and treatment have been made. However, the mortality is still high, about 20% in the first 30 days.3
The diagnosis of IE is based on the combination of clinical, laboratory, and imaging findings. Clinical and echocardiographic findings are non-specific especially in PVE and CIED. According to the latest update of the European Society of Cardiology (ESC) guidelines for the management of IE, 18-fluorine-fluorodeoxyglucose positron emission tomography/computed tomography (18F-FDG PET/CT) is included in the diagnostic flowchart for the diagnosis of IE especially in patients with prosthetic heart valve.4
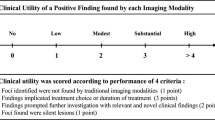
In this context, the use of a simple qualitative criterion with good interpreter reliability, easy reproducibility, and good diagnostic performance would be crucial in the diagnosis. We propose a 4-point score, like Deauville score, to estimate the accuracy of 18F-FDG PET/CT in detecting IE. (The Deauville 5-point scoring system is an internationally accepted and utilized five-point scoring system for FDG avidity in patients with Hodgkin's lymphoma or Non-Hodgkin's lymphoma; scores of 1 and 2 are negative and 4 and 5 are considered to be positive)
We also evaluated a semi-quantitative criterion based on indirect signs such as a diffuse increase in spleen and/or bone marrow (BM) uptake. The host defense against IE involves the activation of polymorphonuclear cells, macrophages, and lymphocytes leading to an increase in the glycolytic metabolism, which could be documented in BM and spleen.5,6
The aim of our study was to examine the value of these 18F-FDG PET/CT methods in the diagnosis of IE.
Methods
Patients’ Selection and Preparation
We retrospectively included 108 patients (57males, 51 females, mean age 62 years; 25 with NVE and 83 with PVE and/or CIED) among patients who underwent 18F-FDG PET/CT scans from 2016 to 2020 for suspicious IE (Table 1).
All patients adopted a specific preparation consisting of a low-carbohydrate, high-protein, and high-fat diet (LCHPHF) protocol started 72 hours before the examination to reduce the high physiological myocardial FDG uptake. The LCHPHF diet was written in a menu of permitted and prohibited food given to the patients at the time of a confirmation phone interaction. To verify the adherence to the diet, at time of PET scan, all patents were specifically inquired about their complete adherence to the diet during the previous 72-hours and on the time of their last meal or snack. The efficacy of the diet was further visually evaluated by two nuclear medicine physicians with experience in cardiac imaging, using a previously validated three-point visual scale7: 0, negligible myocardium FDG uptake; 1, mild uptake and doubtful examination; and 2, homogeneously intense uptake. We included only patients with 0 scores (Figure 1).
18F-FDG PET/CT Imaging
18F-FDG PET/CT was performed in all cases with a glucose level lower than 150 mg⋅dL. An activity of 3.5-4.5 MBq⋅Kg of 18F-FDG was administered intravenously and images were acquired at least 60 ± 10 min after injection from the skull base to the mid-thigh on a Discovery ST PET/CT tomograph (General Electric Company-GE-Milwaukee, WI, USA) with standard parameters (CT: 80 mA, 120 Kv without contrast; 2.5–4 min per bed-PET-step of 15 cm); the reconstruction was performed in a 256 × 256 matrix and 60 cm field of view. Non-attenuation correction (NAC) was routinely performed and analyzed especially in patients with PVE and CIED. Patients were invited to void before imaging acquisition; no oral or intravenous contrast agents were administrated in the days before FDG-PET; a written consent was obtained before the studies.
According to ESC and EANM guidelines, we did not perform routine PET/CT ECG-gated or with contrast-enhanced CT because there is no evidence that these protocols improve the diagnostic accuracy in suspected IE.
For the evaluation of the accuracy of PET/CT results, a combination of clinical, microbiological, and/or imaging follow-up for at least 6 months was taken as reference standard for the final clinical diagnosis (presence of endocarditis or absence), including histopathologic examinations and further imaging studies such as echocardiography, magnetic resonance imaging, and CT with or without contrast.
Positive 18F-FDG PET/CT findings were judged true-positive when endocarditis was confirmed by histopathology or when a subsequent imaging technique showed a response after antibiotic therapy. Positive 18F-FDG PET/CT findings were defined as false-positive when histopathology resulted negative or when the lesions had resolved on subsequent follow-up imaging without any treatment. Negative 18F-FDG PET/CT was conventionally deemed as true-negative when histopathology results were negative or when endocarditis was not demonstrable during the subsequent follow-up. Negative 18F-FDG PET/CT was judged as false-negative if histological examination was positive.
Analysis of 18F-FDG PET Images
Qualitative Assessment
Visual analysis was carried out by two nuclear medicine physicians with experience in this field, who were blinded to all the other patient data. They analyzed PET/CT images using a proposed four-point score similar to Deauville score:
-
0
no focal cardiac uptake
-
1
focal cardiac uptake < mediastinal uptake
-
2
mediastinal uptake < focal cardiac uptake < liver uptake
-
3
focal cardiac uptake ≥ liver uptake.
According to ESC guidelines, cardiac uptake was considered abnormal activity around the site of prosthetic valve implantation or defibrillator leads.
Exams with scores 0, 1, and 2 were considered negative, while images with score 3 were considered positive for IE (Figure 2).
Semi-quantitative Analysis
Indirect signs of infection and/or inflammation were assessed by two blinded experienced observers on a Xeleris workstation (General Electric Company-GE-Milwaukee, WI, USA). Mean Standardized Uptake Values (SUVmean) were obtained from spherical regions of interest (ROI) positioned close to the centers of the spleen and of the right liver lobe, excluding areas of abscess and/or ischemic lesions.
The SUVmean of the bone marrow (BM) was obtained by averaging the SUVmean from spherical ROIs drawings on the bodies of each of the five lumbar vertebrae, excluding any damaged vertebra.
BM and spleen SUVmean values were then normalized to those of the liver, and a hypermetabolism of the BM or spleen (HSBM) was defined as a BM or spleen-to-liver ratio > 1.
Exclusion Criteria
According to ESC guidelines, we did not perform PET/CT during antibiotics or steroids therapy but a patient in our cohort underwent PET/CT during prolonged antimicrobial therapy for chronic inflammatory bowel disease discovered in the follow-up.
According to EANM guidelines, we did not perform PET/CT in patients with glucose blood levels > 150mg⋅dL, patients who did not follow the diet protocol LCHPHF, and patients who had implanted prosthetic valve for less than 3 months. After evaluation of FDG myocardial uptake, we excluded 4 patients.
Statistical Analysis
All statistical analysis was performed using MedCalc Software version 17.1 for Windows (Ostend, Belgium). The descriptive analysis of categorical variables comprised the calculation of simple and relative frequencies. The numeric variables were described as mean, minimal, and maximal.
Sensitivity, specificity, negative predictive value (NPV), positive predictive value (PPV), and accuracy of each method of analysis were assessed in comparison to the clinical final diagnosis. Differences between the two methods were investigated by Spearman’s rho coefficient. Inter-reader variability was assessed using percent agreement and kappa statistics. A P value of ≤ 0.05 was considered as statistically significant.
Results
Of the 108 patients enrolled in the study, 54 (50%) had a final diagnosis of IE of which 19 (35%) had histopathology diagnosis, 14 (25%) had a diagnosis of IE confirmed by imaging, and 21 (38%) had a diagnosis confirmed by clinical follow-up and treatment response.
Comparing the score results with the final clinical diagnosis, the sensitivity, specificity, positive predictive value, negative predictive value, and accuracy of our qualitative score were 93% [95% confidence interval (CI) 83%–98%], 81% (95% CI 67%–90%), 84% (95% CI 75%–9%), 91% (95% CI 80%–96%), and 87% (95% CI 79%–93%), respectively.
Most FP (6/10) results were in patients studied within 3.5–4 months after implantation and demonstrated a focal cardiac uptake, but histological examination showed only inflammatory response. Furthermore, all the 4 FN cases were in patients with NV. Considering patients who underwent PET/CT for suspected NVE, Sensitivity, Specificity, PPV, NPV, and Accuracy were respectively 23%, 92%, 75%, 52%, and 56% (Table 2).
There was a high agreement between the two readers applying these (k = 0.902).
For the evaluation of HSBM, from the 108 patients, 9 patients who showed HSBM were excluded because PET/CT‘s visual analysis demonstrated other inflammatory diseases (3 spondylodiscitis, 4 vasculitis, 1 sarcoidosis, 1 vascular graft infection). Among the 99 remaining patients, 54 (55%) had a clinical final diagnosis of IE. A definite IE was documented in 83% (40/48) of patients showing both HSBM and abnormal cardiac uptake, 44% (4/9) of patients with only abnormal cardiac uptake, 28% (9/32) of patients with only HSBM, and 10% (1/10) of patients with neither one (this patient was on therapy with antibiotics and glucocorticoids). Of the 45 remaining patients, 3 demonstrated bone marrow hypermetabolism due to chronic myeloid leukemia (CML), beta thalassemia, and erythropoietin therapy (Figure 3).
18F-FDG PET/CT fused axial and coronal images that showed 4 cases presented in the evaluation of HSBM: A cardiac uptake and HSBM of the spleen and BM confirmed by histopathology demonstration of NVE; B only cardiac uptake without signs of HSBM consistent in PVE confirmed by persistent positive blood cultures; C no cardiac uptake but signs of HSBM of the spleen consistent in PVE confirmed by cardiac-CT; D no cardiac uptake and no HSBM signs but clinical diagnosis of PVE founded by a major criterion (demonstration of S. viridans in 2 bood cultures) and 3 minor criteria (fever > 38, conjunctival hemorrhages, Janeway lesions). (All cardiac uptakes were confirmed by NAC images)
Using this semiquantitative criterion, we obtained 9 FP attributable to other inflammatory disease and 5 FN, 1 of which is attributable to an antimicrobic therapy in place for other coexisting diseases and 4 to interfering metabolic conditions (such as 2 diabetes, 1 hepatic steatosis, and 1 hepatic cirrhosis).
HSBM was a predictor of IE (P < 0.05), independently of the criterion of abnormal cardiac FDG uptake.
Comparing the two proposed methods for the analysis of 18F-FDG PET/CT images with Spearman test, we obtained a rho = 0.473 with a P < 0.0001 (95% Cl 0.304-0.613).
Discussion
The key role of 18F-FDG PET/CT plays in diagnosis of IE is well established, especially in the “possible” cases according to Duke’s echocardiographic criteria, in PVE and CIED.
18F-FDG PET examinations performed in patients with known or suspected IE are influenced by several interfering factors: first, a physiological myocardial uptake of FDG, which could be avoided by an adequate diet preparation; and secondly the possible effect of antibiotics which could mask a correct diagnosis. For this reason, according to ESC guidelines, this exam must be performed before starting antibiotic or corticosteroid therapies.8
Furthermore, FDG is a non-specific tracer which is taken up in any process with increased glucose utilization; thus FDG uptake is not a “black or white” phenomenon indicating the presence or absence of infections or malignancy but there are some levels of the “gray-zone”, affecting a correct interpretation and a final diagnosis.
In this context, as for neoplastic pathologies, an interpretative standardization of PET/CT images could add great value in the diagnosis of IE with PET/CT.
Our intent was to seek interpretation criteria that are objective, reproducible and easy to apply in the clinical routine, especially in the presence of findings that falls in the “gray zone”.9
We proposed, first of all, a qualitative criterion in which the visual degree of uptake is defined for suspect lesions according to a four-point score, similar to the Deauville criteria for the evaluation of lymphoma patients, as made by the study of Interpretation criteria for FDG-PET/CT in multiple myeloma (IMPeTUs).10,11
The results obtained seem to be strong enough in terms of accuracy, NPV, and PPV responding. These criteria also demonstrated high inter-readers agreement (k = 0.902).
In our study, false-positive results were found in patients with inflammatory response associated with recent implantation of a prosthetic valve, as well as the use of surgical adhesives;12 false-negative results were reported for IE on native valves.13 This may be explained by the small size, avascular nature, and high mobility of vegetation on native valves and by a lower neutrophil population when compared with IE on prosthetic valves. In this case, a gated-PET acquisition may be helpful.14
FDG-PET may provide direct but also indirect signs of infection and/or inflammation, notably a diffuse increase in the spleen and/or bone marrow uptake.15 A FDG uptake in BM greater than liver has been associated with BM hypermetabolism and hyperactivity with a similar observation reported for the spleen.16,17 This phenomenon can be explained by the evidence that the host defense against IE involves the activation of macrophages, lymphocytes, and polymorph nuclear cells leading to an increase in glycolytic metabolism documented in BM (the site of leukocyte progenitor cells production) and spleen (the site of interaction of activated immune cells with microorganism in blood).18,19,20
Our results demonstrated that HSBM might be a helpful additional indirect sign for diagnosis of IE.
Some limitations of this indirect sign, as demonstrated by the FN found in our study, are that hypermetabolism may be impacted by metabolic disorders like hepatic steatosis, insulin resistance, metabolic syndrome, etc. In these cases, the liver exhibits higher FDG activity. Thus, the current standardization to liver activity should be used with caution on FDG-PET exams performed in patients with some metabolic disorders.21,22
Conclusion
The proposed 4-point scale criteria are a simple, qualitative method with substantial inter-interpreter agreement and high positive predictive value and accuracy and may have a significant impact in the diagnosis of IE with PET/CT.
The HSBM is an additional, reliable indirect sign of IE and could strengthen the suspicion of IE, especially in the absence of any other infections, inflammatory or malignant disease.
These criteria could be useful for evaluating treatment response.
Limitations of the Study
This is a single center study with small number of patients, and thus further large multicenter and prospective studies are needed.
New Knowledge Gained
Combination of direct PET/CT interpretation criteria and indirect criteria leads to more reliable imaging methods using FDG/CT in the diagnosis of IE.
Change history
11 February 2022
A Correction to this paper has been published: https://doi.org/10.1007/s12350-022-02919-4
Abbreviations
- IE:
-
Infective endocarditis
- PVE:
-
Prosthetic heart valve endocarditis
- CIED:
-
Cardiac implantable electronic device
- NVE:
-
Native valve endocarditis
- ICD:
-
Indwelling cardiac device
- ESC:
-
European Society of Cardiology
- BM:
-
Bone marrow
- HSBM:
-
Hypermetabolism of spleen and/or bone marrow
- LCHPHF:
-
Low-carbohydrate, high-protein and high-fat diet
- NAC:
-
Non-attenuation correction
References
Slipczuk L, Codolosa JN, Davila CD et al. Infective endocarditis epidemiology over five decades: a systemic review. PLoS ONE 2013; 8:1-17
Moreillon P, Que YA. Infective endocarditis. Lancet 2004; 363:139-49
Verhagen DW, Hermanides J, Korevaar JC et al. Health-related quality of life and posttraumatic stress disorder among survivors of left-sided native valve endocarditis. Clin Infect Dis 2009; 48:1559-65
Habib G, Lancellotti P, Antunes MJ et al. 2015 ESC Guidelines for the management of infective endocarditis. Eur Hear J 2015; 36:3075-23
Lee JW, Lee MS, Chung IK et al. Clinical implication of FDG uptake of bone marrow in PET/CT in gastric cancer patients with surgical resection. World J Gastroenterol 2017; 23:2385-95
Inoue K, Goto R, Okada K et al. A bone marrow F-18 FDG uptake exceeding the liver uptake may indicate bone marrow hyperactivity. Ann Nucl Med 2009; 23:643-49
Gazzilli M, Albano D, Durmo R et al. Improvement of diagnostic accuracy of 18fluorine-fluorodeoxyglucose PET/computed tomography in detection of infective endocarditis using a 72-h low carbs protocol. Nucl Med Commun 2020; 41:753-58
Scholtens AM, van Aarnhem EEHL, Budde RP et al. Effect of antibiotics on FDG-PET/CT imaging of prosthetic heart valve endocarditis. Eur Heart J Cardiovasc Imaging 2016; 9:1462-65
Barrington SF, Qian W, Somer EJ et al. Concordance between four European centres of PET reporting criteria designed for use in multicentre trials in Hodgkin lymphoma. Eur J Nucl Med Imagig 2010; 37:1824-33
Horning SJ, Juweid ME, Schoder H et al. Interim positron emission tomography (PET) scans in diffuse large B-cell lymphoma: An indipendent expert nuclear medicine evaluation of the Eastern Cooperative Oncology Group E3404 study. Blood 2010; 115:775-77
Nanni C, Versari A, Chauvie S et al. Interpretation criteria for FDG PET/CT in multiple myeloma (IMPeTUs): Final results. IMPeTUs (Italian myeloma criteria for PET Use). Eur J Nuc Med Mol Immunity 2018; 45:712-19
Swart LE, Gomes A, Scholtens AM et al. improving the diagnostic performance of 18F-fluorodeoxyglucose positron-emission tomography/computed tomography in prosthetic heart valve endocarditis. Circulation 2018; 138:1412-27
Albano D, Dondi F, Gazzilli M et al. Meta-analysis of the diagnostic performance of 18F FDG-PET/CT in native valve endocarditis. JACC: Cardiovascular Imaging. 2020. https://doi.org/10.1016/j.jcmg.2020.09.021
Siddiqui RF, Abraham JR, Buttany J et al. Bioprosthetic herat valve: Modes of failure. Histopatology 2009; 55:135-44
Boursier C, Duval X, Mahida B et al. Hypermetabolism of the spleen or bone marrow is ana additional albeit indirect sign of infective endocarditis at FDG-PET. J Nucl Cardiol. 2020. https://doi.org/10.1007/s12350-020-020050-2
Inocue K, Goto R, Okada K et al. A bone marrow F-18 FDG uptake exceeding the liver uptake may indicate bone marrow hyperactivity. Ann Nucl Med 2009; 23:643-49
Nam H-Y, Kim SJ, Kim IJ et al. The clinical implication and prediction of diffuse splenic FDG uptake during cancer surveillance. Clin Nucl Med 2010; 35:759-63
Mebius RE, Kraal G. structure and function of the spleen. Nat Rev Immunol 2005; 5:606-16
Bronte V, Pittet MJ. The spleen in local and systemic regulation of immunity. Immunity 2013; 39:806-18
Zhao E, Xu H, Wang L et al. Bone marrow and the control of immunity. Cell Mol Immunol 2012; 9:11-19
Keramida G, Hunter J, Peters AM. Hepatic glucose utilization in hepatic steatosis and obesity. Biosci Rep 2016; 36:e00402
Yoo ID, Lee SM, Lee JW et al. The influence of adipose tissue volume can significantly affect the metabolic activity of references organs in 18F-FDG PET/CT studies of a normal healthy population. Hell J Nucl Med 2017; 20:211-16
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The authors of this article have provided a PowerPoint file, available for download at SpringerLink, which summarizes the contents of the paper and is free for re-use at meetings and presentations. Search for the article DOI on SpringerLink.com.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Gazzilli, M., Albano, D., Lucchini, S. et al. New criteria for the diagnosis of infective endocarditis using 18F-FDG PET/CT imaging. J. Nucl. Cardiol. 29, 2188–2194 (2022). https://doi.org/10.1007/s12350-021-02663-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-021-02663-1