Abstract
Background
Assessment of quality of life in patients with stable angina and normal gated single-photon emission computed tomography myocardial perfusion imaging (MPI) remains undefined. Symptom evolution in response to imaging findings has important implications on further diagnostic testing and therapeutic interventions.
Methods
Prospective cohort study was conducted at the University of Alabama at Birmingham enrolling 87 adult participants with stable chest pain from the emergency room, hospital setting, and outpatient clinics. Patients underwent MPI with technetium-99m Sestamibi and had a normal study. Participants filled out Seattle Angina Questionnaires initially and at 3-month follow-up.
Results
Among the 87 participants (60 ± 12 years; 40% African American, 70% women, 29% diabetes), the mean score increased by an absolute value of 14.2 [95% CI 10.4–18.7, P < .001] in physical limitation, 23.2 [95% CI 17.1–29.4, P < .001] in angina stability, 10.9 [95% CI 7.6–14.1, P < .001] in angina frequency, and 20.6 [95% CI 16.5–24.7, P < .001] in disease perception. There was no significant change in the mean score of treatment satisfaction [− 1.4, 95% CI − 4.7 to 1.8, P = .38]. At 3-month follow-up, 28 of 87 participants (32%) were angina free.
Conclusions
Patients with stable chest pain and normal MPI experience significant improvement in functional status, quality of life, and disease perception in the short term.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Chest pain of suspected cardiac origin is one of the most common presenting complaints across the United States, with an estimated 9 million adults living with chronic stable angina.1,2,3 The diagnostic investigation and management of patients presenting with suspected cardiac chest pain or its equivalence is a common dilemma faced by medical providers. Given the myriad of possibilities as to the cause of chest pain, clinical care pathway models have been developed which often include cardiac stress testing with imaging such as single-photon emission computed tomography myocardial perfusion imaging (MPI) to evaluate for myocardial ischemia.4
MPI provides diagnostic and risk stratification information that guides clinical management.5 In general, a normal MPI is associated with low risk of future adverse cardiovascular events and is therefore reassuring to the patient and referring provider.6,7,8 However, both patients and providers are increasingly focusing on quality of life (QOL) domains in addition to hard cardiovascular outcomes.9The change in symptoms and QOL measures in patients after undergoing a normal MPI has important implications on the implementation of further diagnostic tests and procedures in addition to therapeutic interventions in symptomatic patients. The aim of this study is to assess the evolution of symptoms after a normal MPI in patients with or suspected of having stable coronary artery disease (CAD) by serial administration of the Seattle Angina Questionnaire (SAQ).10
Methods
The Radionuclide Imaging and Symptomatic Evolution study (RISE) is a prospective cohort study conducted at the University of Alabama at Birmingham (UAB) and The Kirklin Clinic. The study was approved by the Institutional Review Board at UAB and was performed in accordance with the ethical standards laid down in the 1975 Declaration of Helsinki and its later amendments. The participants were enrolled between November 2015 and February 2016, with data collection completed by June 2016. Participants provided written informed consent prior to enrollment. Patient eligibility and enrollment were reviewed for appropriateness by two independent investigators. Two authors extracted individual patient demographics, history, and clinical variables via electronic medical chart review and entered data into standardized databases.
Study Population
Participants were enrolled in the study from the stress laboratory after being referred for a clinically indicated MPI from the outpatient clinics, the emergency department, or from the chest pain unit located in the hospital. Patients 18 to 90 years of age presenting with symptoms of chronic stable angina or an angina equivalent who underwent MPI were considered for recruitment. Importantly, patient recruitment occurred prior to performing MPI to decrease bias. To preserve the homogeneity of the cohort, we only recruited patients who underwent regadenoson MPI excluding patients who underwent treadmill or other forms of pharmacologic stress testing. We excluded patients undergoing MPI for indications other than angina or angina equivalent symptoms such as evaluation for transplantation or preoperatively for other surgeries, testing for routine follow-up after coronary revascularization (CR) procedures, and acute coronary syndrome (ACS). Patients with abnormal myocardial perfusion and/or left ventricular ejection fraction (LVEF) on MPI were excluded. All participants were clinically and hemodynamically stable at the time of stress testing.
Seattle Angina Questionnaire (SAQ)
Each participant completed the SAQ, an established and well-validated instrument used to reliably and reproducibly assess the burden of angina symptoms. The SAQ is a 19-item self-administered survey measuring five different dimensions of angina including physical limitation, angina stability, angina frequency, treatment satisfaction, and disease perception. The SAQ has been found to be sensitive in detecting both drastic and more subtle clinical changes in the burden of angina or angina equivalent symptoms over time.10 Higher scores (scores range from 0 to 100) on its five scales represent better perception of health and QOL. The SAQ was administered to each patient to fill out at time of enrollment and prior to undergoing MPI. At 3-month follow-up, the SAQ was readministered over the telephone and responses recorded. In addition, a standardized survey by telephone interview was conducted with the patients to document changes to their medical regimen and clinical diagnoses and to inquire about their vital status, cardiac events including any hospitalization, myocardial infarction (MI), and CR with percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG) and the corresponding event date and reason for hospitalization.
MPI Protocol
All patients underwent gated MPI with technetium-99m Sestamibi. Results were reviewed with patients once available after the administration of the baseline SAQ. Regadenoson MPI was performed using standard protocols per American Society of Nuclear Cardiology recommendations.11 Specifics of stress testing, image acquisition, and reader interpretation in our laboratory have been previously described.7,8,12 In brief, a single bolus of 0.4 mg of regadenoson was administered via peripheral vein access, followed subsequently by normal saline flush.13 None of the patients in our study underwent a combination of treadmill with regadenoson. The tracer, technetium-99m sestamibi, was injected 10 to 20 seconds after the saline flush was given. Gated images were obtained 1 hour post radiotracer administration with a dual-head detector gamma camera using a low energy, high resolution collimator with a 64 × 64 matrix. Rest images were performed when there was uncertainty in the interpretation of the stress images as previously described.14 The presence and extent of perfusion abnormality were determined by a software program (Corridor4DM) with visual supervision.15 LVEF was determined from the gated images.16 Perfusion defects were then quantified as % of LV myocardium and expressed as perfusion defect size with ≥ 5% LV considered to be abnormal. An LVEF ≤ 50% was considered to be abnormal.
Data endpoints and Outcomes Assessment
SAQ scoring is based on the assignment of an ordinal value ranging from 1, which implies the lowest level of functioning, to 5 or 6 at the highest level. The SAQ scores in each of the five domains were derived using standard SAQ methodology.10,17 In addition to determining the mean change in scores, we examined the proportion of patients who experienced a change of 10 points or more in any of the five subsets since such a change has been previously determined to be clinically significant.10
Statistical Analyses
Continuous data were expressed as mean ± standard deviation. Categorical data were displayed as a percentage. Paired t testing (two-tailed) was used to compare initial and 3-month follow-up SAQ scores. Confidence intervals of 95% were used, and P values < .05 were considered statistically significant. The Fisher’s Exact test was used to compare proportions of patients who were angina free (i.e., score of 100 on the angina frequency scale) at index SAQ and 3-month follow-up. A threshold P value < .05 was set apriori to indicate statistical significance.
Results
Baseline Clinical Characteristics
Of the 104 patients we screened for the study, 15 had abnormal perfusion and were excluded per protocol. Another 2 patients completed the initial SAQ but were lost to follow-up and were excluded from the analysis. Follow-up was complete on the remaining 87 patients (98%) who had a normal MPI and they constituted the study cohort of the current report. The baseline characteristics of the cohort are summarized in Table 1. The age of the participants ranged from 33 to 88 with a mean of 60 years. The majority of participants were women (70%) and the cohort included a significant representation of African Americans (40%). The most common indications for MPI were chest pain (78%) and dyspnea (20%). Two patients were referred for symptoms of palpitations with electrocardiographic changes consistent with ischemia.
Between the baseline assessment and the 3-month follow-up visit, 6 (7%) patients were hospitalized for any cause including 2 (2%) for cardiac indications—one for a new diagnosis of atrial fibrillation and another for permanent pacemaker placement and lead revision. Importantly, there were no hospitalizations for ACS, and none of the patients had an MI, stroke, or died during this period.
Medication intake at baseline and at follow-up is detailed in Table 3. At baseline, almost one half of patients were taking at least one anti-anginal medication (48.3%). At follow-up an additional 4 (5%) patients were started on anti-anginal medications (2 on beta-blockers, 2 on long-acting nitrates). No anti-anginal medications were discontinued during the follow-up period and there were no changes in dosage (up or down titration).
SAQ scores for the different scales at baseline and after 3 months of follow-up for the total cohort as well as subgroup analysis for men and women are shown in Table 2.
Physical Limitation Scale
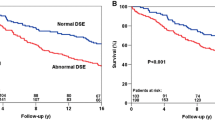
The physical limitation scale quantifies activity limitation and exercise duration due to CAD. Of the 87 patients, we were not able to calculate a score at baseline on 3 (3%) patients due to the patient answering “limited, or did not do for other reasons” for more than 4 items on the scale. At the 3-month follow-up, we were able to calculate a score for 86 (99%) patients including 2 of the 3 patients that did not have scores at baseline. The mean score was 71.3 ± 23.0 [95% CI 66.3–76.2] at baseline and 85.5 ± 19.4 [95% CI 81.7–89.2] at follow-up (Figure 1 and Table 2). The score increased by an absolute mean of 14.2 (P < .001). Further, 40 (46%) patients experienced an increase, while 3 (3.4%) experienced a decrease by 10 or more points (Figure 2). Subgroup analysis showed that the mean score increased by 13.3 for men (P = .0015), 14.6 for women (P < .001), and 15.4 (P < .001) in patients who had no changes in their anti-anginal medications (Figure 3).
Angina Stability Scale
The angina stability scale assesses changes in frequency of angina during the most strenuous levels of activity with lower scores indicating more frequent angina and higher scores associated with less angina at that level of activity. The mean score was 57.7 ± 25.8 [95% CI 52.3–63.1] at baseline and 80.9 ± 22.0 [95% CI 76.3–85.5] at follow-up (Figure 1 and Table 2). The score increased by an absolute mean of 23.2 (P < .001). Further, 53 (60.9%) experienced an increase, while 7 (8.0%) experienced a decrease by 10 or more points (Figure 2). Subgroup analysis showed that the mean score increased by 24.6 for men (P < .001), 22.6 for women (P < .001), and 23.4 (P < .001) in patients who had no changes in their anti-anginal medications (Figure 3).
Angina Frequency Scale
The SAQ angina frequency score correlates accurately with sublingual nitroglycerin usage, the putative gold standard for quantifying patient angina.18] The mean score was 76.3 ± 13.0 [95% CI 73.6–79.1] at baseline and 87.2 ± 12.6 [95% CI 84.5–89.8] at follow-up (Figure 1 and Table 2). The score increased by an absolute mean of 10.9 (P < .001). Further, 31 (35.6%) experienced an increase , while 3 (3.4%) experienced a decrease by 10 or more points (Figure 2). Subgroup analysis showed that the mean score increased by 10.6 for men (P = .0044), 11.0 for women (P < .001), and 10.8 (P < .001) in patients who had no changes in their anti-anginal medications (Figure 3). At baseline, 6 of 87 patients (6.8%) reported being angina free over the prior 4 weeks. At 3-month follow-up, 28 of 87 people (32%) were angina free (P < .001).
Treatment Satisfaction Scale
The treatment satisfaction scale characterizes patient satisfaction with their current treatment. The mean treatment satisfaction score was 91.4 ± 12.1 [95% CI 88.9–94.0] at baseline and 90.0 ± 16.7 [95% CI 86.5–93.5] at follow-up (Figure 1 and Table 2). The score did not significantly change during follow-up with an absolute decrease in the mean by 1.4 (P = .38). Further, 13 (14.9%) experienced an increase , while 12 (13.8%) experienced a decrease by 10 or more points (Figure 2). Subgroup analysis showed that the mean score was unchanged in men (absolute increase 0.2, P = .94), women (absolute decrease 2.1, P = .32), and in patients who had no changes in their anti-anginal medications (absolute decrease 0.1, P = .97) (Figure 3).
Disease Perception Scale
The disease perception scale quantifies the effects of CAD on QOL. The score was 61.5 ± 19.1 [95% CI 57.5–65.5] at baseline and 82.1 ± 16.6 [95% CI 78.6–85.6] at follow-up (Figure 1 and Table 2). The score increased by an absolute mean of 20.6 (P < .001). Further, 66 (75.9%) experienced an increase , while 4 (4.6%) experienced a decrease by 10 or more points (Figure 2). Subgroup analysis showed that the mean score increased by 18.5 for men (P < .001), 21.5 for women (P < .001), and 20.9 (P < .001) in patients who had no changes in their anti-anginal medications (Figure 3).
Discussion
According to the National Center for Health Statistics, chest pain accounts for more than 5.5 million emergency department visits annually.19 Typical angina or angina variants as a potential manifestation of underlying CAD affects approximately 20% of people 1 year after MI 20,21 as well as approximately 45% of those with CAD who live with chronic stable angina.22 Current American College of Cardiology Foundation/American Heart Association Guidelines for the diagnosis and management of patients with stable ischemic heart disease define the goals of treating patients with stable CAD as minimizing the likelihood of death while maximizing health and function.23 More specifically, the guidelines endorse the maintenance or restoration of a level of activity, functional capacity and QOL that is satisfactory to the patient as a main objective of treatment as well as completely, or near completely, eliminating ischemic symptoms. Furthermore, prior studies have demonstrated that health status and QOL are strong predictors of long-term outcomes in patients with CAD.22 Therefore, national performance metrics have started incorporating patient perception of health and functional status, QOL measures, and satisfaction scores.24 Our study sheds light on the evolution of symptoms of patients with stable CAD who have normal perfusion and LVEF on MPI.
While it has been demonstrated that PCI reduces death and MI in patients presenting with ACS25,26 similar benefit has not been observed in those with stable CAD.27,28,29 Large clinical trials in patients with stable CAD have shown that optimal medical therapy, as an initial management strategy, without routine CR can be implemented safely in most patients.27,28 Stress testing with MPI is often used for risk stratification in patients with stable CAD5 and there is ample evidence that a normal MPI confers a low risk of adverse cardiac events in the short, intermediate, and long terms, and that these patients can be managed conservatively without CR.5,6,7,8,30,31,32 Therefore, it is possible to reassure patients who have a normal MPI regarding their overall prognosis.
Management Strategies of Stable Angina
Both medical therapy and CR have been shown to be effective at ameliorating angina in patients with stable CAD.27 Current guidelines recommend anti-ischemic medications as first-line treatment for relief of symptoms with CR reserved for patients who have unacceptable symptoms on medical therapy and in those who cannot tolerate medical therapy.23 A recent controversial blinded, randomized placebo-controlled trial cast doubt on the use of PCI even as second line therapy for relief of angina.33,34 However, in the large International Study of Comparative Health Effectiveness with Medical and Invasive Approaches (ISCHEMIA) trial of patients with stable CAD and at least moderate ischemia, participants who were randomized to the invasive arm (with coronary revascularization when feasible) experienced larger improvement in symptom burden and QOL than those assigned to the conservative arm.35
Clinical Value of Normal MPI in Stable Angina Patients
Our study suggests that patients presenting with chest pain who undergo MPI and have normal perfusion can be reassured that their symptoms are likely to improve over time in the absence of medication uptitration or CR. Our study used the SAQ to assess symptom burden. First introduced in 1994 by Spertus et al, the SAQ is the leading health-related QOL measure for patients with CAD.10,36 This tool has been used in numerous clinical trials that track patient symptom status.35,37,38,39,–40 In our prospective cohort of patients with chest pain who have normal stress MPI, serially administered SAQs showed statistically significant improvement in 4 of the 5 categories including physical limitation, angina stability, angina frequency, and disease perception over a 3-month follow-up. This magnitude of change is considered clinically significant (Figure 2).10 The only scale that did not demonstrate a significant change, the treatment satisfaction scale, was high at baseline and this may have prevented the detection of any improvement over time. It is notable that despite the high score at baseline, no deterioration in the score occurred during follow-up.
Our longitudinal findings provide data suggesting that patient-perceived symptoms improve significantly in the short term in patients with stable angina who have normal perfusion on imaging. These changes occurred even in the absence of intensification of medical treatment or CR. In addition to reassuring patients and providers regarding the evolution of symptoms after stress testing, our study provides important data that can inform future research focused on symptom perception and evolution.
Limitations
First, we used telephone follow-up at 3 months instead of in-person administration of the SAQ. This was done in order to improve loss to follow-up as much as possible. We attempted to mitigate reporting bias by informing patients that responses would not be disclosed to their physicians and would not affect clinical management. Second, our assessment was based on patient assessment of their symptoms at 2 time points (baseline and 3 months) rather than based on a daily angina assessment introducing potential recall bias. Prior reports have demonstrated that the SAQ has excellent correlation with daily diary angina entries.18 Third, our study did not include a ‘no MPI’ arm (i.e., a control group) due to ethical concerns of withholding a clinically indicated test from symptomatic patients. It is therefore difficult to speculate whether the change in symptom burden that we have seen would have been different had the patients not underwent the stress test. In this regard, it is important to note that the symptoms reported at baseline had a chronic component as evidenced by the angina stability scale. Therefore, the change in symptomatology seen in our study may not have been related to the normal MPI (especially in the absence of CR or intensification of medical therapy), but rather due to the natural course of these patients. Nevertheless, it is important to understand the evolution of symptoms over time in patients who have a normal MPI irrespective of the causative factor. Fourth, we did not collect data on the character of the chest pain and therefore are unable to comment on differences between patients experiencing typical angina, atypical angina, and non-anginal chest pain.
New Knowledge Gained
This study suggests that patients with chest pain who have normal MPI as part of a clinical care diagnostic pathway can be reassured that they will experience clinically meaningful improvement in their symptoms in the short term even in the absence of uptitration of anti-anginal medications or CR. Importantly, one-third of symptomatic patients referred for MPI who have a normal study become symptom free within 3 months.
Abbreviations
- MPI:
-
Myocardial perfusion imaging
- QOL:
-
Quality of life
- CAD:
-
Coronary artery disease
- SAQ:
-
Seattle Angina Questionnaire
- CR:
-
Coronary revascularization
- ACS:
-
Acute coronary syndrome
- MI:
-
Myocardial infarction
- PCI:
-
Percutaneous coronary intervention
- CABG:
-
Coronary artery bypass grafting
- LVEF:
-
Left ventricular ejection fraction
References
Ladapo JA, Blecker S, Douglas PS. Physician decision making and trends in the use of cardiac stress testing in the United States: An analysis of repeated cross-sectional data. Ann Intern Med 2014;161:482-90.
Nawar EW, Niska RW, National XuJ, Survey Hospital Ambulatory Medical Care. emergency department summary. Adv Data 2005;2007:1-32.
Writing Group M, Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, et al. Heart disease and stroke statistics-2016 update: A report from the American Heart Association Circulation 2016;133:e38-360.
Mettler FA, Guiberteau MJ. Essentials of nuclear medicine imaging; 2012.
Shaw LJ, Hage FG, Berman DS, Hachamovitch R, Iskandrian A. Prognosis in the era of comparative effectiveness research: Where is nuclear cardiology now and where should it be? J Nucl Cardiol 2012;19:1026-43.
Hachamovitch R, Hayes S, Friedman JD, Cohen I, Shaw LJ, Germano G, et al. Determinants of risk and its temporal variation in patients with normal stress myocardial perfusion scans: What is the warranty period of a normal scan? J Am Coll Cardiol 2003;41:1329-40.
Iqbal FM, Hage FG, Ahmed A, Dean PJ, Raslan S, Heo J, et al. Comparison of the prognostic value of normal regadenoson with normal adenosine myocardial perfusion imaging with propensity score matching. JACC Cardiovasc Imaging 2012;5:1014-21.
Hage FG, Ghimire G, Lester D, McKay J, Bleich S, El-Hajj S, et al. The prognostic value of regadenoson myocardial perfusion imaging. J Nucl Cardiol 2015;22:1214-21.
Mark DB. Assessing quality-of-life outcomes in cardiovascular clinical research. Nat Rev Cardiol 2016;13:286-308.
Spertus JA, Winder JA, Dewhurst TA, Deyo RA, Prodzinski J, McDonell M, et al. Development and evaluation of the Seattle Angina Questionnaire: A new functional status measure for coronary artery disease. J Am Coll Cardiol 1995;25:333-41.
Henzlova MJ, Duvall WL, Einstein AJ, Travin MI, Verberne HJ. ASNC imaging guidelines for SPECT nuclear cardiology procedures: Stress, protocols, and tracers. J Nucl Cardiol 2016;23:606-39.
Andrikopoulou E, AlJaroudi WA, Farag A, Lester D, Patel H, Iskandrian AE, et al. The reproducibility and prognostic value of serial measurements of heart rate response to regadenoson during myocardial perfusion imaging. Eur J Nucl Med Mol Imaging 2016;43:1493-502.
Al Jaroudi W, Iskandrian AE. Regadenoson: A new myocardial stress agent. J Am Coll Cardiol 2009;54:1123-30.
Lester D, El-Hajj S, Farag AA, Bhambhvani P, Tauxe L, Heo J, et al. Prognostic value of transient ischemic dilation with regadenoson myocardial perfusion imaging. J Nucl Cardiol 2016;23:1147-55.
Ficaro EP, Lee BC, Kritzman JN, Corbett JR. Corridor4DM: The Michigan method for quantitative nuclear cardiology. J Nucl Cardiol 2007;14:455-65.
Germano G, Kiat H, Kavanagh PB, Moriel M, Mazzanti M, Su HT, et al. Automatic quantification of ejection fraction from gated myocardial perfusion SPECT. J Nucl Med 1995;36:2138-47.
Kimble LP, Dunbar SB, Weintraub WS, McGuire DB, Fazio S, De AK, et al. The Seattle angina questionnaire: Reliability and validity in women with chronic stable angina. Heart Dis 2002;4:206-11.
Arnold SV, Kosiborod M, Li Y, Jones PG, Yue P, Belardinelli L, et al. Comparison of the seattle angina questionnaire with daily angina diary in the TERISA clinical trial. Circ Cardiovasc Qual Outcomes 2014;7:844-50.
Bhuiya FA, Pitts SR, McCaig LF. Emergency department visits for chest pain and abdominal pain: United States, 1999-2008. NCHS Data Brief 2010:1-8
Plomondon ME, Magid DJ, Masoudi FA, Jones PG, Barry LC, Havranek E, et al. Association between angina and treatment satisfaction after myocardial infarction. J Gen Intern Med 2008;23:1-6.
Maddox TM, Reid KJ, Spertus JA, Mittleman M, Krumholz HM, Parashar S, et al. Angina at 1 year after myocardial infarction: Prevalence and associated findings. Arch Intern Med 2008;168:1310-6.
Spertus JA, Jones P, McDonell M, Fan V, Fihn SD. Health status predicts long-term outcome in outpatients with coronary disease. Circulation 2002;106:43-9.
Fihn SD, Gardin JM, Abrams J, Berra K, Blankenship JC, Dallas AP, et al. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS Guideline for the diagnosis and management of patients with stable ischemic heart disease: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol 2012;60:e44-164.
Spertus JA. Evolving applications for patient-centered health status measures. Circulation 2008;118:2103-10.
Antman EM, Anbe DT, Armstrong PW, Bates ER, Green LA, Hand M, et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction; A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 Guidelines for the Management of patients with acute myocardial infarction). J Am Coll Cardiol 2004;44:E1-211.
Mehta SR, Cannon CP, Fox KA, Wallentin L, Boden WE, Spacek R, et al. Routine vs selective invasive strategies in patients with acute coronary syndromes: A collaborative meta-analysis of randomized trials. JAMA 2005;293:2908-17.
Boden WE, O’Rourke RA, Teo KK, Hartigan PM, Maron DJ, Kostuk WJ, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med 2007;356:1503-16.
Group BDS, Frye RL, August P, Brooks MM, Hardison RM, Kelsey SF, et al. A randomized trial of therapies for type 2 diabetes and coronary artery disease. N Engl J Med 2009;360:2503-15.
Maron DJ, Hochman JS, Reynolds HR, Bangalore S, O’Brien SM, Boden WE, et al. Initial Invasive or Conservative Strategy for Stable Coronary Disease. N Engl J Med 2020;382:1395-407.
Acampa W, Cantoni V, Green R, Maio F, Daniele S, Nappi C et al. Prognostic value of normal stress myocardial perfusion imaging in diabetic patients: A meta-analysis. J Nucl Cardiol 2014;21:893-902; quiz 890-2, 903-5.
Simonsen JA, Gerke O, Rask CK, Tamadoni M, Thomassen A, Hess S, et al. Prognosis in patients with suspected or known ischemic heart disease and normal myocardial perfusion: Long-term outcome and temporal risk variations. J Nucl Cardiol 2013;20:347-57.
Iskander S, Iskandrian AE. Risk assessment using single-photon emission computed tomographic technetium-99m sestamibi imaging. J Am Coll Cardiol 1998;32:57-62.
Al-Lamee R, Thompson D, Dehbi HM, Sen S, Tang K, Davies J, et al. Percutaneous coronary intervention in stable angina (ORBITA): A double-blind, randomised controlled trial. Lancet 2017;391:31-40.
Dilsizian V, Erario M. Is exercise treadmill time or reduction in myocardial ischemia the appropriate primary endpoint to assess success of percutaneous coronary intervention in stable angina (ORBITA)? J Nucl Med 2018;59:1-2.
Spertus JA, Jones PG, Maron DJ, O’Brien SM, Reynolds HR, Rosenberg Y, et al. Health-status outcomes with invasive or conservative care in coronary disease. N Engl J Med 2020;382:1408-19.
Spertus JA, Winder JA, Dewhurst TA, Deyo RA, Fihn SD. Monitoring the quality of life in patients with coronary artery disease. Am J Cardiol 1994;74:1240-4.
Burkhoff D, Schmidt S, Schulman SP, Myers J, Resar J, Becker LC, et al. Transmyocardial laser revascularisation compared with continued medical therapy for treatment of refractory angina pectoris: A prospective randomised trial. ATLANTIC Investigators. Angina Treatments-Lasers and Normal Therapies in Comparison. Lancet 1999;354:885-90.
Holmboe ES, Fiellin DA, Cusanelli E, Remetz M, Krumholz HM. Perceptions of benefit and risk of patients undergoing first-time elective percutaneous coronary revascularization. J Gen Intern Med 2000;15:632-7.
Kimble LP, Kunik CL. Knowledge and use of sublingual nitroglycerin and cardiac-related quality of life in patients with chronic stable angina. J Pain Symptom Manage 2000;19:109-17.
MacDonald P, Stadnyk K, Cossett J, Klassen G, Johnstone D, Rockwood K. Outcomes of coronary artery bypass surgery in elderly people. Can J Cardiol 1998;14:1215-22.
Disclosures
Dr. Hage reports research Grant support from Astellas Pharma and GE Healthcare. Drs. McRee, Brice, Farag, and Iskandrian report no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
McRee, C.W., Brice, L.R., Farag, A.A. et al. Evolution of symptoms in patients with stable angina after normal regadenoson myocardial perfusion imaging: The Radionuclide Imaging and Symptomatic Evolution study (RISE). J. Nucl. Cardiol. 29, 612–621 (2022). https://doi.org/10.1007/s12350-020-02298-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-020-02298-8