Abstract
Stable chest pain is a common symptom with multiple potential causes. Non-invasive imaging has an important role in diagnosis and guiding management through the assessment of coronary stenoses, atherosclerotic plaque, myocardial ischaemia or infarction, and cardiac function. Computed tomography (CT) provides the anatomical evaluation of coronary artery disease (CAD) with the assessment of stenosis, plaque type and plaque burden, with additional functional information available from CT fractional flow reserve (FFR) or CT myocardial perfusion imaging. Stress magnetic resonance imaging, nuclear stress myocardial perfusion imaging, and stress echocardiography can assess myocardial ischaemia and other cardiac functional parameters. Coronary CT angiography can be used as a first-line test for many patients with stable chest pain, particularly those with low to intermediate pre-test probability. Functional testing may be considered for patients with known CAD, where the clinical significance is uncertain based on anatomical testing, or in patients with high pre-test probability. This practice recommendations document can be used to guide the selection of non-invasive imaging for patients with stable chest pain and provides brief recommendations on how to perform and report these diagnostic tests.
Key Points
-
The selection of non-invasive imaging tests for patients with stable chest pain should be based on symptoms, pre-test probability, and previous history.
-
Coronary CT angiography can be used as a first-line test for many patients with stable chest pain, particularly those with low to intermediate pre-test probability.
-
Functional testing can be considered for patients with known CAD, where the clinical significance of CAD is uncertain based on anatomical testing, or in patients with high pre-test probability.
Key recommendations
-
Non-invasive imaging is an important part of the assessment of patients with stable chest pain. The selection of non-invasive imaging test should be based on symptoms, pre-test probability, and previous history. (Level of evidence: High).
-
Coronary CT angiography can be used as a first line test for many patients with stable chest pain, particularly those with low to intermediate pre-test probability. CT provides information on stenoses, plaque type, plaque volume, and if required functional information with CT fractional flow reserve or CT perfusion. (Level of evidence: High).
-
Functional testing can be considered for patients with known CAD, where the clinical significance of CAD is uncertain based on anatomical testing, or in patients with high pre-test probability. Stress MRI, SPECT, PET, and echocardiography can provide information on myocardial ischemia, along with cardiac functional and other information. (Level of evidence: Medium).
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Stable chest pain is a common presenting symptom with multiple potential causes, including coronary artery disease (CAD) and diseases of other structures such as the lungs, mediastinum, and gastrointestinal tract. Stable chest pain refers to a relatively consistent and non-emergent pattern of chest discomfort or pressure, that may be associated with other symptoms and may occur predictably during exertion and subsides with rest. CAD remains one of the most common diseases worldwide and is associated with high morbidity and mortality.
The assessment of patents with stable chest pain suspected to be of coronary origin frequently involves non-invasive imaging. Coronary computed tomography angiography (CCTA) provides information on coronary stenosis, plaque type and plaque burden, and can be used as a first-line test for many patients with stable chest pain. Functional tests, such as stress magnetic resonance imaging (MRI), single photon emission computed tomography (SPECT), positron emission tomography (PET), and echocardiography can provide additional information on myocardial ischaemia and other cardiac functional parameters and can be useful in patients with known CAD or if the diagnosis is uncertain based on anatomical testing.
This practice recommendations document can be used to guide the selection of non-invasive imaging for patients with stable chest pain and provides brief recommendations on how to perform and report these diagnostic tests. The level of evidence for statements is indicated by ** for multi-centre studies and * for single-centre studies.
Assessment of patients with stable chest pain
The clinical assessment of patients with stable chest pain includes history, examination, and assessment of the pre-test probability of obstructive coronary artery disease. Resting electrocardiogram, blood tests, and chest x-ray may also be performed depending on the suspected diagnosis. Various methods are available to assess the pre-test probability of obstructive coronary artery disease, which have been optimised for different patient groups around the world (Fig. 1). They are usually based on age, sex, and symptoms, with additional factors that may be considered including the presence of cardiovascular risk factors, electrocardiogram abnormalities, or CT coronary artery calcium score. Together this information is used to identify which patients would benefit from further assessment with non-invasive imaging. Several guidelines exist for the assessment of stable chest pain [1,2,3] that share common core elements with some variations (Supplementary Table 1, Fig. 1).
How to choose an imaging test
CCTA can be used as a first line test for many patients with stable chest pain, particularly those with low to intermediate (10–60%) pre-test probability (**). Large randomised controlled trials (RCTs) have assessed the prognostic implications and ability to improve patient outcomes based on the assessment of coronary stenoses on CCTA. The prospective multicenter imaging study for evaluation of chest pain (PROMISE) RCT of 10,003 patients showed similar outcomes in patients undergoing initial CCTA compared to functional testing [4]. The Scottish Computed Tomography of the HEART (SCOT-HEART) RCT of 4146 patients showed that CCTA changed management compared to routine evaluation and led to a reduction in fatal or non-fatal myocardial infarction after 5 years [5]. The diagnostic imaging strategies for patients with stable chest pain and intermediate risk of coronary artery disease (DISCHARGE) RCT of 3561 patients showed that major adverse cardiovascular events (MACE) were similar with CT compared to invasive coronary angiography (ICA) guided management, with fewer major procedure-related complications from CT [6]. Together these studies support the use of CCTA to guide management in patients with stable chest pain.
Functional testing can be useful for patients with known CAD or where the clinical significance is uncertain based on anatomical testing alone or in patients with high pre-test probability (**). Prior imaging may help guide selection of appropriate tests. Further considerations which may influence selection of appropriate imaging tests are the presence of known CAD, factors that may influence image quality such as body mass index, and local availability and expertise. No or deferred testing may be appropriate for low-risk patients. At present SPECT is the most used method to assess myocardial perfusion with CT perfusion the least common [7]. Stress cardiac MRI does not expose the patient ionising radiation and PET is the reference standard for quantitative myocardial perfusion imaging [7].
Strengths and weaknesses of available imaging modalities
All diagnostic tests have strengths and weaknesses (Table 1) and can provide different information on the presence, characteristics, and severity of CAD.
The two major techniques for direct imaging of coronary arteries are CCTA and ICA. The main advantages of CCTA over ICA include its non-invasive nature, lower rate of procedural complications, broad availability, lower cost, and standardised robust evaluation [6] (**). In addition, intravenous iodinated contrast used for CCTA is associated with lower rates of contrast-associated acute kidney injury (5.6%) than the intra-arterial iodinated contrast used during ICA (13.2%), particularly if femoral access or cine ventriculography is performed during ICA [8] (*). ICA should be reserved for patients likely to benefit from revascularisation. During ICA, assessment of pressure gradients, intravascular ultrasound (IVUS), or optical coherence tomography (OCT) may increase the accuracy of stenosis gradation and plaque characterisation.
Morphological assessment of luminal diameter does not necessarily reflect hemodynamic significance and assessment of downstream consequences on perfusion may be required, including stress MRI, SPECT, PET, or echocardiography. Haemodynamic information can also be acquired from CT with CT perfusion imaging or CT FFR. Stress echocardiography is widely available but is limited by observer variability. Stress MRI is a robust technique with large studies establishing its diagnostic accuracy [9]; however, scanners are less widely available, and MRI is contra-indicated in patients with certain metal implants. PET and SPECT are established techniques to identify myocardial ischaemia, with PET providing better temporal and spatial resolution, accuracy, and the ability to quantify myocardial blood flow.
Application of non-invasive anatomical testing
Image acquisition with CT
Cardiac CT requires a 64 or greater multi-detector CT scanner with electrocardiogram synchronisation. Patient preparation includes pre-medication as appropriate with beta-blockers to reduce heart rate to a target of 60 beats per minute and reduce heart rate variability (Table 2). Nitroglycerin for coronary vasodilation is used to optimise image quality. More detailed information on image acquisition is available in the ESCR “How I do it” guide (https://www.escr.org). Example reports are provided in Supplementary Table 2. Images are acquired during suspended respiration with prospective or retrospective electrocardiogram synchronisation and iodinated contrast. Cardiac reconstructions at several time points and wide field of view images are generated. Prior to CCTA acquisition a non-contrast electrocardiogram gated CT to assess calcium score may be acquired depending on local practice, as this can be used to guide CCTA scan range and acquisition parameters and provide a quantitative coronary artery calcium score. However, in symptomatic patients, calcium score alone is not enough for the evaluation of CAD.
Coronary stenosis on CCTA
Coronary stenoses can be visually assessed in each segment using multiplanar and curved planar reformations. Per segment diameter stenosis can be graded visually as none, minimal (< 25%), mild (25–50%), moderate (50–70%), severe (> 70%), or occluded (Fig. 2). CCTA has excellent diagnostic accuracy compared to the gold standard of ICA for the identification of coronary stenosis, with a particularly good negative predictive value. In a large meta-analysis, the pooled sensitivity and specificity on a per segment level for the identification of > 50% stenosis were 91% and 96%, respectively [10].
Anatomical assessment with coronary CT angiography in patients with stable chest pain showing curved planar reformations from different patients. A shows a normal coronary artery where the patient was discharged from the clinic. B shows minor (< 25%) and (C) shows mild (< 50%) stenosis where the recommendations would be for preventive therapy. D shows moderate (50–70%) stenosis where the recommendation was for preventive therapy. E shows severe (> 70%) in a patient who subsequently underwent coronary artery bypass grafting. Examples of visually assessed high-risk plaque (arrows) showing (F) spotty calcification, (G) positive remodelling, (H) low attenuation plaque and (I) the napkin ring sign. Two or more high-risk plaque features are an indication for more aggressive medical management, such as lower cholesterol targets for preventive therapy
Coronary plaque assessment on CCTA
Recently, the management of patients with CAD has moved beyond the identification of coronary stenosis to incorporate other aspects of atherosclerosis. The most basic assessment of plaque type is based on attenuation and classifies plaques as calcified, non-calcified, or mixed. Visually assessed high-risk plaque features include positive remodelling, low attenuation plaque, spotty calcifications, and the napkin ring sign (Fig. 2). Positive remodelling describes outward vessel diameter enlargement at the level of a lesion (outer vessel diameter at lesion/the average of the outer diameter of the proximal and distal vessel > 1.1, Fig. 2). Low attenuating plaque is associated with a necrotic core of rupture-prone plaques. Large calcifications are characteristic of advanced disease, and spotty calcifications (< 3 mm) are associated with high-risk plaque. The napkin ring sign describes a combination of positive remodelling, low attenuation plaque and a high attenuation rim which may represent micro-calcification, dissection, or inflammation. Recent studies have shown that 2 or more high-risk plaque features are associated with an increased risk of MACE and their presence could guide the use of more aggressive medical management, such as lower cholesterol targets for preventive therapy [11, 12] (**).
To account for the diffuse nature of CAD, the amount of plaque can be assessed across the coronary tree and can be visually assessed and described as mild, moderate, or severe. Alternately, quantification can be performed using semi-quantitative scores, calcium score, or other quantitative evaluation. Coronary calcium score can be measured on non-contrast CT using the Agatston method. A higher calcium score is associated with an increased risk of subsequent cardiac events, but its diagnostic utility in patients with stable chest pain is debated. Several visual semi-quantitative scores are available for CCTA, with similar prognostic utility [13] (**). CCTA results can also be summarised using the Coronary Artery Disease—data and reporting system (CAD-RADS) [14]. Software tools are also available for the semi-automatic quantification of plaque volume and type on CCTA, and research into how to incorporate this information into clinical practice is emerging.
Application of functional testing
Evaluation of cardiac function and ischaemia
Functional testing in CAD involves the incorporation of multiple complimentary pieces of information regarding cardiac function and ischaemia which can be assessed with stress echocardiography, MRI, SPECT, or PET (Figs. 3, 4).
The most fundamental measurement of cardiac function is ejection fraction, which determines if systolic dysfunction is present. This is complimented by an assessment of regional wall motion abnormalities at rest which may indicate infarction, or during stress which may indicate ischaemia. These can be graded as hypokinetic, akinetic, or dyskinetic and reported following a 17 segment model. MRI also provides information on the absence of wall thickening during systole which may also indicate infarction. However, diagnostic accuracy of these assessments to identify ischaemia is low.
Myocardial ischaemia can be assessed with SPECT, PET, MRI, CT, or echocardiography. Physiological (exercise) or pharmacological stress (adenosine, regadenoson or dipyridamole, Table 2) imaging is performed +/− rest imaging. More detailed information on MRI image acquisition is available in the ESCR “How I do it” guide (https://www.escr.org). Example reports are provided in Supplementary Table 3. Perfusion defects are reported with a 17-segment myocardial model. Inducible ischaemia is present if there is a stress perfusion defect within a coronary territory which is not present at rest. Infarction may be present when the defect persists on stress and rest imaging. Ischaemia and no obstructive coronary arteries (INOCA) can also be identified with functional testing and is an important cause of morbidity and mortality.
Qualitative visual inspection of perfusion can be complimented by quantitative analysis of blood flow. Currently, this is mostly performed using PET, but it is also possible with dedicated MRI sequences and dynamic CTP. Myocardial perfusion reserve (MPR) can be calculated (stress/rest blood flow), with MPR < 2 indicating inducible ischaemia in a recent meta-analysis [15]. MPR is particularly useful for the detection of balanced ischaemia due to severe three vessel disease and microvascular dysfunction [16] (*).
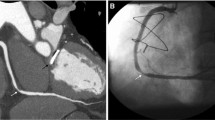
Where CT has been performed as the first-line test, the functional significance of stenosis can also be assessed using simulated fractional flow reserve derived from coronary anatomy (CT FFR) or by using CT perfusion. CT FFR can be performed on any CCTA with adequate image quality. CT perfusion is easier to perform with the latest generation of wide volume or dual-source scanners. CT FFR showed high agreement when compared with invasive fractional flow reserve in a meta-analysis [17]. CT FFR should be measured approximately 2 cm distal to the stenosis of interest, with a CT FFR ≤ 0.8 indicative of lesion-specific flow restriction. Those with a CT-FFR > 0.8 have low rates of cardiovascular events in a meta-analysis [18] and can be deferred from further invasive testing. Myocardial perfusion can be assessed with CT using both static and dynamic protocols and has good accuracy and prognostic ability compared to gold standard assessments [19] (Fig. 5) (**).
Assessment of coronary artery disease with coronary CT angiography. Images A–E A sixty-year-old male with dyspnoea and chest pain. CCTA shows no significant coronary stenosis in left anterior descending artery (A) and left circumflex artery (B). The right coronary artery showed severe stenosis due to calcified plaque in the mid vessel (C, arrow). Dynamic stress CT perfusion imaging was performed for the evaluation of myocardial ischaemia. A deficit of myocardial perfusion was observed in the inferoseptal mid-ventricular segment (D, arrowhead). Severe stenosis in the right coronary artery was confirmed on invasive coronary angiography and treated with percutaneous coronary intervention (E, arrow)
Assessment of myocardial viability
Myocardial viability can be assessed on MRI using late gadolinium enhancement (LGE), which can also be used to assess for fibrosis or infiltration diseases. Myocardial viability assessment may be particularly useful when there are resting wall motion abnormalities or a matched stress perfusion defect. Subendocardial LGE is indicative of prior myocardial infarction with maintained viability, with LGE involving > 50% of the myocardial wall thickness indicating non-viability [20] (**) (Supplementary Table 3).
Additional considerations
Percutaneous and surgical revascularisation
Prior coronary artery stenting or coronary artery bypass grafting (CABG) can cause challenges in the selection and analysis of non-invasive testing. Both myocardial perfusion imaging and CT assessment can be performed for patients with previous revascularisation, but test selection depends on patient and technical factors.
The most important indication to evaluate coronary stents is the exclusion of in-stent restenosis (ISR). ISR rates have declined over progressive stent generations, but remain a clinical issue with diverse aetiology [21]. Stent size, location, and material can all influence the ability of CT assessment; adequate spatial resolution is paramount to confirm stent patency, and only stents with > 3 mm diameter are generally considered suitable for evaluation with current CT technology [22]. Anatomical stent configuration also determines accuracy of evaluation, favouring proximal, non-bifurcation stents. However, lumen visualisation can be improved by applying a sharper kernel and appropriate windowing. A previous meta-analysis showed that 89% of stents were interpretable with CCTA [23]—this will improve with newer high-resolution scanners [24].
Assessment of coronary artery bypass grafts with CT requires a longer field of view, starting just below the clavicles so the origins of the internal mammary arteries are visualised. Several graft configurations can be encountered depending on the indication and surgical preference [25]. Evaluation of graft patency can be impacted by size and the presence of adjacent surgical material, with large surgical clips producing significant beam hardening artefacts. Overall, a meta-analysis showed 96% sensitivity and specificity for graft evaluation with CT, which is slightly higher for venous compared to arterial grafts [26].
Future considerations
Photon counting CT (PCCT) may improve CAD assessment, particularly in patients with severe coronary calcifications, through improved resolution imaging, particularly in patients with severe coronary calcification, and material decomposition analysis of plaque components [27]. Quantitative analysis of CCTA provides a more robust assessment of coronary plaque burden and subtype, and machine learning tools may aid the speed of this assessment [28]. Assessment of pericoronary adipose tissue (PCAT, the fat surrounding the coronary arteries) attenuation, and epicardial adipose tissue (the fat surrounding the heart) may also improve the assessment of cardiovascular risk [29, 30]. Advanced uses of SPECT and PET imaging include new radiotracers for perfusion and plaque assessment and the use of new technology such as PET-MRI systems or Total Body PET scanners. For MRI, new sequences are being developed that automate acquisition, reduce acquisition times, enable non-contrast assessment, and facilitate quantitative perfusion.
Summary statement
Non-invasive imaging tests are an important part of the evaluation of patients with stable chest pain. CT can provide anatomical evaluation of CAD with assessment of stenosis, plaque type and plaque burden, with additional functional information available from CT FFR or CTP. Stress MRI, SPECT, PET, and echocardiography can assess myocardial ischaemia and other cardiac functional parameters. It is important to carefully evaluate the most appropriate technique(s) for each patient. CCTA can be used as a first-line test for many patients with stable chest pain, particularly those with low to intermediate pre-test probability. Functional testing may be considered for patients with known CAD, where the clinical significance is uncertain based on anatomical testing, or in patients with high pre-test probability.
Patient statement
The diagnosis of heart disease is important to enable treatment and prevent the risk of future heart attacks. Several types of scans for heart disease are available that can provide different information. Computed tomography scans provide information on narrowing in the blood vessels that supply the heart and the cause of these narrowings. Other tests such as magnetic resonance imaging and nuclear medicine tests provide information on the blood flow to the heart muscle, along with other information. The choice of imaging test depends on a patient’s symptoms, risk factors and previous medical history, and in some cases, more than one test is required. The information from these tests can suggest whether a patient will benefit from medication or other treatments for coronary artery disease.
Change history
22 April 2024
Source Line layout was corrected.
07 May 2024
Correction of minor typographical error in guest editor’s name.
Abbreviations
- CAD:
-
Coronary artery disease
- CCTA:
-
Coronary computed tomography angiography
- FFR:
-
Fractional flow reserve
- ICA:
-
Invasive coronary angiography
- IVUS:
-
Intravascular ultrasound
- MACE:
-
Major adverse cardiovascular events
- OCT:
-
Optical coherence tomography
References
Knuuti J, Wijns W, Saraste A et al (2020) 2019 ESC guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J 41:407–477
Writing Committee M, Gulati M, Levy PD et al (2022) 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guideline for the evaluation and diagnosis of chest pain: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. J Cardiovasc Comput Tomogr 16:54–122
Recent-onset chest pain of suspected cardiac origin: assessment and diagnosis. https://www.niceorguk/guidance/cg95
Douglas PS, Hoffmann U, Patel MR et al (2015) Outcomes of anatomical versus functional testing for coronary artery disease. N Engl J Med 372:1291–1300
Investigators S-H, Newby DE, Adamson PD et al (2018) Coronary CT angiography and 5-year risk of myocardial infarction. N Engl J Med 379:924–933
Group DT, Maurovich-Horvat P, Bosserdt M et al (2022) CT or invasive coronary angiography in stable chest pain. N Engl J Med 386:1591–1602
Dewey M, Siebes M, Kachelriess M et al (2020) Clinical quantitative cardiac imaging for the assessment of myocardial ischaemia. Nat Rev Cardiol 17:427–450
Schonenberger E, Martus P, Bosserdt M et al (2019) Kidney injury after intravenous versus intra-arterial contrast agent in patients suspected of having coronary artery disease: a randomised trial. Radiology 292:664–672
Le Ven F, Pontana F, Barone-Rochette G et al (2021) Position paper on stress cardiac MRI in chronic coronary syndrome: endorsed by the Societe Francaise de Radiologie (SFR) the Societe Francaise d’Imagerie CardioVasculaire (SFICV) and the Societe Francaise de Cardiologie (SFC). Diagn Interv Imaging 102:337–345
von Ballmoos MW, Haring B, Juillerat P, Alkadhi H (2011) Meta-analysis: diagnostic performance of low-radiation-dose coronary computed tomography angiography. Ann Intern Med 154:413–420
Williams MC, Moss AJ, Dweck M et al (2019) Coronary artery plaque characteristics associated with adverse outcomes in the SCOT-HEART study. J Am Coll Cardiol 73:291–301
Puchner SB, Liu T, Mayrhofer T et al (2014) High-risk plaque detected on coronary CT angiography predicts acute coronary syndromes independent of significant stenosis in acute chest pain: results from the ROMICAT-II trial. J Am Coll Cardiol 64:684–692
Maclean E, Cronshaw R, Newby DE, Nicol E, Williams MC (2023) Prognostic utility of semi-quantitative coronary computed tomography angiography scores in the SCOT-HEART trial. J Cardiovasc Comput Tomogr. https://doi.org/10.1016/j.jcct.2023.08.009
Cury RC, Blankstein R, Leipsic J et al (2022) CAD-RADS 2.0 - 2022 Coronary Artery Disease - reporting and data system an expert consensus document of the Society of Cardiovascular Computed Tomography (SCCT), the American College of Cardiology (ACC), the American College of Radiology (ACR) and the North America society of cardiovascular imaging (NASCI). J Cardiovasc Comput Tomogr. https://doi.org/10.1016/j.jcct.2022.07.002
Green R, Cantoni V, Acampa W et al (2021) Prognostic value of coronary flow reserve in patients with suspected or known coronary artery disease referred to PET myocardial perfusion imaging: a meta-analysis. J Nucl Cardiol 28:904–918
Murthy VL, Naya M, Foster CR et al (2011) Improved cardiac risk assessment with noninvasive measures of coronary flow reserve. Circulation 124:2215–2224
Celeng C, Leiner T, Maurovich-Horvat P et al (2019) Anatomical and functional computed tomography for diagnosing hemodynamically significant coronary artery disease. A Meta-Analysis. JACC Cardiovasc Imaging 12:1316–1325
Norgaard BL, Gaur S, Fairbairn TA et al (2022) Prognostic value of coronary computed tomography angiographic derived fractional flow reserve: a systematic review and meta-analysis. Heart 108:194–202
Chen MY, Rochitte CE, Arbab-Zadeh A et al (2017) Prognostic value of combined CT angiography and myocardial perfusion imaging versus invasive coronary angiography and nuclear stress perfusion imaging in the prediction of major adverse cardiovascular events: the CORE320 multicenter study. Radiology 284:55–65
Shah DJ, Kim HW, James O et al (2013) Prevalence of regional myocardial thinning and relationship with myocardial scarring in patients with coronary artery disease. JAMA 309:909–918
Torrado J, Buckley L, Duran A et al (2018) Restenosis, stent thrombosis, and bleeding complications: navigating between Scylla and Charybdis. J Am Coll Cardiol 71:1676–1695
Narula J, Chandrashekhar Y, Ahmadi A et al (2021) SCCT 2021 expert consensus document on coronary computed tomographic angiography: a report of the Society of Cardiovascular Computed Tomography. J Cardiovasc Comput Tomogr 15:192–217
Sun Z, Almutairi AM (2010) Diagnostic accuracy of 64 multislice CT angiography in the assessment of coronary in-stent restenosis: a meta-analysis. Eur J Radiol 73:266–273
Geering L, Sartoretti T, Mergen V et al (2023) First in-vivo coronary stent imaging with clinical ultra high resolution photon-counting CT. J Cardiovasc Comput Tomogr 17:233–235
Hillis LD, Smith PK, Anderson JL et al (2011) 2011 ACCF/AHA guideline for coronary artery bypass graft surgery: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation 124:e652–e735
Chan M, Ridley L, Dunn DJ et al (2016) A systematic review and meta-analysis of multidetector computed tomography in the assessment of coronary artery bypass grafts. Int J Cardiol 221:898–905
Mergen V, Sartoretti T, Baer-Beck M et al (2022) Ultra-high-resolution coronary CT angiography with photon-counting detector CT: feasibility and image characterization. Invest Radiol 57:780–788
Williams MC, Kwiecinski J, Doris M et al (2020) Low-attenuation noncalcified plaque on coronary computed tomography angiography predicts myocardial infarction: results from the multicenter SCOT-HEART trial (Scottish Computed Tomography of the HEART). Circulation 141:1452–1462
Tzolos E, Williams MC, McElhinney P et al (2022) Pericoronary adipose tissue attenuation, low-attenuation plaque burden, and 5-year risk of myocardial infarction. JACC Cardiovasc Imaging 15:1078–1088
Eisenberg E, McElhinney PA, Commandeur F et al (2020) Deep learning-based quantification of epicardial adipose tissue volume and attenuation predicts major adverse cardiovascular events in asymptomatic subjects. Circ Cardiovasc Imaging 13:e009829
Acknowledgements
This paper was endorsed by the Executive Council of the European Society of Radiology (ESR) and the Executive Committee of the European Society of Cardiovascular Radiology (ESCR) in March 2024.
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Giuseppe Muscogiuri.
Conflict of interest
GM received a travel grant by Bracco. MCW has given talks for Canon Medical Systems, Siemens Healthineers and Novartis and performed consultancy for FEOPS. MCW is supported by the British Heart Foundation (FS/ICRF/20/26002). JRWM is supported by the National Institute for Health and Care Research (NIHR) Cambridge Biomedical Research Centre (BRC-1215-20014). RV is supported by an institutional research grant from Siemens Healthineers, and has received honorarium by Siemens Healthineers and Bayer for invited lectures. CL has received speaker honorarium from Siemens Healthineers, GE Healthcare and Bracco. HA has given presentations for Siemens. Healthcare. HA receives institutional grants from Bayer, Canon, Guerbet, and Siemens. HA is deputy editor of European Radiology. He has not taken part in the review or selection process of this article. JWM is a member of the European Radiology Scientific Editorial Board (Cardiac). He has not taken part in the review or selection process of this article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was not required.
Ethical approval
Institutional Review Board approval was not required.
Study subjects or cohorts overlap
Not applicable.
Methodology
-
Practice recommendations
Additional information
Publisher’s Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article belongs to the ESR Essentials series guest edited by Marc Dewey (Berlin/Germany).
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Muscogiuri, G., Weir-McCall, J.R., Tregubova, M. et al. ESR Essentials: imaging in stable chest pain – practice recommendations by ESCR. Eur Radiol 34, 6559–6567 (2024). https://doi.org/10.1007/s00330-024-10739-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-024-10739-y