Abstract
Background
Patient motion during pharmacological stressing can have substantial impact on myocardial blood flow (MBF) estimated from dynamic PET. This work evaluated a motion correction algorithm with and without adjustment of the PET attenuation map.
Methods
Frame-by-frame motion correction was performed by three users on 30 rubidium-82 studies. Data were divided equally into three groups of motion severity [mild (M1), moderate (M2) and severe (M3)]. MBF data were compared for non-motion corrected (NC), motion-corrected-only (MC) and with adjustment of the attenuation map (MCAC). Percentage differences of MBF were calculated in the coronary territories and 17-segment polar plots. Polar plots of spill-over were also generated from the data.
Results
Median differences of 23% were seen in the RCA and 18% for the LAD in the M3 category for MC vs NC images. Differences for MCAC vs MC images were considerably smaller and typically < 10%. Spill-over plots for MC and MCAC were notably more uniform compared with NC images.
Conclusion
Motion correction for dynamic rubidium data is desirable for future MBF software updates. Adjustment of the PET attenuation map results in only marginal differences and therefore is unlikely to be an essential requirement. Assessing the uniformity of spill-over plots is a useful visual aid for verifying motion correction techniques.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Quantitative MBF using rubidium-82 PET has been shown to have additive and incremental prognostic value over and above relative perfusion data for the assessment of coronary artery disease (CAD).1,2,3 As with any image-derived metric, several technical factors could potentially affect MBF values and hence robust quality control measures are necessary to ensure that the data is accurate and reproducible.4 Recent excellent clinical guidelines published jointly by ASNC and SNMMI on stepwise assessment of MBF data from dynamic PET for its routine use in clinical practice are available.5
Patient motion is a major factor that affects accurate MBF calculation. There are multiple commercial MBF software packages available from a range of vendors,6 with differing handling of patient motion. Three examples are Syngo.PET MBF from Siemens Healthineers, which provides automated motion tracking only7; Corridor4DM from Invia allows manual frame-by-frame correction, and has been used in several recent studies8,9,10 and QPET from Cedars Sinai, which, to the best of our knowledge does not allow any correction for patient motion. This variability of motion compensation techniques could inherently alter MBF values across different vendors and hence there is a need for standardisation.11 Motion and its effect on MBF has been reported in oxygen-15 water studies with motion being tracked either by external markers or optical surface tracking systems.12,13 There have been more recent studies that have investigated the impact of motion on MBF data in rubidium-82 perfusion PET.7,8,9,10,14,15 Simulation data from Hunter et al. demonstrated that frame-by-frame motion correction of dynamic PET data reduced the mean error of 240% to 10% when comparing to the ground truth simulations.14 Due to the increased use of myocardial perfusion PET imaging including MBF data in routine clinical practice across the world, there is a desire to standardize motion correction techniques to ensure consistent results across software from all vendors.
Types of Motion
Reasons for potential heart displacement throughout the scan can be generally classified under two categories: that due to a physical, translational shift of the patient and that due to physiological movement related to increased respiratory rate secondary to vasodilator stress or cardiac motion. Physiological motion can be either periodic (e.g. cardiac beating, respiratory) or non-periodic, i.e. from a general relaxation of the patient or associated with the changes in the gross tidal volume of the lung during pharmacological stress. In myocardial perfusion PET, we are imaging at the time of peak stress and we believe that motion is often attributed to the side effects of the stressing agent diminishing during the PET scan.
Prevalence of Motion
The published prevalence of patient motion during dynamic rubidium cardiac PET is variable but there is an overall greater degree of motion observed in stress images. For a 20-frame dynamic reconstruction, Naum et al. reported motion in 8.7 ± 3.2 frames during adenosine stress compared with 3.7 ± 2.1 frames at rest.12 In our institution, a retrospective analysis of 3097 patients showed significant motion in 30% of stress images but only in less than 5% on rest images.7 Koenders et al. showed non-returning motion in 52/104 stress images compared with 2/104 for rest scans.9 A study from the same institution by van Dijk et al. noted non-returning motion in 31/64 stress images.10 Lee et al. reported mild to severe motion shifts in 66% of stress images compared with 45% of rest images8 and observed that the median shift for stress images was 6.4 mm compared with 4.5 mm for rest images. The degree of variation between published results generally reflects the variation in stress protocol used.7,16
Effects of Motion
The calculation of MBF requires accurate measurement of blood input function and myocardial uptake, derived from semi-automated volumes of interest to generate time activity curves that are used as input data for the kinetic model.17 The presence of motion can move the reconstructed PET data outside of these delineated volumes of interest and hence render the uptake measurements inaccurate. Frame-by-frame adjustment of the volumes to account for this motion is available manually or automatically in some commercially available software; however, the corresponding shifts in the underlying attenuation maps are not accounted for. Hence in addition to the impact of motion correction on time activity curves, there is the additional factor of temporal variation of PET to CT registration and its impact on the frame-to-frame attenuation correction. A study by Rajaram et al. demonstrated that mis-registering PET data in the lateral and cranial directions relative to the CT, could produce mean changes of up to 39% in MBF.18 A simulation study by Pourmoghaddas et al. assessed the impact of superior-inferior motion due to breathing on MBF. They recommended that matched attenuation correction is important if motion correction is applied.19 In contrast, a recent retrospective study by van Dijk et al. concluded that frame-by-frame adjustment of the attenuation map is not necessary when correcting for motion.10 However, their study evaluated “cardiac creep” motion and not general patient motion. Their study included patients stressed exclusively with regadenoson, which has been shown to result in less frequent and less severe patient motion compared with adenosine.7,16 In addition, so far the impact of motion on MBF calculation using clinical data has been performed using only Corridor 4DM.8,9,10 We feel that the inconsistency between findings and the lack of data processed using software from other vendors motivates additional investigation into this particular area.
The common lack of ground truth and non-trivial means of assessing motion correction effectiveness motivates the need to establish indicators of such effectiveness. One possibility may be the use of spill-over data, as certain software packages offer visual representation of the regional spill-over of the early blood-pool activity into the left ventricle volume of interest.
In this study, we evaluate frame-by-frame motion correction, applied to both PET-only and PET and attenuation maps, of dynamic rubidium data on MBF results. In our institution, we use both adenosine and regadenoson for pharmacological stressing. Due to previous studies already demonstrating the impact of motion correction for patients stressed using regadenoson, we focus solely on adenosine. We believe that, by combining our findings with other studies, we will understand the impact of motion on our patient population. The agreement of MBF data generated after motion correction by multiple operators is assessed as well as the use of spill-over plots to illustrate the effectiveness of any motion correction techniques.
Method
Patient Study Cohort
This study was a retrospective evaluation performed on 30 patients who underwent clinically indicated rubidium cardiac PET study stressed with adenosine. Based on the observation that the majority of patient motion occurs in stress images,7,9 the decision was taken to only include the dynamic stress data. The 30 datasets were divided equally into three groups of motion severity [mild (M1), moderate (M2) and severe (M3)]. This semi-quantitative categorisation of patient motion has been used previously in work from our institution.7,20 Briefly, M1 are cases where myocardial frame-by-frame motion is less than half the width of the myocardial wall, M2 cases are greater than half the width of the myocardial wall and M3 cases exhibit severe motion leading to a gross failure of myocardial segmentation. Each of the 10 cases in each category were collected consecutively. The classification of motion for the 30 cases was manually defined by one of three experienced users (IA, MM, KS) with a final consensus amongst these three users on the classification. Patient presentation at scan time was: M1 category: 6/10 suspected CAD, 3/10 for non-cardiac surgery workup and 1/10 known CAD; M2 category: 7/10 suspected CAD and 3/10 known CAD; M3 category: 10/10 with suspected CAD.
Rubidium PET Imaging and Image Reconstruction
All patients abstained from caffeine intake for 12 hours before the test and were administered 1110 MBq (30 mCi) of rubidium chloride from a Cardiogen Sr-82 generator (Bracco Diagnostics) after a low-dose CT for attenuation correction (120 kVp, CAREDose quality reference 11 mAs). In all patients, pharmacological stressing was performed using adenosine at an infusion rate of 140 µg/kg/min for 4.5 minutes. A 7-minute listmode PET scan was performed on a Siemens Biograph mCT equipped with 21.6 cm TrueV field of view (Siemens Healthcare, Knoxville, TN). The rubidium infusion was started 2 minutes after the start of the adenosine infusion and the PET acquisition was started as the rubidium was infused.
Dynamic data were framed into 18 frames as 1 × 10 s, 8 × 5 s, 3 × 10 s, 2 × 20 s and 4 × 60 s. Data were reconstructed with 3D Ordered Subset Expectation Maximisation (OSEM), without incorporation of resolution modelling or time-of-flight data, using 2 iterations, 24 subsets and a 6.5 mm full-width-half-maximum Gaussian post-filter. Registration of PET to the attenuation correction CT was defined during the motion correction process and will be described in the following section.
Motion Correction
Frame-by-frame translational motion correction was performed manually by three experienced users (IA, MM, KS) on the 30 rubidium-82 stress images. The correction was performed on prototype software developed by Siemens Healthcare and was independent of any commercial MBF processing software. Each user corrected all 30 images.
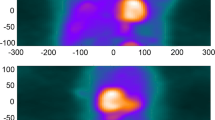
The first stage of the process was to register the PET images of the left ventricle with the CT used to generate the attenuation map for attenuation correction. A “reference” PET frame was selected for each case based upon optimal visualisation of the ventricle—this was towards the end of the dynamic framing and was a trade-off of blood-pool clearance and myocardial image noise in the myocardium due to decay of the rubidium. Due to differences in patient blood-pool clearance, myocardial uptake and noise characteristics, the optimum frame differed from patient to patient and typically frames 15, 16 or 17 (starting at 3, 4 or 5 minutes) were selected. Each user then manually performed PET to CT alignment, using only translational adjustment, on the selected reference frame for each case—the same reference frame was used by all three users on each case. The remaining PET frames were then manually aligned with this reference PET frame by each user; no automated techniques were employed Figure 1 illustrates this process. The window levels of the PET data were manually adjusted on each frame as required to provide optimum visualisation of either the myocardium or blood-pool activity during the late or early phases respectively.
Illustration of frame-by-frame motion correction applied. The chosen reference PET frame (in this case frame 16) is registered to the CT (A). The registered reference PET frame is then shown using a monochrome “edge” colour map and all other dynamic PET frames are registered to this reference PET frame. The example here shows PET frame 12 before (B) and after (C) registration to the reference PET frame. The top row shows a transaxial view and the bottom row shows a corresponding coronal view
Following this PET-CT registration and frame-by-frame alignment of PET data, three sets of reconstructed images were created for each of the three users:
-
1.
a non-motion corrected (NC), where the original frame-to-frame motion was present and PET to attenuation correction CT registration was based upon the single reference frame for each user;
-
2.
a motion corrected only (MC), incorporating the individual user’s frame-to-frame translations and PET to attenuation correction CT registration was based upon the single reference frame;
-
3.
a motion corrected with corresponding adjustment of the attenuation correction map (MCAC), incorporating the individual user’s frame-to-frame translations that were also applied to the CT and attenuation correction map.
The MC data were generated by simply applying the translations to the NC data for each user. Only the MCAC data required a specific reconstruction to be generated where the attenuation map was also shifted according to the frame-by-frame translations. This was performed with prototype offline reconstruction software (e7 tools, Siemens Healthineers).
MBF data were generated in syngo.PET MBF (Siemens Healthineers) for each of these three image sets and for each of the three users. The automated motion tracking that is available in the software was not used in the data analysis to allow the impact of only the users’ motion shifts to be observed. Placement of the blood input volume of interest is automated, within the basal left ventricular cavity, determined from the automated left ventricle segmentation so no user adjustment was performed. The relative differences of MBF were calculated in the three coronary territories and also in 17-segment polar plots. As the direction of the change in MBF was expected to be variable, relative changes in MBF are quoted as the absolute magnitude to give a clearer indication of the impact of motion.
17-segment polar plots of spill-over values calculated according to the single-compartment model fitting17 from Syngo.PET MBF, were generated for NC, MC and MCAC data using in-house developed processing (Python 3.4, Python Software Foundation, https://www.python.org). For syngo.PET MBF the left ventricle segmentation is derived from the late frames when the blood-pool has cleared. Any shift in position of the heart between early and late frames may result in incorrect positioning of the left ventricle volume of interest in the early frames when the ventricle is not yet visible. As the effect of spill-over has greatest influence during the early blood input phase, we propose an assessment of the homogeneity of the spill-over fraction across the 17 segment model. This would indicate firstly correct positioning of the left ventricle volume of interest in these early frames such that it surrounds the blood-pool activity in a uniform fashion with minimal spill-over and secondly whether this position remains consistent or if motion exists during the phase. For each image, the coefficient of variation (CoV) of spill-over across the 17 segments was calculated as a potential quantitative measurement of homogeneity.
Statistical Analysis
In order to assess the variability of the MBF data across the three users, a two-way analysis of variance was performed for MC and MCAC data across the three users across MBF data in the three coronary territories only—the global MBF values were not included as they can be seen as a weighted average of the LAD, LCx and RCA values. This was performed in Microsoft Excel. Following a Bonferroni correction for multiple tests, a significance level of P = 0.008 was used.
Results
Comparison of User Variation
Results from the two-way ANOVA of the three users’ assessment of motion demonstrated no significant inter-user variation (P > 0.05 for all cases). For this reason, the MBF data from the three users were collated in the subsequent plots to demonstrate the realistic range of changes to MBF due to the investigated correction methods, giving three data points per patient and therefore 30 data points per motion category from which medians and inter-quartile ranges were calculated given the data were not normally distributed.
The plots in Figure 2 show the cumulative motion shift in each of the orthogonal directions derived from the frame-by-frame motion shifts for each user. The figure shows that the magnitude of cumulative shifts are comparable in the x-direction (left–right) and y direction (anterior–posterior) while notably larger shifts are seen in the z direction (superior-inferior). To demonstrate the temporal relationship of the shifts, Figure 3 shows the plots of the absolute magnitude of the shift vector for each frame relative to the final frame. It shows that the greatest degree of frame-to-frame translation occurs across frames 14 to 16, which span the period of when the adenosine infusion was completed 2:30 after the start of the PET acquisition. There is a considerable variability in the magnitude of shifts in the early frames, particularly with M3 cases but overall the median value shows a relatively consistent systematic offset for these earlier frames during the scan.
Cumulative motion shifts in orthogonal directions for each of the motion categories. The plot on the left shows cumulative y shifts (anterior–posterior) plotted against x shifts (left–right) and the plot on the right shows cumulative z shifts (superior–inferior) plotted against x shifts. Note that data are shown for each user and so there are 30 points per motion category
Plot showing the temporal relationship of the absolute magnitude of the shift vector. Data shown are the median (black line) and inter-quartile range (grey area) of the absolute magnitude of the shift vectors for each time-point alongside the individual vectors. Note that data are shown for each user and so there are 30 points per motion category
Changes to MBF Values
Figures 4 and 5 show the scatter plots of MBF in the three coronary territories and globally for MC vs NC and MCAC vs MC, respectively. The scatter plots show that change in MBF is greatest in M3 cases but, particularly in the RCA territory, there is positive and negative change with negligible systematic offset. Hence to compliment these graphs, the remaining figures show only the magnitude of change to MBF and not the direction of change. The box-plots in Figures 6 and 7 show the median and inter-quartile range of the magnitude of relative change for MC vs NC and MCAC vs MC, respectively. These plots show more clearly that the degree of change in MBF increases with an increasing degree of motion.
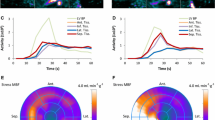
Figure 8 demonstrates the median magnitude of relative change of MBF values for MC vs NC and MCAC vs MC across 17 segment polar plots. The magnitude of the change can be seen to increase amongst progressive motion categories when compared with the NC data, specifically in the anterior and infero-septal regions. The difference when compared with the MCAC data is less pronounced, demonstrating that the effect of frame-by-frame adjustment of the attenuation map when motion is considered is non-zero but small compared with gross motion correction.
Polar plots showing the median magnitude of relative change of MBF measured comparing MC vs NC (left column) and MCAC vs MC (right column). Data are shown for the three motion categories, increasing from top to bottom. The greatest median change was found to be 65% in the apical anterior segment for the M3 category, although intensity is scaled to 50% for consistency with other figures
Figure 9 shows 17 segment polar plots of the median spill-over values for the three different image sets and motion categories. As can be seen, the spill-over values become considerably greater in the RCA territory as the severity of the motion increases for the NC images. This is due to the early blood-pool erroneously overlying the myocardial volume of interest. Even in the M1 category, there is increased spill-over in the infero-septal segments compared with the antero-septal segments. For both MC and MCAC images, there are negligible differences between the plots for all three motion categories. In all spill-over plots, there is increased spill-over in the septal wall, which is thought to be a consequence of activity in the right ventricle during the first pass of the tracer bolus contributing to the left ventricle myocardial volume of interest.
Figure 10 shows the distribution of the CoV data derived from each of the 17-segment spill-over plots for each image. The plot shows that MC and MCAC offer similar distributions for all motion categories and are lower than the CoV from the NC images.
Discussion
In this study, we have evaluated the application of frame-by-frame motion correction, both with and without combined correction of the attenuation map, when determining MBF from dynamic rubidium PET. By including motion correction applied by multiple users on the same data, we have demonstrated that the technique is reproducible. To demonstrate the generality of the correction, we considered any form of motion giving rise to displacement of the heart during the scan and did not constrain the motion selection to non-returning “cardiac creep” motion as done by other authors.9,10 We also believe that this is the first study to demonstrate the impact of general motion on MBF for patients stressed with adenosine and imaged with rubidium as other studies have exclusively used regadenoson.8,9,10
Frame-by-Frame PET Motion Correction
We have demonstrated that motion can have a substantial impact on the calculation of MBF due to incorrect time activity data extracted from myocardial and blood-pool volumes of interest. Looking at MBF in the coronary territories, the RCA territory was the most susceptible to motion with a median absolute percentage change of 23% comparing MC to NC data in the M3 motion category. This is comparable to data presented by Lee et al.8 who reported a mean change of 29% in patients demonstrating mild to moderate motion. The difference in results between the two studies may be attributed to the reconstruction parameters used as Lee et al. incorporated resolution modelling and time-of-flight as opposed to standard OSEM algorithm without resolution modelling or time-of-flight used in our study. Reconstruction parameters will have a significant impact on MBF calculation.20 We accept that the parameters used in our study, including the relatively large amount of post-reconstruction smoothing are likely to reduce the changes in MBF observed—particularly comparing against a study like that of Lee et al. where minimal post-filtering was applied. The parameters were defined when we commenced our rubidium service, and based on the manufacturer’s recommendation. They have remained fixed for consistency. As with the data from Lee et al. our results showed an artificially high MBF in the RCA territory without motion correction. This is due to spill-over of the early blood-pool activity into the myocardial volume of interest. This is supported by the spill-over polar plots for NC data in Figure 9. We also observed a substantial impact of motion on the LAD territory with a median absolute percentage change of 18% comparing MC to NC data in the M3 motion category. In fact, the apical and mid-anterior segments experienced the greatest overall median change of 65% with motion as shown by Figure 8. This is due to significant motion in the mid- to late-phase where the blood-pool activity has cleared, so the change in regional MBF is not due to spill-over, but instead a gross failure of the volume of interest tracking of the myocardium as shown in Figure 11. This compares to only 4% change reported by Lee et al. in the LAD territory. We believe that these differences arise due to the stressing agent. In our study, adenosine was the sole stressing agent, with an infusion that finished 2.5 minutes into the 7-minute listmode acquisition. The side effects of adenosine wear off very quickly and we saw substantial inferior–superior cardiac motion due to changes in respiratory motion patterns as shown in Fig. 3. We believe that this would cause greater errors in the later “tissue phase” compared with that observed by Lee et al.
Frame-by-Frame Attenuation Map Motion Correction
The study by van Dijk et al. reported that frame-by-frame motion correction of the attenuation correction map is not required for patients undergoing regadenoson stress.10 In our study, we have made a similar observation in patients undergoing adenosine stress; a group in whom the magnitude of patient motion has been shown to be greater.7,16 The study by van Dijk focused on motion classified as “cardiac creep”, which the authors demonstrated was associated predominantly by z-axis (superior-inferior) motion. We acknowledge Figure 2 of our study shows that motion is greater in the z-axis direction but we still observe appreciable motion in the x-axis and y-axis directions. By comparing Figure 2 with the motion plots in the study by van Dijk et al., we consider that we have observed greater degree of lateral motion in our study. This is supported by the data from Hunter et al., who looked at general motion, and demonstrated lateral motion in 31% of the images, which resulted in significant error in MBF measurement as a result of CT mis-registration.14 We note that Figure 7 demonstrates a greater variability of the change in MBF for the M2 data compared with M3 data in the RCA territory. Two patients in the M2 group demonstrated a relatively large change in RCA MBF with MCAC vs MC (approximately 20% and 30%) that skewed the variability in the M2 RCA plot in Figure 7. Both the CT and the nature of the PET motion were evaluated for these two patients. Both patients exhibited gradual upward motion in the PET but had quite stark anatomical features seen on CT. One patient had a very highly protruding liver into the chest cavity while the other had a very low-lying liver. Even though motion magnitude was not as great as M3 cases, we suspect that the anatomical features gave rise to larger changes in the RCA region as a result of adjusting the attenuation map. These anatomical features may be a result of the particular phase with the breathing cycle that the CT was acquired at.
Whilst the results from our study are not backed up by follow-up clinical data, our work shows that there is no additional value of attenuation map motion correction. This is supported by the simulation work by Hunter et al., which showed that frame-by-frame motion correction is the single biggest factor in reducing the error on MBF with adjustment of the attenuation map contributing small residual errors. While the implementation of the frame-by-frame motion correction was performed offline, it is entirely feasible that this could be integrated into the processing software for routine use. The use of a second CT after the stress images may be used to reduce mis-registration errors14 but our findings suggests that this is not necessary and the use of a single CT for attenuation correction would suffice.
In our study, we have assessed the absolute values of regional blood-pool to myocardium spill-over of activity as an indicator of the effectiveness of motion correction and generated polar plots with in-house techniques as this is not commonly available in commercial software. In the study by Lee et al., the use of spill-over was used as one of three criteria for judging the alignment of the early blood-pool phase with myocardial contours.8 However, it is not clear from their study whether the group quantitatively equalised spill-over values over the myocardium or this was assessed visually. Based on our observation, both visual inspection and quantification of the uniformity of these spill-over polar plots can be used to identify cases where motion in the early blood-pool phase has been sufficiently corrected. We observed that there is still slightly increased spill-over in the septal region and it is possible that the appearance of spill-over plots is dependent on the reconstruction method. We hypothesise that incorporating resolution modelling and time-of-flight will result in reduced septal spill-over due to better quality images and convergence.20
From the perspective of the kinetic modelling used for the calculation of MBF, it has been demonstrated that there is very little benefit from using short time frames in the myocardial uptake phase21 but this does not take into consideration any intra-frame motion. Our work uses a relatively coarse time sample, too coarse to sample intra-frame motion adequately and hence this will still exist. This is particularly relevant in the later times frames of the dynamic data where 60-second frames were used. It is noted that establishing the impact of motion correction techniques on the absolute accuracy of MBF data in clinical images is challenging as there is no ground truth of actual MBF. One recent study has attempted to assess the reliability of MBF data following motion correction using Bayesian probability model to uncertainty estimates of the extraction coefficient K1 from the compartmental model.22 The work showed that motion correction reduced the uncertainty, implying a more confident assessment of MBF. We believe the homogeneity of spill-over across the myocardium combined with other metrics such as a goodness of fit for the kinetic model could be implemented as a Quality Index in future software versions.
Limitations
A limitation of our study is that motion was only assessed in stress rubidium images. The rationale for this was supported by observations in the recent literature and from our department that stress images are far more susceptible to patient motion due to the effects of vasodilator stress agents. The exception to this is the work by Hunter et al. who observed no significant differences in motion for rest and stress images.14 We believe that the longer lasting side effects of dipyridamole as used in their study may have led to this observation.
We have used a relatively small patient cohort in this study but believe that by including multiple corrections for each case and a range of patient motion severity, we feel that there is sufficient data to support the findings.
Finally, the non-contemporaneous nature of the CT data used for each frame should be noted. The CT acquisition is prior to the PET and therefore the tissue map for attenuation correction does not account for the longer PET acquisition and variation in thoracic structures position during normal respiration and vasodilator induced changes. Therefore, the MCAC data cannot be considered as a gold-standard as opposed to approaches such as morphing the CT data according to PET derived motion-fields. However, considering the negligible incremental value of frame-by-frame adjustment of the attenuation map observed in our study, this added complexity is unlikely to be clinically relevant.
New Knowledge Gained
To the best of our knowledge, this is the first study that has demonstrated the effect of general patient motion, in various degrees of severity on rubidium myocardial blood flow for patients stressed with adenosine. Like previous studies, we have shown that frame-by-frame adjustment of the PET data is by far the more important correction to apply and adjusting the attenuation map results in minimal changes in MBF. We have proposed a novel method of evaluating the effectiveness of motion correction by assessing the uniformity of spill-over polar plots. These plots, together with quantitative assessments of uniformity, could potentially be used to optimise automated frame-by-frame motion correction should such technology become available in software.
Conclusion
This work adds to the growing number of studies that demonstrate that frame-by-frame motion correction strategies is a highly desirable feature in determination of MBF using dynamic rubidium PET. Frame-by-frame adjustment of the attenuation map results in marginal differences and therefore is unlikely to be an essential requirement. This is fortunate as it involves direct integration into the PET reconstruction and is not currently available commercially. Assessing the uniformity of spill-over plots appears to be a useful aid for verifying motion correction techniques.
Abbreviations
- MBF:
-
Myocardial blood flow
- MC:
-
Motion corrected
- MCAC:
-
Motion corrected and attenuation motion corrected
- NC:
-
Non-motion corrected
- PET:
-
Positron emission tomography
References
Ziadi MC, Williams MSK, Guo MEA, Renaud MSJM, Chow MDBJW, et al. Does quantification of myocardial flow reserve using rubidium-82 positron emission tomography facilitate detection of multivessel coronary artery disease? J Nucl Cardiol 2012;19:670-80.
Murthy VL, Naya M, Foster CR, et al. Improved cardiac risk assessment with non-invasive measures of coronary flow reserve. Circulation 2011;124:2215-24.
Ziadi MC, deKemp RA, Williams KA, Guo A, Chow BJW, Renaud JM, et al. Impaired myocardial flow reserve on rubidium-82 positron emission tomography imaging predicts adverse outcomes in patients assessed for myocardial ischemia. J Am Coll Cardiol 2011;58:740-8.
Moody JB, Lee BC, Corbett JR, Ficaro EP, Murthy VL. Precision and accuracy of clinical quantification of myocardial blood flow by dynamic PET: A technical perspective. J Nucl Cardiol 2015;22:935-51.
Muthy VL, Bateman TM, Beanlands RS, Berman DS, Borges-Neto S, Chareonthaitawee P, et al. Clinical quantification of myocardial blood flow using PET: Joint position paper of the SNMMI Cardiovascular Council and the ASNC. J Nucl Cardiol 2018;25:269-97.
Nesterov SV, Deshayes E, Sciagrà R, Settimo L, Declerck JM, Pan X-B, et al. Quantification of myocardial blood flow in absolute terms using 82Rb PET imaging. The RUBY-10 Study. JACC Cardiovasc Imaging 2014;7:1119-27.
Memmott MJ, Tonge CM, Saint KJ, Arumugam P. Impact of pharmacological stress agent on patient motion during rubidium-82 myocardial perfusion PET/CT. J Nucl Cardiol 2018;25:1286-95.
Lee BC, Moody JB, Poitrasson-Riviere A, Melvin AC, Weinberg RL, Corbett JR, et al. Blood pool and tissue phase patient motion effects on 82rubidium PET myocardial blood flow quantification. J Nucl Cardiol 2018. https://doi.org/10.1007/s12350-018-1256-1.
Koenders SS, Van Dijk JD, Jager PL, Ottervanger JP, Slump CH, van Dalen JA. Impact of regadenoson-induced myocardial creep on dynamic rubidium-82 PET myocardial blood flow quantification. J Nucl Cardiol 2019. https://doi.org/10.1007/s12350-019-01649-4.
van Dijk JD, Jager PL, Ottervanger JP, Slump CH, van Dalen JA. No need for frame-wise attenuation correction in dynamic rubidium-82 PET for myocardial blood flow quantification. J Nucl Cardiol 2019. https://doi.org/10.1007/s12350-019-01654-7.
Piccinelli M, Votaw JR, Garcia EV. Motion correction and its impact on absolute myocardial blood flow measures with PET. Curr Cardiol Rep 2018;20:34-41.
Naum A, Laaksonen MS, Tuunanen H, Oikonen V, et al. Motion detection and correction for dynamic 15O-water myocardial perfusion PET studies. Eur J Nucl Med Mol Imaging 2005;32:1378-83.
Koshino K, Watabe H, Enmi J, Hirano Y, et al. Effects of patient movement on measurements of myocardial blood flow and viability in resting 15O-water PET studies. J Nucl Cardiol 2012;19:524-33.
Hunter CRRN, Klein R, Beanlands RS, de Kemp RA. Patient motion effects on the quantification of regional myocardial blood flow with dynamic PET imaging. Med Phys 2016;43:1829-40.
Lee BC, Moody JB, Poitrasson-Riviére A, Melvin AC, Weinberg RL, Corbett JR, et al. Automated dynamic motion correction using normalized gradient fields for 82rubidium PET myocardial blood flow quantification. J Nucl Cardiol 2018. https://doi.org/10.1007/s12350-018-01471-4.
Vleeming EJ, Lazarenko SV, van der Zant FM, Pan XB, Declerck JM, Wondergem M, et al. Cardiac displacement during 13 N-Ammonia myocardial perfusion PET/CT: Comparison between adenosine and regadenoson induced stress. J Nucl Med Technol 2018;46:114-22.
Lortie M, Beanlands RSB, Yoshinaga K, Klein R, Dasilva JN, DeKemp RA. Quantification of myocardial blood flow with 82Rb dynamic PET imaging. Eur J Nucl Med Mol Imaging 2007;34:1765-74.
Rajaram M, Tahari TK, Lee AH, Lodge MA, Tsui B, Nekolla S, et al. Cardiac PET/CT misregistration causes significant changes in estimated myocardial blood flow. J Nucl Med 2013;54:50-4.
Pourmoghaddas A, Klein R, de Kemp RA, Wells G. Respiratory phase alignment improves blood-flow quantification in Rb82 PET myocardial perfusion imaging. Med Phys 2013;40:022503.
Armstrong IS, Tonge CM, Arumugam P. Impact of point spread function modeling and time-of-flight on myocardial blood flow and myocardial flow reserve measurements for rubidium-82 cardiac PET. J Nucl Cardiol 2014;21:467-74.
Lee BC, Moody JB, Weinberg RL, Corbett JR, Ficaro EP, Murthy VL. Optimization of temporal sampling for 82rubidium PET myocardial blood flow quantification. J Nucl Cardiol 2017;24:1517-29.
Saillant A, Armstrong IS, Shah V, Zuehlsdorff S, Hayden C, Declerck J, et al. Assessing reliability of myocardial blood flow after motion correction with dynamic PET using a Bayesian framework. IEEE Trans Med Imaging 2019;38:1216-26.
Disclosures
This project was performed in collaboration with Siemens Medical Solutions USA, Inc., for which financial support was provided to the nuclear medicine department. Antoine Saillant was an employee of Siemens Medical Solutions during this work. Charles Hayden is a current employee of Siemens Medical Solutions.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
All editorial decisions for this article, including selection of reviewers and the final decision, were made by guest editor Stephan G. Nekolla, PhD.
The authors of this article have provided a PowerPoint file, available for download at SpringerLink, which summarises the contents of the paper and is free for re-use at meetings and presentations. Search for the article DOI on SpringerLink.com.
The authors have also provided an audio summary of the article, which is available to download as ESM, or to listen to via the JNC/ASNC Podcast.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Armstrong, I.S., Memmott, M.J., Saint, K.J. et al. Assessment of motion correction in dynamic rubidium-82 cardiac PET with and without frame-by-frame adjustment of attenuation maps for calculation of myocardial blood flow. J. Nucl. Cardiol. 28, 1334–1346 (2021). https://doi.org/10.1007/s12350-019-01834-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-019-01834-5