Abstract
Background
Patient motion has been demonstrated to have a significant impact on the quality and accuracy of rubidium-82 myocardial perfusion PET/CT. This study aimed to investigate the effect on patient motion of two pharmacological stressing agents, adenosine and regadenoson.
Methods and Results
Dynamic data were retrospectively analyzed in 90 patients undergoing adenosine (n = 30), incremental adenosine (n = 30), or regadenoson (n = 30) rubidium-82 myocardial perfusion PET/CT. Severity of motion was scored qualitatively using a four-point (0-3) scale and quantitatively using frame-to-frame pixel shifts. The type of motion, returning or non-returning, and the frame in which it occurred were also recorded. There were significant differences in both the qualitative and quantitative scores comparing regadenoson to adenosine (P = .025 and P < .001) and incremental adenosine (P = .014, P = .015), respectively. The difference in scores between adenosine and incremental adenosine was not significant. Where motion was present, significantly more adenosine patients were classed as non-returning (P = .018). The median frames for motion occurring were 12 for regadenoson and 14 for both adenosine cohorts.
Conclusions
The choice of stressing protocol impacts significantly on patient motion. Patients stressed with regadenoson have significantly lower motion scores than those stressed with adenosine, using local protocols. This motion is more likely to be associated with a drift of the heart away from a baseline position, coinciding with the termination of infusion.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
There is growing evidence on the incremental prognostic value of quantitative myocardial blood flow (MBF) measurement with positron emission tomography (PET) in patients with suspected coronary artery disease (CAD).1,2 The estimation of MBF can be assessed using PET tracers such as 82Rb, implementing compartmental models to derive MBF.3,4 These models rely on accurate measurements of the time-activity curves (TAC) for the blood input function (BIF) and left ventricular myocardium (LVM) uptake. List mode acquisition of data throughout the duration of the 82Rb infusion also allows for creation of static and gated images, as in traditional myocardial perfusion imaging.
Whilst there are several technical factors that could impact on the accuracy of quantification,5,6 the most troublesome is patient motion.7,8,9 Patient motion has been shown to significantly affect the accuracy of quantification, mainly due to the misregistration between the PET and CT data leading to inappropriate attenuation correction.10,11 The magnitude of these effects on MBF can be quite profound, with errors reportedly as high as 500%, under certain conditions.7 The quality of the static reconstructed images can also be heavily impacted by patient motion. The static phase of the reconstruction generally includes 4 minutes of acquired data, therefore the possibility for motion to create spatial blurring and reduce maximal uptake values in the reconstructed data is high.12 The extent of patient motion can be visualized using the dynamic acquisition, and can be classed as intraframe or interframe; the former causing a spatial blurring of the reconstructed data, particularly in the later frames which are of longer duration, and the latter manifesting as motion between successive frames.13
Quantification can be affected as a result of interframe motion due to inaccurate sampling of activity concentrations in the volumes of interest used for dynamic modeling.14 Methods used for correction of frame-to-frame movement have been shown to have good results.7,12 However, these methods are not currently validated for clinical use. Intraframe motion can be mitigated using similar methods with shorter dynamic frames, at the expense of increased image noise; however, both cases will not overcome inappropriate attenuation correction. Reconstruction algorithms incorporating frame-by-frame attenuation correction are not currently available for clinical use.
The inability to fully compensate for the effects of patient motion is particularly pertinent for the calculation of myocardial flow reserve (MFR), as differences in patient motion between stress and rest examinations would give rise to inaccurate MFR estimates. There is a large variability in the literature regarding the prevalence of motion during stress and rest acquisitions. Hunter et al7 reported significant motion in 62% of their patient cohort, although no significant difference was found between rest and dipyridamole stress. Using adenosine, Woo et al12 also found no difference in the prevalence of patient motion between stress and rest studies. With 15O-labeled water, however, Naum et al15 showed significant differences in the incidence of patient motion between rest, adenosine, and exercise stress (18%, 45%, and 80%, respectively). Within our institution, we have observed a greater frequency of patient motion in stress acquisitions than rest,16 using a shorter 4.5-minute adenosine infusion adenosine protocol, compared to 6 minutes used by Woo et al. Therefore, the method of stress and the protocol used appear to have a significant impact of the incidence of patient motion.
Vasodilator agents (adenosine and regadenoson) are the most frequently used for pharmacological stress PET myocardial perfusion imaging. Due to the stimulation of A1, A2B, and A3 receptors, however, the use of adenosine can result in short-term undesirable side-effects, such as dyspnoea, chest pain, and hypotension, along with more severe side-effects such as atrioventricular (AV) block and bronchospasm.17,18 More selective agonists, such as regadenoson, have more recently become available for MPS stress imaging.19 Regadenoson is a fast acting, potent, and selective A2A receptor agonist which has been reported to be very well tolerated by patients, including those with mild-to-moderate airways disease.19,20
Along with differences in the incidence and spectrum of side-effects with adenosine and regadenoson,21 there are also differences in the duration of their action and return of hemodynamic responses to baseline.22 It has been shown in canine and human studies that the return of the hyperemic response to baseline is longer in duration for regadenoson.23,24,25 As the motion appears to be a greater problem during stress acquisition, our hypothesis is that these differences between the pharmaceutical stress agents may have an impact on the degree and frequency of patient motion, and to the best of our knowledge this relationship is yet to be investigated.
This study therefore aims to retrospectively compare the incidence and magnitude of motion during dynamic acquisition in patients referred for 82Rb PET and undergoing either regadenoson or adenosine stress.
Methods
Patient Selection
This study comprises a retrospective review of 30 consecutive patients attending for a clinically indicated 82Rb dynamic PET/CT study who underwent stress using regadenoson. Two comparison groups of 30 patients during the same period who underwent stress via adenosine or incremental adenosine were also randomly selected. In our institution, due to the cost difference between the agents, regadenoson is used only on patients weighing more than 140 kg and/or those with controlled asthma or chronic obstructive pulmonary disease (COPD). Therefore to reduce potential bias arising from patients’ weights, patients in each group were matched with randomly chosen patients of the same weight. Patients with well controlled asthma or COPD are also stressed using an incremental adenosine protocol, and hence this group was included to reduce the bias of existing respiratory conditions on the assessment of motion. The demographics of the three groups are shown in Table 1. The study underwent review by the institutional Research and Innovation department.
Image Acquisition
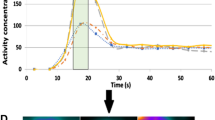
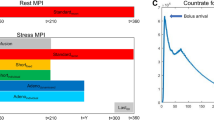
All patients were administered with 1110 MBq (30 mCi) of 82Rb from a Cardiogen® 82Sr generator (Bracco Diagnostics). Adenosine patients underwent pharmacological stressing via a 4.5-minute infusion at a rate of 140 µg/kg/min. Incremental adenosine patients followed our standard incremental protocol of a 1-minute infusion at 50 µg/kg/min, followed by 1 minute at 100 µg/kg/min and 4 minutes at 140 µg/kg/min. Regadenoson patients underwent an injection of 400 µg of Rapiscan (Rapiscan Ltd) over 20 seconds. Data acquisition began 2.5 minutes before the end of the adenosine infusion, 2 minutes before the end of the incremental infusion, or 40 seconds after the end of the Rapiscan injection, see Figure 1. Data were acquired on a Siemens Biograph mCT (Siemens Healthcare, Knoxville, US) with TrueV extended field of view. List mode data acquisition was started at the same time as the 82Rb infusion and lasted 7 minutes. For the dynamic reconstructions, all data were reframed into 18 frames of varying lengths: 1 × 10 seconds, 8 × 5 seconds, 3 × 10 seconds, 2 × 20 seconds, and 4 × 60 seconds. Prior to the rest acquisition, a low-dose (0.4 mSv) CT acquisition was performed for purposes of attenuation correction. A static reconstruction based on the fourth minute of the acquisition was used to check and correct for any misregistration between the PET and CT data, and the correction applied to all frames. Data were reconstructed using 3D Ordered Subset Expectation Maximization (OSEM), with 2 iterations, 12 subsets, and a 6.5-mm full-width half-maximum 3D Gaussian post-filter.
Qualitative Motion Assessment
Patient studies were anonymized and the dataset presented to two observers with no prior clinical information in a randomized order. The dynamic datasets were reviewed using the SyngoMBF software (Siemens Healthcare Ltd, Knoxville, USA), which allows the user to visualize successive dynamic frames with the heart presented in the standard cardiac orientation. Patient motion was assessed qualitatively on a scale from 0 to 3, using our department’s routine quality control procedure. Observers had an initial standardization session to ensure this interpretation and scoring was consistent. Motion was scored as follows: 0—no motion present; 1—minor motion present, but less than half the width of the left ventricular (LV) myocardial wall; 2—motion present greater than half the width of the LV myocardial wall, but the LV contours generated by the program were preserved; and 3—as for 2 but the contouring of the myocardium failed, as seen on either the dynamic frames or as artifacts on the polar plots, see Figures 2 and 3. The software automatically applies rigid translation to the volumes of interest to compensate for interframe motion, but with the long-axis location held constant across all frames. There is also a ‘high-motion correction’ option whereby the regions are rotated and translated in all axes, to allow more accurate tracking of the heart. To assess the success of contouring in those with a score of 2, this correction was applied and if the contouring still failed then the study was scored a 3.
Horizontal long-axis slices from frames 13 to 18 of two dynamic 82Rb stress studies. Top Patient demonstrating no motion, given a score of 0. Bottom A different patient demonstrating a non-returning motion is seen from frame 14 onwards, with a magnitude of greater than half a LVM width. This study was scored as a 3 as the contours were not preserved throughout the dynamic frames, causing artifactual MBF values in the LAD territory
Change in the MBF polar plot before A and after B ‘high-motion correction’ was selected for the same patient as for the bottom image in Figure 2. The anterior defect in A indicates a failure of contouring due to motion. This study was scored as a 3 due to the effect on the flow calculation
For scores >0, the type of motion was described as ‘returning’ or ‘non-returning.’ Returning motion was defined as motion which varied around an average position, whereas non-returning motion was defined as a sustained departure from a baseline position i.e., a drift. The frame in which the motion occurred was also recorded. Significant motion was defined as a score of 2 or 3.
The above scoring system has been in use at our institution for several years. To establish the frequency and severity of patient motion in our demographic, a retrospective review of 3097 motion scores for patients attending prior to the introduction of regadenoson was also performed.
Quantitative Motion Assessment
Along with the qualitative assessment, motion present in the dynamic acquisition was also assessed quantitatively. A template-matching algorithm was developed using Matlab (The MathWorks Inc., Natick, MA, 2000) to calculate the pixel shift in three-dimensions between successive frames, with the heart orientated in the standard cardiac axes. Due to the rapidly changing activity distribution in the early short duration frames, only those with a high correlation-coefficient (>0.80) were used to ensure the resultant motion vector reflected only anatomical displacement. For each study, the degree of motion was characterized using the sum of the displacement vector for the final 6 minutes of the acquisition (frames 11-18). These scores were also compared to our quantitative assessment used in routine clinical practice. The voxel dimensions in our PET reconstruction were anisotropic; hence due to this, and the rotations applied, absolute quantification of distance was not possible. The above measure therefore served only as a comparative measure.
Analysis
When the motion scores between the observers agreed, this score was accepted. Where there was disagreement, a third trained observer reviewed the data and a consensus was reached between the three observers. The resulting scores for each observer were analyzed using Fisher’s exact probability tests, where <80% of individual values had expected value <5, or Chi-Squared analysis, with a value of significance taken to be .05. All continuous values were tested for significance using the Mann-Whitney U Test for non-parametric data. Statistics were calculated using StatsDirect (StatsDirect Ltd, UK).
Results
Qualitative Motion Score
The results of a retrospective review of 3097 patient motion scores prior to the introduction of regadenoson are shown in Table 2. A significant difference (P < .001) is seen between the rest and stress acquisitions, with the stress acquisition having a larger degree of motion. Adenosine was used to stress all patients.
A histogram of consensus motion scores for the patient cohort in this study is shown in Figure 4. Results from the Fisher probability test demonstrate a significant difference between the distributions for regadenoson and adenosine (P = .025), and regadenoson and incremental adenosine (P = .014). There was no significant difference between the scores for adenosine and incremental adenosine (P = .75). For adenosine, 18/30 patients scored 0 or 1 and 12/30 scored 2 or 3; for incremental adenosine, 10/30 scored 2 or 3. The number of patients with significant motion, scores 2 or 3, for regadenoson was 3/30, significantly lower than for both adenosine and incremental adenosine (P < .01), calculated using the Chi-Squared test. Therefore, patients in this cohort who were stressed with regadenoson had significantly less severe motion than with either adenosine or incremental adenosine.
Table 3 shows the relationship between the motion score for the rest and stress acquisitions. In total, 81% of rest acquisitions had a motion score of 0, showing similar results to our retrospective analysis. In all patients with a rest score of greater than zero, 76% also had non-zero stress scores. However, this rate was similar in those with rest scores of zero, 73%, with an odds ratio of 1.23 [CI 0.65-2.30], indicating that motion in the rest acquisition was not predictive of stress motion.
Quantitative Motion Score
The correlation between the stress qualitative and quantitative motion assessment is shown in Figure 5. Successive qualitative scores had greater pixel displacement in the final 6 minutes of the acquisition, providing validation for our routine clinical method. There was also a significant difference between the quantitative scores for the three cohorts, Figure 6, with regadenoson patients demonstrating significantly less motion than both adenosine (P < .001) and incremental adenosine (P = .015). There was no significant difference in the degree of motion between those patients stressed with adenosine and incremental adenosine (P = .42).
Motion Type
Patients stressed with either adenosine protocol were significantly more likely to have non-returning motion than with regadenoson (P = .018). In the 16 patients stressed with regadenoson who had motion scores >0, 69% (11/16) were classed as non-returning, whereas 96% (23/24) stressed with adenosine and 96% (25/26) of those stressed with incremental adenosine were classed as non-returning.
Motion Frame
The median frame [min-max] for motion occurring was 12 [6-15], 14 [10-15], and 14 [12-15]. for regadenoson, adenosine, and incremental adenosine, respectively, although the variation in frame numbers was greater for regadenoson.
Discussion
We believe that this is the first study to directly compare the effect of pharmacological stress agent on patient motion during dynamic myocardial perfusion PET/CT. Patients in this cohort who were stressed with regadenoson demonstrated significantly less motion, based on both quantitative and qualitative analyses. The median frame for onset of cardiac motion, particularly in patients stressed with adenosine, was frame 14. This corresponds to 120-140 seconds into the acquisition and is approximately the frame in which the infusion of adenosine is terminated. This, and the fact that we see significantly more motion in stress studies, indicates that the choice of stressing protocol has a large impact on patient motion. An explanation for this is the duration of the effect of the stressing agent, along with its physiological side-effects.
Gao et al26 investigated the relationship between the affinity and reversal time of coronary vasodilation after termination of regadenoson administration in isolated perfused rat and anesthetized pig hearts. Time to reversal was defined as the time taken for the coronary conductance to return to 90% of maximum. They demonstrated a linear relationship between binding affinity and time to reversal. The time to 90% and 50% reversal for regadenoson in rats was found to be 11.3 and 5.2 minutes; in comparison adenosine had significantly shorter reversal times of 5.6 and 1.6 minutes, respectively. Trochu et al23 found similar differences between adenosine and regadenoson in the conscious canine. The authors found that using a dose of 2.5 µg/kg, coronary blood flow remained greater than twice baseline values for 97 seconds for regadenoson, compared to 24 seconds following a 267 µg/kg administration of adenosine.
In humans, Lieu et al24 investigated the effect of regadenoson on coronary flow velocity by use of a doppler-tipped guide wire. In total, 38 patients underwent administrations of 10-500 µg of regadenoson. At 400 µg, an increase of coronary blood flow greater than 2.5 times baseline was sustained for 2.3 minutes, and an increase of twice baseline was sustained for 8.5 minutes. Wilson et al25 studied the effect of adenosine on human coronary arterial circulation. They found that when infusing with a dose of 140 µg/kg/min, the average time from the offset of infusion until coronary blood flow returned to baseline levels was 145 seconds.
These studies indicate that the duration of action of regadenoson is of the order of minutes as opposed to seconds for adenosine. With adenosine, the duration of infusion and time to return to baseline appear to correlate well with the frames where motion occurs. Significantly, more patients stressed with adenosine had non-returning motion when compared with those stressed with regadenoson. Adenosine is known to stimulate respiration,27 with bolus administrations leading to significant increases in both respiration depth and rate, within 20 seconds of administration. These effects have a similar duration post-administration. We propose therefore that a relaxation of these changes in tidal volume post-stress with adenosine leads to the positional changes of the myocardium seen in the dynamic study. As regadenoson is associated with a longer duration of action and reduced respiratory side-effects, the distribution of the type of motion seen with regadenoson is mixed and its incidence reduced. This is supported by a recent article by Lassen et al28 who investigated the impact of stressing agent on respiratory gating. They found that adenosine led to a change in the respiratory rate between the initial and final minutes of the 82Rb acquisition, with the infusion terminating 4.5 minutes after the start of data collection and concluded that dobutamine over adenosine should be used to provide better quality reconstructed static images when employing respiratory gating.
In a study by Woo et al,12 the incidence and magnitude of motion in patients undergoing adenosine stress was lower than in our study, with no difference seen between stress and rest. A possible explanation for this is the stress protocol used. In their study, the 82Rb infusion began 90 seconds after the start of a 7-minute adenosine infusion. Four 1-minute static images were reconstructed during the last 4 minutes of the infusion, and the degree of motion assessed using a novel algorithm. As the adenosine infusion was terminated at the end of the image acquisition, we would not expect to see the effects demonstrated in this paper. It is therefore possible that changing the duration and timing of the adenosine infusion would also reduce the prevalence of patient motion during dynamic imaging.
Across our three cohorts, the main difference in demographics was the existence of existing respiratory disease and, although not significant, the age of the patients. As adenosine is known to have an effect on the respiratory system, we included the incremental group as a control for the regadenoson comparison. We saw no difference in the frequency or magnitude of motion between the two adenosine groups and hence are therefore confident that the results seen are due to the stressing agent and not underlying respiratory pathology. It could be argued that the age of the patient would also have an effect on the occurrence and degree of motion, with older patients potentially being lees compliant throughout the data acquisition. We did see a non-significant difference in the age of our three cohorts, with the adenosine patients tending to be older. To investigate this further, the qualitative and quantitative scores were evaluated against age. No significant trends were seen in either measure, indicating that age was not a compounding factor in this study.
The effect and significance of patient motion on MBF calculation is an area of on-going research. Rajaram et al11 investigated the effect of misregistration between PET and CT data on estimated MBF. Their results show that significant changes in absolute flow can occur with 5 mm of misregistration. Whilst the misregistration in this case was applied to the whole dataset, and not individual frames as with patient motion, their results do show the importance of correct frame-to-frame attenuation correction. This is specifically important when looking at the perfusion reserve as motion, and hence misregistration, can be more prevalent in the stress acquisition.
Prosetto et al8 evaluated the effect on quantification of cardiac and respiratory motion with various reconstruction algorithms for a custom-built dynamic phantom. The authors found that the presence of physiological motion overestimated the activity in the myocardium during situations mimicking the early blood pool phases of a dynamic acquisition, by around 25-45%. Conversely, when myocardial uptake was more prominent than the cavity, as in the later phases of a dynamic acquisition, an underestimation of activity was seen of 10-25%. Naum et al15 investigated patient motion in 15O-labeled water investigations of MBF under conditions of rest, adenosine exercise, and bicycle exercise, using external radioactive markers. They found a greater number of frames in the adenosine and exercise stress studies required correction than during the rest acquisition; the average magnitude of global motion in all datasets was approximately 6 mm. After correction for measured motion, the authors saw an increase of approximately 40% in estimated MBF values for both adenosine and bicycle stress, although only the value for bicycle stress was significant (P < .02).
A more recent paper by Hunter et al7 used the non-uniform rational B-splice (NURBS)-based cardiac torso (NCAT) computational phantom to generate dynamic data containing a variety of motion types. The percentage error when compared to motion free data was calculated. From clinical data they found the most common types of motion were translational shifts in superior and inferior directions, corresponding simulations showed a 20-mm shift at 60 seconds into the acquisition resulted in median MBF errors of around 10%, when the CT images were aligned to the later frames of the acquisition. The most significant errors were produced when the heart was translated in the right to left direction, with maximal segmental errors of up to 500%, although this was less frequently observed in the clinical demographic.
Assessment of quantitative accuracy requires a gold standard result, which is non-trivial with clinical data, as demonstrated by the use of computational phantom data in the above paper. Correction or simulation of motion would require manipulation of the raw PET and CT data prior to the reconstruction of each dynamic frame, this functionality is not currently available within our institution and hence it is not possible to assess the impact of the motion seen in this study on quantitative results.
From the above work it is clear, however, that patient motion can result in significant changes in the MBF calculation. Reduction of the incidence of patient motion therefore is the key in performing accurate and high-quality cardiac PET and the choice of either stressing agent or indeed stressing paradigm should be considered an important factor.
New Knowledge Gained
The choice of pharmacological stressing agent or protocol significantly affects the prevalence of patient motion during 82Rb myocardial perfusion PET/CT. Using the protocols used in this study, regadenoson results in a significantly lower incidence of patient motion compared with adenosine.
Limitations
This study was a retrospective review of previously acquired clinical data, and hence it was not possible to randomly allocate patients to different stressing protocols. Although all attempts were made to control bias due to demographics, it is still possible that some bias may still remain. These findings therefore serve to highlight the importance of choosing an appropriate stressing protocol when performing dynamic myocardial perfusion PET and a prospective, randomized controlled trial would be required to fully assess the impact of individual stress paradigms.
Conclusions
Patients stressed with regadenoson have a significantly lower degree of motion compared to those stressed with adenosine, using the protocols outlined in this study. This motion is more likely to be associated with a drift of the heart away from a baseline position, occurring at times coincidental with the termination of the stress infusion. The design of a stressing protocol therefore, and its impact on both image quality and accuracy of quantitation, requires careful consideration when performing 82Rb myocardial perfusion PET.
Abbreviations
- AV:
-
Atrioventricular
- BIF:
-
Blood input function
- CAD:
-
Coronary artery disease
- COPD:
-
Chronic obstructive pulmonary disease
- CT:
-
Computed tomography
- LAD:
-
Left anterior descending
- LVM:
-
Left ventricular myocardium
- MBF:
-
Myocardial blood flow
- OSEM:
-
Ordered-subset expectation-maximization
- PET:
-
Positron emission tomography
- TAC:
-
Time-activity curve
References
Ziadi MC, DeKemp RA, Williams K, Guo A, et al. Does quantification of myocardial flow reserve using rubidium-82 positron emission tomography facilitate detection of multivessel coronary artery disease? J Nucl Cardiol 2012;19:670–80.
Murthy VL, Naya M, Foster CR, et al. Improved cardiac risk assessment with non-invasive measures of coronary flow reserve. Circulation 2011;124:2215–24.
Prior JO, Allenbach G, Valenta I, Kosinski M, et al. Quantification of myocardial blood flow with 82Rb positron emission tomography: Clinical validation with 15O-water. Eur J Nucl Med Mol Imaging 2012;39:1037–47.
Lortie M, Beanlands R, Yoshinaga K, Klein R, DaSilva J, deKemp R. Quantification of myocardial blood flow with 82Rb dynamic PET imaging. Eur J Nucl Med Mol Imaging 2007;34:1765–74.
Kaufmann PA, Camici PG. Myocardial blood flow measurement by PET: Technical aspects and clinical applications. J Nucl Med 2005;46:75–88.
Tout D, Tonge CM, Muthu S, Arumugam P. Assessment of a protocol for routine simultaneous myocardial blood flow measurement and standard myocardial perfusion imaging with rubidium-82 on a high count rate positron emission tomography system. Nucl Med Commun 2012;33:1202–11.
Hunter CRRN, Klein R, Beanlands RS, de Kemp RA. Patient motion effects on the quantification of regional myocardial blood flow with dynamic PET imaging. Med Phys 2016;43:1829–40.
Presotto L, Gianolli L, Gilardi MC, Bettinardia V. Evaluation of image reconstruction algorithms encompassing Time-Of-Flight and Point Spread Function modelling for quantitative cardiac PET: Phantom studies. J Nucl Cardiol 2015;22:351–63.
Koshino K, Watabe H, Enmi J, Hirano Y, et al. Effects of patient movement on measurements of myocardial blood flow and viability in resting 15O-water PET studies. J Nucl Cardiol 2012;19:524–33.
McCord ME, Bacharach SL, Bonow RO, Dilsizian V, et al. Misalignment between PET transmission and emission scans: Its effect on myocardial imaging. J Nucl Med 1992;33:1209–14.
Rajaram M, Tahari AK, Lee AH, et al. Cardiac PET/CT misregistration causes significant changes in estimated myocardial blood flow. J Nucl Med 2013;54:50–4.
Woo J, Tamarappoo B, Dey D, Nakazato R, et al. Automatic 3D registration of dynamic stress and rest 82Rb and flurpiridaz F 18 myocardial perfusion PET data for patient motion detection and correction. Med Phys 2011;38:6313–26.
Mohy-ud-Din H, Karakatsanis NA, Goddard JS, Baba J, et al. Generalized dynamic PET inter-frame and intra-frame motion correction—Phantom and human validation studies. In: IEEE nuclear science symposium and medical imaging conference (NSSMIC) 2012. p. 3067–78.
Klein R, Renaud JM, Ziadi MC, Thorn SL, et al. Intra- and inter-operator repeatability of myocardial blood flow and myocardial flow reserve measurements using rubidium-82 PET and a highly automated analysis program. J Nucl Cardiol 2010;17:600–16.
Naum A, Laaksonen MS, Tuunanen H, Oikonen V, et al. Motion detection and correction for dynamic 15O-water myocardial perfusion PET studies. Eur J Nucl Med Mol Imaging 2005;32:1378–83.
Armstrong IS, Tonge CM, Arumugam P. Impact of point spread function modeling and time-of-flight on myocardial blood flow and myocardial flow reserve measurements for rubidium-82 cardiac PET. J Nucl Cardiol 2014;21:467–74.
Cerqueira MD, Verani MS, Schwaiger M, Heo J, et al. Safety profile of adenosine stress perfusion imaging: Results from the adenoscan multicentre trial registry. J Am Coll Cardiol 1994;23:384–9.
Cerqueira MD. The future of pharmacological stress: Selective A2A adenosine receptor antagonists. Am J Cardiol 2004;94:33D–40D.
Iskandrian AE, Bateman TM, Belardinelli L, et al. Adenosine versus regadenoson comparative evaluation in myocardial perfusion imaging: Results of the ADVANCE phase 3 multicenter international trials. J Nucl Cardiol 2007;14:645–58.
Iqbal FM, Hage FG, Ahmed A, Dean PJ, et al. Comparison of the prognostic value of normal regadenoson with normal adenosine myocardial perfusion imaging with propensity score matching. JACC Cardiovasc Imaging 2012;5:1014–21.
Zahid M, Kapila A, Eagan CE, Yusko DA, et al. Prevalence and significance of electrocardiographic changes and side effect profile of regadenoson compared with adenosine during myocardial perfusion imaging. J Cardiovasc Dis Res 2003;4:7–10.
Zhao G, Linke A, Xu X, Ochoa M, et al. Comparative profile of vasodilation by CVT-3146, an novel A2A receptor agonist, and adenosine in conscious dogs. J Pharmacol Exp Ther 2003;307:182–9.
Trouchu JN, Zhao G, Heiner P, Xu X, et al. Selective A2A adenosine receptor agonist as a coronary vasodilator in conscious dogs: Potential for use in myocardial perfusion imaging. J Cardiovasc Pharmacol 2003;41:132–9.
Lieu HD, Shryock JC, von Mering GO, Gordi T, et al. Regadenoson, a selective A2A adenosine receptor antagonist, causes dose-dependent increases in coronary blood flow velocity in humans. J Nucl Cardiol 2007;14:514–20.
Wilson RF, Wyche K, Christensen BV, Zimmer S, et al. Effects of adenosine on human coronary arterial circulation. Circulation 1990;82:1595–606.
Gao Z, Li Z, Baker SP, Lasley RD, et al. Novel short-acting A2A adenosine receptor agonists for coronary vasodilation: Inverse relationship between affinity and duration of action of A2A agonists. J Pharmacol Exp Ther 2001;298:209–18.
Watt AH, Routledge PA. Adenosine stimulates respiration in man. Br J Clin Pharmacol 1985;20:503–6.
Lassen ML, Rasmussen T, Christensen TE, Kjaer A, Hasbak P. Respiratory gating in cardiac PET: Effects of adenosine and dipyridamole. J Nucl Cardiol 2016. doi:10.1007/s12350-016-0631-z.
Acknowledgements
The authors would also like to acknowledge the work by Andy Bradley, Ian Armstrong, and Heather Williams in assisting with the collection of historical data for assessing the incidence of patient motion.
Disclosure
There are no conflicts of interest for Matthew J. Memmott, Christine M. Tonge, Kimberley J. Saint, or Parthiban Arumugam.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Memmott, M.J., Tonge, C.M., Saint, K.J. et al. Impact of pharmacological stress agent on patient motion during rubidium-82 myocardial perfusion PET/CT. J. Nucl. Cardiol. 25, 1286–1295 (2018). https://doi.org/10.1007/s12350-016-0767-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-016-0767-x