Abstract
Introduction
Radionuclide angiography is widely used for left ventricular function assessment. This study establishes normative data and inter-study repeatability on peak ventricular filling and emptying rates obtained by a cadmium–zinc–telluride SPECT camera.
Method
Cancer patients (N = 764) without diabetes or cardiovascular diseases referred for baseline assessment of cardiac function were included. Repeatability was assessed in 46 patients where two separate acquisitions were performed. Left and right ventricular emptying rates (LPER, RPER) and filling rates (LPFR, RPFR) were obtained and whenever possible also atrial filling rates (PFRa).
Results
Filling rates were higher in women than men. Emptying rates tended to increase with age, whereas filling rates and the E/A ratio decreased. One patient was excluded from the repeatability analysis due to an unexplained high intra-observer variation. Intraclass correlation coefficients for LPER, RPER, LPFR, and RPFR were 0.99, 0.94, 0.99, and 0.84, no proportional biases were detected.
Conclusion
Reference values and relations to age and gender in chemotherapy-naïve cancer patients without cardiopulmonary disease are presented. The CZT camera provides reproducible estimates of peak emptying and filling rates.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Advances in cancer treatment regimens as well as screening procedures has improved survival and resulted in an increase in long-term cancer survivors.1,2 As a consequence, management of potential long-term treatment side effects, of which cardiovascular complications are frequent, is becoming a major challenge. Chemotherapy-induced cardiac damage may be induced by a direct toxic effect in the heart or as an accelerated development of cardiovascular disease, and may appear up to years after the initiation of treatment.3
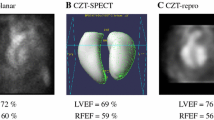
Monitoring cardiac function during treatment with potentially cardiotoxic chemotherapy is, therefore, of increasing importance. Usually this is addressed by serial assessments of left ventricular ejection fraction (LVEF) performed using echocardiography, magnetic resonance imaging or multi-gated radionuclide angiography,1,2 the latter acquired with either planar acquisition or single-photon emission computer tomography (SPECT).
However, it is likely that a substantial change in LVEF does not occur until an advanced stage of the pathological process where a critical amount of myocardial damage has taken place.2,4 This stresses the need for markers of early pathological changes in myocardial function.
Several studies using echocardiography or cardiac magnetic resonance have suggested ventricular diastolic dysfunction as an early indicator of chemotherapy-induced myocardial damage.5,6,7 Left ventricular peak filling rate is a frequently studied parameter and is supposed to reflect ventricular relaxation during diastole, similar to measurements obtained from mitral flow velocities in echocardiography.8 Thus, ventricular filling rates might be of clinical value in the evaluation of cardiac function in these patients.
A new type of dedicated cardiac SPECT gamma camera equipped with Cadmium Zinc Telluride (CZT) detectors in stationary multipinhole-collimators has improved the spatial and energy resolution, acquisition time, and sensitivity as compared to traditional NaI crystal gamma cameras.9,10,11 As reference values of cardiac function derived from nuclear methods may vary with the acquisition method and software used,12 normative data for this type of camera is needed.
Previously, we provided normative data on left and right ventricle ejection fraction.13 However, normal ranges for left and right ventricle filling and emptying rates estimated with the CZT camera technique has not been established previously. In the present study, we address this by investigating chemotherapy-naïve cancer patients without cardiovascular disease referred for baseline measurement of LVEF prior to chemotherapeutic treatment.
Second, we wish to examine age and gender dependence and assess interstudy repeatability in serial acquisitions in individual subjects.
Methods
Population
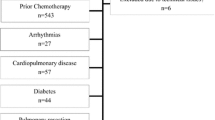
In the period from October 1st 2012 to February 28th 2016, we performed routine assessments of left ventricular function in 1976 patients (Figure 1). Patients were excluded if they had diabetes, pleural effusions, prior lung resection, previous cancer-related chemotherapy, known cardiovascular disease including atrial flutter/fibrillation, cardiac insufficiency, valve disease, myocardial infarction, coronary revascularization, and cardiac arrhythmias treated medically or with pacemaker. Additionally, patients who could not be placed in the camera (due to large thoracic circumferences or patients unable to rest with their left arm above the head) were not included.(A total of 764 patients (348 men and 416 women) were included. Among these, 37% had breast cancer, 1% had prostate cancer, 24% hematologic cancers, 27% carcinomas, 18% sarcomas and 8% other cancer forms.
For the additional study of interstudy repeatability, we included 45 patients (10 males, 35 females) referred in the period from October 1st 2012 to February 28th 2016 for assessment of cardiac function prior to (80% of the assessments) or during potentially cardiotoxic chemotherapy. Cancer forms included breast cancer (60%), ovarian cancer, (9%), prostate cancer (4%), renal cancer (4%), hematologic cancers (13%), and sarcomas (9%). The two scans were performed sequentially, interrupted by complete repositioning of the patient from standing on the floor next to the camera (approximately 5 minutes between acquisitions). Patients with BMI > 35 (and thereby increased risk of too high thoracic circumference compromising the ability to focus the heart within the field of view) or patients with irregular heart rhythm during the first acquisition were not asked to participate in this sub study.
The study was approved by the Danish data protection Agency, and informed consent was given in all cases.
Image Acquisition and Processing
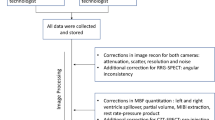
All acquisitions were performed at the Department of Clinical Physiology and Nuclear Medicine at Herlev Hospital. Radionuclide angiographies were performed on a dedicated cardiac CZT SPECT gamma camera, GE Discovery 530c (GE Healthcare, Milwaukee, WI, USA). Each subject was given 550-600 MBq (15-16 mCi) 99mTc-labeled human serum albumin (HSA) intravenously. An acquisition protocol for multigated acquisition, using 16 bins per R-R interval, set to acquire 600 accepted beats, and a 20% energy window centered on 140 keV was carried out.
For image analyses, we used a Xeleris 3 Imaging workstation reorientation software (GE Healthcare, Milwaukee, WI, USA, version no. 3.0562) and Cedars-Sinai QBS processing software (Cedars-Sinai, Los Angeles, CA, revision 2009.0). The software provides values of left and right ventricular peak emptying rates (LPER and RPER) and left and right ventricular filling rates (LPFR and RPFR) using the bicubic spline interpolation of the ventricle volume/time curve, where the filling rate/time curve is computed from the first derivative of the volume/time curve.13
Each acquisition was analyzed twice by two experienced technologists independently of one another, and mean values of the cardiac variables were calculated. Furthermore, secondary peak filling rates, reflecting the late atrial filling were obtained (PFRa) and the ratio between early (PFR) and late (PFRa) peak filling rate (E/A ratio) was calculated.14
Additional Data
Gender, age, reason for referral, blood pressure, heart rate, body weight, body height, information about hypertension, hypercholesterolemia and smoking status were registered prior to the scans.
Statistical Analysis
For the normative data, non-parametric statistics was used as the data could not be expected to be normally distributed. Mann–Whitney U test was used to test for gender differences. Relations between age and cardiac and hemodynamic variables was tested using Kruskal–Wallis test.
Interstudy repeatability was assessed by calculating the intraclass correlation coefficient (ICC) with 95% confidence intervals for the two acquisitions. Furthermore, to exclude proportional bias, Bland–Altman analysis was carried out by calculating the differences and the mean values, as well as 95% CI of the differences.15,16
We used the software package R (version 3.4.1) for statistical evaluation.
Results
Establishment of Normative Data
An overview of demographic data is presented in Table 1. Men were older, taller, had higher blood pressure and a higher incidence of hypertension and tobacco use than women.
Peak filling rates for both ventricles were higher in women, and left ventricular peak emptying rate was higher in men (Table 2).
Peak emptying and filling rates in both ventricles are illustrated divided in age groups in Figures 2 (men) and 3 (women). Table 3 presents relations between the cardiac variables and age, heart rate and blood pressure, in men (A) and women (B).
Mean left (A) and right (B) peak filling and emptying rates for men by age groups. Peak emptying rates are displayed as absolute values. Error bars: standard error of the mean. Age groups: < 30 years (n = 18), 30–40 years (n = 12), 40–50 years (n = 32), 50–60 years (n = 61), 60–70 years (n = 116), 70–80 years (n = 87), > 80 years (n = 22)
Mean left (A) and right (B) peak filling and emptying rates for women by age groups. Peak emptying rates are displayed as absolute values. Error bars: Standard error of the mean. Age groups: < 30 years (n = 23), 30–40 years (n = 28), 40–50 years (n = 66), 50–60 years (n = 78), 60–70 years (n = 106), 70–80 years (n = 106), > 80 years (n = 35)
In women, PFR decreased and PER increased with age for left ventricle (Figure 3 and Table 3b). In men, PFR decreased for both ventricles, and right PER increased with age (Figure 1 and Table 3a).
In 576 patients (75% of the population, 267 men and 309 women), left PFRa was obtainable from the LV filling curve, allowing for calculation of the LV E/A ratio. There was a significant gender difference with a median E/A ratio of 2.0 (0.1-18) in women and 1.6 (0.2-18) in men (P < 0.001). As illustrated in Figure 4a and b, the E/A ratio decreased with age in both genders (P < 0.001). For the right ventricle, PFRa could not be defined in any cases.
Interstudy Repeatability
ICC and 95% confidence intervals for LPER, RPER, LPFR, and RPFR were 0.99 (0.99-1.00), 0.94 (0.89-0.97), 0.99 (0.98-0.99), and 0.84 (0.72-0.91), respectively. No significant proportional bias was detected for any of the variables.
One patient had an extremely high influence on the simple linear regression analysis performed to identify proportional bias (Cook’s distance > 1). A review of the raw data revealed a high intra-observer variation for both acquisitions. Subsequently, this patient was excluded from the analysis.
Discussion
Monitoring LVEF estimated by either radionuclide angiography or echocardiography is an essential part of treatment with anthracyclines and Trastuzumab. Improvement of camera technologies allows estimation of emptying and filling rates during the cardiac cycle, which might be a useful supplement in the evaluation of cardiac function in these patients.
In a previous work, using planar radionuclide ventriculography in 34 breast cancer patients treated with anthracycline, we found a significant decrease in LVEF, accompanied by only marginal changes in PFR,17 suggesting that diastolic variables derived from a nuclide angiography do not add significant information to LVEF measurements. However, the improved resolution, sensitivity and discrimination of the ventricles of the CZT-detector SPECT technique might reveal effects that are not detectable with planar scintigraphy. Cochet and colleagues18 used planar radionuclide angiography to assess diastolic and systolic variables of the LV and found that the time to PFR predicted cardiotoxicity during subsequent treatment with Trastuzumab in Anthracycline-treated breast cancer patients treated, while LVEF did not. On the contrary, Reuvekamp et al19 found with the same technique that although LV PFR decreased during primary Trastuzumab treatment, LVEF decreased similarly. Dores et al20 investigated Trastuzumab-treated patients with echocardiography and found a reduction in early diastolic filling velocity, but no change in other diastolic or systolic parameters. Thus, the potential role of filling and emptying rates in the evaluation of cardiac function during treatment with anthracyclines and/or Trastuzumab is not yet completely understood.
In the present study, we compiled reference values of cardiac filling and emptying rates determined by our CZT camera in a large population of chemotherapy-naïve cancer patients without cardiovascular disease, representative for the typical patient presented to the oncologist before anticancer treatment. The values presented here are comparable to previous results in healthy populations obtained with planar radionuclide angiography17,18,21,18, as well as gated blood pool SPECT using conventional gamma cameras.19,22 In comparison, Nichols and colleagues found lower values in a group of patients with heart failure (LPER -1.0, LPFR 0.9, RPER -1.6, RPFR 1.3) probably reflecting both left and right caridiac dyfunction in this group.19
Age and Gender Differences
For both ventricles, PFR was larger in women than in men, whereas left ventricle PER was larger in men. Left ventricle PFR decreased with age in both genders. In women, left ventricle PER increased with age, in men the same was the case for the right ventricle PER. In addition, left ventricle E/A ratio decreased with age in both genders.
To our knowledge, gender- and age-specific reference values of dynamic cardiac variables obtained with SPECT radionuclide angiography has not been presented previously.
However, our findings are consistent with results from previous studies using gated planar radionuclide ventriculography, which generally report a negative relationship between LV PFR and age.23,24,25,26 Furthermore, in a myocardial perfusion SPECT/CT study, Akincioglu et al13 found LV PFR to vary with age and gender similar to our data.
From Doppler echocardiography studies, which distinguishes between early and late ventricular filling, LV early PFR as well as the E/A ratio is known to decrease with age for both men and women.14,27 Gender differences have not been studied as intensely, however, several studies have reported lower early filling velocity as well as E/A ratio in women, consistent with our findings.28 In a cardiac MRI study, Maceira et al29,30 found peak rate of the early, passive ventricular filling (corresponding to PFR in the present study) to decrease with age in both genders and both ventricles. The same was the case for E/A ratio. Thus, our findings are consistent with data from studies using other techniques to investigate cardiac function. Furthermore, we also included measures of RV function, which generally showed the same age and gender dependencies as the LV.
Age-Related Diastolic Dysfunction
The finding that early filling rate correlated positively to age might reflect increasing prevalence of diastolic dysfunction with age.31 Important age-related changes in the heart includes increased size of fewer myocytes and asymmetric myocardial thickening with the largest increase in the interventricular septum, resulting in changes in cardiac shape, wall stress and contractile function.32 An increasing amount of collagen causes decreased elasticity of the ventricle, decreased wall compliance and compromised LV filling in the early diastole. Reduced rates of calcium reuptake in the myocardial sarcoplasmic reticulum calcium ATPase (SERCA2a) might delay ventricular relaxation, thus enhancing this effect. The late diastolic filling caused by atrial contraction might therefore increase, causing increased atrial pressure and risk and atrial hypertrophy.33
We have previously found that ventricular volumes decreased while ejection fraction increased with age in the current population,34 possibly caused by decreased wall compliance and thus compromised diastolic filling. However, this effect was only demonstrated in the left ventricle for women. The current finding confirms this and extends it to include both ventricles and both genders. This suggests PFR and E/A ratio assessed with multi-gated radionuclide angiography could be used as more sensitive measures of early diastolic dysfunction. An alternative explanation might be that more subjects were included in the current study.
Repeatability
In 44 of the 45 subjects, we found a very high repeatability. In a single case (corresponding to 2% of the included population) there was a strikingly high variation between the estimates calculated by the two observers. Careful subsequent review of the raw data did not provide an explanation for that, except for a high heart rate in this patient (103 beats per minute), which might be a contributing factor. However, this case was easily identified by the high inter-observer variation. Thus, given a high agreement between the values obtained by two technologists the estimates seems to be highly reliable.
Limitations
In the present study, we provide age- and gender-specific normal ranges for left and right ventricular peak emptying and filling rates using CZT-detector technique. We included a large sample of newly diagnosed cancer patients prior to chemotherapeutic or radiation treatment with no known cardiovascular or pulmonary disease, thus with regard to the cardiopulmonary system it might be considered a normal population. However, it should be noted that this is an approximation.
Conclusion
Peak filling and emptying rates for left and right ventricle using multi-gated radionuclide angiography with a CZT camera are reproducible in terms of inter-observer variation and short-term repeatability. We present normative data of these dynamic cardiac variables obtained from a large group of patients without cardiovascular disease, representative for the typical patient presented to the oncologist before anticancer treatment.
Further studies are required to determine whether these variables are clinically useful as early markers of subclinical cardiotoxicity in chemotherapeutic treatment before a decrease in ejection fraction is detectable.
New Knowledge Gained
We assess cardiac function with a cardiac-dedicated cadmium–zinc–telluride detector camera and report normal values in a large group of chemotherapy-naïve cancer patients without diabetes or known cardiovascular or pulmonary disease. Furthermore, we investigate and describe relationships to age and gender. These data might allow the dynamic cardiac variables to be included as additional parameters in the monitoring of cardiac function in cancer patients receiving potentially cardiotoxic chemotherapy.
Abbreviations
- CZT:
-
Cadmium zinc telluride
- LV:
-
Left ventricle
- LVEF:
-
Left ventricular ejection fraction
- MUGA:
-
Multigated acquisition scan
- NaI:
-
Sodium iodide
- R/LPER:
-
Right/left ventricle peak emptying rate
- R/LPFR:
-
Right/left ventricle peak filling rate
- SPECT:
-
Single-photon emission computed tomography
References
Carver JR, Shapiro CL, Ng A, et al. American Society of Clinical Oncology clinical evidence review on the ongoing care of adult cancer survivors : Cardiac and pulmonary late effects late effects of cancer. J Clin Oncol 2016;25:3991-4008.
Curigliano G, Cardinale D, Suter T, et al. Cardiovascular toxicity induced by chemotherapy, targeted agents and radiotherapy: ESMO clinical practice guidelines. Ann Oncol 2012;23:155-66.
Zamorano JL, Lancellotti P, Muñoz DR, et al. 2016 ESC position paper on cancer treatments and cardiovascular toxicity developed under the auspices of the ESC committee for practice guidelines: The task force for cancer treatments and cardiovascular toxicity of the european society of cardiology (ESC.). Russ J Cardiol 2017;143:105-39.
de Geus-Oei L-F, Mavinkurve-Groothuis AMC, Bellersen L, et al. Scintigraphic techniques for early detection of cancer treatment-induced cardiotoxicity. J Nucl Med Technol 2013;41:170-81.
Nagiub M, Nixon JV, Kontos MC. Ability of nonstrain diastolic parameters to predict doxorubicin-induced cardiomyopathy: A systematic review with meta-analysis. Cardiol Rev 2018;26:29-34.
Ong G, Brezden-Masley C, Dhir V, et al. Myocardial strain imaging by cardiac magnetic resonance for detection of subclinical myocardial dysfunction in breast cancer patients receiving trastuzumab and chemotherapy. Int J Cardiol 2018;261:228-33.
Nair N, Gongora E. Heart failure in chemotherapy-related cardiomyopathy: Can exercise make a difference? BBA Clin 2016;6:69-75.
Nagueh SF, Smiseth OA, Appleton CP, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 2016;29:277-314.
Bocher M, Blevis IM, Tsukerman L, et al. A fast cardiac gamma camera with dynamic SPECT capabilities: Design, system validation and future potential. Eur J Nucl Med Mol Imaging 2010;37:1887-902.
Songy B, Lussato D, Guernou M, et al. Comparison of myocardial perfusion imaging using thallium-201 between a new cadmium–zinc–telluride cardiac camera and a conventional SPECT camera. Clin Nucl Med 2011;36:776-80.
Garcia EV, Faber TL, Esteves FP. Cardiac dedicated ultrafast SPECT cameras: new designs and clinical implications. J Nucl Med 2011;52:210-7.
Hesse B, Lindhardt TB, Acampa W, et al. EANM/ESC guidelines for radionuclide imaging of cardiac function. Eur J Nucl Mol Imaging 2008;35:851-85.
Akincioglu C, Berman DS, Nishina H, et al. Assessment of diastolic function using 16-Frame 99m Tc-Sestamibi gated myocardial perfusion SPECT: normal values. J Nucl Med 2005;46:1102-9.
Nagueh SF, Appleton CP, Gillebert TC, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography. Eur J Echocardiogr 2009;10:165-93.
Martin Bland J, Altman D. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986;327:307-10.
Bland JM, Altman DG. Measuring agreement in method comparison studies. Stat Methods Med Res 1999;8:135-60.
Cochet A, Quilichini G, Dygai-Cochet I, et al. Baseline diastolic dysfunction as a predictive factor of trastuzumab-mediated cardiotoxicity after adjuvant anthracycline therapy in breast cancer. Breast Cancer Res Treat 2011;130:845-54.
Reuvekamp EJ, Bulten BF, Nieuwenhuis AA, et al. Does diastolic dysfunction precede systolic dysfunction in trastuzumab-induced cardiotoxicity? Assessment with multigated radionuclide angiography (MUGA). J Nucl Cardiol 2016;23:824-32.
Nichols KJ, van Tosh A, De Bondt P, et al. Normal limits of gated blood pool SPECT count-based regional cardiac function parameters. Int J Cardiovasc Imaging 2008;24:717-25.
Dores H, Abecasis J, Correia MJ et al (2013) Detection of early sub-clinical trastuzumab-induced cardiotoxicity in breast cancer patients. Arq Bras Cardiol 100:328–332
Appel JM, Jensen BV, Nielsen DL, et al. Systolic versus diastolic cardiac function variables during epirubicin treatment for breast cancer. Int J Cardiovasc Imaging 2010;26:217-23.
Zavadovsky KV, Krivonogov NG, Lishmanov YB. The usefulness of gated blood pool scintigraphy for right ventricular function evaluation in pulmonary embolism patients. Ann Nucl Med 2014;28:632-7.
Iskandrian AS, Hakki AH. Age-related changes in left ventricular diastolic performance. Am Heart J 1986;112:75-8.
Lee KJ, Southee AE, Bautovich GJ, et al. Normalised radionuclide measures of left ventricular diastolic function. Eur J Nucl Med 1989;15:1237.
Muntinga HJ, Van den Berg F, Knol HR, et al. Normal values and reproducibility of left ventricular filling parameters by radionuclide angiography. Int J Card Imaging 1997;13:165-71.
Miller TR, Grossman SJ, Schectman KB, et al. Left ventricular diastolic filling and its association with age. Am J Cardiol 1986;58:531-5.
Prasad A, Popovic ZB, Arbab-Zadeh A, et al. The effects of aging and physical activity on Doppler measures of diastolic function. Am J Cardiol 2007;99:1629-36.
Ryu DR. Normal reference values for Doppler echocardiography : Influences of ageing, gender and ethnicity. J Cardiovasc Ultrasound 2016;24:112-4.
Maceira AM, Prasad SK, Khan M, Pennell DJ. Reference right ventricular systolic and diastolic function normalized to age, gender and body surface area from steady-state free precession cardiovascular magnetic resonance. Eur Heart J 2006;27:2879-88.
Maceira AM, Prasad SK, Khan M, Pennell DJ. Normalized left ventricular systolic and diastolic function by steady state free precession cardiovascular magnetic resonance. J Cardiovasc Magn Reson 2006;8:417-26.
Wan SH, Vogel MW, Chen HH. Pre-clinical diastolic dysfunction. J Am Coll Cardiol 2014;63:407-16.
Fleg JL, Strait J. Age-associated changes in cardiovascular structure and function: A fertile milieu for future disease. Heart Fail Rev 2012;17:545-54.
Dai D-F, Chen T, Johnson SC, et al. Cardiac aging: From molecular mechanisms to significance in human health and disease. Antioxid Redox Signal 2012;16:1492-526.
Haarmark C, Haase C, Jensen MM, Zerahn B. Pre-chemotherapy values for left and right ventricular volumes and ejection fraction by gated tomographic radionuclide angiography using a cadmium-zinc-telluride detector gamma camera. J Nucl Cardiol 2016;23:87-97.
Disclosure
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The authors of this article have provided a PowerPoint file, available for download at SpringerLink, which summarizes the contents of the paper and is free for re-use at meetings and presentations. Search for the article DOI on SpringerLink.com.
All editorial decisions for this article, including selection of reviewers and the final decision, were made by guest editor Daniel S. Berman, MD.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hansen, N.L., Haarmark, C. & Zerahn, B. Ventricular peak emptying and filling rates measured by gated tomographic radionuclide angiography using a cadmium–zinc–telluride SPECT camera in chemotherapy-naïve cancer patients. J. Nucl. Cardiol. 27, 1193–1201 (2020). https://doi.org/10.1007/s12350-019-01756-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-019-01756-2