Abstract
Background
The significance of post-stress reduction in left ventricular ejection fraction (LVEF) in patients with normal perfusion on adenosine stress/rest imaging remains controversial.
Methods
Consecutive patients who underwent 2-day adenosine gated stress/rest 99mTc-sestamibi imaging and had normal perfusion were analyzed. LVEF was quantified at rest and 1 hour post-adenosine. Patients were followed up for hard (cardiac death or nonfatal MI) and soft (coronary revascularization or congestive heart failure) cardiac events for 24.1 ± 11.0 months.
Results
Of 560 patients included in the study, 135 (24.1%) had a post-stress reduction in LVEF of ≥ 5%. Rest LVEF (P < 0.001), known history of CAD (P = 0.01) and transient ischemic dilatation ratio (P = 0.02) were independent predictors of LVEF reduction. Event-free survivals were similar in patients with and without ≥ 5% LVEF reduction (P = 0.8). The unadjusted hazard ratio (95% CI) for cardiac events for ≥ 5% LVEF reduction was 1.09 (0.55-2.15), P = 0.81, while the hazard ratio adjusted for known history of CAD, smoking, post-stress LVEF and peak heart rate was 0.87 (0.44-1.75), P = 0.71.
Conclusions
Significant post-adenosine reduction in LVEF occurs in about one-fourth of patients with normal perfusion but does not confer adverse prognosis compared with patients without such reduction.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The presence of post-stress reduction in left ventricular ejection fraction (LVEF) by gated single-photon emission computed tomography (SPECT) has been described as a marker of underlying severe/extensive coronary artery disease (CAD) and adverse cardiac events.1,2,3,4,5,6,7,8,9 Although the significance of post-stress reduction in LVEF is more established with exercise stress,10,11,12 it has been also reported with vasodilator stress.5,10,11,12,13 Vasodilator stress with agents, such as adenosine, differs from exercise stress in that it does not cause demand ischemia but it can induce ischemia in the presence of severe coronary artery stenos due to coronary steal syndrome.14,15
Two principle mechanisms have been proposed for the stress-induced reduction in LVEF following both exercise and vasodilator stress.5,8,10,16,17 The first mechanism is a “true” post-stress myocardial stunning of areas with stress-induced ischemia, which can last 1 hour or longer following the end of stress.18,19,20,21,22 The second mechanism pertains to possible underestimation of LVEF due to inaccurate tracking of endocardial surface in areas with severely decreased stress perfusion.5,16,23 Common to both proposed mechanisms is the need for stress-induced perfusion abnormalities (defects), typically of severe degree as these abnormalities are necessary for both the development of true myocardial stunning and grossly inaccurate tracking of endocardial surface on gated stress images leading to underestimation of post-stress LVEF. Interestingly, however, stress-induced reduction in LVEF associated with severe/extensive CAD and/or adverse cardiac events has also been described in patients with normal stress perfusion.8,17 The explanation of this finding is challenging although “balanced ischemia” has been proposed as a possible mechanism.8,17 Yet, the frequency of stress-induced reduction in LVEF with normal stress perfusion has not been fully explored in studies involving large number of patients, including those undergoing vasodilator stress, such as adenosine. Moreover, in the absence of stress-induced ischemia, the significance of post-stress reduction in LVEF remains controversial. The aim of this study is to evaluate the frequency and prognostic value of post-adenosine stress reduction in LVEF in a large cohort of patients with normal perfusion on their scan.
Methods
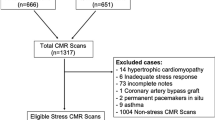
This retrospective study was approved by the Institutional Review Board (IRB) of Jordan University Hospital. The study cohort included all patients with known or suspected coronary artery disease who underwent a clinically indicated two-day adenosine-stress/rest gated SPECT study using 99mTc-sestamibi between January 1, 2015, and October 31, 2017, and had normal perfusion on their scan. The 2-day adenosine-stress/rest gated SPECT 99mTc-sestamibi was the standard myocardial perfusion imaging approach used at our institution during the study period because we intended to investigate the prevalence and prognostic significance of post-adenosine reduction in LVEF, and the 2-day protocol was deemed more suitable for this purpose since any stress-induced myocardial stunning would have completely recovered when patients are imaged at rest on a different day.22
Gated-SPECT Acquisition and Interpretation
Gated adenosine stress SPECT images were obtained 1 hour after injection of 15 mCi (555 MBq) of 99mTc-sestamibi (20 mCi [740 MBq] in obese patients) given 3 minutes into a 6-minute infusion of adenosine at a concentration of 140 µg/kg/min. Gated rest SPECT images were performed within one week thereafter, also 1 hour after injection of 15 mCi(555 MBq) of 99mTc-sestamibi (20 mCi [740 MBq in obese patients) with no intervening cardiac event or intervention between the stress and rest scans.
SPECT images were acquired using a dual-head gamma camera (E.CAM; Siemens Medical Solutions, Malvern, Pennsylvania, USA) equipped with a high-resolution parallel hole collimator with the peak energy set at 140 keV with a 20% window width, 180° rotation arc, 32 projections, 25 s/projection, 16 frames/heart cycle and 64 × 64 matrix. Processing was performed using filtered backprojection to transaxial tomographic images, and these were reoriented to the short, vertical and horizontal long axes. No attenuation correction was performed. We used beat-rejection software to acquire data with a stable R-R interval. A tolerance window of 20% was strictly enforced in all patients included in this study, and all beats outside this window were rejected. Patients with atrial fibrillation and PVCs, who made up about 5% of our patients, were only gated after applying this beat-rejection software.
Both the rest and post-stress scans were visually and semi-quantitatively assessed by two board-certified physicians with > 10 years experience in nuclear cardiology using the quantitative automated software programs QPS and QGS (Cedar Sinai Medical Center, Los Angeles, CA) for the perfusion and functional parameters, respectively.24 Both readers were blinded to patients’ outcome.
Myocardial uptake in a 20-segment model was scored based on a 5-point scale ranging from 0 (normal uptake) to 4 (no detectable tracer uptake) with computation of the summed stress score (SSS) and summed rest score (SRS) for each patient by adding the scores of the 20 segments in the stress and rest images, respectively. The summed difference score (SDS) was computed as SSS-SRS. Scans with a SSS of ≤ 3 were considered negative (normal perfusion). Only patients with normal perfusion are included in the present study. QGS was used to measure the global LVEF, regional wall motion and thickness, LV end-systolic volume (LVESV) and LV end-diastolic volume (LVEDV) at rest and post-stress, while QPS was used to calculate the transient ischemic dilatation (TID) ratio.
The interobserver variability for the LVEF measure at our institution was determined based on ten patients whose rest and post-stress LVEF’s were computed independently by two-board certified physicians using the QGS program. The reproducibility of the rest LVEF was found to be within 2.8%, which represented ± 2 SD of the mean difference between the two rest LVEF measurements performed by the two physicians while the reproducibility of post-stress LVEF was within 4.4% representing ± 2 SD of the mean difference between the two post-stress LVEF measurements.
The intraobserver variability for the LVEF measure was determined based on as set of another ten patients whose rest and post-stress LVEF’s were computed twice by the same board-certified physician using the QGS program. In this case, the reproducibility of the rest and post-stress LVEF’s was identical, within 2.6% representing ± 2 SD of the mean difference between the two rest LVEF measurements or the two post-stress LVEF measurements performed by the same physician.
Patient Outcome
Patients were followed up for both hard (cardiac death or nonfatal MI) and soft (coronary revascularization and congestive heart failure requiring hospitalization) cardiac events by review of hospital records and by telephone contact with the patient, relatives or referring physician. The mean follow-up period was 24.1 ± 11.0 months. Cardiac death was defined as that due to MI or sudden cardiac death ascertained as such by trained board-certified emergency room physicians or cardiologists.25 Nonfatal MI was defined based on the third universal definition, the hallmark of which is the detection of a rise and/or fall of cardiac biomarker values, with at least one of the values being elevated (i.e., > 99th percentile upper reference limit, URL). High sensitivity troponin I is used in our laboratory in addition to one of the following conditions: symptoms suggestive of myocardial infarction, ECG changes, evidence of myocardial damage or identification of coronary thrombus. Coronary revascularization is defined as either percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG). Congestive heart failure hospitalization is defined as hospitalization due to pulmonary edema diagnosed by clinical criteria, laboratory data and echocardiography.
Statistical Analysis
Categorical variables, reported as frequencies and as percentages, were compared using Pearson’s χ2 test or Fisher Exact test, as appropriate. Mann-Whitney U test was used to compare continuous variables. These were reported using means ± the standard deviations.
We examined the frequency, prognostic significance and predictors of LVEF reduction thresholds of ≥ 5% and ≥ 10%, as previously reported in the literature.7,8,9,23 Cardiac event-free survivals for reduction in LVEF ≥ 5% and < 5% were compared using Kaplan-Meier plots and log rank test. The same approach was used to compare cardiac event-free survivals for reduction in LVEF ≥ 10% and < 10%. Hazard ratios for reductions in LVEF ≥ 5% and ≥ 10% were obtained through the Cox proportional hazard model.
Univariate analysis was first carried out to identify which variables among all possible variables known by published literature to potentially affect a certain outcome, such as LVEF reduction or cardiac events were significant predictors in our patient population. The variables included were age, sex, family history of CAD, known history of CAD, diabetes, hypertension, dyslipidemia, rest LVEF, post-stress LVEF, delta LVEF, TID ratio, rest and post-stress LVEDVs, rest and post-stress LVESVs and heart rate response (HRR), defined as maximum percent change in baseline heart rate post-adenosine.26
Multivariate analyses for possible independent predictor variables of cardiac events and LVEF reductions of ≥ 5% and ≥ 10% were carried out using the logistic regression model. Only significant variables (P ≤ 0.05) by univariate analysis were entered into the multivariate analysis. Statistical significance was determined at two-sided P value ≤ 0.05. Analyses were performed in R version 3.5.0 and relevant package.27
Results
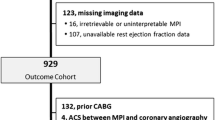
The database query for the time period between January 1, 2015, and October 31, 2017, yielded 587 patients who underwent 2-day adenosine-stress/rest gated SPECT study using 99mTc-sestamibi and had normal perfusion on their scan. Of those, 27 patients (4.6%) were lost to follow-up leaving a final study cohort of 560 patients. Table 1 shows the baseline characteristics of these patients.
History of CAD was confirmed in 229 of the 560 patients (41%) by the presence of documented prior myocardial infarction or the documentation of CAD by coronary angiography of which 72% required coronary revascularization.
ECG changes suggestive of ischemia (ST-depression ≥ 1 mm of horizontal or downsloping depression of the ST-segment 80 ms after the J-point) were seen in only 11% of the patients. No ST-elevation was observed.
Post-stress Change in LVEF and LV Volumes
Change in LVEF was normally distributed (P = 0.13 based on Shapiro’s test indicting lack of departure from normality). The mean (± SD) change in LVEF was − 0.8% ± 5.3% (range; − 18% to 18%). Two hundred ninety-one patients (52%) had > 0% reduction vs. 221 (39%) with > 0% increase in LVEF. Forty-eight patients (9%) had no change in their LVEF. Hundred and thirty-five patients (24.1%) had ≥ 5% reduction vs 86 (15%) with ≥ 5% increase in LVEF and 28 patients (5%) had ≥ 10% reduction vs 14 (2.5%) with ≥ 10% increase in LVEF.
Tables 2 and 3 show the distribution of clinical, perfusion and functional parameters in patients with LVEF reductions of ≥ 5% and ≥ 10% as compared to those with < 5% and < 10% reduction.
The mean post-stress LVEF reduction in the 135 patients with ≥ 5% reduction was − 7.7 ± 2.6% (range − 5 to − 18%), whereas the mean post-stress LVEF reduction in the 28 patients with ≥ 10% reduction was − 11.6 ± 1.9% (range − 10 to − 18%).
In patients with ≥ 5% reduction in LVEF, the mean post-stress LVEDV was 94 ± 31 mL, not significantly different from the mean rest LVEDV of 90 ± 31 mL (P = 0.19). In contrast, the mean post-stress LVESV was significantly higher than the mean rest LVESV (39 ± 24 vs 32 ± 23 mL; P < 0.001). Thus, the ≥ 5% LVEF reduction was due to an increase in LVESV rather than a decrease in LVEDV. Similar findings were seen in patients with ≥ 10% LVEF reduction. In patients without ≥ 5% or ≥ 10% LVEF reduction, no significant change was noted in either LVEDV or LVESV following adenosine stress (P = 0.27-0.56).
Predictors of Post-stress Reduction in LVEF
In univariate analysis, among age, gender, family history of CAD, known history of CAD, smoking, hypertension, diabetes, rest LVEF, rest LVEDV, rest LVESV, post-stress LVEF, post-stress LVEDV, post-stress LVESV, TID ratio, baseline HR, peak HR and HRR, only known history of CAD, rest LVEF, post-stress LVEF, rest LVESV, post-stress LVESV and TID ratio were significantly associated with LVEF reduction of ≥ 5% (Table 2). Rest LVEF, post-stress LVEF and rest LVESV were significantly associated with LVEF reduction of ≥ 10% (Table 3).
There was no difference in HRR post-adenosine between patients with ≥ 5% or ≥ 10% reduction in LVEF vs those without such reductions (P = 0.99 and 0.11, respectively). Blunted HRR defined as < 20% maximum percent change in baseline heart rate was seen in 50% of patients with ≥ 5% vs 49% of patients with < 5% reduction in LVEF (P = 0.88). Similarly, there was no relationship between blunted HRR and reduction in LVEF of ≥ 10% (27% in patients with ≥ 10% vs. 50% in patients with < 10% reduction, P = 0.22). Finally, no significant association was found between adenosine-induced ischemic ST-depression and LVEF reduction of ≥ 5%; 15% of those patients had ischemic ST-depression vs 10% inpatients without ≥ 5% reduction (P = 0.32). There was also no significant difference (P = 0.11) in the rate of adenosine-induced ischemic ST-depression between patients with and without ≥ 10% LVEF reduction.
At multivariate analysis performed with the significant variables by univariate analysis, only known history of CAD, rest LVEF and TID ratio were significant predictors of LVEF reduction of ≥ 5% whereas only rest LVEF was a significant predictor of LVEF reduction of ≥ 10% (Tables 4, 5).
Figure 1 shows the relationship between the rest LVEF and change in LVEF in all patients. Significant inverse correlation is found between the two variables (r = − 0.26, P < 0.001).
Predictors of Cardiac Events
After a mean follow-up period of 24.1 ± 11.0 months, 45 patients (8%) had a cardiac event, including 4 (0.7%) hard (2 cardiac deaths and 2 nonfatal MI) and 41(7.3%) soft events (35 revascularization and six congestive heart failure requiring hospitalization).
Table 6 shows the potential variables that may predict cardiac events in the study population. Among those variables, only known history of CAD, smoking, post-stress LVEF and peak HR were significant predictors of future cardiovascular events. In contrast, change in LVEF as continuous variable or as a cutoff reduction of 5% or 10% was not a significant predictor (P = 0.91, 0.96 and 0.27, respectively).
There was no significant difference in HRR between patients with and without cardiac events (17.2 ± 15.8 vs 23.2 ± 18.4 beats/min; P = 0.21), and no significant association was found between blunted HRR and cardiac events; cardiac event rate was 12% in patients with blunted HRR vs 7% in those without HRR blunting (P = 0.31).
At multivariate analysis, only known history of CAD was a significant predictor of cardiac events (P < 0.001) (Table 7).
Post-stress Reduction in LVEF and Cardiac Events
Eleven of the 135 patients (8.1%) who had ≥ 5% reduction in their LVEF had cardiac events (0% hard, 8.1% soft). The soft events included ten revascularization and one congestive heart failure requiring hospitalization. Thirty-four of the 425 patients (8%) with < 5% LVEF reduction had cardiac events, including 4 (1%) hard (two cardiac deaths and two nonfatal MI) and 30(7%) soft events (25 revascularization and five congestive heart failure requiring hospitalization). No significant differences in the hard, soft or total cardiac event rates were found between the patients with and without ≥ 5% LVEF reduction (P = 0.58, 0.82 and > 0.99, respectively; Fig. 2A). There were also no significant differences in the hard, soft or total cardiac event rates between patients with ≥ 10% vs. those with < 10% reduction in LVEF (P > 0.99, = 0.14 and = 0.27, respectively; Fig. 2B).
A Total, soft and hard cardiac event rates in the patients with ≥ 5% post-adenosine reduction in LVEF vs those in the patients without such reduction. B Total, soft and hard cardiac event rates in the patients with ≥ 10% post-adenosine reduction in LVEF vs those in the patients without such reduction
Figure 3A and B show the unadjusted and adjusted Kaplan-Meier event-free survival curves in the patients with and without ≥ 5% and ≥ 10% LVEF reductions.
A Unadjusted and adjusted Kaplan-Meier event-free survival curves in the patients with and without ≥ 5% post-adenosine reduction in LVEF showing similar event-free survivals in both groups of patients (P = 0.8). B Unadjusted and adjusted Kaplan-Meier event-free survival curves in the patients with and without ≥ 10% post-adenosine reduction in LVEF showing similar event-free survivals in both groups of patients (P = 0.2)
Event-free survivals were similar in patients with ≥ 5% reduction in LVEF and those without such reduction (P = 0.8). The unadjusted hazard ratio (95% confidence intervals) for cardiac events was 1.09 (0.55-2.15), P = 0.81, while the hazard ratio adjusted for the variables of known history of CAD, smoking, post-stress LVEF and peak HR was 0.87 (0.44-1.75), P = 0.71. There were also similar event-free survivals in patients with ≥ 10% reduction in LVEF and those without such reduction (P = 0.2). The unadjusted hazard ratio for cardiac events was 1.84 (0.66-5.18), P = 0.25, while the hazard ratio adjusted for the variables of known history of CAD, smoking, post-stress LVEF and peak HR was 1.48 (0.52-4.3), P = 0.46.
Discussion
To our knowledge, this study is the largest reporting on the frequency of LVEF reduction and its prognostic significance in patients who underwent adenosine stress imaging and had normal perfusion on their scan.5,13,28
In the current investigation, about 24% of patients with normal perfusion on adenosine stress imaging had ≥ 5% reduction in their LVEF following adenosine, which is generally considered significant.8,9,17,23 A similar proportion of patients (22%) had such reduction in the study by Ferro et al. albeit in diabetic patients with normal perfusion following exercise or dipyridamole stress.9 Brinkman et al reported an even higher percentage of patients (36.5%) with normal perfusion and ≥ 6% LVEF reduction post-adenosine suggesting that significant reductions in LVEF (≥ 5%) are relatively common in patients undergoing adenosine-stress who have normal perfusion on their scan.28
Factors Affecting Reduction in LVEF
Multivariate analysis of the factors determining post-adenosine reduction in LVEF of ≥ 5% showed that rest LVEF, known history of CAD and the TID ratio were the only independent predictors of such reduction. In Ferro’s study involving only diabetic patients, rest LVEF was also found to be an independent predictor of ≥ 5% LVEF reduction.9 The association of TID ratio with LVEF reduction is expected and explained by the fact that the post-stress LVEF reduction resulted in increased post-stress LV volumes (primarily LVESV) compared with rest, thereby increasing the TID ratio. The association between prior CAD and LVEF reduction may be related to occult coronary microvascular dysfunction (CMD) in these patients with presumably multiple risk factors, including diabetes and hypertension. In fact, diabetes has been reported to result in loss in contractile reserve, presumably due to CMD despite absence of significant CAD.29,30,31,32
LVEF Reduction Post-adenosine Stress and Cardiac Events
Perhaps the most important finding of our study is that, in patients with normal perfusion a post-adenosine LVEF reduction, regardless whether ≥ 5% or ≥ 10% was not associated with increased cardiac events. Lack of association between post-exercise or post-dipyridamole reduction in LVEF and cardiac events was previously reported by Marcassa et al and a similar conclusion was reached by Gomez et al using regadenoson when testing both ≥ 5% and ≥ 10% cutoff reductions in LVEF in patients with and without ischemia.23,33 Interestingly, Ferro et al also reported that their diabetic patients with normal stress perfusion who had ≥ 5% LVEF reduction following exercise or dipyridamole had similar event-free survival to those without such reduction.9
Only one SPECT study using 99mTc-sestamibi with exercise or dipyridamole stress reported lower cardiac event-free survival in patients without-stress induced ischemia who had post-stress reduction in LVEF of ≥ 5% compared with those without such reduction. However, this study was small, involving only 114 patients of whom the majority (63%) underwent exercise rather than vasodilator stress.8
Proposed Mechanisms of LVEF Reduction Post-adenosine
Considering the lack of prognostic significance of post-stress LVEF reduction in patients with normal perfusion in our and in most other studies, it is intriguing to speculate about the mechanism(s) of such reduction. It seems unlikely that the LVEF reduction is due to post-ischemic myocardial stunning caused by “balanced” global ischemia not apparent on the perfusion scan considering the similar cardiac event rates (both hard and soft) observed in our patients with and without a significant post-stress LVEF reduction and the lack of any hard cardiac events in the former patients after a mean follow-up of 2 years. In fact, a previous report by Supino et al showed that in patients with 3-vessel disease treated only medically the hard event rate (cardiac death or nonfatal MI) in those with ≥ 5% post-exercise reduction in LVEF was about 5% per year (2.8% with 0 to 7% LVEF reduction and 6.9% with ≥ 8% LVEF reduction) or about 10% over 2 years.34 Thus, we would have expected a hard event rate of about 10% in two years in our patients with ≥ 5% LVEF reduction (of whom about half had ≥ 8% LVEF reduction) if those patients truly had 3-vessel CAD (or ≥ 50% left main stenosis) and our sample size would have sufficed to detect this rate. In our study, no hard cardiac events were observed in any patient with ≥ 5% or ≥ 10% reduction although all of these patients underwent medical treatment only following the index scan. Another noteworthy observation is that although just nine of our patients with ≥ 5% LVEF reduction underwent diagnostic coronary angiography based on a clinical indication other than the adenosine scan result, only one had severe/extensive CAD (defined a ≥ 50% left main stenosis or ≥ 70% stenosis of the LAD, circumflex and RCA or their major branches), not significantly different from the 2 of 31 patients with < 5% LVEF reduction who also underwent diagnostic coronary angiography.
Potential explanations include measurement errors in determining the LVEF using the QGS program that may exceed 4% in some patients which may be the case with high background activity adjacent to the myocardium and marked attenuation-related defects (breast and/or diaphragmatic attenuation artifacts) resulting in inaccurate endocardial tracking with overestimation of LVESV and underestimation of LVEF akin to one of the proposed mechanisms of measured decreased LVEF in patients with severe true perfusion defects.5,16 The reproducibility of LVEF measurement at our institution measured by two operators and by one operator at two different times was within 4.4%, which is similar to the 5.2% reproducibility of LVEF measurement determined by Johnson et al who considered only a reduction greater than 5% (i.e., ≥ 6%) as significant.10 To account for potentially higher measurement errors, we examined a higher threshold of a significant reduction in LVEF of ≥ 10% with no change in overall study conclusions.
Although the change in LVEF in the overall cohort was essentially normally distributed with only a very small shift to the right, the somewhat higher percentage of patients with LVEF reduction compared with LVEF increase suggests that there may a “real” effect behind the more frequent LVEF reductions.
One possible mechanism could be autonomic dysfunction, especially in patients with diabetes who comprised about half of our patients. Heart rate response (HRR) post-adenosine can serve as a simple marker of autonomic dysfunction but, in our study, there was no difference in HRR between patients with ≥ 5% or ≥ 10% reduction in LVEF vs those without such reductions. Moreover, HRR blunting, defined as < 20% maximum percent change in baseline heart rate was seen in almost equal proportions of patients with ≥ 5% and < 5% reduction in LVEF with no significant difference in HRR blunting between patients with ≥ 10% vs < 10% reduction in LVEF although the sample sizes for the latter comparison is quite small.
We can only speculate about other possible mechanism(s) for the observed LVEF reductions in patients with normal perfusion but CMD in patients with known CAD, diabetes and, potentially in the elderly may have contributed to this phenomenon.29,30,31,32
Limitations
One of the limitations of our study is its retrospective nature and that it was conducted at a single institution. We did not have a sufficient number of patients who underwent coronary angiography to draw firm conclusions regarding the presence of severe and/or extensive CAD in patients with significant post-stress reduction in LVEF vs those without because patients with normal perfusion typically do not undergo coronary angiography unless other findings are present compelling the cardiologist to perform coronary angiography. Reduction in LVEF with normal perfusion is also normally not an indication for coronary angiography without other compelling findings. This was one of the main reasons for using cardiac events as the primary endpoint in our study. Due to the retrospective nature of the study, we could not study the post-stress reduction in LVEF at more than one timepoint, for example at 30 min, 1 and 2 h to determine the time of peak decline in LVEF and eventual recovery in patients who showed LVEF reduction. Finally, despite our sample size being the largest to date in this particular patient population, it is insufficient to detect small differences in outcome rates considering that those are quite low. Yet, our study can be considered as hypothesis-generating and might lead to larger studies for further investigation and confirmation.
New Knowledge Gained
Significant (≥ 5%) and even marked (≥ 10%) reductions in LVEF following adenosine do not seem to be associated with adverse prognosis compared with patients without such reduction when the stress/rest gated adenosine SPECT study is normal. The post-adenosine LVEF reduction in this setting is probably not related to “balanced ischemia” and is likely to be seen more often in patients with known CAD and those patients with higher rest LVEF.
Conclusion
The present study showed that significant post-adenosine stress reduction in LVEF does not confer an adverse prognosis and is not an independent prognosticator in patients with normal perfusion on 99mTc-sestamibi myocardial perfusion scan. However, due to the relatively small sample size of our study and the relatively low event rates, our study conclusions are preliminary and need to be supported by larger studies. If confirmed, this may have implications in management of patients with normal perfusion and normal LVEF on their post-stress scan.
Abbreviations
- EF:
-
Ejection fraction
- LV:
-
Left ventricular
- MBq:
-
Megabecquerel
- mCi:
-
Millicurie
- SPECT:
-
Single photon emission computerized tomography
- SSS:
-
Summed stress score
- SRS:
-
Summed rest score
- SDS:
-
Summed difference score
- Tc-99m:
-
Technetium-99m
- MI:
-
Myocardial infarction
References
Dorbala S, Ananthasubramaniam K, Armstrong IS, Chareonthaitawee P, DePuey EG, Einstein AJ, et al. Single photon emission computed tomography (SPECT) myocardial perfusion imaging guidelines: Instrumentation, acquisition, processing, and interpretation. J Nucl Cardiol. 2018;25:1784-846.
Sharir T, Bacher-Stier C, Dhar S, Lewin HC, Miranda R, Friedman JD, et al. Identification of severe and extensive coronary artery disease by postexercise regional wall motion abnormalities in Tc-99m sestamibi gated single-photon emission computed tomography. Am J Cardiol. 2000;86:1171-5.
Paul AK, Hasegawa S, Yoshioka J, Mu X, Maruyama K, Kusuoka H, et al. Characteristics of regional myocardial stunning after exercise in gated myocardial SPECT. J Nucl Cardiol. 2002;9:388-94.
Emmett L, Iwanochko RM, Freeman MR, Barolet A, Lee DS, Husain M. Reversible regional wall motion abnormalities on exercise technetium-99m-gated cardiac single photon emission computed tomography predict high-grade angiographic stenoses. J Am Coll Cardiol. 2002;39:991-8.
Druz RS, Akinboboye OA, Grimson R, Nichols KJ, Reichek N. Postischemic stunning after adenosine vasodilator stress. J Nucl Cardiol. 2004;11:534-41.
Toba M, Kumita S, Cho K, Ibuki C, Kumazaki T, Takano T. Usefulness of gated myocardial perfusion SPECT imaging soon after exercise to identify postexercise stunning in patients with single-vessel coronary artery disease. J Nucl Cardiol. 2004;11:697-703.
Hida S, Chikamori T, Tanaka H, Usui Y, Igarashi Y, Nagao T, et al. Diagnostic value of left ventricular function after stress and at rest in the detection of multivessel coronary artery disease as assessed by electrocardiogram-gated SPECT. J Nucl Cardiol. 2007;14:68-74.
Dona M, Massi L, Settimo L, Bartolini M, Gianni G, Pupi A, et al. Prognostic implications of post-stress ejection fraction decrease detected by gated SPECT in the absence of stress-induced perfusion abnormalities. Eur J Nucl Med Mol Imaging. 2011;38:485-90.
Ferro A, Petretta M, Acampa W, Fiumara G, Daniele S, Petretta MP, et al. Post-stress left ventricular ejection fraction drop in patients with diabetes: A gated myocardial perfusion imaging study. BMC Cardiovasc Disord. 2013;13:99.
Johnson LL, Verdesca SA, Aude WY, Xavier RC, Nott LT, Campanella MW, et al. Postischemic stunning can affect left ventricular ejection fraction and regional wall motion on post-stress gated sestamibi tomograms. J Am Coll Cardiol. 1997;30:1641-8.
Tanaka H, Chikamori T, Hida S, Usui Y, Harafuji K, Igarashi Y, et al. Comparison of post-exercise and post-vasodilator stress myocardial stunning as assessed by electrocardiogram-gated single-photon emission computed tomography. Circ J. 2005;69:1338-45.
Demir H, Tan YZ, Isgoren S, Gorur GD, Kozdag G, Ural E, et al. Comparison of exercise and pharmacological stress gated SPECT in detecting transient left ventricular dysfunction. Ann Nucl Med. 2008;22:403-9.
Chun KA, Cho IH. Adenosine-induced long-standing postischemic left ventricular dysfunction evaluated with gated SPECT. Clin Nucl Med. 2005;30:18-22.
Ben-Haim S, Gips S, Merdler A, Front A, Tamir A. Myocardial stunning demonstrated with rest and post-stress measurements of left ventricular function using dual-isotope gated myocardial perfusion SPECT. Nucl Med Commun. 2004;25:657-63.
Van Tosh A, Votaw JR, Reichek N, Palestro CJ, Nichols KJ. The relationship between ischemia-induced left ventricular dysfunction, coronary flow reserve, and coronary steal on regadenoson stress-gated (82)Rb PET myocardial perfusion imaging. J Nucl Cardiol. 2013;20:1060-8.
Bonow RO. Gated myocardial perfusion imaging for measuring left ventricular function. J Am Coll Cardiol. 1997;30:1649-50.
Dorbala S, Vangala D, Sampson U, Limaye A, Kwong R, Di Carli MF. Value of vasodilator left ventricular ejection fraction reserve in evaluating the magnitude of myocardium at risk and the extent of angiographic coronary artery disease: a 82Rb PET/CT study. J Nucl Med. 2007;48:349-58.
Braunwald E, Kloner RA. The stunned myocardium: prolonged, postischemic ventricular dysfunction. Circulation. 1982;66:1146-9.
Gerber BL, Wijns W, Vanoverschelde JL, Heyndrickx GR, De Bruyne B, Bartunek J, et al. Myocardial perfusion and oxygen consumption in reperfused noninfarcted dysfunctional myocardium after unstable angina: direct evidence for myocardial stunning in humans. J Am Coll Cardiol. 1999;34:1939-46.
Barnes E, Hall RJ, Dutka DP, Camici PG. Absolute blood flow and oxygen consumption in stunned myocardium in patients with coronary artery disease. J Am Coll Cardiol. 2002;39:420-7.
Barnes E, Dutka DP, Khan M, Camici PG, Hall RJ. Effect of repeated episodes of reversible myocardial ischemia on myocardial blood flow and function in humans. Am J Physiol Heart Circ Physiol. 2002;282:H1603-8.
Benz DC, Gaemperli O. The right timing for post-ischemic stunning. J Nucl Cardiol. 2017;24:1302-4.
Gomez J, Golzar Y, Fughhi I, Olusanya A, Doukky R. The significance of post-stress decrease in left ventricular ejection fraction in patients undergoing regadenoson stress gated SPECT myocardial perfusion imaging. J Nucl Cardiol. 2018;25:1313-23.
Sharir T, Germano G, Waechter PB, Kavanagh PB, Areeda JS, Gerlach J, et al. A new algorithm for the quantitation of myocardial perfusion SPECT. II: validation and diagnostic yield. J Nucl Med. 2000;41:720-7.
Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, the Writing Group on behalf of the Joint ESC/ACCF/AHA/WHF Task Force for the Universal Definition of Myocardial Infarction. Third universal definition of myocardial infarction. Circulation. 2012;126:2020-35.
Hage FG, Perry G, Heo J, Iskandrian AE. Blunting of the heart rate response to adenosine andregadenoson in relation to hyperglycemia and the metabolic syndrome. Am J Cardiol. 2010;105:839-43.
Mente S, Kuhn M. The use of the R language for medicinal chemistry applications. Curr Top Med Chem. 2012;12:1957-64.
Brinkman N, Dibbets-Schneider P, Scholte AJ, Stokkel MP. Myocardial perfusion scintigraphy with adenosine: Does it impair the left ventricular ejection fraction obtained with gated SPECT? Clin Nucl Med. 2008;33:89-93.
Mustonen JN, Uusitupa MI, Tahvanainen K, Talwar S, Laakso M, Lansimies E, et al. Impaired left ventricular systolic function during exercise in middle-aged insulin-dependent and noninsulin-dependent diabetic subjects without clinically evident cardiovascular disease. Am J Cardiol. 1988;62:1273-9.
Prior JO, Quinones MJ, Hernandez-Pampaloni M, Facta AD, Schindler TH, Sayre JW, et al. Coronary circulatory dysfunction in insulin resistance, impaired glucose tolerance, and type 2 diabetes mellitus. Circulation. 2005;111:2291-8.
Storto G, Pellegrino T, Sorrentino AR, Luongo L, Petretta M, Cuocolo A. Estimation of coronary flow reserve by sestamibi imaging in type 2 diabetic patients with normal coronary arteries. J Nucl Cardiol. 2007;14:194-9.
Marciano C, Galderisi M, Gargiulo P, Acampa W, D’Amore C, Esposito R, et al. Effects of type 2 diabetes mellitus on coronary microvascular function and myocardial perfusion in patients without obstructive coronary artery disease. Eur J Nucl Med Mol Imaging. 2012;39:1199-206.
Marcassa C, Giubbini R, Acampa W, Cittanti C, Djepaxhija O, Gimelli A, et al. Impact of imaging protocol on left ventricular ejection fraction using gated-SPECT myocardial perfusion imaging. J Nucl Cardiol. 2017;24:1292-301.
Supino PG, Borer JS, Herrold EM, Hochreiter C. Prognostication in 3-vessel coronary artery disease based on left ventricular ejection fraction during exercise: Influence of coronary artery bypass grafting. Circulation. 1999;100:924-32.
Disclosure
The authors have no conflicts of interest to report.
Author information
Authors and Affiliations
Contributions
OSO, MEJ: contributed to the conception and design of the study, analysis and interpretation of data, drafting and final approval of the manuscript. AA, BB, OA, MA, HZ, OA, MAJ, SJ, HJ, OA, OA: actively involved in collecting and analyzing data and approved the of final manuscript.
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The authors of this article have provided a PowerPoint file, available for download at SpringerLink, which summarises the contents of the paper and is free for re-use at meetings and presentations. Search for the article DOI on SpringerLink.com.
Funding
No funding source was used to support this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Obeidat, O.S., Alhouri, A., Baniissa, B. et al. Prognostic significance of post-stress reduction in left ventricular ejection fraction with adenosine stress in Jordanian patients with normal myocardial perfusion. J. Nucl. Cardiol. 27, 1596–1606 (2020). https://doi.org/10.1007/s12350-019-01725-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-019-01725-9