Abstract
Purpose
We assessed the impact of type 2 diabetes, in the presence of other major cardiovascular risk factors, on coronary microvascular function and myocardial perfusion in patients without obstructive coronary artery disease (CAD).
Methods
In this prospective study, 23 patients with type 2 diabetes and 26 nondiabetic patients matched for age, sex and other cardiovascular risk factors underwent a cold pressure test (CPT) and dipyridamole transthoracic echocardiography to determine their coronary flow (CF) ratio. Within 2 weeks, all diabetic patients also underwent dipyridamole-rest myocardial perfusion single-photon emission (MPS) CT. None of the patients with or without diabetes had significant CAD on invasive coronary angiography.
Results
The CPT-CF ratio was significantly lower in diabetic patients than in nondiabetic patients (1.46 ± 0.26 vs. 1.71 ± 0.32, p = 0.006) and was correlated significantly with fasting glycaemia (r = −0.35, p = 0.01), but not with glycated haemoglobin. The dipyridamole-CF ratio was also lower in diabetic patients than in nondiabetic patients (2.38 ± 0.74 vs. 2.75 ± 0.49, p = 0.04). On MPS imaging, 5 diabetic patients (22%) had stress-induced ischaemia and the remaining 18 (78%) had normal myocardial perfusion. The dipyridamole-CF ratio was not different in patients with and without reversible defects (2.3 ± 1.1 vs. 2.4 ± 0.6, p = 0.97).
Conclusion
Coronary microvascular function is impaired in type 2 diabetic patients without significant CAD, compared to nondiabetic patients with similar other cardiovascular risk factors. In the majority of diabetic patients, microvascular dysfunction is associated with normal myocardial perfusion.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Diabetes mellitus is associated with increased cardiovascular risk that has been attributed mainly to its detrimental effects on vascular function [1]. In fact, in diabetic patients without additional cardiac risk factors, endothelial dysfunction has been demonstrated and explained by associated causes, including autonomic dysfunction, chronic hyperglycaemia and insulin resistance [2]. However, the increased cardiac risk in diabetic patients compared to nondiabetic patients becomes more evident only after the age of 50 years, when additional risk factors, mostly hypertension, dyslipidaemia, and obesity, often coexist with diabetes, and substantially contribute to the increase in risk [1]. All major cardiac risk factors, including diabetes, impair endothelial function that represents the earliest step to atherosclerosis, leading to microvascular dysfunction before the development of structural vascular changes or significant coronary artery stenosis [3]. Yet, although endothelial and microvascular dysfunction have been found in diabetic patients in studies comparing them to healthy nondiabetic subjects, in the previous studies diabetic patients were not matched for other major risk factors to their control groups, so that how much diabetes contributes to microvascular dysfunction is not completely clear [4, 5]. Additionally, no studies have evaluated coronary microvascular function and myocardial perfusion in the same patients. The aim of the present study was to assess the impact of type 2 diabetes mellitus, in the presence of other major cardiac risk factors, on coronary microvascular function and myocardial perfusion, comparing two groups of patients with angiographically normal coronary arteries, with and without diabetes, but with comparable additional major risk factors.
Materials and methods
Study population
This was a prospective study enrolling 23 patients with type 2 diabetes and 26 nondiabetic patients, matched for age, sex and other cardiovascular risk factors (Table 1). For enrolment, patients had to fulfil the following criteria: (1) being a candidate for coronary angiography for cardiac symptoms; (2) without significant epicardial vessel stenosis on coronary angiography; (3) without previous myocardial infarction; and (4) with normal regional left ventricular (LV) wall motion, LV ejection fraction (≥55 %), and LV mass index (49–115 g/m2 in men and 43–95 g/m2 in women) [6] on echocardiography. Exclusion criteria included: (1) congestive heart failure; (2) angiographically significant coronary artery disease (CAD), according to the guidelines of the European Society of Cardiology [7]; (3) valvular heart disease; (4) atrial fibrillation; (5) inadequate echocardiographic quality; (6) presence of a cardiac implantable device; and (7) significant endocrine, hepatic, renal, pulmonary, or inflammatory disease. Within the same week, all patients underwent coronary angiography and transthoracic Doppler echocardiography after a cold pressure test (CPT) and dipyridamole infusion performed during the same period of the day (between 9 am and 10 am). Venous plasma and serum samples were taken after an overnight fast on the same day as echocardiography. At the time of coronary angiography, cardiovascular risk factors were recorded, including family history of CAD, being overweight (defined as a body mass index ≥25 kg/m2), arterial hypertension (systolic blood pressure >140 mmHg, diastolic blood pressure >90 mmHg, or taking antihypertensive medication), dyslipidaemia (total serum cholesterol level >200 mg/dl, or taking lipid-lowering medication), smoking (having smoked at least five cigarettes per day within the last month), and cardiovascular and antidiabetic medication. Type 2 diabetes mellitus was defined according to the Standards of Medical Care in Diabetes of the American Diabetes Association [8]. In diabetic patients glycaemia control was assessed by measurement of glycated haemoglobin (HbA1c). All patients with diabetes also underwent dipyridamole-rest myocardial perfusion single-photon emission (MPS) CT within 2 weeks of echocardiography. The local Institutional Review Board approved the study and informed consent was obtained from each participant.
Doppler echocardiography
Standard Doppler echocardiography was performed using a Vivid Seven machine (GE, Horten, Norway) in the morning after an overnight fast of 12–14 h; subjects were instructed to avoid all coffee-containing drinks and theophylline-containing medications, and to abstain from smoking and heavy exercise from 24 h before the study. The distal left anterior descending artery was assessed by colour Doppler recording using a 5-MHz shallow-focus phased-array transducer in a foreshortened apical two-chamber view. The Doppler sample volume was placed on the colour signal of the left anterior descending artery and the spectral pulsed wave-Doppler signal was recorded so as to examine the characteristic biphasic flow velocity pattern with a larger diastolic and a smaller systolic component. The highest three spectral Doppler signals were averaged to measure coronary peak diastolic velocity. The coronary flow (CF) velocity pattern was recorded in each patient at rest and sequentially after CPT by placing the subject’s hand and distal part of the forearm in an ice water slurry for 4 min [8, 9] and after dipyridamole infusion (0.84 mg/kg over 6 min) [10]. The CF ratio was defined as the ratio of hyperaemic (either after CPT or dipyridamole) to resting diastolic peak velocities. Corrected CF values for the CPT studies were also calculated using the following formula: uncorrected value/rate × pressure product × 10−4 [11–13]. Heart rate, arterial blood pressure, and electrocardiography (ECG) were monitored during both the tests. In all patients, the dipyridamole test was performed at least 1 h after CPT. The methods and reproducibility in our laboratory for CF ratio measurement have been previously reported [14, 15]. Two investigators who were blinded to the patient characteristics and the results of MPS imaging analysed the Doppler-derived coronary images off-line.
MPS imaging
All diabetic patients also underwent same-day sestamibi dipyridamole-rest MPS imaging, according to the recommendations of the European Association of Nuclear Medicine and European Society of Cardiology [16] as previously described in detail [17]. Dipyridamole was infused at a dose of 0.56 mg/kg per min intravenously over 4 min. A dose of 100 mg of aminophylline was administered intravenously in the event of chest pain or other symptoms, or after significant ST depression. Heart rate, blood pressure and 12-lead ECG data were recorded at rest, at the end of each stress stage, at peak stress and in the delay phases at rest. Data were acquired using a dual head rotating gamma camera (E.CAM; Siemens Medical Systems, Hoffman Estates, IL) equipped with a low-energy high-resolution collimator and connected to a dedicated computer system. No attenuation or scatter correction was used. A semiquantitative analysis of relative perfusion distribution was performed using standardized segmentation of 17 myocardial segments. An automated software program (Cedars-Sinai Medical Center, Los Angeles, CA) was used to calculate the variables incorporating both the extent and severity of perfusion defects [17, 18]. A scan was considered normal if the summed stress score (SSS) was <3, mildly to moderately abnormal if the SSS was between 3 and 7, and severely abnormal if the SSS was >7, as previously reported [18]. Operators unaware of the CF results analysed the MPS studies.
Statistical analysis
Statistical analysis was performed using SPSS Statistical Software 15.0 (SPSS, Chicago, IL). Continuous variables are expressed as means±SD and categorical data as percentages. Groups were compared using Student t-test for unpaired data and the chi-squared test, as appropriate. Pearson’s correlation was used to assess the relationships between parameters. A p value <0.05 was considered statistically significant.
Results
Characteristics of the study population
A total of 49 patients were enrolled in the study: 23 patients with type 2 diabetes and 26 nondiabetic patients with comparable cardiovascular risk factors (Table 1). In particular, no differences between diabetic and nondiabetic patients were observed in total and low-density lipoprotein cholesterol, triglycerides, systolic and diastolic blood pressure, creatinine, and glomerular filtration rate. No significant differences were observed in the consumption of drugs between diabetic and nondiabetic patients. In diabetic patients, mean HbA1c was 6.7 ± 0.8% and mean duration of diabetes was 7.7 ± 6.9 years. Five of the diabetic patients were in dietary therapy, 11 were taking oral antidiabetic drugs, 2 oral antidiabetic drugs and insulin, and 5 insulin only.
Endothelium-dependent and endothelium-independent vasodilation
The CPT-CF ratio, which reflects endothelium-dependent vasodilation, and the dipyridamole-CF ratio, which reflects endothelium-independent vasodilation, were determined in all 49 patients without major adverse effects or symptoms or ECG changes. CF velocities, blood pressure, heart rate at rest and after CPT or dipyridamole were not significantly different between diabetic and nondiabetic patients (Table 2). The CPT-CF ratio was significantly lower in patients with diabetes than in nondiabetic patients (1.46 ± 0.26 vs. 1.71 ± 0.32, p = 0.006; Fig. 1a). This difference between diabetic and nondiabetic patients remained significant when using CF ratio values corrected for rate-pressure product (1.44 ± 0.53 vs. 1.70 ± 0.38, p < 0.05). The dipyridamole-CF ratio was also lower in diabetic patients than in nondiabetic patients (2.38 ± 0.74 vs. 2.75 ± 0.49, p = 0.043; Fig. 1b). In the whole study population, the CPT-CF ratio values were significantly correlated with fasting glycaemia (r = −0.35, p = 0.01; Fig. 2a), but not with HbA1c (r = −0.13, p = 0.54). When fasting glycaemia was expressed as the natural logarithm, the same results were obtained. The natural logarithm of fasting glycaemia was significantly correlated with the CPT-CF ratio (r = −0.40, p = 0.004; Fig. 2b). However, no significant correlation between fasting glycaemia and the CPT-CF ratio was found when only diabetic patients were considered.
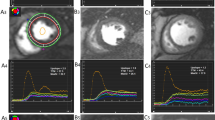
Myocardial perfusion
On stress MPS imaging, 5 of the 23 patients (22%) with diabetes had mild-to-moderate reversible perfusion defects, with a mean SSS of 4.0 ± 0.7. The myocardial perfusion defects were localized in the inferior region in three patients and in the inferoseptal region in two patients. The remaining 18 diabetic patients (78%) had normal myocardial perfusion. Individual values of dipyridamole-CF ratio in diabetic patients with and without stress-induced ischaemia are shown in Fig. 3. Dipyridamole-CF ratio was not different between patients with reversible defects and those with normal perfusion (2.3 ± 1.1 vs. 2.4 ± 0.6, p = 0.97).
Discussion
The findings of the present study demonstrate that in diabetic patients without obstructive CAD, coronary microvascular function is substantially more impaired than in nondiabetic patients matched for cardiovascular risk factors. They also suggest a relevant contribution of endothelium-dependent mechanisms to abnormal microvascular function, as shown by the 42% reduction in CPT-CF ratio compared to nondiabetic subjects. In contrast, the impairment of the dipyridamole-CF ratio, that mainly reflects endothelium-independent vasodilatation, was less evident, supporting the prominent role of endothelial dysfunction as a cause of impaired microvascular function.
Comparison with previous studies
Impairment of coronary epicardial and microvascular function in patients with diabetes has been previously reported [4, 5]. However, in previous studies diabetic patients were usually compared to control groups that substantially differed for the presence of additional cardiovascular risk factors (mostly hypertension and dyslipidaemia) that also exert relevant unfavourable effects on endothelial function. To the best of our knowledge, this is the first study that evaluated endothelium-dependent and independent coronary microvascular function in adult patients with type 2 diabetes mellitus compared to nondiabetic patients without obstructive CAD on coronary angiography, who were matched for all other cardiovascular risk factors, including blood pressure, lipid profile, renal function, and body mass index. Di Carli et al. [4] reported impaired coronary microvascular function, evaluated by PET, in patients with type 1 and 2 diabetes mellitus compared to controls. At variance with our study, in that study the diabetic patients did not undergo coronary angiography, were substantially younger (mean age 39 years) and showed about 1 mmol/dl higher levels of total cholesterol as well higher creatinine and blood pressure values compared to controls, making more uncertain the contribution of diabetes to vascular impairment. More recently, Galderisi et al. [5] also reported reduced CF reserve assessed by dipyridamole transthoracic Doppler echocardiography in hypertensive diabetic patients compared to normotensive nondiabetic subjects with had significantly different blood pressure values. Furthermore, in that study only nonendothelium-dependent vasodilatation was tested [5]. Abnormal epicardial vascular reactivity has also been reported in diabetic hypertensive patients without obstructive CAD and correlated with adverse prognosis [19]. Impaired epicardial coronary reactivity strictly correlates with PET-measured response of myocardial blood flow to CPT [20], consistent with the adverse prognostic role that CF abnormalities play in patients at high cardiac risk [21].
Notably, the CPT-CF ratios observed in the current study were substantially higher than values derived from PET measurements [11–13]. This discrepancy is probably a result of the differences between measurement of absolute CF values with PET and echocardiographic measurement of CF velocity that has no linear correlation with laminar flow. In fact, previous studies evaluating CF velocity by transthoracic Doppler echocardiography [14, 22] or MRI [23] during CPT have found velocity ratios very consistent with the values observed in the present study.
Mechanisms of abnormal microvascular function in diabetes
The findings of the study support the pathogenetic role of diabetes mellitus-mediated endothelial dysfunction. In fact, since diabetic and nondiabetic patients were matched for other major cardiovascular risk factors, the difference in the degree of endothelium-mediated microvascular function observed in our study cannot be explained by the concomitant presence of additional risk factors that is commonly observed in diabetes, and represents, therefore, the contribution of the disease to vascular dysfunction.
Hyperglycaemia-mediated formation of free radicals and nitric oxide inactivation [24], together with protein kinase C activation induced by hyperglycaemia [25] have been reported as peculiar mechanisms of endothelial dysfunction in diabetic patients. Autonomic neuropathy, frequently present in diabetic patients, has also been shown to contribute to endothelial dysfunction [26]. In the present study a significant inverse correlation was found between fasting glycaemia and endothelium-dependent vasodilatation (r = −0.34), but not between fasting glycaemia and endothelium-independent vasodilatation in the whole population, which is similar to the findings reported by Di Carli et al. (r = −0.42) [4]. However, this correlation was not confirmed when only diabetic patients were considered, as also observed by Marini et al. [27], suggesting that pathogenesis of microvascular dysfunction in diabetic patients is multifactorial and also determined by the coexistence of additional major cardiovascular risk factors.
Myocardial perfusion
In the present study, mild-to-moderate reversible perfusion defects were observed on dipyridamole stress MPS imaging in 22% of diabetic patients, whereas no perfusion abnormalities at rest were documented. This is consistent with previous findings using nuclear imaging techniques that demonstrate the effects of endothelial dysfunction on myocardial perfusion [27–31]. In particular, Djaberi et al. [28] reported regional perfusion defects on adenosine-MPS in 32% of 95 diabetic patients without obstructive CAD on multislice CT angiography that were associated with abnormal brachial artery flow-mediated dilation. Storto et al. [30] and Marini et al. [27] also found, using dipyridamole MPS, homogeneously impaired vascular function in diabetic patients, showing regional perfusion defects in about 30% of them. Therefore, endothelial dysfunction might also account, in part, for the reversible perfusion defects noted in 22% of the diabetic patients enrolled in our study. Among patients with cardiac risk factors who do not have significant coronary artery stenosis on angiography, those with reversible SPECT perfusion defects are more likely to have endothelial dysfunction, as evidenced by diminished brachial artery reactivity, than those without stress-induced perfusion abnormalities [30, 31]. In the study by Storto et al. [30], diabetic patients with reversible perfusion defects tended to have lower flow reserve estimates than those without defects (1.02 ± 0.5 vs. 1.51 ± 0.9). Although this difference did not achieve statistical significance, the relatively modest number of subjects in each group limited the statistical power of the study to identify differences in perfusion reserve if any between the two groups.
Study limitations
This study had some limitations that should be considered. First, we evaluated a relatively small number of patients and, therefore, our results need to be confirmed in a larger population. We also acknowledge that trans-thoracic Doppler echocardiography, although widely available and repeatable, provides an indirect estimate of coronary microvascular function compared to absolute flow quantification by PET. In particular, changes in the section of epicardial vessels upon dipyridamole and CPT stimulation may affect measurements of flow velocity. In fact, it has been reported that CPT determines paradoxical vasoconstriction, assessed on invasive angiography, of epicardial atherosclerotic vessels without obstructive stenosis in patients with cardiovascular risk factors [32–34], which may contribute, in addition to reduced microvascular function, to reducing the CPT-CF ratio. The coronary cross-sectional area was not measured in the present study, which may have led to underestimation of the vasodilatation response to CPT and dipyridamole [35]. Thus, lack of simultaneous cross-sectional coronary area and flow velocity prevents precise dissection of the independent contribution of macrovascular and microvascular abnormal reactivity to impaired CF ratios [36]. In addition, lack of MPS data in nondiabetic patients may also represent a limitation of the study. Finally, the absence of coronary artery stenosis on coronary angiography does not necessarily exclude a significant atherosclerotic burden of the vessel wall [37].
Conclusion
This study demonstrated that, in the absence of obstructive CAD, coronary microvascular function is impaired in adult patients with type 2 diabetes mellitus compared to nondiabetic patients with matched cardiovascular risk factors, and contributes to the clarification of the pathogenetic impact of diabetes in fostering the atherosclerotic process and promoting cardiac events. Yet, the relevance of coronary microvascular dysfunction in adult diabetic patients as a prognostic marker or therapeutic target, and whether the occurrence of perfusion abnormalities in some of these patients is associated with adverse prognosis, remain to be elucidated.
References
Schramm TK, Gislason GH, Køber L, Rausmussen S, Rausmussen JN, Abildstrøm SZ, et al. Diabetes patients requiring glucose-lowering therapy and nondiabetics with a prior myocardial infarction carry the same cardiovascular risk: a population study of 3.3 million people. Circulation. 2008;117:1945–54.
Pitkanen OP, Nuutila P, Raitakari OT, Ronnemaa T, Koskinen PJ, Iida H, et al. Coronary flow reserve is reduced in young men with IDDM. Diabetes. 1998;47:248–54.
Camici PG, Crea F. Coronary microvascular dysfunction. N Engl J Med. 2007;356:830–40.
Di Carli MF, Janisse J, Grunberger G, Ager J. Role of chronic hyperglycemia in the pathogenesis of coronary microvascular dysfunction in diabetes. J Am Coll Cardiol. 2003;41:1387–93.
Galderisi M, Capaldo B, Sidiropulos M, D’Errico A, Ferrara L, Turco A, et al. Determinants of reduction of coronary flow reserve in patients with type 2 diabetes mellitus or arterial hypertension without angiographically determined epicardial coronary stenosis. Am J Hypertens. 2007;20:1283–90.
Lang RM, Bieriq M, Devereux RB, Devereux RB, Flachskampf FA, Foster E, et al. Recommendations for chamber quantification. Eur J Echocardiogr. 2006;7:79–108.
Fox K, Garcia MA, Ardissino D, Buszman P, Camici PG, Crea F, et al. ESC guidelines on the management of stable angina pectoris. Eur Heart J. 2006;27:1341–81.
Rodbard HW, Blonde L, Braithwaite SS, Brett EM, Cobin RH, Handelsman Y, et al. American Association of Clinical Endocrinologists medical guidelines for clinical practice for the management of diabetes mellitus. Endocr Pract. 2007;13:1–68.
Wirch JL, Wolfe LA, Weissgerber TL, Davies GA. Cold pressor test protocol to evaluate cardiac autonomic function. Appl Physiol Nutr Metab. 2006;31:235–43.
Sicari R, Nihoyannopoulos P, Evangelista A, Kasprzak J, Lancellotti P, Poldermans D, et al. Stress echocardiography expert consensus statement: European Association of Echocardiography (EAE). Eur J Echocardiogr. 2008;9:415–37.
Campisi R, Czernin J, Schöder H, Sayre JW, Marengo FD, Phelps ME, et al. Effects of long-term smoking on myocardial blood flow, coronary vasomotion, and vasodilator capacity. Circulation. 1998;98:119–25.
Campisi R, Nathan L, Pampaloni MH, Schöder H, Sayre JW, Chaudhuri G, et al. Noninvasive assessment of coronary microcirculatory function in postmenopausal women and effects of short-term and long-term estrogen administration. Circulation. 2002;105:425–30.
Siegrist PT, Gaemperli O, Koepfli P, Schepis T, Namdar M, Valenta I, et al. Repeatability of cold pressor test-induced flow increase assessed with H(2)(15)O and PET. J Nucl Med. 2006;47:1420–6.
Biondi B, Galderisi M, Pagano L, Sidiropulos M, Pulcrano M, D’Errico A, et al. Endothelial mediated coronary flow reserve in patients with mild thyroid hormone deficiency. Eur J Endocrinol. 2009;161:323–9.
Galderisi M, Cicala S, Caso P, De Simone L, D’Errico A, Petrocelli A, et al. Coronary flow reserve and myocardial diastolic dysfunction in arterial hypertension. Am J Cardiol. 2002;90:860–4.
Hesse B, Tägil K, Cuocolo A, Anagnostopoulos C, Bardiés M, Bax J, et al. EANM/ESC procedural guidelines for myocardial perfusion imaging in nuclear cardiology. Eur J Nucl Med Mol Imaging. 2005;32:855–97.
Petretta M, Acampa W, Evangelista L, Daniele S, Ferro A, Cuocolo A. Impact of inducible ischemia by stress SPECT in cardiac risk assessment in diabetic patients: rationale and design of a prospective, multicenter trial. J Nucl Cardiol. 2008;15:100–4.
Hachamovitch R, Berman DS, Kiat H, Cohen I, Cabico A, Friedman J, et al. Exercise myocardial perfusion SPECT in patients without known coronary artery disease. Circulation. 1996;93:905–14.
Nitenberg A, Pham I, Antony I, Valensi P. Cardiovascular outcome of patients with abnormal coronary vasomotion and normal coronary arteriography is worse in type 2 diabetes mellitus than in arterial hypertension: A 10 year follow-up study. Atherosclerosis. 2005;183:113–20.
Schindler TH, Nitzasche EU, Schelbert HR, Olschewski M, Saayre J, Mix M, et al. Positron emission tomography-measured abnormal responses of myocardial blood flow to sympathetic stimulation are associated with the risk of developing cardiovascular events. J Am Coll Cardiol. 2005;45:1505–12.
Herzog BA, Husmann L, Valenta I, Gaemperli O, Siegrist PT, Tay FM, et al. Long-term prognostic value of 13N-ammonia myocardial perfusion positron emission tomography added value of coronary flow reserve. J Am Coll Cardiol. 2009;54:150–6.
Mahfouz RA, Dwidar AE, El Tahlawi MA. Endothelial-mediated coronary flow reserve and its relation to mitral annular tissue Doppler velocities in offspring of hypertensive parents. Echocardiography. 2011;28:1113–8.
Moro PJ, Flavian A, Jacquier A, Kober F, Quilici J, Gaborit B, et al. Gender differences in response to cold pressor test assessed with velocity-encoded cardiovascular magnetic resonance of the coronary sinus. J Cardiovasc Magn Reson. 2011;13:54–62.
Williams SB, Goldfine AB, Timimi FK, Ting HH, Roddy MA, Simonson DC, et al. Acute hyperglycemia attenuates endothelium-dependent vasodilation in humans in vivo. Circulation. 1998;97:1695–701.
Sobrevia L, Mann GE. Dysfunction of the endothelial nitric oxide signaling pathway in diabetes and hyperglycemia. Exp Physiol. 1997;82:423–52.
Di Carli F, Bianco-Batlles D, Landa ME, Kazmrs A, Groehn H, Muzik O, et al. Effects of autonomic neuropathy on coronary blood flow in patients with diabetes mellitus. Circulation. 1999;100:813–9.
Marini C, Bezante GP, Gandolfo P, Modonesi E, Morbelli SD, Depascale A, et al. Optimization of flow reserve measurement using SPECT technology to evaluate the determinants of coronary microvascular dysfunction in diabetes. Eur J Nucl Med Mol Imaging. 2010;37:357–67.
Djaberi R, Roodt J, Schuijf JD, Rabelink TJ, de Koning EJ, Pereira AM, et al. Endothelial dysfunction in diabetic patients with abnormal myocardial perfusion in the absence of epicardial obstructive coronary artery disease. J Nucl Med. 2009;50:1980–6.
Perrone-Filardi P, Cuocolo A, Brevetti G, Silvestro A, Storto G, Dellegrottaglie S, et al. Relation of artery flow-mediated vasodilation to significant coronary artery disease in patients with peripheral arterial disease. Am J Cardiol. 2005;96:1337–41.
Storto G, Pellegrino T, Sorrentino AR, Luongo L, Petretta M, Cuocolo A. Estimation of coronary flow reserve by sestamibi imaging in type 2 diabetic patients with normal coronary arteries. J Nucl Cardiol. 2007;14:194–9.
Pellegrino T, Storto G, Perrone-Filardi P, Sorrentino AR, Silvestro A, Petretta M, et al. Relationship between brachial artery flow-mediated dilation and coronary flow reserve in patients with peripheral artery disease. J Nucl Med. 2005;46:1997–2002.
Nabel EG, Ganz P, Gordon JB, Alexander RW, Selwyn AP. Dilation of normal and constriction of atherosclerotic coronary arteries caused by the cold pressure test. Circulation. 1988;77:43–52.
Jeserich M, Schindler TH, Olschewski M, Unmussing M, Just H, Solzbach U. Vitamin C improves endothelial function of epicardial coronary arteries in patients with hypercholesterolemia or essential hypertension – assessed by cold pressure testing. Eur Heart J. 1999;20:1676–80.
Schindler TH, Magosaki N, Jeserich M, Olschewski M, Nitzsche E, Holubarsch C, et al. Effect of ascorbic acid on endothelial dysfunction in chronic smokers assessed by cold pressure testing. Cardiology. 2000;94:239–46.
Kiviniemi TO, Toikka JO, Koskenvuo JW, Sabaste A, Saraste M, Parkka JP, et al. Vasodilation of epicardial coronary artery can be measured with transthoracic echocardiography. Ultrasound Med Biol. 2007;33:362–70.
Sudhir K, MacGregor JS, Barbant SD, Foster E, Fitzgerald PJ, Chatterjee K, et al. Assessment of coronary conductance and resistance vessel reactivity in response to nitroglycerin, ergonovine and adenosine: in vivo studies with simultaneous intravascular two-dimensional and Doppler ultrasound. J Am Coll Cardiol. 1993;21:1261–8.
Perrone-Filardi P, Achenbach S, Möhlenkamp S, Reiner Z, Sambuceti G, Schuijf JD, et al. Cardiac computed tomography and myocardial perfusion scintigraphy for risk stratification in asymptomatic individuals without known cardiovascular disease: a position statement of the Working Group on Nuclear Cardiology and Cardiac CT of the European Society of Cardiology. Eur Heart J. 2011;32:1986–93.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Marciano, C., Galderisi, M., Gargiulo, P. et al. Effects of type 2 diabetes mellitus on coronary microvascular function and myocardial perfusion in patients without obstructive coronary artery disease. Eur J Nucl Med Mol Imaging 39, 1199–1206 (2012). https://doi.org/10.1007/s00259-012-2117-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-012-2117-9