Abstract
Background
The U-shaped left ventricular (LV) contraction pattern, identified by MRI or echocardiography, is associated with improved CRT response. Gated SPECT MPI can measure both myocardial viability and mechanical dyssynchrony in a single scan. The aim of this study is to examine the relationship of the LV contraction pattern and the response of CRT in patients with left bundle branch block (LBBB).
Methods
Fifty-eight patients who met CRT guidelines and who had pre-CRT MPI were enrolled. Myocardial segments with tracer uptake < 50% of maximum were considered as scar. The LV contraction pattern was considered as U-shaped or non-U-shaped (U-shaped has a block line in the direction of contraction propagation). CRT response was defined as an increase in left ventricular ejection fraction ≥ 5% after 6-month follow-up.
Results
Twenty-eight patients (48%) had a U-shaped contraction pattern and thirty patients (52%) had a non-U-shaped contraction pattern. The U-shaped group showed a significantly higher response rate than the non-U-shaped group (90% vs. 57%; P = 0.005). By univariate and multivariate logistic regression analysis, the U-shaped pattern was an independent predictor of CRT response.
Conclusion
Non-invasive gated SPECT MPI can characterize LV mechanical contraction patterns. A U-shaped contraction pattern identified is associated with improved CRT response. This may prove useful for improved patient selection for CRT.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
CRT has been proved to be an effective treatment option for patients with drug-refractory heart failure, dilated left ventricular (LV) cavity, and electrical dyssynchrony usually demonstrated by prolonged QRS duration and LBBB morphology.1,2 Although CRT can improve the quality of life, reduce heart failure-related hospitalization and mortality, or even reverse electromechanical remodeling, 30%-40% patients fail to respond to CRT.3
Previous studies have demonstrated that different LV pacing sites or LV electrical activation patterns can induce a variety of changes of LV systolic function. Bundle branch blocks and intraventricular conduction delay may lead to the heterogeneity of LV electrical activation pattern, which may have a negative impact on LV function.2 Biventricular pacing in patients with CRT can improve LV function.4,5,6
Two types of LV electrical activation patterns have been identified by non-contact mapping (NCM) performed during electrophysiological evaluation in patients with LBBB: U-shaped pattern and non-U-shaped pattern. Compared to the non-U-shaped pattern, the U-shaped pattern (caused by a line of block in the direction of electrical activation propagation) showed a higher response rate of CRT.7,8,9 NCM is the golden standard to assess the LV electrical activation, but the relative risk and invasiveness limit its widely clinical application.7
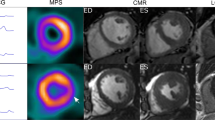
Several non-invasive myocardial imaging methods, such as three-dimensional (3D) speckle-tracking echocardiography (STE) and cardiac magnetic resonance (CMR), have been used to assess LV mechanical contraction patterns and investigate the influence of the associated electromechanical characteristics to the CRT response.8,9,10,11,12 Sohal et al. demonstrated a strong relationship between LV electrical activation sequences and mechanical contraction pattern, and reported that the U-shaped LV mechanical contraction pattern identified by CMR had an increased response rate to CRT as well.10 However, the limited availability, long examining and imaging time, and inability to scan patients with implanted devices impede the development of CMR in routine assessment of contraction patterns.13
Compared to echocardiography and CMR, ECG-gated SPECT MPI can assess both LV myocardial viability and mechanical contraction in a single scan. The phase analysis technique of gated SPECT MPI to measure LVMD is well established and has good repeatability and reproducibility.14,15 This study is aimed to apply phase analysis of SPECT MPI to identify the mechanical contraction pattern and evaluate its influence on CRT response in patients with LBBB.
Methods
Study Population
Fifty-eight patients with LBBB who met CRT guidelines were enrolled in this study at The First Affiliated Hospital of Nanjing Medical University from October 2013 to February 2016. The indication of CRT in this study included (1) sinus rhythm; (2) diminished LV systolic function (LVEF ≤ 35%); (3) typical LBBB morphology (classified as QS or rS complex in V1 and/or V2; mid QRS notching or slurring in two or more of leads: I, aVL, V5, or V6 and QRS duration ≥ 130 ms); (4) New York Heart Association (NYHA) functional class II to IV; and (5) optimized medical treatment for at least 6 months before CRT implantation.
The patients with atrial fibrillation rhythm, intraventricular conduction delay, right bundle branch block, and those being upgraded from right ventricular pacing were excluded. In order to further investigate the contraction pattern in LBBB patients with heart failure, 6 LBBB patients with normal LV function were also enrolled in the study. Gated SPECT MPI image processing and contraction pattern assessment were performed for all the enrolled patients. The study was approved by the ethics committee of The First Affiliated Hospital of Nanjing Medical University, and all patients gave written informed consent.
CRT Implantation
All the patients underwent implantation of a CRT or CRT-D. The devices were implanted by standard procedures. The right ventricular (RV) lead was systematically implanted at the RV apex or septum, and the position of the LV lead was determined by experienced electrophysiologists targeting the anterolateral, lateral, or posterolateral coronary veins. The final position was decided by coronary venous anatomic characteristics with good stability, satisfactory pacing threshold, and no phrenic nerve capture. After implantation, the LV lead position was assessed by fluoroscopic venograms in the RAO 30° and LAO 45°. LV concordance was defined as the concordance of LV lead position and latest activating segments.
Transthoracic Echocardiography
All the patients underwent standard transthoracic echocardiography by an experienced ultrasound specialist who was blinded to the study at baseline and 6-month follow-up. LVEF was recorded using the 2-dimensional modified biplane Simpson method. CRT response was defined as ≥5% improvement of LVEF at 6-month follow-up.
Gated SPECT MPI
Resting ECG-gated SPECT MPI was performed in all the enrolled patients before CRT implantation. 20-30 mCi of Tc-99m sestamibi was injected and the gated SPECT scan was performed ~60 minutes after injection. SPECT planar images were obtained using a dual-headed camera with a standard resting protocol (CardioMD, Philips Medical Systems, Milpitas, CA). The imaging parameters were set to 20% energy window around 140 keV, 180° orbit, 32 steps with 25 seconds per step, 8-bin gating, and 64 planar projections per gate. Image reconstruction and reorientation were completed using Emory Reconstruction Toolbox (ERToolbox; Atlanta, GA). SPECT images were reconstructed by ordered subset expectation maximization (OSEM) with 3 iterations and 10 subsets, and then filtered by a Butterworth low-pass filter with a cutoff frequency of 0.3 cycles/mm and an order of 10.
Myocardial Viability and Mechanical Dyssynchrony Assessed by Gated SPECT MPI
The LV sampling was completed with an automatic sampling algorithm by searching in 3D for maximal count circumferential profiles of LV.16 The percentage of tracer uptake was displayed on polar map using a 13-segmentation model, illustrated in Figure 1A. Segments with <50% maximum uptake were defined as scar. The onset of LV contraction was calculated and quantified by a phase analysis tool based on the first-harmonic Fourier approximation.14,15 The mean phase angle of each segment was displayed on the 13-segmentation polar map, as shown in Figure 1A. Phase standard deviation (PSD) and phase histogram bandwidth (PBW) from phase analysis were used to measure the global LV mechanical dyssynchrony (MD).14
Measurement of left ventricular myocardial viability and mechanical dyssynchrony from gated SPECT MPI. (A) Polar map of regional myocardial viability. The bright color represents the viable myocardium. The perfusion with less than 50% of the maximum tracer uptake was defined as scar. The number in each segment indicates the percentage of scar in this segment. (B) Polar map of regional mechanical contraction onsets. The bright color or big number represents the late contraction. The number in each segment is the mean phase angle of this segment. The phase angle was calculated by phase analysis based on the first-harmonic Fourier approximation of wall thickening to characterize the contraction onset of each myocardial sample in a cardiac cycle.14,15
Assessment of Contraction Pattern
The contraction patterns were assessed by 2 independent observers. Two types of LV mechanical contraction patterns were demonstrated in our study (Figure 2). The U-shaped contraction pattern (Figure 2A) was defined as the presence of a significant delay caused by a block line in the direction of LV contraction propagation. The non-U-shaped pattern was defined as homogenous (Figure 2B) or other heterogeneous (Figure 2C) contraction pattern.
Examples of different contraction patterns. (A) The regional contraction onsets (left) and contraction sequence (right) of an example with the U-shaped mechanical contraction pattern. The anteroseptum (blue) contracted firstly, and then the contraction propagated from the apex to the lateral wall, but it was blocked at the anterior wall, showed by yellow arrows. The anterior wall became the latest contraction site (red). (B) The regional contraction onsets (left) and contraction sequence (right) of an example with the non-U-shaped contraction pattern (homogeneous pattern). There was no apparent contraction delay in the propagation direction from the septum to lateral wall. (C) The regional contraction onsets (left) and contraction sequence (right) of an example with the other type of the non-U-shaped contraction pattern. Multiple sites with the significant contraction delays were present in this patient
Statistical Analysis
Statistical analysis was performed by SPSS version 21.0 (SPSS Inc, Chicago, IL). Categorical variables were expressed as numbers or percentages, and group comparisons were performed by the chi-square test or Fisher test. The student test was used to compare continuous variables in two groups, which were expressed as mean ± standard deviation. Then, univariate and multivariate binary logistic regression analyses evaluating odds ratios and 95% confidence intervals were used to explore the independent predictors of CRT response. The univariate factors with P < 0.05 were entered into the multivariate model. P < 0.05 was considered statistically significant.
Results
Baseline Characteristics
Table 1 shows that the characteristics of the enrolled cohort. The age of entire cohort was 61.7 ± 11.6 years and 37(64%) of them were men. The majority of patients (90%) had non-ischemic dilated cardiomyopathy. 19 (32.8%) patients were classified as NYHA II, 34 (58.6%) were NYHA III, and 5 (8.6%) were NYHA IV. The QRS duration was 171.9 ± 13.7 ms and the LVEF was 29.8 ± 6.5% at baseline.
Based on the identification by gated SPECT, 28 patients (48.3%) were classified to have a U-shaped contraction pattern, while 30 (51.7%) had a non-U-shaped pattern. Baseline QRS durations were similar between the two groups (171.4 ± 12.2 vs. 172.5 ± 15.2, respectively; P = 0.769). The PSD and PBW in the U-shaped group were greater than those in the non-U-shaped contraction (PSD: 61.3 ± 15.5 vs. 36.6 ± 21.0; PBW: 214.2 ± 64.2 vs. 118.7 ± 77.0, respectively; P < 0.0001). All the patients received optimized medical treatment and there was no statistical difference between the two groups in the use of angiotensin converting enzyme inhibitors (ACEI)/angiotensin receptor blockers (ARB), b-blockers, and aldosterone antagonists or diuretics. The number of patients with cardiovascular risk factors in each group was not statistically different at baseline. In addition, all the 6 patients with normal LV function and LBBB showed a homogenous mechanical contraction pattern (mean PSD: 18.7°, mean PBW: 48.3°).
Site Distribution of the Block Lines, Myocardial Scar, LV Leads, and Latest LV Contraction
The site distributions of block lines and myocardial scar were different. For the patients with U-shaped contraction pattern, 14 had a block line in the anterior wall, 11 in anteroseptal region, and 3 in the interior wall. The distribution of scar was as follows: 6 patients had septal scar, 2 had interior scar, 3 had apical scar, 1 had anterior scar, 1 had posterior scar, and 6 patients had scar in multiple sites. In addition, we did not find myocardial scar in 9 patients. Furthermore, in the U-shaped group, the site of block line was concordant with the scar region in only 5 (17.9%) patients.
Most of LV leads (92%) were placed in anterolateral, lateral, or posterolateral coronary veins, as determined by coronary venous anatomic characteristics. Besides, 44% of patients had the latest LV contraction in the posterior or lateral region, 29% in anterior region, and 24% in septal wall, respectively. Furthermore, the placement of LV lead was concordant with the site of latest contraction in 24 (41%) patients. The conduction velocity and contraction were slower in the peri-block regions and the site of block line was adjacent to the site of latest contraction in the U-shaped group (Figure 2a).
Outcomes of 6-Month Follow-Up
After 6-month follow-up, according to the changes of NHYA class and echocardiographic parameters in Table 2, the patients in the U-shaped group had increased CRT response. In the U-shaped group, 25 (89%) patients were considered as responders and only 3(11%) were non-responders in terms of LVEF improvement ≥5% at follow-up. The U-shaped group showed a significantly higher rate of response than the non-U-shaped group (89% vs. 57%; P = 0.005). In addition, the U-shaped group showed a significant improvement in the changes of LV diastolic diameter (11.50 ± 7.38 vs. 7.37 ± 8.07; P = 0.047), LV systolic diameter (15.2 ± 8.4 vs. 8.8 ± 8.9; P = 0.007), and LVEF(16.1 ± 9.7 vs. 9.5 ± 10.1; P = 0.014). The reduction of NYHA functional class (1.00 ± 0.67 vs. 0.77 ± 0.57; P = 0.156) in the U-shaped group tended to be greater than that in the non-U-shaped group, and NHYA functional class I was more prevalent (42.9%) in patients with the U-shaped contraction pattern.
The Prediction of CRT Response
Table 3 shows the patients classified as two groups according to CRT response; 42 patients were identified as CRT responders.
Responders had a trend toward a broader QRS duration than non-responders, but the difference did not reach statistical significance (173.2 ± 12.5 vs. 168.7 ± 16.4; P = 0.272). In responders, the LVEF (30.8 ± 6.6 vs. 26.9 ± 5.2; P = 0.037) assessed by echocardiography was greater than that in non-responders, whereas the scar burden (18.3 ± 11.3 vs. 27.1 ± 19.5; P = 0.036) derived from SPECT MPI was less in responders. The placement of LV lead was concordant with the site of latest contraction in 24 patients. Lead placement in the latest contraction location tended to increase the CRT response (54% vs 33%, P = 0.174).
In a univariate logistic regression model analysis including eight predefined parameters (Table 4), the U-shaped contraction pattern was statistically a significant independent predictor of CRT response, with an odds ratio of 6.37 (95% CI 1.57-25.80; P = 0.009). Multivariate analysis showed the same result, and the U-shaped propagation pattern was associated with high CRT response (OR: 16.01; 95%CI: 1.82 to 140.58; P = 0.012).
Discussion
The major finding of our study is that the U-shaped contraction pattern assessed by gated SPECT MPI had a significantly higher rate of CRT response.
LV Contraction Patterns and CRT Response
In this study, 28 patients (48%) were determined by gated SPECT MPI to have a U-shaped contraction pattern. The U-shaped pattern is characterized by a U-shaped propagation of mechanical contraction caused by a line of block and was seen in our study in accordance with that in previous studies.7,8,9,10,11 Auricchio et al.7 was the first to report the LV U-shaped electrical activation pattern and the block lines that existed at the anterior or lateral wall in almost all their patients (96%) with LBBB based on electrophysiological mapping. The lower prevalence of the U-shaped pattern was, however, reported also by Lambiase et al. (60%)17 and Fung et al. (65%).9 Sohal et al.10 and Jackson et al.11 used CMR to identify the U-shaped pattern in patients scheduled to implant CRT. Approximately 48% and 51% of patients were identified as having the U-shaped pattern in their studies, which is close to our study. In addition, Seo et al.8 found the U-shaped pattern in 38 of 81(47%) patients and 37(74%) of 50 patients with LBBB patients by 3D-STE. The locations of block lines were in different LV walls. Fung et al.9 and Hartlage et al.12 reported that the block lines were in the anterior, inferior, or septal wall. In our study, the lines of block were also found in various myocardial regions: 14 in anterior wall, 3 in inferior wall, and 11 in septal wall.
The previous studies showed that the U-shaped pattern correlated with good CRT response. Seo et al.8 reported the response rate was 95% for the U-shaped group using 3D-STE. The response rate reported by both Fung et al.9 and Sohal et al.10 was 80% for the U-shaped group using the LV reverse remodeling as the criteria for CRT response. In our study, most of the patients in the U-shaped group (89%) had good response from CRT. Only 3 patients were non-responders: one non-responder had good mechanical synchronicity (PSD = 29.9°). Previous studies have shown that applying CRT to patients without underlying dyssynchrony might lead to poor outcomes. A cutoff of PSD > 43° at baseline was suggested for CRT patient selection,18 and the second non-responder had extensive LV scar burden. Adelstein et al.19 demonstrated that extensive scar burden unfavorably affected clinical and LV functional outcomes after CRT and the third non-responder had discordance between the position of LV lead and the site of latest contraction. Previous studies20 have demonstrated that the placement of the LV lead in the site of latest contraction conferred the increased CRT response.
Friehling et al.21 successfully incorporated the presence of LV baseline scar burden, mechanical dyssynchrony, and the latest activation site to predict acute CRT response. Accordingly, an improved response rate to CRT may be expected when integrating LV baseline scar burden, mechanical dyssynchrony, the latest activation site, and contraction pattern into CRT patient selection.
The response rate in the non-U-shaped group of our study was 57%, higher than 11% in the 3D-STE study.8 The relatively high CRT response rate in our non-U-shaped patients might be explained by the fact that all patients had LBBB, broad QRS duration (172.50 ± 15.19 ms), and most had non-ischemic cardiomyopathy (90%). Previous study had shown that LBBB, prolonged QRS duration (QRS > 150 ms), and non-ischemic cardiomyopathy predict a favorable response to CRT.2,22
Electromechanical Coupling and Mechanical Dyssynchrony
Several reasons might explain why the U-shaped pattern can predict the favorable CRT response. Electromechanical coupling in the U-shaped pattern might be the main factor. Recently, Suever et al.23 showed a significant correlation between mechanical and electrical delay in patients undergoing CRT. In their cohort, the site of the latest electrical activation corresponded to the site of the latest mechanical contraction in 91% of patients. For the LV activation and contraction pattern, Fung et al.9 were the first to provide information about electromechanical characteristics in humans by combining echocardiographic and NCM in the same patients undergoing CRT. Sohal et al.10 identified the U-shaped pattern by CMR and NCM. Their results suggested that there was a good association of LV electromechanical parameters in the U-shaped group, and that CRT corrected the electrical dyssynchrony and synchronized mechanical contraction, which resulted in favorable electromechanical coupling and reverse remodeling in these patients. But this relationship could not be found in the non-U-shaped group or homogenous group.
Furthermore, LVMD was more severe in the U-shaped group than that in the non-U-shaped group in our cohort, which may also increase the CRT response rate. Patients with the U-shaped contraction pattern had greater PSD and PBW than those in patients with the non-U-shaped pattern. A baseline PSD and PBW (PSD > 43° and PBW > 135°) derived from SPECT were useful for the prediction of response to CRT.18
The Potential Formation Mechanism of the U-Shaped Pattern
In patients with LBBB, electrical activation propagates from the RV to the LV through the interventricular septum. In LV, the first activation site is the septum and subsequently the electrical activation of the lateral wall.6 Previous studies had showed that the U-shaped pattern could be identified in patients with heart failure and LBBB.5,6,7,8,9 LBBB may be related to the U-shaped pattern.
However, Sohal et al.10 enrolled patients with heart failure and prolonged QRS duration (≥120 ms) and demonstrated that about half of their patients had the U-shaped contraction pattern. Besides, Seo et al.8 also identified the U-shaped pattern by 3D-STE in patients without LBBB. In our study, 28 patients with LBBB and heart failure were identified as the U-shaped pattern, but all the 6 patients with LBBB and normal LV function were identified as having homogenous activation pattern. Therefore, we speculate that the cause of the U-shaped contraction pattern was related to heart failure and dilated LV.
We believe that the cause of the U-shaped pattern in patients with LBBB may be explained as followed: firstly, RV is activated and contracts prior to the LV in patients with LBBB, resulting in LV contraction pattern that spreads from the septum to lateral wall. Such pattern may exclude the interventricular septum from supporting LV function, which leads to the loss of coordinated global LV systolic function. The uncoordinated LV systolic motion leads to a decrease of LVEF and myocardial efficiency. Lastly, the LV begins to enlarge and remodel. Dilated LV made the myocardial wall thinner, mechanical motion deformed, the electrical conductivity and mechanical contraction slower, and the appearance of the functional block lines. Therefore, dilated LV and heart failure may have a dominant role in the formation of the U-shaped pattern.
Furthermore, Auricchio et al.7 previously substantiated that the nature of block lines was functional by the facts that most of their patients had idiopathic cardiomyopathy and myocardial scar was also excluded by non-contact mapping. In addition, the line of block disappeared or the location was changed when asynchronous pacing was applied, which strongly supported a functional basis. In our study, the site of block line was concordant with the scar region in only 5 (18%) patients. However, all these 5 patients had non-ischemic dilated cardiomyopathy. Therefore, the nature of the block line may be functional in our study as well.
Clinical Application of Gated SPECT MPI to Assess LV Contraction Patterns
Our results confirmed and extended previous findings regarding contraction patterns by echocardiography and CMR.8,9,10,11 We used gated SPECT MPI which has unique advantages because it is widely clinically used, has high cost-effectiveness and reproducibility, and can assess both myocardial viability and mechanical dyssynchrony in a single scan. The univariate and multivariate logistic regression showed that the U-shaped pattern was an independent predictor of CRT response. Thereafter, our method has great promise for clinical use for CRT patient selection.
Limitation
In this study, apart from LVMD measured by gated SPECT MPI, no LV electrical activation parameters were collected. The LV concordance was defined as the LV lead position in the latest activating segment, while myocardial viability of the target segment was not considered. After CRT implantation, the LV lead position was assessed by dual-view fluoroscopy. This study had a relative small sample size and short follow-up period performed at a single center. The U-shaped pattern to predict CRT response must be assessed in the large randomized multicenter prospective studies.
New Knowledge Gained
This is the first study of assessing LV contraction pattern using gated SPECT MPI and evaluating its influence to the CRT response in patients with LBBB. Our study demonstrates that the U-shaped contraction pattern leads to a significantly higher rate of response than the non-U-shaped pattern.
Conclusion
The non-invasive gated SPECT MPI can identify LV mechanical contraction patterns. The U-shaped contraction pattern assessed by MPI is significantly associated with favorable response of CRT. Assessment of LV mechanical contraction patterns may provide incremental value to improve patient selection and predict the response of CRT.
Abbreviations
- SPECT:
-
Single-photon emission computed tomography
- MPI:
-
Myocardial perfusion imaging/images
- LV:
-
Left ventricle/ventricular
- CRT:
-
Cardiac resynchronization therapy
- LBBB:
-
Left bundle branch block
- LVMD:
-
Left ventricular mechanical dyssynchrony
- PSD:
-
Phase standard deviation
- PBW:
-
Phase histogram bandwidth
References
Abraham WT, Fisher WG, Smith AL, Delurgio DB, Leon AR, Loh E, et al. Cardiac resynchronization in chronic heart failure. N Engl J Med. 2002;346:1845–53.
Peterson PN, Greiner MA, Qualls LG, Al-Khatib SM, Curtis JP, Fonarow GC, et al. QRS duration, bundle-branch block morphology, and outcomes among older patients with heart failure receiving cardiac resynchronization therapy. JAMA. 2013;310(6):617–26.
Auricchio A, Prinzen FW. Non-responders to cardiac resynchronization therapy: the magnitude of the problem and the issues. Circ J. 2011;75:521–7.
Butter C, Auricchio A, Stellbrink C, Fleck E, Ding J, Yu Y, et al. Effect of resynchronization therapy stimulation site on the systolic function of heart failure patients. Circulation. 2001;104:3026–9.
Fung JW, Yu CM, Yip G, Zhang Y, Chan H, Kum CC, et al. Variable left ventricular activation pattern in patients with heart failure and left bundle branch block. Heart. 2004;90:17–9.
Seo Y, Ishizu T, Sakamaki F, Yamamoto M, Aonuma K. Left bundle branch block and echocardiography in the era of CRT. J Echocardiogr. 2015;13:6–14.
Auricchio A, Fantoni C, Regoli F, Carbucicchio C, Goette A, Geller C, et al. Characterization of left ventricular activation in patients with heart failure and left bundle-branch block. Circulation. 2004;109:1133–9.
Seo Y, Ishizu T, Kawamura R, Yamamoto M, Kuroki K, Igarashi M, et al. Three-dimensional propagation imaging of left ventricular activation by speckle-tracking echocardiography to predict responses to cardiac resynchronization therapy. J Am Soc Echocardiogr. 2015;28:606–14.
Fung JW, Chan JY, Yip GW, Chan HC, Chan WW, Zhang Q, et al. Effect of left ventricular endocardial activation pattern on echocardiographic and clinical response to cardiac resynchronization therapy. Heart. 2007;93:432–7.
Sohal M, Shetty A, Duckett S, Chen Z, Sammut E, Amraoui S, et al. Noninvasive assessment of LV contraction patterns using CMR to identify responders to CRT. JACC Cardiovasc Imaging. 2013;6:864–73.
Jackson T, Sohal M, Chen Z, Child N, Sammut E, Behar J, et al. A U-shaped type II contraction pattern in patients with strict left bundle branch block predicts super-response to cardiac resynchronization therapy. Heart Rhythm. 2014;11:1790–7.
Hartlage GR, Suever JD, Clement-Guinaudeau S, Strickland PT, Ghasemzadef N, Magrath RP, et al. Prediction of response to cardiac resynchronization therapy using left ventricular pacing lead position and cardiovascular magnetic resonance derived wall motion patterns: a prospective cohort study. J Cardiovasc Magn Reson. 2015;17:57.
Lardo AC, Abraham TP, Kass DA. Magnetic resonance imaging assessment of ventricular dyssynchrony: current and emerging concepts. J Am Coll Cardiol. 2005;46(12):2223–8.
Chen J, Garcia EV, Folks RD, Cooke CD, Faber TL, Tauxe EL, et al. Onset of left ventricular mechanical contraction as determined by phase analysis of ECG-gated myocardial perfusion SPECT imaging: development of a diagnostic tool for assessment of cardiac mechanical dyssynchrony. J Nucl Cardiol. 2005;12(6):687–95.
Zhou W, Garcia EV. Nuclear image-guided approaches for cardiac resynchronization therapy (CRT). Curr Cardiol Rep. 2016;18(1):7.
Garcia EV, Cooke CD, Van Train KF, Folks R, Peifer J, DePuey EG, et al. Technical aspects of myocardial SPECT imaging with technetium-99m sestamibi. Am J Cardiol. 1990;66(13):23E–31E.
Lambiase PD, Rinaldi A, Hauck J, Mobb M, Elliott D, Mohammad S, et al. Non-contact left ventricular endocardial mapping in cardiac resynchronisation therapy. Heart. 2004;90:44–51.
Henneman MM, Chen J, Dibbets-Schneider P, Stokkel MP, Bleeker GB, Ypenburg C, et al. Can LV dyssynchrony as assessed with phase analysis on gated myocardial perfusion SPECT predict response to CRT? J Nucl Med. 2007;48:1104–11.
Adelstein EC, Saba S. Scar burden by myocardial perfusion imaging predicts echocardiographic response to cardiac resynchronization therapy in ischemic cardiomyopathy. Am Heart J. 2007;153:105–12.
Khan FZ, Virdee MS, Palmer CR, Pugh PJ, O’Halloran D, Elsik M, et al. Targeted left ventricular lead placement to guide cardiac resynchronization therapy: the TARGET study: a randomized, controlled trial. J Am Coll Cardiol. 2012;59:1509–18.
Friehling M, Chen J, Saba S, Bazaz R, Schwartzman D, Adelstein EC, et al. A prospective pilot study to evaluate the relationship between acute change in left ventricular synchrony after cardiac resynchronization therapy and patient outcome using a single-injection gated SPECT protocol. Circ Cardiovasc Imaging. 2011;4(5):532–9.
Marsan NA, Bleeker GB, van Bommel RJ, Ypenburg C, Delgado V, Borleffs CJ, et al. Comparison of time course of response to cardiac resynchronization therapy in patients with ischemic versus nonischemic cardiomyopathy. Am J Cardiol. 2009;103(5):690–4.
Suever JD, Hartlage GR, Magrath RP, Iravanian S, Lloyd MS, Oshinski JN. Relationship between mechanical dyssynchrony and intra-operative electrical delay times in patients undergoing cardiac resynchronization therapy. J Cardiovasc Magn Reson. 2014;16:4.
Acknowledgements
This research was supported by a grant from Science and Technology Department of Jiangsu Province (Project Number: BE2016764, PI: Jiangang Zou) and a New Faculty startup grant from the University of Southern Mississippi (Project Number: DE01791, PI: Weihua Zhou).
Disclosure
The authors have declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding authors
Additional information
The authors of this article have provided a PowerPoint file, available for download at SpringerLink, which summarises the contents of the paper and is free for re-use at meetings and presentations. Search for the article DOI on SpringerLink.com.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Tao, N., Qiu, Y., Tang, H. et al. Assessment of left ventricular contraction patterns using gated SPECT MPI to predict cardiac resynchronization therapy response. J. Nucl. Cardiol. 25, 2029–2038 (2018). https://doi.org/10.1007/s12350-017-0949-1
Received:
Revised:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-017-0949-1