Abstract
Background
Patients requiring vasodilator single-photon emission computed-tomography myocardial perfusion imaging (SPECT-MPI) have a higher mortality risk than those selected for exercise or vasodilator with low-level exercise SPECT-MPI. However, it is unknown whether the increased mortality is driven by cardiac deaths alone or cardiac and non-cardiac deaths.
Methods
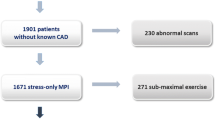
In a prospective cohort of 1,511 consecutive patients referred for SPECT-MPI, patients were classified according to stress test modality: exercise, adenosine with low-level exercise (AdenoEx), and adenosine. Subjects were followed for events of all-cause mortality and cause of death. Survival analyses using multivariate Cox regression and propensity score matching methods were performed.
Results
During a follow-up of 4.9 ± 0.9 years, a total of 68 (4.5%) deaths occurred: 50 non-cardiac and 18 cardiac. The adenosine group had the highest annual mortality (all-cause 3.65%, non-cardiac 2.36%, cardiac 1.29%), while exercise stress had the lowest mortality (all-cause 0.42%, non-cardiac 0.37%, cardiac 0.05%) and AdenoEx had an intermediate mortality (all-cause 1.3%, non-cardiac 0.91%, cardiac 0.39%); all P values <0.001. The majority of non-cardiac deaths were attributed to cancer. Using exercise stress as a reference standard, multivariable Cox regression analyses demonstrated that adenosine stress was independently predictive of all-cause mortality [HR 3.23 (CI 1.77-5.88); P < 0.001], non-cardiac death [HR 2.67 (CI 1.34-5.31); P = 0.005], and cardiac death [HR 6.30 (CI 1.55-25.56); P = 0.010] after adjusting for univariate predictors of mortality. These findings were consistent in the subgroups of patients with normal and abnormal MPI. AdenoEx was predictive of all-cause, non-cardiac, and cardiac deaths in univariate analysis, but it was not predictive by multivariate analysis. Propensity score matched cohort analysis showed that the adenosine stress group had the highest all-cause (P < 0.001), non-cardiac (P = 0.013), and cardiac deaths (P < 0.001), while the exercise stress group had the lowest mortality of any cause.
Conclusions
The inability to perform any level of exercise during a SPECT-MPI stress is associated with high mortality risk, which is derived from both cardiac and non-cardiac deaths.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Over the past decades, there has been a steady increase in the proportion of patients undergoing vasodilator stress myocardial perfusion imaging (MPI) with single-photon emission computed-tomography (SPECT), while the rate of those undergoing symptom-limited exercise SPECT-MPI has been declining.1 This trend is likely the result of aging and the increasing prevalence of obesity in the population with resultant higher cardiac and non-cardiac comorbidities. Existing data indicate that patients who require a vasodilator stress test have a worse prognosis compared to those who can exercise, even in the context of a normal study.2-5 Recently, it has been established that among patients who undergo SPECT-MPI, mortality is highest for the ones selected for adenosine stress, intermediate for those able to perform low-level exercise with vasodilator stress, and lowest with exercise stress.6,7 However, it remains unknown whether the observed differential mortality is driven by cardiac deaths alone or by non-cardiac deaths as well. It is plausible that exercise-limiting cardiac and non-cardiac comorbidities contribute to non-cardiac deaths. In this investigation, we sought to determine the impact of stress modality on non-cardiac and cardiac mortality in patients undergoing SPECT-MPI.
Design and Methods
This is a substudy with extended follow-up of a prospective cohort of 1,511 consecutive patients referred for outpatient, clinically-indicated SPECT-MPI between August 15, 2007 and May 15, 2010. The study was approved by the institutional review board of Rush University Medical Center. An initial report detailing the methodology of the cohort formation was published elsewhere.8 Baseline demographics, risk factors, cardiovascular history, and medications were prospectively tabulated. Chest pain syndromes were classified as typical angina, atypical angina, and non-anginal on the basis of pain location, relation to exercise, and resolution with rest or nitroglycerin.9 Dyspnea was considered non-anginal chest pain. The pretest probability of obstructive coronary artery disease (CAD) was determined according to Diamond and Forrester tables on the basis of age, gender, and chest pain type.9
Stress and Myocardial Perfusion Imaging Protocols
All subjects underwent a one-day, rest/stress, 99mTc-sestamibi protocol conforming with the American Society of Nuclear Cardiology guidelines.10 Patients were instructed to fast for at least 8 hours and to abstain from caffeinated products for 24 hours prior to the test. As clinically appropriate, patients underwent one of the following stress modalities: exercise Bruce protocol, adenosine infusion with low-level exercise (AdenoEx), or standard 6-minute adenosine infusion.11,12 Patients with left bundle branch-block or ventricular pacemaker received a standard 6-minute adenosine stress, irrespective of their ability to exercise.10 Based on the stress modality implemented, patients were divided into three groups: (1) exercise; (2) AdenoEx; and (3) adenosine. All MPI scans were acquired using an upright acquisition, dual-head, dedicated cardiac SPECT camera without attenuation correction. Using QPS/QGS software (Cedars-Sinai Cardiac Suite; Los Angeles, CA), MPI scans were semiquantitatively interpreted by a blinded, single expert nuclear cardiologist using a 17-segment model, deriving summed stress scores (SSS), summed rest scores, and summed difference scores (SDS). Myocardial perfusion was categorized as normal (SSS ≤ 3), mildly abnormal (SSS 4-8), and moderately or severely abnormal (SSS ≥ 9).3,8 A normal study was defined as one with normal myocardial perfusion (SSS ≤ 3) and normal post-stress gated-SPECT left ventricular ejection fraction (EF ≥ 50%). Known CAD was defined as a composite of prior myocardial infarction (MI), prior percutaneous coronary intervention, or prior coronary artery bypass grafting surgery. A random sample of 151 scans (10%) was independently interpreted by two blinded, board-certified nuclear cardiologists. Excellent inter-rater interpretation agreement between the main reader and the two control readers was established, as published elsewhere.8
Outcome Determination
Subjects were prospectively followed for events of all-cause mortality as determined by a review of medical records and a Social Security Death Index search conducted in March 2014. Patients not found to be deceased at the time of the search were considered to be alive. Cause of death was ascertained by review of the death certificate obtained from the Illinois Department of Health and Human Services. The primary cause of death was determined by a consensus of three adjudicators reviewing the diagnoses listed on each death certificate. Outcome assessors were blinded to clinical history, stress modality, and MPI findings. Cardiac death was defined as resulting from MI, sudden cardiac death, heart failure, or lethal arrhythmia. All other causes of death, including stroke and pulmonary embolism, were considered non-cardiac. A death was also considered cardiac if MI was listed as a contributing cause of death (such as an MI in the setting of multisystem organ failure). The primary endpoint was non-cardiac death. The secondary endpoint was cardiac death.
Statistical Analysis
The chi-square test was used to compare dichotomous variables, which were expressed as a number (percentage). Between groups, comparisons of continuous variables were performed using one-way analysis of variance (ANOVA) method. The Bonferroni correction was applied for multiple comparisons of continuous variables. Univariate Cox proportional-hazards models were used to determine univariate predictors of non-cardiac and cardiac deaths. Multivariate Cox proportional-hazards models were used to compare event-free survival between different stress modality groups, adjusting for univariate predictors of non-cardiac and cardiac death. Hazard ratios (HR) of death with AdenoEx and adenosine stress modality with 95% confidence interval (CI) were reported in reference to the exercise modality group. Proportionality of hazards assumption was confirmed by demonstrating parallel “log minus log” survival plots. Sensitivity analyses using multivariate Cox proportional-hazards models were performed assuming that all patients with unknown cause of death died from a cardiac etiology rather than a non-cardiac cause.
To account for inherent differences in baseline clinical and imaging characteristics between the study groups, we performed secondary survival analyses using propensity score matching methodology. A multivariate logistic regression model for all-cause mortality was fit to generate standardized propensity scores accounting for baseline characteristics (Table 1) found to be statistically different between any two study groups (P < .05). The generated propensity scores were matched to the closest value in a 3:1:1 ratio (3, exercise; 1, AdenoEx; 1, adenosine) using a matching algorithm written in the Python programming language version 2.6.7 (Python Software Foundation, Python.org) and the NumPy scientific package (numpy.org). Kaplan-Meier curves and the log-rank test were used to compare event-free survival between propensity score matched stress modality groups. Two-tailed P values <.05 were considered significant. The PASW 18.0 software (SPSS, Inc., Chicago, IL) was used for all statistical analyses.
Handling of Missing Data
Patients with missing death certificates were considered to have died from a non-cardiac cause, as this was the most common mode of death in the cohort.8 To ensure that such an assumption did not alter the conclusions of the study, we performed sensitivity analyses using multivariate Cox proportional-hazards models in which we assumed that all patients with unknown cause of death died from a cardiac etiology rather than a non-cardiac cause.
Results
Among the 1,511 subjects, 56.5% were men. The mean age was 59 ± 13 years. A total of 1,164 patients (77%) underwent exercise, 157 (10%) AdenoEx, and 190 (13%) adenosine stress. Detailed baseline characteristics of all three stress modality groups are outlined in Table 1. Notably, patients in the exercise group were younger, predominantly men, and had a lower prevalence of hypertension, diabetes mellitus, and known CAD. Furthermore, patients in the exercise stress group were less likely to have an abnormal perfusion study or left ventricular systolic dysfunction (Table 1). There was no difference in the prevalence of ischemic equivalent symptoms (chest pain or dyspnea) as an indication for testing. Patients in the adenosine and AdenoEx groups had significantly higher mean likelihood of obstructive CAD (Table 1). During 4.9 ± 0.9 years follow-up, a total of 68 (4.5%) deaths were observed: 50 (3.3%) non-cardiac and 18 (1.2%) cardiac. As shown in Table 2, the adenosine group had the highest rates of all-cause, non-cardiac, and cardiac deaths. The mortality rate was lowest in the exercise stress group and intermediate in the AdenoEx group. The majority of non-cardiac deaths were attributed to cancer. The most notable causes of death in each study group are outlined in Table 2.
As shown in Table 3, univariate predictors for both non-cardiac and cardiac death were age, known CAD, abnormal MPI (SSS ≥ 4), EF, and stress modality; these were selected for multivariate analysis. Although myocardial ischemia was a univariate predictor of cardiac death, it was not included in multivariate analysis since it is largely encompassed in the abnormal MPI variable.
Multivariable Cox regression analyses, adjusting for univariate predictors of non-cardiac and cardiac deaths, demonstrated that adenosine stress was independently predictive of all-cause mortality [HR 3.23 (CI 1.77-5.88); P < .001], whereas AdenoEx was not (P = .313), as shown in Figure 1A. In this model, age [HR 1.07 per year (CI 1.04-1.09); P < .001], EF [HR 0.74 per 10-point increment (CI 0.62-0.89); P = .002], and known CAD [HR 2.08 (CI 1.25-3.47); P = .005] were independently predictive of all-cause mortality, while abnormal MPI (SSS ≥ 4) was not (P = .576). Similarly, after adjusting for predictors of non-cardiac death, multivariate Cox regression analysis indicated that adenosine stress was independently predictive of non-cardiac death [HR 2.67 (CI 1.34-5.31); P = .005], while AdenoEx was not (P = .590), as shown in Figure 1B. Other independent predictors of non-cardiac death were age, EF, and known CAD, whereas abnormal myocardial perfusion was not predictive (Table 3). Likewise, multivariate Cox regression analysis, after adjusting for predictors of cardiac death, determined that adenosine stress was an independent predictor of cardiac death [HR 6.30 (CI 1.55-25.56); P = .010] while AdenoEx was not (P = .207), as illustrated in Figure 1C. Age was independently predictive of cardiac mortality, whereas EF, known CAD, and abnormal perfusion were not (Table 3). In the above three models, substituting SSS as a continuous variable for abnormal MPI (SSS ≥ 4) yielded similar results, with SSS not being independently predictive of death of any cause (P values > .28).
Mortality according to stress modality. The graphs depict Cox proportional-hazards survival plots for all-cause mortality (A), non-cardiac death (B), and cardiac death (C). Hazard ratios and confidence intervals were adjusted for significant clinical and imaging covariates: age, known coronary artery disease, abnormal myocardial perfusion imaging (SSS ≥ 4), and ejection fraction. AdenoEx, adenosine with low-level exercise; HR, hazard ratio; CI, 95% confidence interval
Patients with Normal MPI Study
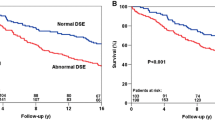
As illustrated in Figure 2, Cox regression analyses among patients who had a normal study (SSS ≤ 3 and normal EF) showed that adenosine stress modality was predictive of all-cause mortality [HR 7.59 (CI 3.82-15.09); P < .001], non-cardiac death [HR 5.49 (CI 2.53-11.90); P < .001], and cardiac death [HR 41.41 (CI 4.84-354.49); P = .001], whereas AdenoEx was not predictive of mortality (non-cardiac or cardiac).
Mortality according to stress modality among patients with normal myocardial perfusion imaging and normal post-stress ejection fraction. The graphs depict Cox proportional-hazards survival plots for all-cause mortality (A), non-cardiac death (B), and cardiac death (C). AdenoEx, adenosine with low-level exercise; HR, hazard ratio; CI, 95% confidence interval
Patients with Abnormal MPI Study
As illustrated in Figure 3, Cox regression analyses among patients who had an abnormal study (SSS ≥ 4 or EF < 50%) showed that adenosine stress modality was predictive of all-cause mortality [HR 5.18 (CI 2.16-12.43); P < .001], non-cardiac death [HR 4.36 (CI 1.50-12.62); P = .007], and cardiac death [HR 7.23 (CI 1.50-34.82); P = .014], while AdenoEx was not predictive of mortality of any cause.
Mortality according to stress modality among patients with abnormal myocardial perfusion imaging or abnormal post-stress ejection fraction. The graphs depict Cox proportional-hazards survival plots for all-cause mortality (A), non-cardiac death (B), and cardiac death (C). AdenoEx, adenosine with low-level exercise; HR, hazard ratio; CI, 95% confidence interval
Sensitivity Analyses
Assuming that all 8 subjects with unknown cause of death had died from a cardiac cause, multivariate Cox regression models showed that adenosine stress modality remained independently predictive of non-cardiac and cardiac deaths (P values = .029 and <.001, respectively), whereas AdenoEx stress modality was not (P values >.05).
Propensity Score Matching Analysis
A total of 775 patients were propensity score matched in a 3:1:1 ratio (465, exercise; 155, AdenoEx; 155, Adenosine). There was no significant difference in the mean propensity score between all three stress modality groups (P = .24), indicating that the groups were well matched. In the propensity score matched cohort, Kaplan-Meier survival analyses demonstrated that adenosine stress was associated with the highest all-cause mortality (P < .001), non-cardiac death (P = .013), and cardiac death (P < .001), whereas exercise stress was associated with the lowest mortality from any cause (Figure 4).
Survival according to stress modality in a propensity score matched cohort. The graphs depict Kaplan-Meier survival curves and log-rank test P values for all-cause mortality (A), non-cardiac death (B), and cardiac death (C). Propensity scores were weighted to statistically significant differences in baseline characteristics listed in Table 1. AdenoEx, adenosine with low-level exercise
Discussion
In this prospective cohort study of ambulatory patients undergoing SPECT-MPI, we confirmed that subjects who were unable to perform any level of exercise, thereby requiring the use of standard adenosine stress modality, had the highest mortality as compared to those who underwent exercise or AdenoEx stress protocols. These findings were consistent in patients with normal and abnormal MPI studies. In addition, we demonstrated that the high mortality associated with adenosine stress was derived not only from an increased rate of cardiac deaths, as previously established, but also from an increase in non-cardiac deaths. These findings were independent from clinical and imaging predictors of mortality.
In a recent study, Nair et al6 investigated the incidence of cardiac death and non-fatal MI in 19,367 consecutive patients undergoing SPECT-MPI. The authors demonstrated similar results to the present study with regards to adenosine being an independent predictor of cardiac death. They also established that AdenoEx protocol is independently associated with higher rates of cardiac and non-cardiac deaths compared to exercise stress, but is associated with lower mortality than adenosine stress. Similarly, Thomas et al5 studied the prognostic value of SPECT-MPI in an outpatient setting and demonstrated that patients who underwent AdenoEx protocol had an intermediate event rate of cardiac death or MI, higher than exercise stress but lower than adenosine stress protocol. However, neither of these studies investigated the impact of stress modality on non-cardiac deaths. Moreover, Johnson et al7 retrospectively followed 3,479 patients with normal SPECT-MPI for 4.3 ± 1.0 years for all-cause mortality according to stress modality. These investigators demonstrated that patients who received an adenosine stress test had the highest mortality, followed by the ones selected for AdenoEx, while those who had an exercise stress test had the lowest mortality. Nonetheless, the study did not investigate the cause of death. Finally, Rozanski et al13 studied 6,069 patients without known CAD who underwent either adenosine or exercise SPECT-MPI and followed them for 10.2 years for all-cause mortality. Using propensity score matching, these authors demonstrated that patients who underwent adenosine stress had higher all-cause mortality than those who exercised. Nonetheless, the study did not look into the cause of death.
In our investigation, patients in the AdenoEx group had an intermediate survival between the exercise and adenosine groups, in agreement with previous reports.5,7 Although AdenoEx was predictive of non-cardiac and cardiac deaths in univariate analysis, it was not predictive in multivariate analysis after adjusting for clinical and imaging covariates. However, we observed a consistent, yet not statistically significant trend toward higher mortality as compared to exercise stress. This apparent deviation from previous reports6,7 is likely due to “type II error” in our investigation as the AdenoEx group was limited by a small sample size and a relatively low-risk population. Indeed, these were ambulatory, low-risk patients, primarily referred by primary care physicians for office-based testing.8,14 We observed an annualized cardiac mortality of 0.24%, which appears to be lower than noted in previous reports (0.8%).15
We demonstrated that patients who are selected for adenosine stress test have higher non-cardiac mortality than those who can perform any level of exercise. This is likely due to the fact that these patients are older and have multiple exercise-limiting non-cardiac comorbidities; thus, they are likely to die from these diseases or their related complications. Notably, the majority of the deaths observed were attributed to non-cardiac causes for all three stress modalities, with cancer being the leading cause of non-cardiac death. We speculate that some of these stress tests were ordered as part of a pre-mortality cluster of testing to investigate symptoms related to cancer or other terminal illnesses.
Despite being a univariate predictor of cardiac and non-cardiac mortality, abnormal MPI (SSS ≥ 4) was not independently predictive of mortality in multivariate analyses. This observation may be caused by collinearity between pharmacologic stress modality and perfusion imaging, such that patients who underwent pharmacologic stress are the ones with the most abnormal MPI (given their higher baseline risk). This collinearity could have negated the predictive value of perfusion imaging in multivariate analyses. Additionally, this observation may be due to “over-fitting” of the multivariate Cox regression models, particularly the cardiac death model, leading to type II error.
Limitations
The Social Security Death Index may have underestimated mortality due to delay in reporting and the cause of death listed on the death certificate could have been inaccurate in some cases. Furthermore, despite adjusting for significant covariates, we cannot entirely exclude the possibility of the results being biased by unidentified confounders. To address this matter, we analyzed a propensity score matched cohort accounting for a wide array of significant confounders. The fact that multivariate Cox regression analyses and propensity score matching have yielded similar findings strengthens the study’s conclusion. Another limitation is that the study is underpowered to assess the impact of AdenoEx stress modality on outcome. Finally, given the limited mortality events observed, particularly cardiac death, multivariate Cox regression models (Figure 1; Table 3) were probably over-fitted, introducing a possible type II error and wide confidence intervals.
New Knowledge Gained
We demonstrated that the higher mortality associated with adenosine stress is not only due to higher cardiac mortality, but also from an excess of non-cardiac deaths.
Conclusion
This study confirms that inability to perform any level of exercise during SPECT-MPI stress is associated with high mortality risk due to an increase in both non-cardiac and cardiac deaths.
References
AMR/Arlington Medical Resources Inc. Myocardial Perfusion Monthly Monitor, November, 2012
Shaw LJ, Hendel R, Borges-Neto S, Lauer MS, Alazraki N, Burnette J, et al. Prognostic value of normal exercise and adenosine (99m)Tc-tetrofosmin SPECT imaging: results from the multicenter registry of 4,728 patients. J Nucl Med 2003;44:134-9.
Hachamovitch R, Berman DS, Shaw LJ, Kiat H, Cohen I, Cabico JA, et al. Incremental prognostic value of myocardial perfusion single photon emission computed tomography for the prediction of cardiac death: differential stratification for risk of cardiac death and myocardial infarction. Circulation 1998;97:535-43.
Hachamovitch R, Hayes S, Friedman JD, Cohen I, Shaw LJ, Germano G, et al. Determinants of risk and its temporal variation in patients with normal stress myocardial perfusion scans: What is the warranty period of a normal scan? J Am Coll Cardiol 2003;41:1329-40.
Thomas GS, Miyamoto MI. Should simultaneous exercise become the standard for adenosine myocardial perfusion imaging? Am J Cardiol 2004;94:3D-10D discussion D-1D.
Nair SU, Ahlberg AW, Katten DM, Heller GV. Does risk for major adverse cardiac events in patients undergoing vasodilator stress with adjunctive exercise differ from patients undergoing either standard exercise or vasodilator stress with myocardial perfusion imaging? J Nucl Cardiol 2014
Johnson NP, Schimmel DR Jr, Dyer SP, Leonard SM, Holly TA. Survival by stress modality in patients with a normal myocardial perfusion study. Am J Cardiol 2011;107:986-9.
Doukky R, Hayes K, Frogge N, Balakrishnan G, Dontaraju VS, Rangel MO, et al. the impact of appropriate use on the prognostic value of SPECT myocardial perfusion imaging. Circulation 2013;128:1634-43.
Diamond GA, Forrester JS. Analysis of probability as an aid in the clinical diagnosis of coronary-artery disease. N Engl J Med 1979;300:1350-8.
Henzlova MJ, Cerqueira MD, Mahmarian JJ, Yao SS. Stress protocols and tracers. J Nucl Cardiol 2006;13:e80-90.
Doukky R. Pharmacologic stress testing in myocardial perfusion imaging: Technical applications. In: Mann A, Heller GV, Hendel RC, editors. Nuclear cardiology: Technical applications. New York: McGraw-Hill; 2007. p. 107-24.
Elliott MD, Holly TA, Leonard SM, Hendel RC. Impact of an abbreviated adenosine protocol incorporating adjunctive treadmill exercise on adverse effects and image quality in patients undergoing stress myocardial perfusion imaging. J Nucl Cardiol 2000;7:584-9.
Rozanski A, Gransar H, Hayes SW, Friedman JD, Hachamovitch R, Berman DS. Comparison of long-term mortality risk following normal exercise vs adenosine myocardial perfusion SPECT. J Nucl Cardiol 2010;17:999–1008.
Doukky R, Frogge N, Balakrishnan G, Hayes K, Collado FM, Rangel MO, et al. The prognostic value of cardiac SPECT performed at the primary care physician’s office. J Nucl Cardiol 2013;20:519-28.
Groutars RG, Verzijlbergen JF, Muller AJ, Ascoop CA, Tiel-van Buul MM, Zwinderman AH, et al. Prognostic value and quality of life in patients with normal rest thallium-201/stress technetium 99m-tetrofosmin dual-isotope myocardial SPECT. J Nucl Cardiol 2000;7:333-41.
Hendel RC, Berman DS, Di Carli MF, Heidenreich PA, Henkin RE, Pellikka PA, et al. ACCF/ASNC/ACR/AHA/ASE/SCCT/SCMR/SNM 2009 appropriate use criteria for cardiac radionuclide imaging: A report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the American Society of Nuclear Cardiology, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the Society of Cardiovascular Computed Tomography, the Society for Cardiovascular Magnetic Resonance, and the Society of Nuclear Medicine. J Am Coll Cardiol 2009;53:2201-29.
Acknowledgment
The authors sincerely thank Guillaume Lambert for his contribution to the group matching process for the propensity score matched analysis.
Disclosure
Rami Doukky has served on the Advisory Board of Astellas Pharma, USA, and received investigator initiated research grant support from Astellas Pharma, USA. Other authors have no conflicts to disclose.
Author information
Authors and Affiliations
Corresponding author
Additional information
See related editorial, doi:10.1007/s12350-015-0103-x.
Funding
The original study leading to the formation of the study cohort was funded by an investigator-initiated Grant from Astellas Pharma US (Northbrook, IL). Grant fiduciary: Rush University Medical Center. Principal Investigator: Rami Doukky, MD. The funding source had no input in the study design, execution, data analysis and interpretation, or manuscript preparation and approval.
Rights and permissions
About this article
Cite this article
Poulin, MF., Alexander, S. & Doukky, R. Prognostic implications of stress modality on mortality risk and cause of death in patients undergoing office-based SPECT myocardial perfusion imaging. J. Nucl. Cardiol. 23, 202–211 (2016). https://doi.org/10.1007/s12350-014-0064-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-014-0064-5