Abstract
Background
A novel ultra-fast solid-state cardiac camera (Discovery NM 530c, General Electric) allows much shorter acquisition times compared to standard dual-detector SPECT cameras. This design enables investigation of the potential for early myocardial perfusion imaging (MPI) following a rest injection of technetium-99m (Tc-99m) rather than the conventional 45-60 minute delay in image acquisition.
Methods
A total of 30 patients underwent MPI at rest using Tc-99m sestamibi (n = 9) or tetrofosmin (n = 21). A 12 minute image acquisition in list mode was performed immediately following isotope injection. Patients also underwent a conventional delayed image acquisition 60 minutes following the rest isotope injection (image acquisition over 4 minutes). The immediate 12 minute acquisition was divided into three 4-minute intervals for image reconstruction (0-4, 4-8, and 8-12 minutes). The perfusion images were interpreted by two experienced physicians who evaluated each study for overall image quality (good, acceptable, or unacceptable) and graded each image using the summed rest score (SRS) and the standard 17-segment, 5-point scale model.
Results
The images acquired in the 0-8 minute time interval were predominantly uninterpretable due to excessive blood pool uptake. The images acquired in the 8-12 minute time interval were interpretable and compared to the conventional images obtained at 60 minutes. Overall image quality was better on the 60 minute image (17 good, 13 acceptable) compared with 8-12 minute image (3 good, 25 acceptable, 2 unacceptable). Sixteen of the 30 patients had an improvement in overall image quality by at least one category using the 60 minute delayed image. Nine of the 30 patients (2 Tc-99m sestamibi; 7 Tc-99m tetrofosmin) had at least one uninterpretable myocardial segment due to liver and/or bowel overlapping the myocardium on the 8-12 minute images vs 1 patient (1 myocardial segment) with this problem on the 60 minute delayed images (P = .005). Uninterpretable segments (total of 16) on the 8-12 minute images were confined to the apex and inferior wall. The mean SRS of the interpretable 8-12 minute images (n = 21) was 3.2 (95% confidence intervals; 1.0, 5.4) compared to 1.6 (95% confidence intervals; 0, 3.3) on the 60 minute delayed images in those patients (P = .005).
Conclusions
Overall image quality was better with fewer uninterpretable studies and a lower SRS on the rest images obtained at 60 minutes compared to early image acquisition (8-12 minutes following isotope injection). These findings do not support the routine use of early image acquisition with this new solid-state ultra-fast camera system.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Recent advances in nuclear cardiology have included the development of solid-state cardiac cameras in an effort to both improve image quality and reduce image acquisition time. Novel cardiac-dedicated solid-state gamma cameras using cadmium zinc telluride (CZT) detectors in place of sodium iodide-based detectors have demonstrated the ability to enhance image quality with improved energy and spatial resolution when compared to conventional single photon emission computed tomography (SPECT) systems. The direct conversion of a gamma ray to an electronic pulse in CZT detector systems has enabled a significant reduction in detector size. In conjunction with certain system designs (stationary, heart-focused detectors, and pinholes) this has resulted in dramatic sensitivity improvements allowing for shorter image acquisition times. Advancements in nuclear cardiology hardware and associated software have led to the development of new imaging protocols with goals of reducing both total protocol time and radiation exposure. The purpose of this study was to perform early imaging using an ultra-fast, solid-state cardiac SPECT camera (Discovery NM 530c, General Electric Healthcare) following a rest injection of technetium-99m (Tc-99m) sestamibi or tetrofosmin and to compare these earlier images to a conventional delayed image acquisition.
Methods
Study Population
Following approval by our institutional review board, 30 patients referred for a clinically indicated stress SPECT myocardial perfusion imaging (MPI) study at Mayo Clinic between the dates of January and May 2009 were enrolled and comprised the study population.
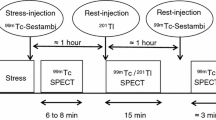
Imaging Protocol and Methods
Patients underwent supine myocardial perfusion imaging at rest using 333-407 MBq (9-11 mCi) of Technetium-99m (Tc-99m) sestamibi (n = 9) or tetrofosmin (n = 21) using an ultra-fast, solid-state cardiac SPECT camera (Discovery NM 530c, GE Healthcare). This solid-state camera system uses multiple pinhole collimators arranged in a 108° array around the myocardium. Each pinhole collimator is interfaced with a small 8 × 8 cm CZT detector. This arrangement facilitates simultaneous cardiac imaging via 19 cardiac views. The pinhole collimation uses a 5.1 mm effective diameter aperture made of tungsten, and each detector contains 32 × 32 pixilated elements with dimensions 2.5 × 2.5 mm and 5-mm-thick.1,2 Patients were imaged in the supine position with the arms elevated above the head. Automated heart positioning in the field of view was assisted by real-time imaging.
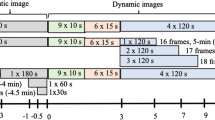
The imaging protocol is illustrated in Figure 1. Following patient and gantry positioning in an effort to predict the cardiac position within the field of view center, a 12 minute image acquisition in list mode was performed immediately following rest injection of the Tc-99m agent. The Discovery NM 530c allows for the saved data acquired in list mode format to be reformatted post-acquisition with user selection of parameters such as gamma ray energy, spatial coordinates, occurrence time, and gated ECG trigger.1 The immediate 12 minute list mode acquisition was subsequently divided into three 4-minute intervals for image reconstruction (0-4, 4-8, and 8-12 minutes). Patients also underwent a conventional delayed image acquisition at 60 minutes following the rest isotope injection using the Discovery NM 530c (image acquisition over 4 minutes).
Image Analysis
The perfusion images were interpreted by consensus of two experienced physicians. Image quality was assessed using a visual grading scale (good, acceptable, or unacceptable) which comprised both overall image quality and the degree of extracardiac radioactivity interference (good = no extracardiac activity or minor extracardiac activity not adjacent to the myocardium; acceptable = extracardiac activity adjacent to the myocardium but not significantly affecting image interpretation; unacceptable = excessive blood pool isotope activity or extracardiac activity reducing confidence in interpretation). Each myocardial segment was scored using a standard 5-point scoring system and the summed rest score (SRS) was calculated by adding the rest scores of the 17-segment model.
Statistical Analysis
All continuous variables are expressed as mean ± standard deviation. The McNemar test was used to express the differences between the categorical variables on a per-patient basis. The summed rest score comparison used a paired t test. A P value <.05 was considered significant for all comparisons.
Results
Clinical Characteristics
The clinical characteristics of the patients are shown in Table 1. The mean age of the study population was 60 ± 8 years and comprised 26 men and 4 women. The mean weight was 91.2 ± 13.2 kg with a body mass index of 30.1 ± 2.8. A history of hypertension (70%) and hyperlipidemia (77%) were common, while few patients had diabetes mellitus (10%). Approximately 1 in 4 patients had a clinical history of a prior myocardial infarction (27%) and 50% of patients had previously undergone coronary artery revascularization procedures (percutaneous coronary intervention or coronary artery bypass graft surgery).
Image Quality
The images acquired in the 0-4 minute time interval were uninterpretable due to excessive blood pool uptake, and the images acquired in the 4-8 minute time interval were predominantly uninterpretable due to either increased blood pool uptake or apical and inferior wall perfusion defects. The images acquired in the 8-12 minute time interval were interpretable and compared to the conventional images obtained at 60 minutes. Overall image quality (Figure 2) was better on the 60 minute image (17 good, 13 acceptable) compared with 8-12 minute image (3 good, 25 acceptable, 2 unacceptable). Sixteen of the 30 patients had an improvement in overall image quality by at least one category using the 60 minute delayed image. Nine of the 30 patients (2 Tc-99m sestamibi; 7 Tc-99m tetrofosmin) had at least one uninterpretable myocardial segment due to liver and/or bowel overlapping the myocardium on the 8-12 minute images vs 1 patient (1 myocardial segment) with this problem on the 60 minute delayed images (P = .005) (Figure 3). Uninterpretable segments (total of 16) on the 8-12 minute images were confined to the apex and inferior wall. The mean SRS of the interpretable 8-12 minute images (n = 21) was 3.2 (95% confidence intervals; 1.0, 5.4) compared to 1.6 (95% confidence intervals; 0, 3.3) on the 60 minute delayed images (P = .005) in those patients (Figure 4).
Resting myocardial perfusion as assessed by the summed rest scores. Individual summed rest score (SRS) data points for the patients without uninterpretable segments (n = 21) at early image acquisition and delayed image acquisition. The mean SRS of the interpretable 8-12 minute images was 3.2 (95% confidence intervals; 1.0, 5.4) compared to 1.6 (95% confidence intervals; 0, 3.3) on the 60 minute delayed images (P = .005) in those patients
Discussion
The principal findings of this study indicate that overall image quality was better with fewer uninterpretable studies and a lower SRS on the rest images obtained at 60 minutes compared to early image acquisition (8-12 minutes following isotope injection).
Many of the significant advancements in nuclear cardiology over the past few years can be attributed to the development of new solid-state gamma cameras that offer improvements in both intrinsic spatial resolution and energy resolution. More importantly, these new camera systems allow for unique designs that yield significant gains in sensitivity, allowing for shorter acquisition times and/or reduced administered doses of radiopharmaceuticals. Dedicated cardiac solid-state gamma cameras using CZT detectors in place of the sodium iodide-based detectors have demonstrated comparable or improved image quality with significantly shorter acquisition times when compared to conventional, standard dual-head detector SPECT systems.
These new designs have also spurred innovation in collimation and image processing. On conventional gamma cameras, multi-pinhole and cone-beam collimation approaches are being used in an effort to improve sensitivity, and shorten acquisition times compared to standard parallel-hole collimation. Eagle Heart Imaging (Westminster, CO) has used a multi-pinhole approach in conjunction with the Emory Reconstruction Toolbox (Syntermed, Atlanta, GA) to upgrade conventional dual-head gamma cameras with an available product referred to as MP-SPECT™.3 Another system (IQ-SPECT, Siemens) designed in part to reduce image acquisition time (reported acquisition times of 4 minutes) employs variable focus collimation, cardio-centric orbit, and a proprietary iterative reconstruction algorithm.3
These advancements in nuclear cardiology hardware and associated software have led to the development of new imaging protocols with goals of reducing both total protocol time and radiation exposure.4-6 One possibility for reducing total protocol time is to shorten the time from rest isotope injection to onset of image acquisition. Nuclear cardiology imaging and procedure guidelines recommend a 30-60 minute waiting period following injection of the conventional myocardial perfusion imaging agents, such as Tc-99m sestamibi and Tc-99m tetrofosmin, before rest image acquisition is commenced.7,8 The wait period between injection and image acquisition was incorporated into conventional practice and guidelines in order to allow for clearance of the radiotracers from the hepatic system. The presence of increased hepatic uptake on early rest image acquisitions often compromised interpretation of the left ventricular apex and inferior walls of the heart. This was due to several factors, such as incomplete angular sampling of the heart and adjacent organs (180° instead of 360°), which can result in distortion and artifact in the reconstructed images, and use of filtered back projection, which was more susceptible to the impact of increased adjacent hepatic activity on the myocardial images. The hope was that the improved angular sampling offered by the unique geometry of the Discovery NM 530c coupled with use of iterative reconstruction algorithms, would overcome the limiting factors described above and enable a reduction in the time period from injection to imaging. The presence or absence of list mode did not impact our findings. The capability of list mode acquisition was a significant benefit with the Discovery NM 530c system for this study in that it allowed us to acquire data over a 12-minute period and reconstruct any segment of that time period during post-acquisition reconstruction.
The conventional image acquisition protocols long-used in daily practice are coming under increased scrutiny with the advent of the solid-state cardiac cameras. Several investigators9,10 recently reported their experience using a novel, rapid stress thallium-201/rest Tc-99m agent myocardial perfusion protocol with a solid-state cardiac camera (D-SPECT, Spectrum Dynamics). Berman et al9 compared their rapid stress dual isotope protocol to a standard single isotope (Tc-99m) agent protocol with respect to image quality. The rest images in the rapid stress dual isotope protocol were comprised of a single 4-minute acquisition which began 2 minutes following Tc-99m isotope injection. Overall image quality in the rapid stress dual isotope protocol was either good or excellent in 96% compared to only 2 of 374 (0.5%) patients having uninterpretable or poor images. Retrospective analysis of the rest image quality demonstrated that nearly all (98.9%) were good or excellent compared with 2 (0.5%) patients with fair rest image quality and 2 (0.5%) patients with uninterpretable/poor rest image quality. The impact of extracardiac activity was limited as all images were interpretable and 83.7% of patients in the rapid dual isotope protocol had no extracardiac activity in the field of view or minor extracardiac activity not adjacent to the myocardium. These findings differ from those described in this study as we observed that images acquired in the 0-8 minute time interval were predominantly uninterpretable (due to either excessive blood pool uptake or apical and inferior wall perfusion defects) and overall image quality was deemed unacceptable in 6.7% of patients on the 8-12 minute images. In addition, 30% of patients had at least one uninterpretable myocardial segment due to liver and/or bowel interference with the myocardium on the 8-12 minute rest images. The reason for the discrepancy in overall image quality and impact of extracardiac activity in the early rest image acquisitions described by these two studies is uncertain. However, it is important to note that different types of solid-state cardiac cameras were used in this study (Discovery NM 530c) and that of Berman et al (D-SPECT system, Spectrum Dynamics). The method for image acquisition is very different between these two systems and may account for the different findings between studies. The D-SPECT employs nine small gamma cameras (4 × 16 cm) each equipped with parallel-hole collimation. During acquisition setup, each camera is ‘tuned’ to only scan a region around the myocardium (‘region-centric’ acquisition), thus minimizing inclusion of non-cardiac activity in the acquisition data. The Discovery NM 530c employs an array of 19 pin-hole gamma cameras (each 4 × 4 cm) arranged in a 3-dimensional pattern around the myocardium. While many of these 19 cameras are positioned in an array around the region of the myocardium, some are positioned superior to the heart, but orientated obliquely to look down at the myocardium, while others are positioned inferior to the heart and again angled obliquely to look up at the myocardium. This arrangement may be more sensitive to the presence of hepatic and bowel isotope activity compared to the D-SPECT system, as some of the small cameras may view the myocardium from an orientation that also includes hepatic activity. The oblique view obtained by some of these cameras makes it difficult to ascertain the full impact of hepatic activity on the reconstruction algorithm. This problem may also be compounded by the use of reconstruction techniques applying limited angle tomography where the presence of non-cardiac activity in some of the views may more readily corrupt the reconstruction.
Another study that was performed using the GE Discovery NM 530c and following a 1-day low-dose (370 MBq) stress/high-dose (740 MBq) rest protocol initiated rest imaging 15 minutes after isotope injection. Image quality on the resting images was rated good or better in 97% of patients.11 All other studies that have been published on UFC camera technology to date have reported initiation of rest imaging with the conventional 60-90 minutes delay after isotope injection.2,4,5,12-14
As described in the results section, the 60 minute delayed images demonstrated improved overall image quality, fewer uninterpretable myocardial segments, and a lower SRS. In addition to the subtle (one grade improvements) in segmental myocardial perfusion, there were examples where the apical and inferior wall myocardial perfusion dramatically improved on the 60 minute images as shown in Figure 5. These examples demonstrate the potential hazard of early image acquisition (both rest and potentially post-stress) as early acquisition-only studies may suggest the presence of myocardial infarction in the absence or significant coronary artery disease or fail to detect myocardial ischemia.
Rest myocardial perfusion images. Top panel: Short axis images (1st row, time 0-4 minutes; 2nd row, time 4-8 minutes; 3rd row, time 8-12 minutes; 4th row, time 60-64 minutes) demonstrates excessive blood pool activity on the 0-4 minute images, a discrete apical and inferior wall perfusion defect on the 4-8 and 8-12 minute images, and near-normal apical and inferior wall perfusion on the 60-64 minute images. Bottom panel: Vertical long axis images (1st row, time 0-4 minutes; 2nd row, time 4-8 minutes; 3rd row, time 8-12 minutes; 4th row, time 60-64 minutes) demonstrates excessive blood pool activity on the 0-4 minute images, a inferior wall perfusion defect on the 4-8 and 8-12 minute images, and further improvement in the inferior wall perfusion on the 60-64 minute images
Limitations
Interpretation of the images was performed as described in the methods section and relied on a semiquantitative visual analysis with consensus of two nuclear cardiologists. Computer-based quantitative analysis was not used for interpretation of the images as normal limits for this camera have not yet been established.
Conclusions
Overall image quality was better with fewer uninterpretable studies and a lower SRS on the rest images obtained at 60 minutes compared to early image acquisition (8-12 minutes following isotope injection). These findings do not support the routine use of early image acquisition with this new solid-state ultra-fast camera system.
References
Bocher M, Blevis IM, Tsukerman L, Shrem Y, Kovalski G, Volokh L. A fast cardiac gamma camera with dynamic SPECT capabilities: Design, system validation and future potential. Eur J Nucl Med Mol Imaging 2010;37:1887-902.
Esteves F, Raggi P, Folks R, Keidar Z, Wells Askew J, Rispler S, et al. Novel solid-state-detector dedicated cardiac camera for fast myocardial perfusion imaging: Multicenter comparison with standard dual detector cameras. J Nucl Cardiol 2009;16:927-34.
Slomka P, Patton J, Berman D, Germano G. Advances in technical aspects of myocardial perfusion SPECT imaging. J Nucl Cardiol 2009;16:255-76.
Buechel RR, Herzog BA, Husmann L, Burger IA, Pazhenkottil AP, Treyer V, et al. Ultrafast nuclear myocardial perfusion imaging on a new gamma camera with semiconductor detector technique: First clinical validation. Eur J Nucl Med Mol Imaging 2010;37:773-8.
Herzog BA, Buechel RR, Katz R, Brueckner M, Husmann L, Burger IA, et al. Nuclear myocardial perfusion imaging with a cadmium–zinc–telluride detector technique: Optimized protocol for scan time reduction. J Nucl Med 2010;51:46-51.
Sharir T, Slomka PJ, Berman DS. Solid-state SPECT technology: Fast and furious. J Nucl Cardiol 2010;17:890-6.
Henzlova MJ, Cerqueira MD, Hansen CL, Taillefer R, Yao S-S. ASNC imaging guidelines for nuclear cardiology procedures: Stress protocols and tracers. 2009. Available at: http://www.asnc.org/section_73.cfm
Holly TA, Abbott BG, Al-Mallah M, Calnon DA, Cohen MC, DiFilippo FP, et al. Single photon-emission computed tomography. J Nucl Cardiol 2010;17:941-73.
Berman DS, Kang X, Tamarappoo B, Wolak A, Hayes SW, Nakazato R, et al. Stress thallium-201/rest technetium-99m sequential dual isotope high-speed myocardial perfusion imaging. J Am Coll Cardiol Imaging 2009;2:273-82.
Nakazato R, Tamarappoo BK, Kang X, Wolak A, Kite F, Hayes SW, et al. Quantitative upright-supine high-speed SPECT myocardial perfusion imaging for detection of coronary artery disease: Correlation with invasive coronary angiography. J Nucl Med 2010;51:1724-31.
Gimelli A, Bottai M, Giorgetti A, Genovesi D, Kusch A, Ripoli A, et al. Comparison between ultrafast and standard single-photon emission ct in patients with coronary artery disease/clinical perspective. Circulation 2011;4:51-8.
Duvall W, Croft L, Godiwala T, Ginsberg E, George T, Henzlova M. Reduced isotope dose with rapid SPECT MPI imaging: Initial experience with a CZT SPECT camera. J Nucl Cardiol 2010;17:1009-14.
Sharir T, Ben-Haim S, Merzon K, Prochorov V, Dickman D, Ben-Haim S, et al. High-speed myocardial perfusion imaging: Initial clinical comparison with conventional dual detector anger camera imaging. J Am Coll Cardiol Imaging 2008;1:156-63.
Sharir T, Slomka PJ, Hayes SW, DiCarli MF, Ziffer JA, Martin WH, et al. Multicenter trial of high-speed versus conventional single-photon emission computed tomography imaging: Quantitative results of myocardial perfusion and left ventricular function. J Am Coll Cardiol 2010;55:1965-74.
Acknowledgment
Drs Askew and O’Connor were investigators of a research grant funded by GE Healthcare to evaluate the Discovery NM 530c.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Askew, J.W., Miller, T.D., Ruter, R.L. et al. Early image acquisition using a solid-state cardiac camera for fast myocardial perfusion imaging. J. Nucl. Cardiol. 18, 840–846 (2011). https://doi.org/10.1007/s12350-011-9423-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-011-9423-7